Abstract
Importance
COVID‐19 has been associated with excess mortality among patients not diagnosed with COVID‐19, suggesting disruption of acute health care provision may play a role.
Objective
To determine the degree of declines in emergency department (ED) visits attributable to COVID‐19 and determine whether these declines were concentrated among patients with fewer comorbidities and lower severity visits.
Design
We conducted a differences‐in‐differences analysis of all commercial health insurance claims for ED visits in the first 20 weeks of 2018, 2019, and 2020. The intervention period began March 9 (week 11) of 2020, following state stay‐at‐home orders.
Setting
We analyzed claims from Blue Cross Blue Shield of Louisiana (BCBSLA), located in a state with an early US COVID‐19 outbreak. Visit and patient risk was assessed through comorbidities previously described as increasing the risk of COVID‐19 decompensation, the hospital location's COVID‐19 outbreak status, and the Ambulatory Care Sensitive Condition algorithm.
Participants
The study population comprised all ED visits from all BCBSLA members, whether admitted or discharged. There were 332,917 ED visits over the study period. The study population spanned member demographics including sex, age, and geography. Uninsured adults were not included due to data limitations.
Exposure(s)
The COVID‐19 outbreak beginning March 9, 2020 in Louisiana.
Main outcome(s) and measure(s)
The main outcome of interest for this analysis is the difference (percent change) in all ED visits, categorized as either respiratory or non‐respiratory, from week 1–20 in 2019 and week 1–10 in 2020, compared to week 11–20 in 2020.
Results
In this differences‐in‐differences study using data from a commercial health insurer, we found that non‐respiratory ED visits declined by 39%, whereas respiratory visits did not experience a significant decline. Visits that were potentially deferrable or from lower risk patient populations showed greater declines, but even high‐risk patients and non‐avoidable visits experienced large declines in non‐respiratory ED visits. Non‐respiratory ED visits declined by only 18% in areas experiencing COVID outbreak.
Conclusions and relevance
COVID‐19 has resulted in significant avoidance of ED care, comprising a mix of deferrable and high severity care. Hospital and public health pronouncements should emphasize appropriate care seeking.
1. INTRODUCTION
1.1. Background
The COVID‐19 coronavirus pandemic is ongoing. As the number of COVID‐19 cases and hospitalizations began to increase in March 2020, news media, politicians, and health officials initially cautioned the public to avoid hospitals for "unnecessary" care. Public health warnings and stay‐at‐home orders, despite explicitly allowing medical visits, may have contributed to fears that emergency departments (EDs) in hospitals are places of particularly high risk for contracting the virus. 1 These concerns, along with a reduced presence of risk factors for injury such as automotive travel, likely contributed to an overall ED visit decline of 42% during the early COVID‐19 pandemic, from a mean of 2.1 million per week (March 31–April 27, 2019) to 1.2 million (March 29–April 25, 2020). 2
1.2. Importance
Existing data on this early overall decline leave significant gaps in our understanding of how the pandemic affected ED visits and the broader implications of these declines for patients and health systems. ED visits span a broad range of severities, from low acuity to imminently lethal. 3 , 4 There may be significant health consequences to avoiding emergency care for severe conditions, contributing to the estimated 87,000 excess non‐COVID deaths thus far. 5 For example, these deaths may be caused by failure to receive important care such as emergent cardiac catheterizations for ST‐segment–elevation myocardial infarctions (STEMI). 6 Whether catheterization laboratory activations declined because of more stringent activation criteria (reducing semielective activations), or because fewer patients presented to EDs for their chest pain remains unknown. Alternatively, telemedicine use increased, 7 and given that 14% to 27% of ED visits are diagnosed with a condition treatable at an alternative care site, these missed ED visits may have saved health system costs 8 while having minimal consequences for health. Elective procedures also declined, 5 meaning fewer ED visits for complications. 9 Furthermore, existing data are not divided by acuity or granular disease categories. Because COVID‐19 induces a variety of chief complaints, most notably respiratory complaints, the aggregation in previous studies may have masked an even more substantial decline in non‐respiratory disease.
Moreover, the initial decline may have been temporary. After an initial message to stay away from hospitals, calls to not avoid emergency care have become prominent, 10 once the probability of overwhelming hospital capacity decreased, raising the possibility that visits have since increased. Finally, the data on overall declines do not reveal whether patients are responsive to local capacity constraints compared to more diffuse fears.
