Abstract
Background
Inequality in gender varies across social contexts, which may influence the health of both men and women. Based on theories of gender as a social system, we examine whether systematic gender inequality at the macro-level influences health of men and women.
Method
Using harmonized panel data from the Gateway to Global Aging Data in 23 high- and middle-income countries (N = 168 873), we estimate disability prevalence and incidence for men and women ages 55–89 (2000–2016). Within each country or geographic region, we also investigate gender differences in age gradients of the probability of disability onset. We, then, pool data from all countries and test the hypothesis that gender inequality increases the probability of disability onset.
Results
We found substantial cross-country variation in disability incidence rates, and this variation is greater for women than for men. Among ages 65–69, disability incidence rates ranged from 0.4 to 5.0 for men and from 0.5 to 9.4 for women. Our within-country analysis showed significant gender differences in age gradients of the probability of disability onset in the United States, Korea, Southern Europe, Mexico, and China, but not in Northern, Central, and Eastern Europe, England, and Israel. Testing hypothesized effects of gender inequality, we find that gender inequality is significantly associated with the probability of disability onset for women, but not for men.
Conclusions
Macro-level societal gender inequality is significantly associated with the probability of disability onset for women. Reducing and eliminating gender inequality is crucial to achieving good health for women.
Keywords: Activities of daily living, Cross-country, Health disparity, Longitudinal analysis
Gender takes a prominent place in the health disparities literature. In contrast to a person’s biological status of sex, gender refers to the culturally defined roles, responsibilities, attributes, and entitlements associated with being a woman or man in a social context (1). In explaining the observed difference between men and women, recent scholarship has called for “contextualizing” gender difference in health research (2–4). This approach refers to taking a step further from the primary emphasis on individual-level differences in biological, behavioral, and social factors to expand the analysis to examine the effects of macro-level structural differences.
Building on this literature, we examine the association between macro-level gender inequality and the health of men and women. Gender inequality is a characteristic of most societies. Although reducing gender inequality has been an important goal globally in the past 2 decades, many countries are lagging behind, leaving gender parity as one of the core goals of the United Nations’ 2030 Agenda for Sustainable Development (5). Recognizing the critical importance of this issue, recently the Lancet commissioned a series of papers on gender equality and health (1,6–8), providing a conceptual framework for the link between gender inequalities and health based on the theories of gender as a social system. Briefly, individuals born biologically male or female develop into gendered beings, and sexism and patriarchy intersect with other forms of discrimination to structure pathways, such as differential exposures, health-related behaviors, and unequal access to care, leading to poor health. The feminist sociology (1,2) and economics literatures (9,10) found that gender inequalities in power and resources negatively shape the health of women, and as recent health disparities literature signifies in “biological embedding,” gender inequalities affect an individual on a molecular and physiological level and these burdens accumulate over a lifetime (4,11). Further, structural inequalities undermine the social fabric and make the entire society less productive and healthy (1,3).
Based on this conceptual framework, we hypothesize a negative association between macro-level gender inequality and the health of both men and women. We test this hypothesized relationship after controlling for other macro-level factors as well as individual-level characteristics, examining whether living in a society where gender inequality is more pronounced increases the health risk, for both men and women. This work builds on the growing body of the literature on structural sexism (3,12). It is important to note that the hypothesized negative relationship for men is consistent with modern feminist studies of masculinities (13), but contrary to the conflict theory of classical gender stratification that views higher level of gender inequality provides benefits to the men (14). According to modern feminist studies of masculinities, patriarchal social systems foster a toxic culture that harms men through multiple pathways. Hegemonic gender norms linked to gender inequality emphasize beliefs and practices (eg, strength and invulnerability) that lead to poor health-related beliefs and behaviors, limited social roles, restrictive and unattainable expectations, and reduced social support, all negatively impacting men’s psychosocial and emotional experiences (14,15).
For the health outcome, our analysis focuses on disability, narrowly defined as limitations in activities of daily living (ADL). While women outlive men in almost every society, women may suffer from more physical limitations than men of the same age in later life (16). We examine both disability prevalence and incidence, as disability prevalence rates provide good estimates of the disability burden, and disability incidence rates from representative samples are excellent measures of risk (17). While cross-sectional studies typically find that women are more likely to report disabilities than men, a systematic review of gender differences in disability incidence has not yielded consistent findings (18). Further, the majority of relevant studies have been conducted in the United States and other high-income countries, with a recent exception by Auais and colleagues (19), who studied disability incidence in Canada, Albania, Colombia, and Brazil (N = 1506). Building on this literature, we estimate age-specific, country-level disability prevalence and incidence rates for men and women, drawing on nationally representative samples of older adults in 23 high- and middle-income countries (N = 168 873).
Pooling panel data over a 16-year period from all 23 countries, we then investigate gender differences in the probability of disability onset, and examine the relationship with gender inequality, while controlling for other potential risk factors for disability onset, such as individual-level risk factors, including age, education, and lifetime occupation. Older age and lower education have been found to be important risk factors for disability, and individuals without a lifetime occupation have been found to have an increased risk for developing disability (20,21).
Further, we also control for other macro-level environmental factors that might influence the onset of disability, such as the level of economic development and public health insurance coverage. Economic development is considered an important determinant of population health (22). There exists a strong positive association between average income of the country and indicators of population health status across countries. Economic development can improve nutrition through an increase in the consumption of nutritious food, and it may affect the supply side of health if it allows governments to increase spending on effective public health services. There is a consistent, positive relationship between health insurance coverage and health-related outcomes in the prior literature (23). The best evidence suggests that health insurance is associated with more appropriate use of health care services and better health outcomes.
Economic development is closely related to gender inequality. Gender inequality is often higher in poorer populations, both within and across countries (24). Such close association between economic development and gender inequality calls for an estimation strategy that controls for economic development in order to tease out the independent effect of gender inequality, which was lacking in prior cross-country analyses. For example, a cross-sectional study by Mechakra-Tahiri and colleagues (25) reports larger gender gaps in disability in regions with higher gender inequality. This is one of the first studies showing evidence of the relationship between gender inequality and the gender gap in disability, but whether this association would be held up after controlling for economic development calls for further study. In the United States, Homan (3) recently estimated health effects of state-level gender inequality while controlling for state-level poverty and individual-level risk factors and reported its harmful effects on both men’s and women’s morbidity, self-reports of health, and physical functioning. This is a significant improvement over Kawachi and colleagues’ (26) work, which examined the bivariate association between state-level variations in gender inequality with mortality and functional health in the United States. Expanding this growing literature, we investigate whether country-level gender inequality is associated with the risk of disability onset foremen and women in 23 high- and middle-income countries.
Figure 1 summarizes these theories into our conceptual model. It postulates that health across the life course is affected by individual characteristics (education and work experience) and the macro-level environment (gender inequality, economic development, and public health insurance), which themselves are also related to education and work experience. Implicit in this simplified figure, but central to our study, is that the effect of gender inequality is likely to be larger for women than for men.
Figure 1.
Conceptual model.
