Abstract
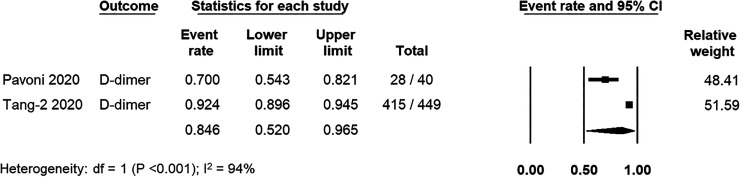
Coagulation activation has been reported in several cohorts of patients Coronavirus Disease 2019 (COVID-19). However, the true burden of systemic coagulopathy in COVID-19 remains unknown. In this systematic review and meta-analysis, we performed a literature search using PubMed, EMBASE, and Cochrane Database to identify studies that reported the prevalence of systemic coagulopathy using established criteria in patients with COVID-19. The primary outcome was the prevalence of systemic coagulopathy (disseminated intravascular coagulation [DIC] and/or sepsis-induced coagulopathy [SIC]). Pooled prevalences and 95% confidence intervals [CIs] were calculated using random-effects model. A total of 5 studies including 1210 patients with confirmed COVID-19 were included. The pooled prevalence of systemic coagulopathy was 7.1% (95%CI: 3.2%,15.3%, I2 = 93%). The pooled prevalence of DIC (N = 721) and SIC (N = 639) were 4.3% (95%CI 1.7%, 10.4%, I2 = 84%) and 16.2% (95%CI: 9.3%, 26.8%, I2 = 74%), respectively. Only 2 studies reported the prevalence of elevated D-dimer levels with the pooled prevalence of 84.6% (95%CI: 52.0%,96.5%, I2 = 94%). Average D-dimer and fibrinogen levels were remarkably increased, while platelet counts, PT, and aPTT ratios were minimally affected in COVID-19. The estimated prevalence of systemic coagulopathy in patients with COVID-19 was low despite D-dimer elevation in most patients. Relatively low systemic coagulopathy in COVID-19 may contribute to the high incidence of thrombosis rather than bleeding in patients with COVID-19.
Keywords: systemic coagulopathy, disseminated intravascular coagulation, sepsis-induced coagulopathy, COVID-19, meta-analysis
Introduction
Since the first cluster of pneumonia was identified in China in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 33 million individuals and caused more than 1 million deaths worldwide.1 Although SARS-CoV-2 predominantly affects the respiratory system, a significant proportion of patients with Coronavirus Disease 2019 (COVID-19) are complicated by systemic inflammatory response syndrome and multiple organ failure mimicking severe bacterial sepsis.2 In addition, increased coagulation activation has been reported in a majority of patients with COVID-19 and is associated with increased mortality.3,4 Notably, anticoagulant therapy was shown in one study to be associated with decreased mortality in severe COVID-19 patients with coagulopathy.5 However, an early report from the largest cohort in China documented very low prevalence (0.1%) of disseminated intravascular coagulation (DIC) in SARS-CoV-2 infected patients.6 Despite markedly elevated D-dimer levels, COVID-19 patients have relatively normal levels of platelets, prothrombin time (PT) and fibrinogen leading to insufficient criteria to support diagnosis of DIC as defined by the DIC score of the International Society of Thrombosis and Hemostasis (ISTH).3–6 Hypothetically, pulmonary intravascular coagulopathy may mainly contribute to hemostatic alterations in patients with COVID-19 rather than DIC linked to systemic infections.7,8 Recently, the ISTH has proposed the sepsis-induced coagulopathy (SIC) score to identify patients with sepsis-associated organ dysfunction and coagulopathy.9 A Chinese cohort using the SIC score identified one fifth patients with COVID-19 met the criteria for diagnosis of SIC.5 Until now, the burden of SARS-CoV-2 induced systemic coagulopathy has yet determined. We conducted a systematic review and meta-analysis to estimate the burden of systemic coagulation activation in patients with COVID-19.
Methods
The protocol for this review was prespecified, and the study was subsequently conducted following Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.10 The primary objective of this study was to evaluate the prevalence of systemic coagulation activation (DIC and/or SIC) in hospitalized patients with COVID-19. The secondary aims were to characterize abnormal coagulation tests in patients with COVID-19.