1.3. Goals of this investigation
To provide insight into these mechanisms, we use insurance data from one of the first states to see a major outbreak, Louisiana, where patient morbidity is high 11 and which surpassed 1000 cases of COVID‐19 by March 20, 2020. 12 These cases were not distributed evenly throughout the state; rather, denser areas were first affected, and New Orleans saw cases and hospitalizations increase before Baton Rouge. 13 A statewide stay‐at‐home order was put in place on March 22. We use this differential timing to analyze how the COVID‐19 pandemic has affected the magnitude and composition of ED visits for non‐COVID related (non‐respiratory) diseases when compared to the same weeks in the previous years.
2. METHODS
2.1. Study design
To understand the impact of COVID‐19 on ED care seeking, we used claims data from the largest health care insurer in Louisiana, Blue Cross Blue Shield of Louisiana (BCBSLA). The insurer provided anonymized ED claims data for BCBSLA enrollees age 18‐years or older from week 1 (January) through week 20 (May) of 2018, 2019, and 2020. All ED visits seen by a clinician and submitted for claims were considered–both outpatient and those that led to an inpatient admission.
We identified ED visits using primary diagnosis code (International Classification of Diseases, Tenth Revision [ICD‐10]), place of service, and procedure codes. First, we identified facility claims using Milliman category methodology, which identifies claims with a claim category of "FOP Emergency Room–Hospital–ED Ambulatory Care" or "FOP Observation–ED Observation." Then we group professional claims and facility claims into visits. We take the earliest date of service as the date of the ED visit.
2.2. Analysis
The main outcome of interest for this analysis is the difference (percent change) in all ED visits, categorized as either respiratory or non‐respiratory, from week 1–20 in 2019 compared to week 1–20 in 2020. As a falsification test, week 1–20 of 2019 is compared to week 1–20 for 2018. Among non‐respiratory ED visits, the following subcategories were analyzed separately: cardiac, diabetes, ear conditions, gastrointestinal, headache, mental health, orthopedic, and urinary system.
Primary variables included in this analysis were as follows: (1) patient demographics ‐ age (18‐44, 45–64, 65–79, 80+) and sex (male, female); (2) whether a member had any 1 of the following comorbid conditions that were considered to be “high risk” for COVID, (3) whether the members hospital was located in a COVID area, and (4) whether the members ED visit was avoidable or not as determined by Billings’ Ambulatory Care Sensitive Conditions algorithm. 14 To apply the algorithm, we translated ICD‐9 to ICD‐10 codes using a crosswalk combined with guidance from the insurer's medical director. An ED visit was considered avoidable if it had at least 1 primary diagnosis code from facility and professional claims matching the list. When defining conditions considered high risk for COVID we drew from available preprint data at the time of study initiation 15 and mapped those onto risk factors available in our claims data. Members were considered high risk for COVID if they had a previous diagnosis of chronic obstructive pulmonary disease; asthma; diabetes; end‐stage renal disease; congestive heart failure; primary diagnosis of acute myocardial infarction within the most recent 6 months; any diagnosis of coronary artery disease and had bypass, stent, or catheterization procedure within the most recent 6 months; liver disease, or body mass index ≥ 40.
The Bottom Line
An analysis of more than 300,000 ED visits among commercially insured patients in the southern United States showed that non‐respiratory ED visits declined by 39%, whereas respiratory visits did not experience a significant decline during the initial weeks of the COVID‐19 pandemic. These results suggest that COVID‐19 resulted in significant avoidance of ED care, comprising a mix of deferrable and high severity care
The main methodology for this research was the differences‐in‐differences (DID) technique, frequently used in economics and health services research, to measure the change induced by a particular treatment or event, in this case, the COVID‐19 pandemic. The basic premise of this DID analysis was to examine the effect of COVID‐19 by comparing separate categories of ED visits (non‐respiratory, respiratory, cardiac, diabetes, ear conditions, gastrointestinal, headache, mental health, orthopedic, and urinary system) during the same calendar weeks in 2019 and 2020 as well as before and after week 10 in 2020 (January 1, 2020–March 7, 2020 vs March 8, 2020–May 16, 2020), when hospitals began taking measures to provide remote care because of the COVID‐19 pandemic.
Our multiple regression analysis includes controls for member demographics and characteristics. The structure of our count data lends itself to a high number of zero counts, mostly in smaller visit categories. These are due to the way we partitioned our counts into relatively restrictive bins and not because we have separate data generating processes for zeros and for positive counts. Therefore, we have not used zero inflated models or hurdle models, as the zeros are likely to come from the same data generating process as the positive values. The models were estimated using a negative binomial distribution as follows:
where the number of visits for sex, COVID‐19 risk and age group i, year and week t, condition c, avoidable/non‐avoidable visit v, and hospital being in COVID‐19 affected area h, are regressed against these categories as well as a DID variable that received a value of 1 after week 10 of 2020 when stay‐at‐home measures were put in place. All models were generated using Stata Version 15.