Method
Data
We use the harmonized data files developed by the Gateway to Global Aging Data (g2aging.org), an NIH-funded data and information portal. These harmonized data files are designed for cross-country analysis using the international family of Health and Retirement Studies. The first of these studies was the Health and Retirement Study (HRS), which started in 1992 as a nationally representative panel study of people over the age of 50 living in the United States and their spouses. The HRS has been conducted biennially since its start and has added additional cohorts every 60 years.
Since 2001, a growing number of sister studies have been started around the world, which are purposefully designed to be comparable to the HRS. These sister studies include the Mexican Health and Aging Study (MHAS), the English Longitudinal Study of Ageing (ELSA), the Survey of Health, Ageing and Retirement in Europe (SHARE), the Korean Longitudinal Study of Aging (KLoSA), and the China Health and Retirement Longitudinal Study (CHARLS). The HRS family studies are coordinated with the explicit goal of facilitating cross-country comparisons. Like the HRS, most or all of these studies have (i) biennial interviews with respondents and their spouses; (ii) a multidisciplinary questionnaire design that elicits a wealth of information about health, demographics, and other topics; and (iii) regular refreshment samples to keep the sample representative of the older population. The details about each survey, their biennial interview, sample size, sample characteristics, and numbers of observations are summarized in Table 1.
Table 1.
Consecutive Biennial Interview Sample Characteristics for Studies Within the Family of Health and Retirement Study (HRS), Unweighted
| Survey | Country | Individuals | Women (%) | Birth Cohort (%)a | Number of Set of Consecutive Biennial Interviews Completed | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1920–1929 | 1930–1939 | 1940–1949 | 1950–1959 | 1960–1969 | Maximum | Mean | ||||
| HRS | United States | 28 641 | 57.4 | 16.4 | 25.8 | 24.0 | 29.4 | 4.4 | 8 | 4.8 |
| MHAS | Mexico | 19 044 | 57.2 | 9.9 | 20.4 | 33.3 | 26.0 | 10.5 | 2 | 1.4 |
| ELSA | England | 14 955 | 55.1 | 12.4 | 22.6 | 31.6 | 27.1 | 6.3 | 7 | 4.0 |
| SHARE | Austria | 4958 | 57.6 | 8.0 | 20.5 | 34.9 | 30.0 | 6.6 | 4 | 2.2 |
| Belgium | 7155 | 55.0 | 9.0 | 18.2 | 27.4 | 33.0 | 12.4 | 4 | 2.2 | |
| Croatia | 2009 | 56.4 | 1.9 | 11.7 | 28.9 | 40.1 | 17.4 | 1 | 1.0 | |
| Czechia | 5483 | 59.0 | 4.1 | 18.7 | 38.3 | 33.1 | 5.9 | 3 | 2.3 | |
| Denmark | 4378 | 54.4 | 6.5 | 15.5 | 29.4 | 33.0 | 15.6 | 4 | 2.2 | |
| Estonia | 6506 | 59.9 | 5.9 | 23.5 | 29.4 | 29.9 | 11.3 | 3 | 2.3 | |
| France | 5636 | 57.0 | 10.7 | 20.3 | 28.0 | 32.5 | 8.5 | 4 | 2.2 | |
| Germany | 5423 | 53.1 | 6.2 | 19.4 | 30.8 | 30.8 | 12.9 | 4 | 2.0 | |
| Greece | 3989 | 57.8 | 8.8 | 22.1 | 29.7 | 31.1 | 8.3 | 2 | 1.3 | |
| Israel | 2632 | 56.9 | 9.0 | 24.2 | 32.0 | 30.4 | 4.5 | 3 | 1.9 | |
| Italy | 5634 | 55.0 | 6.4 | 20.8 | 33.4 | 28.8 | 10.7 | 4 | 2.2 | |
| Luxembourg | 1398 | 54.2 | 2.8 | 12.2 | 29.1 | 42.0 | 13.9 | 2 | 1.6 | |
| Netherlands | 3074 | 55.4 | 8.9 | 21.7 | 37.3 | 29.4 | 2.7 | 2 | 1.3 | |
| Poland | 1466 | 57.6 | 3.6 | 14.7 | 30.6 | 39.5 | 11.6 | 1 | 1.0 | |
| Slovenia | 4170 | 57.4 | 5.0 | 18.8 | 30.3 | 36.5 | 9.4 | 3 | 1.9 | |
| Spain | 6441 | 55.1 | 11.0 | 23.5 | 29.2 | 29.8 | 6.6 | 4 | 2.2 | |
| Sweden | 4808 | 53.4 | 9.4 | 22.9 | 39.5 | 24.1 | 4.1 | 4 | 2.1 | |
| Switzerland | 3422 | 54.8 | 7.0 | 20.1 | 32.6 | 34.0 | 6.3 | 4 | 2.5 | |
| KLOSA | Korea | 9768 | 56.3 | 8.1 | 22.6 | 26.4 | 28.9 | 14.1 | 5 | 3.9 |
| CHARLS | China | 17 883 | 52.4 | 1.8 | 9.7 | 22.8 | 35.9 | 29.8 | 2 | 1.8 |
Notes: CHARLS = the China Health and Retirement Longitudinal Study; ELSA = the English Longitudinal Study of Ageing; KLoSA = the Korean Longitudinal Study of Aging; MHAS = the Mexican Health and Aging Study; SHARE = the Survey of Health, Ageing and Retirement in Europe.
aRespondents born prior to 1920 or after 1969 are not included in the denominator of the birth cohort %.
There are some notable exceptions to the interview frequency, respondent age, and spouse inclusion for these studies. While the majority of studies conduct interviews biennially, MHAS respondents experienced a 9-year survey interval between 2003 and 2012 and SHARE respondents experienced a 4-year survey interval between 2007 and 2011. While HRS, MHAS, ELSA, and SHARE interview respondents age 50 and older, KLoSA and CHARLS interview respondents age 45 and older. The exception to the inclusion of spouses regardless of age is KLoSA, which interviews only age-eligible spouses. It is also important to note that the number of countries included in SHARE varies across survey waves (subject to funding of individual countries). We included all SHARE countries that conducted at least one set of 2 consecutive biennial interviews in our analysis. As a result, from SHARE we included Austria, Belgium, Croatia, Czechia, Denmark, Estonia, France, Germany, Greece, Israel, Italy, Luxembourg, Netherlands, Poland, Slovenia, Spain, Sweden, and Switzerland.
Despite the high degree of coordination, there are numerous small differences between the studies ranging from question text and response categories to blocks of questions about country-specific health care systems or pension systems. The Gateway to Global Aging Data has developed harmonized versions of these data sources, which use consistent variable names and definitions, in user-friendly longitudinal files. These are the files we use in this study. The analysis data are from the RAND HRS Longitudinal File 2016 Version 1 (27) and Harmonized HRS Version B (United States) (28), Harmonized MHAS Version B beta (Mexico) (29), Harmonized ELSA Version F (England) (28), Harmonized SHARE Version E (Continental Europe and Israel) (30), Harmonized KLoSA Version C (South Korea) (31), and Harmonized CHARLS Version C (China) (32).