Data Source, Search Strategy and Study Selection
A systematic search of electronic databases was performed using PubMed, EMBASE, and Cochrane Library Database from inception to May 22nd, 2020 to identify studies reporting the prevalence of DIC or SIC in COVID-19 patients. The following search terms were used: disseminated intravascular coagulation, DIC, sepsis-induced coagulopathy, SIC, novel coronavirus 2019, COVID-19, SARS-CoV-2 and 2019-nCoV.
The inclusion criteria for eligible studies are as follows: (1) randomized controlled trials, retrospective or prospective observational studies, or case series of adults (age ≥ 18 years) who were hospitalized for COVID-19, (2) included at least 10 patients and (3) reported the incidence of SIC as defined by the ISTH criteria or DIC as defined by either the ISTH or the Japanese Association for Acute Medicine (JAAM) criteria.9,11 Non-original articles (such as reviews, commentaries, or guidelines) and duplicated studies were excluded. Two authors (N.U. and T.C.) independently searched the literature, screened titles and abstracts, and reviewed full texts to identify potentially eligible studies. Disagreements were resolved by consensus or a third reviewer (P.R.) when necessary. The selection result was reported according to the PRISMA flowchart.
Data Extraction
The primary outcome was the prevalence of systemic coagulopathy (DIC and/or SIC). The secondary outcomes were the prevalence of DIC, the prevalence of SIC, the prevalence of elevated D-dimer, and the values of coagulation parameters (i.e., platelet counts, prothrombin time [PT], activated partial thromboplastin time [aPTT], D-dimer levels, and fibrinogen levels). DIC was defined as ISTH DIC score of ≥ 5 or JAAM DIC score of ≥ 4, while SIC was defined as ISTH SIC score of ≥ 4. Elevated D-dimer was defined according to individual studies.
For each study, the following data were extracted: study design, inclusion criteria, number of participants, baseline characteristics of participants (age, sex, and underlying diseases), administration of anticoagulants, proportion of patients with severe pneumonia or intensive care unit (ICU) admission, prevalence of DIC and/or SIC, prevalence of elevated D-dimer, mortality rate, and the following laboratory variables: platelet counts, PT, aPTT, D-dimer levels, and fibrinogen levels.
Quality Assessment
The methodological quality of included studies was performed independently by 2 authors (N.U. and T.C.) using a validated tool for assessing studies reporting prevalence data.12 The tool contains 10 items assessing the external validity and internal validity of the study. For each item, a score of 0 and 1 was assigned to the answers yes and no, respectively. The summary assessment of overall risk of bias was rated according to the responses to the 10 items and included studies were classified based on the total score as low (0-3), moderate (4-6), or high risk (7-9) of bias.
Data Analysis
The meta-analysis was performed using Comprehensive Meta-analysis (Version 2; Biostat, Englewood, NJ, USA. The weighted mean prevalences of primary and secondary outcomes were calculated using DerSimonian and Laird method with random-effects model and were reported as pooled prevalences with 95% confidence intervals (CIs). For laboratory parameters, the pooled mean was calculated. Parameters presented in medians and interquartile ranges were converted to estimated means and standard deviations following the formula as previously reported.13
Statistical heterogeneity was assessed using I2 statistic, which measures the inconsistency across study results. Inter-study heterogeneity was assigned as insignificant (I2 = 0-25%), low (I2 = 26-50%), moderate (I2 = 51-75%), and high (I2 > 75%).14 The funnel plot for evaluation of publication bias was not performed due to the low number of studies included (less than 10 studies).