We use data from the waves conducted in the 2000–2016 period. All surveys ask respondents whether they have difficulty with (or that they cannot or do not do) any of the following basic ADLs: bathing, dressing, feeding, toileting, and getting in or out of bed. Disability is a binary variable, indicating any difficulty in at least one of these 5 ADLs. ADLs are specific and concrete, and therefore, prior studies found less subject to cultural differences (33,34). We define having a disability at the individual level as reporting a difficulty with any of these ADLs in the current wave. The disability prevalence rate is the fraction of individuals in the population having a disability. More information about how this ADL summary operates in this sample of countries can be found in Lee and colleagues (35). Correspondingly, we define developing a disability, or disability onset, at the individual level as reporting a difficulty with any of these ADLs in the current wave while reporting not having a difficulty with any of these ADLs in the previous wave, and not developing a disability as reporting no difficulties in both waves. If the respondent already reported an ADL difficulty in the previous wave, or was not interviewed in the previous wave, developing a disability is missing. The disability incidence rate is the fraction of individuals who developed a disability between the previous and current wave, relative to the population of individuals who are present in both waves and did not have a disability in the previous wave.
We also use survey data on the following individual characteristics: age, gender, educational attainment, and lifetime working status. Both age and gender are based on self-reports. Educational attainment is categorized into 3 levels, less than upper secondary education, upper secondary and vocational training, and tertiary education, based on the 1997 International Standard Classification of Education (ISCED) codes (36). Individual lifetime working status is derived using survey questions which ask respondents whether they have ever worked, though there is study variation as to whether this work was for pay and the duration of work which counts as ever having worked.
As an indicator of gender inequality, we use the United Nations Development Programme (UNDP)’s Gender Inequality Index (GII) (37). In 2010, UNDP introduced the GII and calculated it for 137 countries (38). GII is a composite measure that quantifies the inequalities women face in reproductive health, empowerment, and the labor market (39). The GII ranges from 0 to 1; higher GII values indicate greater gender inequality. Appendix Table 1 shows the country-level GII together with each component for the countries we have micro data on. The ranges of GII for the countries we study in this are .05 in Sweden to .40 in Mexico.
We account for 2 macroeconomic characteristics of countries, the level of economic development and public health insurance coverage, in our analysis of health effects of gender inequality. For the level of economic development, we use the log of purchasing power parity (PPP) adjusted Gross National Income (GNI) per capita, as provided by the World Bank (40). PPP is the rate of currency conversion that equalizes the purchasing power of different currencies, by eliminating the differences in price levels between countries, that is, the currency conversion rate such that a certain basket of goods and services would cost the same in different countries. For public health insurance coverage, we use public health care coverage from the Organization for Economic Cooperation and Development (OECD) (41), which refers to the share of the population that is eligible for health care goods and services under public programs.
Statistical Analysis
All analyses were done using Stata version 15 (42). Unless otherwise stated, all our analyses use the sampling weights provided by the surveys to ensure representativeness for the sampled population in each wave in each country. We first estimated disability prevalence and incidence rates for each country by gender. Specifically, the year we focus on is 2014, the year with the largest sample size, and the incidence rate is the fraction developing a disability, as defined above, that is, among those who did not have any disabilities in the previous wave. We estimated 2-year incidence rates.
Second, we estimated the probability of disability onset at each age by pooling data from multiple waves. The years we focus on are 2000–2016. Because of smaller sample sizes in the SHARE countries, we pooled data from multiple waves and combined the European countries in 4 groups for most of these analyses: Northern (Denmark, Sweden), Central (Austria, Belgium, France, Germany, Luxembourg, Netherlands, Switzerland), Southern (Croatia, Greece, Italy, Spain), and Eastern (Czechia, Estonia, Poland, Slovenia). We scaled the weights such that they added up to the sample size by country-wave before we pooled the data. Thus, the total weight of each country-wave is equal to its sample size, as it would be if all countries had drawn a simple random sample of the same size. (One could consider other scaling factors. For example, macroeconomic studies typically perform unweighted analyses with the country-wave as the unit of observation, which would suggest scaling such that the weights in each country-wave sum to the same total. At the other end of the spectrum would be the option to scale the weights such that they add up to population size of the country in the year of interview, which would be consistent with a view of the joint data set as a stratified sample from the population of individuals in the sampled countries and years. However, this is not a particularly meaningful population and it would essentially reduce the analysis to an analysis of a handful of very large countries [China, United States] and make the contributions of the small countries negligible. Both of these extremes remove the relation between sample size and influence on the estimates, which we find undesirable. An analogous discussion of what the proper weights are in the context of cross-state comparisons, which includes some further theoretical considerations, is given by Angrist and Pischke (43), pp. 202–203.) Standard errors accounted for clustering at the individual level when data from multiple waves were combined.
We then examined gender differences in the age gradients of disability onset, as the risk for developing a disability when one gets older might vary by gender. Specifically, we estimated the probability of developing a disability for both men and women separately for 5-year age groups. We computed the gender differences by subtracting men’s from women’s probability of developing a disability, so that a zero value would indicate there is no gender difference and positive values indicate women have higher probability of developing a disability than men. We also tested for gender differences within each country group using a standard Wald test for the joint significance of the coefficients of the female dummy and its interaction with age.
Finally, we conducted a cross-country analysis of the probability of developing a disability, investigating the association between gender inequality and the probability of developing a disability by pooling data from all 23 countries. As discussed in the beginning of this article, when describing our conceptual model, we hypothesized that gender inequality is positively associated with the probability of developing disability for both men and women after controlling for other risk factors for disability. We estimated the probability of developing a disability using a logistic regression model with 5-year age group dummies and (10-year) birth cohort dummies, using 4 different specifications. In the first model, we estimated the effect of being female. This is essentially a description of the data adjusted for age and birth cohort, providing a baseline difference that we try to explain. In the second model, we added the GII value and the interaction between GII value and being female. This provides suggestive evidence whether gender inequality may matter for explaining the gender difference in disability onset, but it leaves open the possibility that this gender difference may be explained by other factors that are correlated with gender inequality. In the third model, we added controls for GNI and public health insurance coverage. This explores whether the relation found in the second model could be attributed to these other country characteristics. The fourth model implements the complete conceptual model as presented in Figure 1. It adds individual-level educational attainment and a dummy for ever having worked as controls. This is important, because the GII contains population-level gender differences in educational attainment and labor force participation, which are correlated with these individual-level measures, so it could be that in Model 3, the GII coefficient would pick up the effects of individual-level education and work history instead of gender inequality as intended. By controlling for these individual-level measures, this potential source of confounding is eliminated.
Results
Cross-country Variation in Disability Prevalence and Incidence Rates
We first examine cross-country variation in disability prevalence rates and incidence rates. Table 2 shows disability prevalence rates and incidence rates for men and women ages 65–69 in 23 countries; disability prevalence rates and incidence rates for all other age groups can be found in Appendix Table 2. Across all age groups, cross-country variation in disability prevalence rates and incidence rates is smaller for men than for women.
Table 2.
Disability Prevalence and Incidence Rate (%) by Country; Selected Age Groups; 2000–2016
| Ages 65–69 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Gender Difference | |||||||||||
| Disability Prevalence | Disability Incidence | Disability Prevalence | Disability Incidence | Prevalence | Incidence | ||||||||
| Country | n | Estimate | SE | Estimate | SE | n | Estimate | SE | Estimate | SE | |||
| United States | 11 224 | 10.5 | 0.5 | 5.4 | 0.3 | 14 569 | 13.7 | 0.4 | 6.9 | 0.3 | −3.2 | −1.5 | |
| Mexico | 4265 | 9.9 | 1.0 | 7.0 | 1.0 | 4730 | 15.0 | 1.1 | 11.4 | 1.5 | −5.0 | −4.4 | |
| England | 5586 | 17.0 | 0.7 | 7.5 | 0.5 | 6578 | 16.9 | 0.6 | 8.2 | 0.5 | 0.1 | −0.7 | |
| Austria | 1409 | 7.2 | 0.9 | 3.2 | 0.7 | 1815 | 6.1 | 0.8 | 3.6 | 0.7 | 1.1 | −0.4 | |
| Belgium | 1991 | 10.5 | 0.8 | 5.3 | 0.7 | 2165 | 10.8 | 0.8 | 5.9 | 0.7 | −0.3 | −0.7 | |
| Croatia | 449 | 7.3 | 1.5 | 5.1 | 1.6 | 425 | 10.2 | 1.8 | 8.1 | 2.4 | −2.8 | −3.0 | |
| Czechia | 1882 | 9.1 | 0.9 | 6.7 | 1.0 | 2616 | 8.8 | 0.8 | 6.2 | 0.8 | 0.3 | 0.6 | |
| Denmark | 1342 | 8.1 | 0.9 | 5.8 | 0.9 | 1414 | 5.7 | 0.8 | 3.9 | 0.7 | 2.4 | 1.9 | |
| Estonia | 1473 | 12.8 | 1.1 | 8.1 | 1.0 | 2014 | 11.8 | 0.9 | 6.7 | 0.8 | 1.0 | 1.4 | |
| France | 1522 | 7.2 | 0.8 | 4.0 | 0.7 | 1871 | 7.8 | 0.7 | 4.9 | 0.7 | −0.6 | −0.9 | |
| Germany | 1793 | 8.7 | 0.9 | 5.6 | 0.9 | 1743 | 8.7 | 0.9 | 5.0 | 0.8 | 0.0 | 0.6 | |
| Greece | 1074 | 4.1 | 0.7 | 0.8 | 0.4 | 1148 | 4.8 | 0.8 | 1.8 | 0.7 | −0.6 | −1.1 | |
| Israel | 888 | 7.2 | 1.2 | 1.7 | 0.7 | 1063 | 7.8 | 1.0 | 3.0 | 0.7 | −0.6 | −1.2 | |
| Italy | 1957 | 5.6 | 0.6 | 3.8 | 0.6 | 2196 | 8.2 | 0.7 | 5.0 | 0.7 | −2.6 | −1.3 | |
| Luxembourg | 381 | 5.7 | 1.6 | 1.7 | 0.9 | 358 | 10.1 | 2.0 | 7.0 | 2.3 | −4.5 | −5.3 | |
| Netherlands | 997 | 4.6 | 0.7 | 3.0 | 1.0 | 1016 | 5.7 | 0.9 | 5.2 | 1.3 | −1.0 | −2.2 | |
| Poland | 848 | 13.2 | 1.4 | 5.7 | 2.2 | 958 | 16.1 | 1.5 | 8.9 | 2.5 | −3.0 | −3.2 | |
| Slovenia | 1026 | 8.4 | 1.0 | 4.9 | 1.0 | 1171 | 6.3 | 0.9 | 4.7 | 0.9 | 2.0 | 0.2 | |
| Spain | 1825 | 7.0 | 0.9 | 3.3 | 0.7 | 1998 | 8.0 | 0.9 | 5.7 | 0.9 | −1.0 | −2.4 | |
| Sweden | 1785 | 6.3 | 0.7 | 3.7 | 0.6 | 2049 | 7.1 | 0.7 | 4.2 | 0.7 | −0.8 | −0.6 | |
| Switzerland | 1165 | 4.7 | 0.8 | 3.2 | 0.7 | 1269 | 5.2 | 0.8 | 2.9 | 0.6 | −0.5 | 0.3 | |
| Korea | 3282 | 3.0 | 0.4 | 1.9 | 0.3 | 3988 | 2.0 | 0.3 | 1.0 | 0.2 | 1.0 | 0.9 | |
| China | 3255 | 16.3 | 0.9 | 9.9 | 0.8 | 3185 | 24.1 | 1.1 | 18.7 | 1.2 | −7.8 | −8.8 | |
| Mean | 8.5 | 4.7 | 9.6 | 6.0 | −1.1 | −1.4 | |||||||
| Range | 14.1 | 9.1 | 22.1 | 17.8 | 10.2 | 10.7 | |||||||
Note: N is the total number of respondents used to calculate prevalence, and incidence is calculated among people without an existing disability. Disability incidence is the rate of people without a disability at the previous interview (2 years ago) of developing a disability. All estimates are produced using sampling weights and displayed in percent. Range is difference between highest and lowest in the column. Gender difference is calculated as men’s estimate minus women’s estimate.
For example, among ages 65–69, the disability prevalence rate for men ranges from 3.0% in Korea to 17.0% in England, while it ranges from 2.0% in Korea to 24.1% in China for women. Similarly, the disability incidence rate for men ranges from 0.8% in Greece to 9.9% in China, while it ranges from 1.0% in Korea to 18.7% in China for women. There is notable cross-country variation in the gender difference in both the disability prevalence rates and the incidence rates. Chinese women at ages 65–69 had about 8–9 percentage points higher disability prevalence rates and incidence rates than Chinese men, whereas Danish women at the same age had about 2 percentage points lower disability prevalence rates and incidence rates than Danish men.
At older ages, the cross-country variation in the gender differences in disability prevalence and incidence rates becomes larger. For example, among ages 80–84, women in countries like Belgium, Croatia, Spain, and China had over 10 percentage points higher disability prevalence rates than men. However, women in Denmark, Luxembourg, and Sweden had about 2–3 percentage points lower in disability prevalence rate. In terms of disability incidence rate, women in Croatia, Italy, and China had over 10 percentage points higher than men in those countries, but women in Luxembourg and Sweden had 6–8 percentage lower disability incidence rates than men.