Results
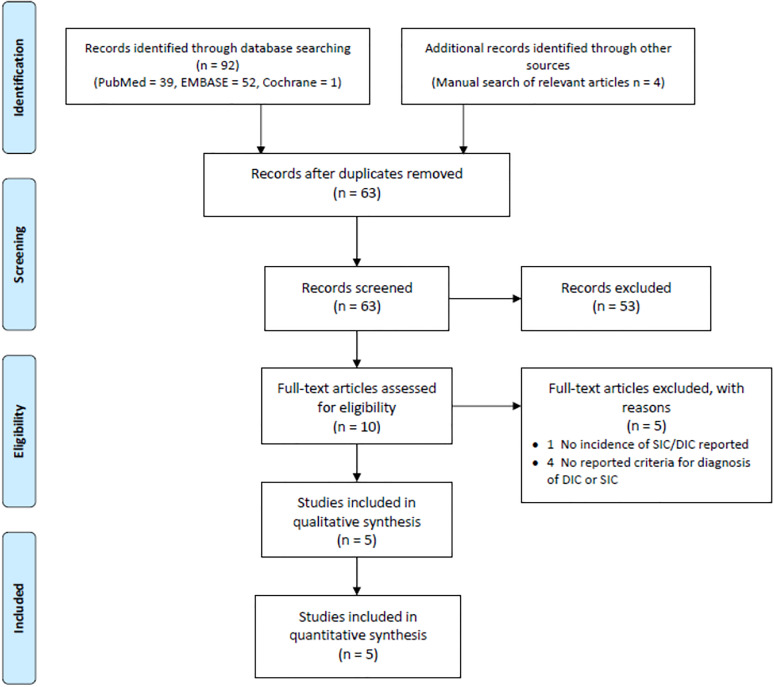
The PRISMA flow diagrams are shown in Figure 1. A total of 63 unique studies were identified by literature search and were screened by title and abstract. Of these, 53 were excluded and 10 full texts were screened for eligibility. Eventually, 5 studies met the eligibility criteria and were included in the meta-analysis.3,5,15-17 All 5 included studies were assessed to have low risk of bias (Supplementary data, Table S1).
Figure 1.
PRISMA flow diagram.
Study Characteristics
The main characteristics of the 5 included studies are summarized in Table 1. A total of 1210 patients were included for analysis. The number of participants of individual studies ranged from 40 to 449. The average age was 61.6 years and the proportion of male patients was 64.1%. All studies included hospitalized patients with COVID-19. More than half of the included patients (700 of 1210, 57.9%) had severe pneumonia and/or admitted in the ICU. In the 3 European cohorts, all patients admitted in the ICU received heparin for thromboprophylaxis.15–17
Table 1.
Demographic and Clinical Data of Studies on the Prevalence of Systemic Coagulopathy in Patients With COVID-19.
| Authors | Study design | N | Inclusion criteria | Study period | Primary outcome | Diagnosis criteria for DIC/SIC | Timing of DIC/SIC assessment | Mean age (years) | M/F (N) | ICU | Prophylactic Anticoagulation, N (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Helms 202015 | Prospective | 150 | All patients with SARS-CoV-2 ARDS included on admission in intensive care units | March 3 rd to March 31st 2020 | Any thrombotic events | ISTH and JAAM for DIC/ISTH for SIC | During ICU stay | 62.3 | 122/28 | 150 (100%) | 150 (100%); LMWH or UH (100%) |
| Lodigiani 202016 | Retrospective | 388 | Consecutive adult symptomatic patients with laboratory-proven COVID-19 | February 13th to April 10th 2020 | Venous and arterial thromboembolic events | ISTH for DIC | Not specified | 65.3 | 264/124 | 61 (15.7%) | 307 (79.1%); 61/61 (100%) in ICU, 246/327 (75.2%) in general wards; LMWH (100%) |
| Pavoni 202017 | Retrospective | 40 | Severe COVID-19 admitted to ICU | February 28th to April 10th 2020 | Coagulation function by rotational thromboelastometry | ISTH for SIC | SOFA score at ICU admission; laboratory profiles on admission, day 5 and day 10 | 61 | 24/16 | 40 (100%) | 40 (100%); LMWH (100%) |
| Tang 20203 | Retrospective | 183 | Consecutive patients with confirmed novel coronavirus pneumonia |
January 1st to February 3 rd 2020 | Coagulation parameters | ISTH for DIC | On admission and during hospital stay | 54.1 | 98/85 | NR | NR |
| Tang 20205 | Retrospective | 449 | Patients with severe COVID-19 enrolled into the study | January 1st to February 13th 2020 | 28-day mortality | ISTH for SIC | At the time the patient met the definition of severe COVID-19 | 65.1 | 268/181 | NR | 99 (22%)1; 94 (21%) LMWH and 5 (1%) UH |
1Patients had received heparin for at least 7 days. DIC, disseminated intravascular coagulation; SIC, sepsis-induced coagulopathy; JAAM, Japanese Association for Acute Medicine; ISTH, International Society on Thrombosis and Haemostasis; M/F, male/female; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COVID-19, coronavirus disease 2019; NR, not reported; LMWH, low molecular weight heparin; UH, unfractionated heparin.