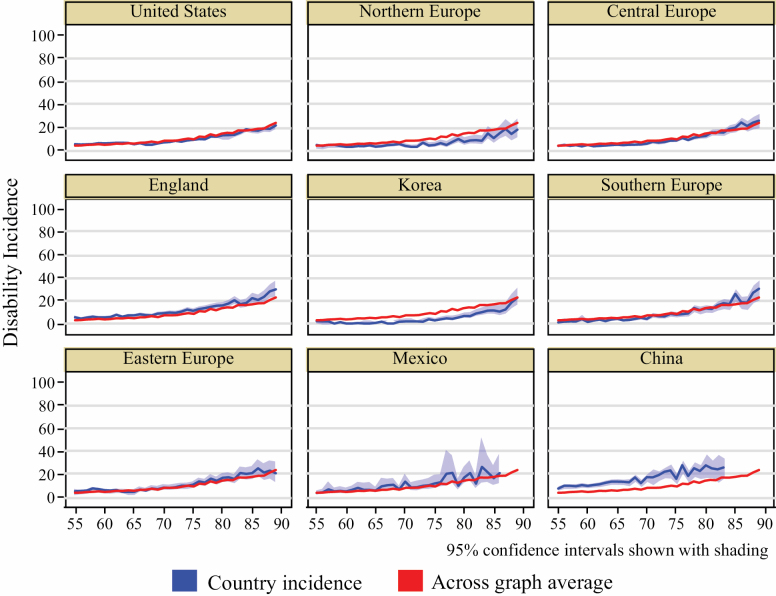
Age Gradients of Disability Incidence by Country (Group): Within-Country Analysis
We now investigate cross-country variation in age gradients of disability incidence by pooling all available data from 2000 to 2016. As noted earlier, we combined the European countries in 4 groups due to the smaller sample sizes in SHARE countries. Figure 2 shows the age gradients of disability incidence in the United States, England, Korea, Mexico, China, and the 4 groups of European countries. Compared to the all country average, China has much higher levels of disability incidence rates across the age span we studied, whereas the disability incidence rates in Korea are lower across the age span. For Northern Europe, the disability incidence rates are noticeably lower after age 70 compared to the all country average. The 95% confidence intervals for Mexico are relatively large due to smaller number of consecutive waves that allow to measure 2-year disability incidence.
Figure 2.
Age gradients of disability incidence in ages 55–89 by country (group) for people born 1920–1969; 2000–2016.
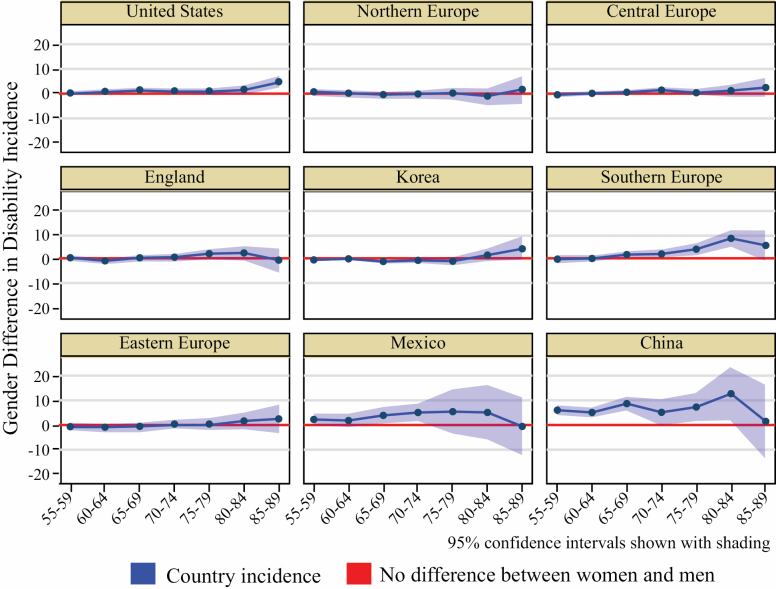
We further examined gender differences in age-specific disability incidence. We find no statistically significant gender difference in the age gradients of disability incidence in Northern, Central, and Eastern Europe, England, and Israel, whereas we find statistically significant gender differences in the age gradients of disability incidence in the United States, Korea, Southern Europe, Mexico, and China (Appendix Table 3 presents the test statistics for these differences).
Among the countries where significant gender differences exist, we observe further variation in the age of onset. As shown in Figure 3, gender differences in disability incidence occur at different ages. For example, in the United States and Southern Europe, we find gender differences at relatively older ages, while gender differences in disability incidence are observed at younger ages in developing countries like China and Mexico.
Figure 3.
Gender difference in age-specific disability incidence in ages 55–89 by country (group) for people born 1920–1969; 2000–2016.
Effects of Gender Inequality: Cross-country Analysis
The results of the logistic regressions are presented in Table 3. In addition to the common controls (age dummies and birth cohort dummies), Model 1 only includes a gender dummy (reference: men). This shows a highly significant gender discrepancy in disability onset, with women more likely to develop a disability than men (conditional on age and birth cohort). Model 2 adds the GII and its interaction with the gender dummy. Compared to Model 1, the main effect of gender disappears and instead, both GII and its interaction with gender are statistically significant. The former implies that in countries with very little gender inequality, women and men are about equally likely to develop a disability. The main effect of GII reflects the effect of gender inequality at the country level on men’s likelihood of developing a disability. It shows that men in countries with higher gender inequality are more likely to develop a disability than men in more equal countries. The interaction of GII with the gender dummy indicates to what extent this effect is stronger for women than for men. It is indeed substantially stronger for women, so women in unequal countries are more likely to develop a disability than men in unequal countries, and than women in more equal countries.
Table 3.
Cross-country Multivariate Analysis of the Relationship Between Gender Inequality and Disability Incidence in Ages 55–89 for People Born 1920–1969; 2000–2016
| Covariates | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Women | 0.164 *** | 0.029 | 0.021 | −0.048 |
| (0.019) | (0.045) | (0.044) | (0.045) | |
| GII (2010) | 1.656 *** | −0.049 | −0.390 | |
| (0.179) | (0.239) | (0.237) | ||
| Women × GII | 0.702 ** | 0.756 ** | 0.897 *** | |
| (0.233) | (0.231) | (0.230) | ||
| 2010 Log PPP-adjusted GNI per capita | −0.600 *** | −0.465 *** | ||
| (0.030) | (0.031) | |||
| 2010 public health care coverage | −0.450 *** | −0.649 *** | ||
| (0.0601 | (0.061) | |||
| Education Level 2 (upper secondary and vocational training) | −0.317 *** | |||
| (0.023) | ||||
| Education Level 3 (tertiary education) | −0.742 *** | |||
| (0.031) | ||||
| Ever worked | −0.027 | |||
| (0.040) | ||||
| Constant | −2.911 | −3.547 | 3.468 | −0.009 |
| (0.053) | (0.072) | (0.386) | (0.043) | |
| N | 320 745 | 320 745 | 317 440 | 317 440 |
Notes: GII = Gender Inequality Index; GNI = Gross National Income; PPP = purchasing power parity. 1. Controls for 5-year age groups and 10-year birth cohorts are included in all models and regressions are weighted. 2. Public health care coverage is not available for Croatia or Luxemburg so these countries are dropped from Model 3 and 4. SEs in parentheses.
**p < .01, ***p < .001.
As discussed above, GII tends to be correlated with economic development, and thus we want to assess whether the effects found in Model 2 are due to gender inequality or whether they can be attributed to economic development in different countries. Model 3 addresses this issue by adding per capita income in the country as a measure of economic development. Moreover, another potential confounder related to gender inequality and economic development is the amount of coverage of the public or social health system, which is also likely to affect disability onset. Therefore, we have also added the population share that is covered by public or social health insurance as a control variable. The table shows that economic development and health insurance coverage are indeed highly significantly related to disability onset, in the hypothesized directions. The main effect of GII drops considerably and is not statistically significant anymore, confirming the importance of distinguishing between gender inequality and economic development. Interestingly, however, the same does not hold for the interaction between GII and the gender dummy. The coefficient even slightly increases in magnitude. Hence, we do not have evidence that gender inequality hurts men, but strong evidence that it is associated with higher rates of disability development among women.
As discussed above, country-level education levels and labor force participation, which are important components of the GII, are correlated with individual-level education and labor force history, so one may be worried that the GII coefficient reflects the effects of the individual-level characteristics instead of the effect of gender inequality. To address this, Model 4 adds individual-level education (2 dummies for a 3-category education variable) and lifetime work status (a dummy for having ever worked) to the equation. This shows that higher individual-level education is indeed strongly significantly associated with lower probability of disability onset. The coefficient of the lifetime work dummy is small and not significant. Most importantly for the purpose of this paper, the coefficient of the interaction between GII and the gender dummy further increases a bit in magnitude compared to Model 3 and remains highly statistically significant. This result indicates that the results from Models 2 and 3 were not due to a spurious effect of individual education and lifetime work status.
To illustrate the implications of the model, we performed the following experiment. For each observation in the sample, we computed the predicted probability of a disability onset. Then we computed the averages of these by country. These are the predicted average incidence rates by country for the period studied (2000–2016) for individuals age 55–89. Next, we replaced the country’s GII value by Sweden’s GII value, the lowest in our data set-leaving all other variables untouched, and recomputed the resulting model-predicted disability onset probabilities and incidence rates. The comparison between the 2 predicted incidence rates gives an impression of the extent to which GII is estimated to contribute to a country’s disability incidence rate. It should be noted, however, that this is imperfect and should be viewed as only a rough indication of the importance of gender inequality. For example, if the GII value is lowered by increasing access of women to the labor market, this will also affect income, which we keep at its original value in this experiment. The results of this exercise are presented in Table 4. As expected based on the results in Table 3, the effects on men’s incidence rates are small in all countries, and they are all zero or positive, that is, incidence rates for men would be slightly higher with less gender inequality (Mexico is an outlier where men would be more noticeably worse off). For women, the results are stronger and in the opposite direction. In each country, the predicted baseline incidence rate for women is higher than for men, and the reductions of women’s predicted incidence rates are universally larger than the increases in the men’s incidence rates. In all countries, this reduces gender inequality in incidence rates. Naturally, the magnitudes of these effects depend on the level of the baseline GII, with no effect for Sweden, Denmark, and the Netherlands, which had the lowest baseline GIIs, and the largest effects for Mexico, China, and the United States, which had the highest baseline GIIs. For most countries, the effects are modest, reflecting relatively low GII to begin with, but the reductions in gender inequality in disability incidence are meaningful for countries with high GII values.
Table 4.
Predicted Disability Incidence Rate (%) Under Current and Improved GII by Country; ages 55–89; 2000–2016
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Country | Mean Under Current GII | Mean If Swedish GII | Difference | Mean Under Current GII | Mean If Swedish GII | Difference |
| United States | 6.4 | 6.9 | 0.5 | 8.1 | 7.4 | −0.7 |
| Mexico | 9.3 | 10.5 | 1.2 | 12.1 | 10.4 | −1.7 |
| England | 5.6 | 5.8 | 0.3 | 7.0 | 6.6 | −0.4 |
| Austria | 4.6 | 4.7 | 0.1 | 5.9 | 5.7 | −0.2 |
| Belgium | 5.4 | 5.5 | 0.1 | 6.2 | 6.0 | −0.1 |
| Czechia | 6.3 | 6.5 | 0.2 | 7.7 | 7.4 | −0.3 |
| Denmark | 4.5 | 4.5 | 0.0 | 5.3 | 5.3 | 0.0 |
| Estonia | 6.9 | 7.2 | 0.3 | 8.6 | 8.1 | −0.4 |
| France | 5.7 | 5.9 | 0.1 | 7.0 | 6.9 | −0.2 |
| Germany | 4.9 | 5.0 | 0.1 | 6.2 | 6.1 | −0.1 |
| Greece | 7.0 | 7.3 | 0.3 | 8.4 | 8.0 | −0.4 |
| Israel | 6.0 | 6.2 | 0.2 | 6.1 | 5.8 | −0.3 |
| Italy | 7.1 | 7.3 | 0.2 | 8.0 | 7.7 | −0.3 |
| Netherlands | 5.5 | 5.5 | 0.0 | 6.6 | 6.6 | 0.0 |
| Poland | 7.2 | 7.5 | 0.3 | 9.2 | 8.7 | −0.5 |
| Slovenia | 5.8 | 6.0 | 0.2 | 7.7 | 7.4 | −0.3 |
| Spain | 7.2 | 7.4 | 0.2 | 8.2 | 8.0 | −0.2 |
| Sweden | 5.4 | 5.4 | 0.0 | 5.9 | 5.9 | 0.0 |
| Switzerland | 4.3 | 4.4 | 0.0 | 5.3 | 5.2 | 0.0 |
| Korea | 5.9 | 6.0 | 0.1 | 7.7 | 7.5 | −0.2 |
| China | 11.0 | 11.5 | 0.5 | 12.5 | 11.8 | −0.7 |
| Mean | 6.3 | 6.5 | 0.2 | 7.6 | 7.3 | −0.3 |
| Range | 6.6 | 7.1 | 1.2 | 7.3 | 6.6 | 1.7 |
Note: GII = Gender Inequality Index. Incidence is predicted based on Model 4 regression results. Range is difference between highest and lowest in the column. Croatia and Luxembourg are not included in Model 4, so not shown in this table.
Discussion
In this study, we used harmonized data from the Gateway to Global Aging Data to analyze disability prevalence and incidence from 23 countries across different levels of economic development and gender inequality. We found substantial cross-country variation in disability prevalence and incidence rates, and much larger cross-country variation in age-specific disability prevalence and incidence rates for women than for men. Our within-country analysis showed significant gender differences in age gradients of disability incidence in the United States, Korea, Southern Europe, Mexico, and China, but not in Northern, Central, and Eastern Europe, England, and Israel. Furthermore, our cross-country analysis indicated that the gender difference in disability onset was significantly associated with gender inequality, independent of stage of economic development across these countries or individual socioeconomic characteristics.
The gender gap in disability has been reported in many developed countries. For example, Serrano-Alarcón and Perelman (44) found that women 65–79 years old in Spain, Portugal, and Italy were 3.3% more likely than men to have severe function limitations; increasing the age bracket to those age 80 or older increased this likelihood to 15.5%. A recent study spanning 16 European countries found that gender disparities in activity limitations that disfavored women were larger in southern Europe and generally increased with age; however, these trends were not universally present in every country studied (45). Moreover, a systemic review of 21 longitudinal studies conducted mostly in high-income countries failed to show a consistent gender difference in the incidence of functional disability (18). Our study adds to the literature by demonstrating cross-country variation in gender difference of disability incidence. Significant gender difference was present in the United States, Korea, Southern Europe, Mexico, and China, but not in many other European countries.