Regarding the hemorrhagic and thrombotic events, Helms and colleague15 reported a 2.7% (4/150) bleeding rate, while Lodigiani and colleague16 reported no bleeding episodes in 388 patients with COVID-19 in their cohort. Thromboembolism was reported in 3 studies.15–17 Thromboembolic rates were 18% (27/150),15 7.7% (28/362)16 and 50% (20/40)17 in Helms, Lodigiani and Pavoni studies, respectively. We did not perform pooled prevalence of these events in patients with COVID-19 as it is beyond the scope of our study. In addition, to precisely estimate the bleeding and thromboembolic rates in COVID-19 patients requires different searching strategies.
Prevalence of Systemic Coagulopathy in Patient With COVID-19
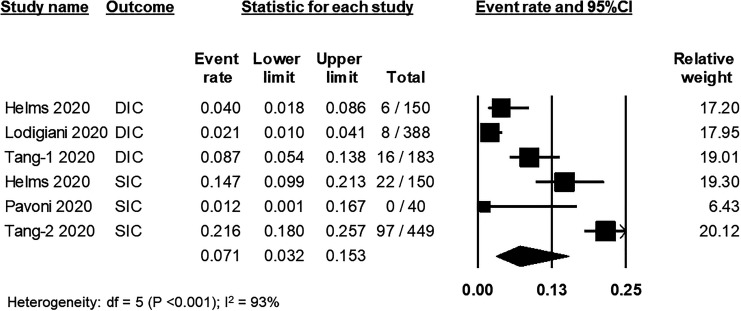
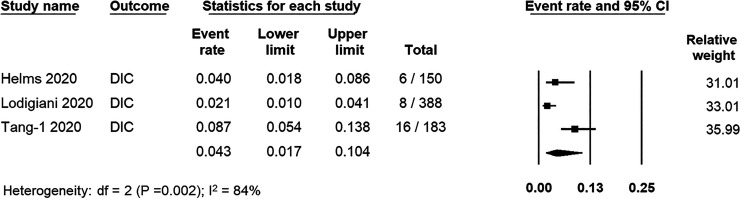
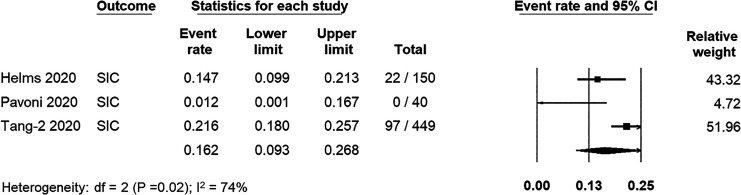
From 5 studies (N = 1210 patients), the prevalence of systemic coagulopathy was 7.1% (95% CI: 3.2%, 15.3%; I2 = 93%) (Figure 2). Three studies (N = 721 patients)3,15,16 reported the prevalence of DIC, while 3 studies (N = 639 patients)3,5,15 reported the prevalence of SIC. The pooled prevalence of DIC was 4.3% (95%CI: 1.7%, 10.4%; I2 = 84%) (Figure 3), while the pooled prevalence of SIC was 16.2% (95%CI: 9.3; I2 = 74%) (Figure 4).
Figure 2.
Forest plot showing pooled estimated prevalence of systemic coagulopathy in COVID-19.
Figure 3.
Forest plots showing pooled estimated prevalence of disseminated intravascular coagulation in COVID-19.
Figure 4.
Forest plot showing pooled estimated prevalence of sepsis-induced coagulopathy in COVID-19.
The prevalence of DIC varied according to the different diagnostic criteria that were utilized. Among 150 patients, Helms and colleagues reported that none were diagnosed with DIC using the ISTH criteria, whereas 6 patients would fulfill the diagnosis of DIC using JAAM criteria.15 The estimated prevalence of DIC using only the ISTH criteria was 2.8% (95%CI: 0.7%, 11.2%; I2 = 87%).
Although the average D-dimer levels were substantially elevated in all 5 studies, only 2 studies reported the prevalence of elevated D-dimer levels.5,17 From these 2 studies, the pooled prevalence of elevated D-dimer levels was 84.6% (95%CI: 52.0%, 96.5%; I2 = 94%) (Figure 5).
Figure 5.
Forest plot showing pooled estimated prevalence of D-dimer elevation in COVID-19.
Coagulation Parameters in Patients With COVID-19
Hemostatic parameters associated with systemic coagulopathy in patients with COVID-19 are summarized in Table 2. D-dimer levels3,5,15-17 were reported in all studies, while platelet counts5,15,17, fibrinogen levels3,15,17 and antithrombin activities3,15,17 were reported in 3 individual studies. The pooled means (± standard errors) of platelet counts, D-dimer levels, fibrinogen levels and antithrombin activities were 223 × 109 (± 21.1 × 109)/L, 1659.6 (± 199.7) ng/mL, 6.78 (± 1.21) g/L, and 90.0 (± 0.6), respectively (Table 3).
Table 2.
Coagulation Parameters Associated With Systemic Coagulopathy in Patients Infected With COVID-19.
| Authors | N | Platelet count (× 109/L) | PT or INR or PT %activity | aPTT | D-dimer levels (ng/mL) | Fibrinogen levels (g/L) | Antithrombin activity (%) |
|---|---|---|---|---|---|---|---|
| Helms, 202015 | 150 | 200 (152; 267)1
[150-400]2 |
1.12 (1.05; 1.25) [1.00-1.15] |
1.2 (1.1; 1.3) [0.7-1.2] |
2270 (1160; 20000) [< 500] |
6.99 (6.08; 7.73) [2-4] |
91 (78;102) |
| Lodigiani, 202016 | 388 | NR | NR | NR | Survivors n = 215: 353 (236; 585)1 Non-survivors n = 70: 869 (470; 2130) |
NR | NR |
| Pavoni, 202017 | 40 | 317.5 ± 1683 | 65.1% ± 9.8 | 32.2 ± 2.9 sec | 1556 ± 1090 | 8.96 ± 1.10 | 87.2 ± 13.5 |
| Tang, 20203 | 183 | NR | 13.7 (13.1; 14.6) sec [11.5-14.5] |
41.6 (36.9; 44.5) sec [29.0-42.0] |
660 (380-1500) [< 500] |
4.55 (3.66; 5.17) [2-4] |
91 (83;97) |
| Tang, 20205 | 449 | 215 ± 100 [125-350] |
15.2 ± 5 sec [11.5-14.5] |
NR | 1940 (900-9440) [< 500] |
NR | NR |
NR = not reported; 1Median (interquartile 1; interquartile 3); 2[normal range]; 3Mean ± standard deviation.
Table 3.
Pooled Analysis of Coagulation Parameters Associated With Systemic Coagulopathy in Patients With COVID-19.
The PT as well as PT %activity and INR values3,15,17 were within the normal range in most reported studies, with the exception of a minimal prolongation in one report.5 The aPTT or aPTT ratio were within normal range in all reported cohorts.3,15,17 Due to the inconsistency in the reported formats, we were not able to calculate the pooled mean for PT and aPTT.
Discussion
In this systematic review and meta-analysis that included 5 studies from 4 countries (N = 1210 patients), we report a relatively low prevalence (7.1%) of systemic coagulopathy in hospitalized COVID-19 patients. When analyzed separately, the pooled prevalence of DIC and SIC were 4.3% and 16.2%, respectively. D-dimer elevation occurred in the majority of patients (84.6%). The higher prevalence of SIC compared to DIC in COVID-19 may be mainly explained by the higher threshold for thrombocytopenia (<150 × 109/L in SIC vs <100 × 109/L in DIC) and the incorporation of sequential organ failure assessment (SOFA) score, especially the respiratory SOFA which is the main organ involvement in COVID-19.5 Therefore, the SIC score may be more sensitive than the DIC score for detecting systemic coagulopathy in patients suffering from infection-associated organ dysfunctions such as acute lung injuries in COVID-19. Further studies for applying SIC score in detecting systemic coagulopathy in non-septic organ dysfunctions are warranted.
Systemic coagulation activation leading to DIC or SIC is a disorder characterized by a widespread intravascular activation of coagulation due to the crosstalk between the immune and inflammatory response and the coagulation system. Various infectious agents and non-infectious insults lead to immune stimulation, especially the innate immune system, and release of inflammatory cytokines which subsequently trigger activation of coagulation and extensive microvascular thrombosis as well as multi-organ dysfunction.18,19 However, different organs showed variable procoagulant responses toward inflammatory cytokines and various degrees of microthrombus formation in their vasculature following DIC. Vascular bed-specific hemostasis and tissue microenvironment are postulated to explain the marked differences in localized thrombus formation among the involved organs, in which lung is among the organs most commonly affected by infection and sepsis.20,21
The first cohort of COVID-19 patients from China included 1099 patients and reported only 1 (0.1%) case diagnosed with DIC.6 However, the criteria for DIC diagnosis was not specified in this cohort. Subsequent cohorts from China reported the prevalence of DIC and SIC using the ISTH criteria of 8.7% and 21.6%, respectively.3,5 A recent meta-analysis, which included 22 studies from China with a total of 4889 COVID-19 patients, reported a pooled DIC prevalence of 6.2% (95%CI: 2.6%, 9.9%).22 However, most studies included in this analysis did not specify the criteria for diagnosis of DIC.