Previous research has attempted to explore the potential underlying reasons for gender differences in health. Studies focusing more on biological mechanisms have indicated that gender differences in body composition and comorbid medical conditions, such as cardiovascular diseases, arthritis, osteoporosis, and cognitive decline, may contribute but do not fully explain this gender gap (46). Others noted how gender inequalities in power, access to social and economic resources, and unequal division of domestic responsibilities may have led to worse health among women (1,2). Pooling harmonized longitudinal data from the 23 countries at different stages of economic development, we demonstrated evidence that the societal level of gender inequality matters for women’s (but not men’s) risk of developing disability. The association between gender inequality and women’s disability onset remained significant after controlling for macrosocial variables of economic development and public health care coverage, and individual-level educational attainment and work history. This result extends findings from the United States by Homan (3) and Mechakra-Tahiri and colleagues (25), who reported a larger gender gap in disability prevalence in regions with more gender inequality. It also supports the structural sexism literature (3,4), which shows that gender inequalities in health outcomes may be explained by inequalities between men and women in not only important socioeconomic determinants of health at the individual level but also macrosocial determinants of health, such as political power, the welfare state, social protection policies, and economic and labor market policies.
The wide cross-country variation in age-specific disability incidence rates and the significant association between gender inequality and increased women’s risk of developing a disability call for attention from both academics and policy makers. Limited studies have shown that government political representation, employment, and family policies that intended to explicitly support women and families were associated with diminished gender inequalities and improved health outcomes for women (47). It has been suggested that Nordic social democratic welfare regimes and dual-earner family models could promote women’s health, which is consistent with our finding of no significant gender difference in disability incidence among older Europeans, except those in southern Europe.
This study has many strengths: It is based on rich and longitudinal data, which has allowed us to examine disability incidence, independent of the survivor effect. The data used are from nationally representative samples and several have sample sizes large enough for adequate statistical power in their country. Another strength is that the data used have been collected with the aim of comparability across countries, and we have used harmonized measures of disability, making the data directly comparable. Some limitations should also be noted. We have focused on basic ADLs as the measure of disability. However, disability is complex. We may not be able to extrapolate our findings to other domains of disability, such as instrumental ADLs or mobility impairments. We have relatively small sample sizes for some European countries, and therefore, we have grouped countries into geographic regions for the analysis of the incidence data. There may be important differences in population characteristics and government policies across these countries that are averaged out with this grouping. The measure used for work history is limited, only capturing whether the individual ever worked for pay, and therefore its insignificant association with disability onset may be due to measurement error when thought of as a measure of work history.
Despite these limitations, our study is one of the first that provides empirical evidence on disability incidence among older adults in both developed and developing countries around the world. Using internationally comparable longitudinal data from 23 countries across different levels of economic development, we have examined the gender gap in disability onset and its association with gender inequality across countries. Future studies are needed to identify what further contributes to such cross-country differences beyond economic development, public health insurance, and individual socioeconomic status.
Supplementary Material
Acknowledgment
Earlier results were presented at the Plenary Session on Healthy Ageing and Health Equity at the 2018 International Federation of Ageing Annual Conference and at the 2018 English Longitudinal Study of Ageing Wave 8 Launch Meeting.
Funding
This work was supported by the National Institute on Aging (R01 AG030153) and the World Health Organization (WHO) Ageing and Health Unit, Department of Maternal, Newborn, Child, Adolescent Health and Ageing.
Conflict of Interest
None declared.
Author Contributions
J.L., E.M., and P.H. conceptualized the paper together. D.P. conducted data analysis under the supervision of J.L. and E.M. J.L. drafted the first version of the manuscript. All authors contributed to the writing of the manuscript.
References
- 1. Heise L, Greene ME, Opper N, et al. ; Gender Equality, Norms, and Health Steering Committee Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;393:2440–2454. doi: 10.1016/S0140-6736(19)30652-X [DOI] [PubMed] [Google Scholar]
- 2. Read JG, Bridget KG. Gender and health inequality. Ann Rev Soc. 2010;36:371–386. doi: 10.1146/annurev.soc.012809.102535 [DOI] [Google Scholar]
- 3. Homan P. Structural sexism and health in the United States: a new perspective on health inequality and the gender system. Am Soc Rev. 2019;84:486–516. doi: 10.1177/0003122419848723 [DOI] [Google Scholar]
- 4. Krieger N. Measures of racism, sexism, heterosexism, and gender binarism for health equity research: from structural injustice to embodied harm—an ecosocial analysis. Annu Rev Public Health. 2020;41:37–62. doi: 10.1146/annurev-publhealth-040119-094017 [DOI] [PubMed] [Google Scholar]
- 5. United Nations. The Millennium Development Goals Report. 2015. https://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf. Accessed March 17, 2020.
- 6. Clark J, Horton R. A coming of age for gender in global health. Lancet. 2019;393:2367–2369. doi: 10.1016/S0140-6736(19)30986-9 [DOI] [PubMed] [Google Scholar]
- 7. Weber AM, Cislaghi B, Meausoone V, et al. ; Gender Equality, Norms and Health Steering Committee Gender norms and health: insights from global survey data. Lancet. 2019;393:2455–2468. doi: 10.1016/S0140-6736(19)30765-2 [DOI] [PubMed] [Google Scholar]
- 8. Heymann J, Levy JK, Bose B, et al. ; Gender Equality, Norms and Health Steering Committee Improving health with programmatic, legal, and policy approaches to reduce gender inequality and change restrictive gender norms. Lancet. 2019;393:2522–2534. doi: 10.1016/S0140-6736(19)30656-7 [DOI] [PubMed] [Google Scholar]
- 9. Sen A. Mortality as an indicator of economic success and failure. Econ J. 1998;108:1–25. doi: 10.1111/1468-0297.00270 [DOI] [Google Scholar]
- 10. Jayachandran S. The roots of gender inequality in developing countries. Ann Rev Econ. 2015;7:63–88. doi: 10.1146/annurev-economics-080614-115404 [DOI] [Google Scholar]