From our meta-analysis, elevated D-dimer was found in the majority of patients. Additionally, Helms and colleague reported that greater than 95% of patients had elevated D-dimer and fibrinogen levels. In contrast, platelet counts, PT and aPTT values were normal or minimally affected in most patients with COVID-19, while fibrinogen levels were significantly elevated. In addition, antithrombin activities, which were incorporated in the modified JAAM-DIC criteria,11 remained within normal ranges in most patients with COVID-19. Therefore, D-dimer elevation is probably secondary to the breakdown of pulmonary microthrombi by local fibrinolysis.23 Taken together, hemostatic alterations in patients infected with SARS-CoV2 may be localized in pulmonary microvasculature rather than involved systemic microcirculation.
The findings from our study suggest that coagulation activation evidenced by elevated D-dimer levels is very common in COVID-19. In contrast, systemic coagulopathy is relatively infrequent. This may contribute to the high incidence of thrombosis rather than bleeding in patients affected with SARS-CoV2.24 Of 5 studies included in our analysis, the bleeding events in patients with COVID-19 were apparently low, while thromboembolism was much more prevalent.15–17 The precise estimation of bleeding as well as thromboembolism in patients with COVID-19 requires a meta-analysis which includes a larger number of patients.
The pathological examination obtained from lung autopsy in patients with COVID-19 demonstrated widespread thrombosis with microangiopathy in pulmonary vessels. In addition, alveolar capillary microthrombi were nearly 10 times more prevalent in patients with COVID-19 than in patients with influenza with acute respiratory distress syndrome.25 Notably, the pooled prevalence of DIC reported in our study (4.3%) is relatively lower than those previously reported in severe sepsis or non-COVID-19 severe pneumonia (30%).26 These findings suggest localized coagulation dysregulation in pulmonary vasculature leading to pulmonary intravascular coagulopathy rather than systemic coagulopathy in COVID-19. The mechanisms underlying pulmonary vascular disease in COVID-19 were extensively reviewed in recent publications.7,8,23,27 However, the mechanistic studies investigating hemostatic alterations in COVID-19 are still lacking.
Our study is the first meta-analysis focusing on only systemic coagulopathy that were diagnosed on the basis of validated scoring systems. This strategy strengthens the accuracy of the reported DIC or SIC events in the individual studies as well as the pooled estimate summarized by in our meta-analysis. However, several limitations should be considered in our study. First, all included studies were observational studies, with most being retrospective in design. Thus, there were high heterogeneity, both among and within studies, with respect to patient characteristics, timing and ascertainment of DIC/SIC, and the distribution of potentially relevant confounders such as the use of prophylactic anticoagulation. In addition, due to the lack of primary data and limited number of studies, we were not able to explore the outcomes in specific subgroups, the effects of anticoagulation, or the association of systemic coagulopathy and mortality in COVID-19. Currently, there are several prospective studies as well as clinical trials evaluating efficacies of anticoagulants and other novel agents in the treatment of patients with severe COVID-19, and their results will be available shortly. An updated meta-analysis may be required when relevant data from prospective cohorts and clinical trials are published.
Conclusion
Hemostatic disturbance is evidenced in patients with COVID-19. Although elevated D-dimer levels were systematically detected in most patients with COVID-19, the prevalence of systemic coagulopathy was much lower. Pulmonary intravascular coagulopathy may play an important role hemostatic alterations in SARS-CoV2 infected patients. Additionally, our data may explain the higher risk of thromboembolism rather than bleeding in COVID-19. Due to limited numbers of studies and heterogeneity of data, a future meta-analysis may be warrant when more relevant evidence becomes available.