- 11. Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102:936–944. doi: 10.2105/AJPH.2011.300544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Palència L, Malmusi D, De Moortel D, et al. The influence of gender equality policies on gender inequalities in health in Europe. Soc Sci Med. 2014;117:25–33. doi: 10.1016/j.socscimed.2014.07.018 [DOI] [PubMed] [Google Scholar]
- 13. Connell R. Gender, health and theory: conceptualizing the issue, in local and world perspective. Soc Sci Med. 2012;74:1675–1683. doi: 10.1016/j.socscimed.2011.06.006 [DOI] [PubMed] [Google Scholar]
- 14. Collins R. A conflict theory of sexual stratification. Soc Prob. 1971;19:3–21. doi: 10.2307/799936 [DOI] [Google Scholar]
- 15. Kavanagh SA, Graham M. How gender inequity impacts on men’s health: an exploration of theoretical pathways. Int J Men Soc Commun Health. 2019;2:d11–121. doi: 10.22374/ijmsch.v2i1.5 [DOI] [Google Scholar]
- 16. Hubbard RE, Rockwood K. Frailty in older women. Maturitas. 2011;69:203–207. doi: 10.1016/j.maturitas.2011.04.006 [DOI] [PubMed] [Google Scholar]
- 17. Jacob ME, Marron MM, Boudreau RM, Odden MC, Arnold AM, Newman AB. Age, race, and gender factors in incident disability. J Gerontol A Biol Sci Med Sci. 2018;73:194–197. doi: 10.1093/gerona/glx194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rodrigues MA, Facchini LA, Thumé E, Maia F. Gender and incidence of functional disability in the elderly: a systematic review. Cad Saude Publica. 2009;25:S464–S476. doi: 10.1590/s0102-311x2009001500011 [DOI] [PubMed] [Google Scholar]
- 19. Auais M, Ahmed T, Alvarado B, et al. Gender differences in four-year incidence of self-reported and performance-based functional disability: The International Mobility in Aging Study. Arch Gerontol Geriatr. 2019;82:266–272. doi: 10.1016/j.archger.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 20. van der Vorst A, Zijilstra GAR, Witte ND, et al. Limitations in activities of daily living in community-dwelling people aged 75 and over: a systematic literature review of risk and protective factors. PLoS ONE 2016;11:e0165127. doi: 10.1371/journal.pone.0165127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gu D, Yi Z. Sociodemographic effects on the onset and recovery of ADL disability among Chinese oldest-old. Demograph Res. 2004;11:1–42. doi: 10.4054/DemRes.2004.11.1 [DOI] [Google Scholar]
- 22. Lange S, Vollmer S. The effect of economic development on population health: a review of the empirical evidence. Br Med Bull. 2017;121:47–60. doi: 10.1093/bmb/ldw052 [DOI] [PubMed] [Google Scholar]
- 23. Institute of Medicine (US). Committee on the Consequences of Uninsurance. Washington DC: National Academies Press; 2002. [Google Scholar]
- 24. Duflo E. Women’s empowerment and economic development. J Econ Lit. 2012;50:1051–1079. doi: 10.3386/w17702 [DOI] [Google Scholar]
- 25. Mechakra-Tahiri SD, Freeman EE, Haddad S, Samson E, Zunzunegui MV. The gender gap in mobility: a global cross-sectional study. BMC Public Health. 2012;12:598. doi: 10.1186/1471-2458-12-598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kawachi I, Kennedy BP, Gupta V, Prothrow-Stith D. Women’s status and the health of women and men: a view from the States. Soc Sci Med. 1999;48:21–32. doi: 10.1016/s0277-9536(98)00286-x [DOI] [PubMed] [Google Scholar]
- 27. Bugliari D, Campbell N, Chan C, et al. RAND HRS Longitudinal File 2016 (V1) Documentation: includes 1992–2016 (early release). Santa Monica, CA: RAND Center for the Study of Aging; 2019. [Google Scholar]
- 28. Beaumaster S, Chien S, Crosswell A, et al. Harmonized ELSA Documentation, Version F (2002–2016). Los Angeles, CA: Center for Economic and Social Research, University of Southern California; 2018. [Google Scholar]
- 29. Michaels-Obregon A, Lin A, Phillips D, Wilkens J, Wong R, Lee J. Harmonized MHAS Documentation, Version A. Los Angeles, CA: Center for Economic and Social Research, University of Southern California; 2017. [Google Scholar]
- 30. Chien S, Phillips D, Valev M, Wilkens J, Lee J. Harmonized SHARE Documentation, Version E (2004–2018). Los Angeles, CA: Center for Economic and Social Research, University of Southern California; 2019. [Google Scholar]
- 31. Chien S, Phillips D, Valev M, Wilkens J, Yonter V, Lee J. Harmonized KLoSA Documentation, Version C (2006–2016). Los Angeles, CA: Center for Economic and Social Research, University of Southern California; 2019. [Google Scholar]
- 32. Beaumaster S, Chien S, Lau S, et al. Harmonized CHARLS Documentation, Version C. Los Angeles, CA: Center for Economic and Social Research, University of Southern California; 2018. [Google Scholar]
- 33. Avlund K, Luck M, Tinsley R. Cultural differences in functional ability among elderly people in Birmingham, England, and Glostrup, Denmark. J Cross Cult Gerontol. 1996;11:1–16. doi: 10.1007/BF00116262 [DOI] [PubMed] [Google Scholar]
- 34. Kim S, Won CW. How can we evaluate disability without bias? Ann Geriatr Med Res. 2020;24:152–153. doi: 10.4235/agmr.20.0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lee J, Lau S, Meijer E, Hu P. Living longer, with or without disability? A global and longitudinal perspective. J Gerontol A Biol Sci Med Sci. 2019;75:162–167. doi: 10.1093/Gerona/glz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Organization for Economic Cooperation and Development (OECD). Classifying Educational Programmes: Manual for ISCED-97 Implementation in OECD Countries. 1999. http://www.oecd.org/education/skills-beyond-school/1962350.pdf. Accessed March 20, 2020.
- 37. United Nations Development Programme. Human Development Data [data set]. 2019. http://hdr.undp.org/en/data. Accessed March 23, 2020.
- 38. Klugman J. Human Development Report 2010.United Nations Development Programme.2010. http://hdr.undp.org/sites/default/files/reports/270/hdr_2010_en_complete_reprint.pdf. Accessed August 18, 2019. [Google Scholar]
- 39. Klasen S. Human Development Indices and Indicators: A Critical Evaluation.2018. UNDP Human Development Report Office.http://hdr.undp.org/sites/default/files/klasen_final.pdf. Accessed December 8, 2019. [Google Scholar]
- 40. World Bank. DataBank: World Development Indicators. 2020. http://databank.worldbank.org/data/reports.aspx?source=2&series=NY.GDP.PCAP.PP.CD. Accessed January 17, 2020.
- 41. Organization for Economic Cooperation and Development (OECD). OECD Health Statistics 2019: Definitions, Sources and Methods. 2019. http://www.oecd.org/health/health-data.htm. Accessed March 23, 2020.
- 42. Stata Corp. Stata: Release 15. Statistical Software. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 43. Angrist JD, Pischke JS. Mastering Metrics. Princeton University Press; 2015:202–203. [Google Scholar]
- 44. Serrano-Alarcón M, Perelman J. Ageing under unequal circumstances: a cross-sectional analysis of the gender and socioeconomic patterning of functional limitations among the Southern European elderly. Int J Equity Health. 2017;16:175. doi: 10.1186/s12939-017-0673-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schmitz A, Lazarevič P. The gender health gap in Europe’s ageing societies: universal findings across countries and age groups? Eur J Ageing. 2020. doi: 10.1007/s10433-020-00559-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23:343–350. doi: 10.1093/oxfordjournals.epirev.a000810 [DOI] [PubMed] [Google Scholar]
- 47. Borrell C, Palència L, Muntaner C, Urquía M, Malmusi D, O’Campo P. Influence of macrosocial policies on women’s health and gender inequalities in health. Epidemiol Rev. 2014;36:31–48. doi: 10.1093/epirev/mxt002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.