Supplemental Material
Supplemental Material, sj-pdf-1-cat-10.1177_1076029620987629 for Systemic Coagulopathy in Hospitalized Patients With Coronavirus Disease 2019: A Systematic Review and Meta-Analysis by Noppacharn Uaprasert, Chatphatai Moonla, Darintr Sosothikul, Ponlapat Rojnuckarin and Thita Chiasakul in Clinical and Applied Thrombosis/Hemostasis
Footnotes
Authors’ Note: NU and TC contributed to study design, data collection, data interpretation, statistical analysis, and drafting of the manuscript. CM and DS contributed to study design and critical review of the manuscript. PR contributed to study design, data interpretation and critical review of the manuscript. All authors have read the manuscript and approved its submission.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Noppacharn Uaprasert  https://orcid.org/0000-0003-4562-9139
https://orcid.org/0000-0003-4562-9139
Chatphatai Moonla  https://orcid.org/0000-0001-6257-0867
https://orcid.org/0000-0001-6257-0867
Ponlapat Rojnuckarin  https://orcid.org/0000-0001-7912-1996
https://orcid.org/0000-0001-7912-1996
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Worldometer. COVID-19 coronavirus pandemic. Published 2020 Accessed September 28, 2020. https://www.worldometers.info/coronavirus/
- 2. Li H, Liu L, Zhang D, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395(10235):1517–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McGonagle D, O’Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020;2(7):e437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Levi M, Thachil J. Coronavirus disease 2019 coagulopathy: disseminated intravascular coagulation and thrombotic microangiopathy-either, neither, or both. Semin Thromb Hemost. 2020;46(7):781–784. doi:10.1055/s-0040-1712156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Iba T, Levy JH, Warkentin TE, Thachil J, van der Poll T, Levi M; Scientific and Standardization Committee on DIC, and the Scientific and Standardization Committee on Perioperative and Critical Care of the International Society on Thrombosis and Haemostasis. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17(11):1989–1994. [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Iba T, Di Nisio M, Thachil J, et al. Revision of the Japanese Association for Acute Medicine (JAAM) disseminated intravascular coagulation (DIC) diagnostic criteria using antithrombin activity. Crit Care. 2016;20:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. [DOI] [PubMed] [Google Scholar]
- 13. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring in consistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Helms J, Tacquard C, Severac F; et al. CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis). High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lodigiani C, Iapichino G, Carenzo L; et al. Humanitas COVID-19 Task Force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pavoni V, Gianesello L, Pazzi M, Stera C, Meconi T, Frigieri FC. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID-19 pneumonia. J Thromb Thrombolysis. 2020;50(2):281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gando S, Levi M, Toh C-H. Disseminated intravascular coagulation. Nat Rev Dis Prim. 2016;2(1):16037. [DOI] [PubMed] [Google Scholar]
- 19. Ito T. PAMPs and DAMPs as triggers for DIC. J Intensive Care. 2014;2(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosenberg RD, Aird WC. Vascular-bed-specific hemostasis and hypercoagulable states. N Engl J Med. 1999;340(20):1555–1564. [DOI] [PubMed] [Google Scholar]
- 21. Levi M, van der Poll T, Schultz M. Systemic versus localized coagulation activation contributing to organ failure in critically ill patients. Semin Immunopathol. 2012;34(1):167–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jin S, Jin Y, Xu B, Hong J, Yang X. Prevalence and impact of coagulation dysfunction in COVID-19 in China: a meta-analysis. Thromb Haemost. 2020;120(11):1524–1535. doi:10.1055/s-0040-1714369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kwaan HC. Coronavirus disease 2019: the role of the fibrinolytic system from transmission to organ injury and sequelae. Semin Thromb Hemost. 2020;46(7):841–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Al-Samkari H, Karp Leaf RS, Dzik WH, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136(4):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Park JY, Park S, Park SY, et al. Day 3 versus day 1 disseminated intravascular coagulation score among sepsis patients: a prospective observational study. Anaesth Intensive Care. 2016;44(1):57–64. [DOI] [PubMed] [Google Scholar]
- 27. Thachil J, Srivastava A. SARS-2 coronavirus-associated hemostatic lung abnormality in COVID-19: is it pulmonary thrombosis or pulmonary embolism? Semin Thromb Hemost. 2020;46(7):777–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-cat-10.1177_1076029620987629 for Systemic Coagulopathy in Hospitalized Patients With Coronavirus Disease 2019: A Systematic Review and Meta-Analysis by Noppacharn Uaprasert, Chatphatai Moonla, Darintr Sosothikul, Ponlapat Rojnuckarin and Thita Chiasakul in Clinical and Applied Thrombosis/Hemostasis