3. RESULTS
Table 1 reports member characteristics for ED visits for the prepandemic weeks (1‐10) of 2020 and then for weeks 11–20 (after initiation of stay‐at‐home orders). Distributions are similar for age, sex, and comorbidities with over 40% of adults being 18–44, more females than males (58% vs 42%) and over a third (37%) having 1 or more of the “high‐risk” COVID comorbid conditions. There was a significant difference when it comes to avoidable versus non‐avoidable ED visits with 32% of non‐respiratory visits being avoidable versus 67% for respiratory.
TABLE 1.
Member characteristics
| Weeks 1‐10, 2020 | Weeks 11‐20, 2020 | Change | ||
|---|---|---|---|---|
| N (%) | N (%) | N (%) | P* | |
| Total Patients | 49,305 | 33,895 | −15,410 (−31.3%) | |
| Total Visits | 58,398 | 40,040 | −18,358 (−31.4%) | |
| Age | ||||
| 18–44 | 25,065 (42.9%) | 17,023 (42.5%) | −8042 (−32.1%) | 0.21 |
| 45–64 | 20,321 (34.8%) | 15,119 (37.8%) | −5202 (−25.6%) | <0.01 |
| 65–79 | 8305 (14.2%) | 5179 (12.9%) | −3126 (−37.6%) | <0.01 |
| 80+ | 4707 (8.1%) | 2719 (6.8%) | −1988 (−42.2%) | <0.01 |
| Sex | ||||
| Female | 34,100 (58.4%) | 22,204 (55.5%) | −11,896 (−34.9%) | <0.01 |
| Male | 24,298 (41.6%) | 17,836 (44.5%) | −6462 (−26.6%) | <0.01 |
| High‐Risk COVID(1) | ||||
| Yes | 23,875 (40.9%) | 16,444 (41.1%) | −7431 (−31.1%) | 0.56 |
| No | 34,523 (59.1%) | 23,596 (58.9%) | −10,927 (−26.6%) | 0.56 |
| Facility in COVID Region(2) | ||||
| Yes | 28,226 (48.3%) | 20,699 (51.7%) | −7527 (−26.7%) | <0.01 |
| No | 30,172 (51.7%) | 19,341 (48.3%) | −10,831 (−35.9%) | <0.01 |
| ED Avoidable(3) | ||||
| Yes | 21,471 (36.8%) | 13,139 (32.8%) | −8332 (−38.8%) | <0.01 |
| No | 36,927 (63.2%) | 26,901 (67.2%) | −10,026 (−27.2%) | <0.01 |
(1) High Risk COVID defined as whether or not member had 1 of the following comorbid conditions: chronic obstructive pulmonary disease; asthma; diabetes; end‐stage renal disease; congestive heart failure; primary diagnosis of acute myocardial infarction within most recent 6 months; any diagnosis of coronary artery disease and had bypass, stent, or catheterization procedure within the most recent 6 months; liver disease, or body mass index ≥ 40.
(2) Facility in COVID Region defined as whether the members hospital was located in a COVID area.
(3)ED visit was avoidable–if it had at least 1 primary diagnosis code from facility and professional claims matching the Billings’ Ambulatory Care Sensitive Conditions algorithm (ref 11).
Figure 1 displays the percentage change in non‐respiratory ED visits across the entire state by week for weeks 1–20 for 2020 versus 2019 and 2019 versus 2018. Percentage changes were consistent for both years until week 10 (the week of the statewide stay‐at‐home order) when a decline of 40% occurred within 3 weeks in 2020 but not in 2019. Although not displayed, similar declines were seen by age and sex with the sharpest decline in adults age 65+ (over 50%) and females (over 40%).
FIGURE 1.
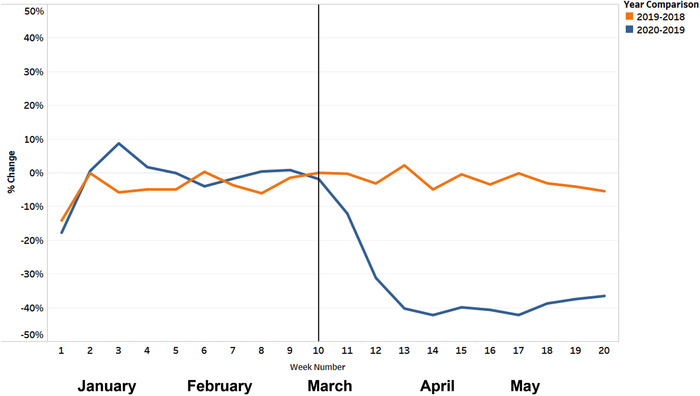
Percentage change in ED visits by week 1–20 for 2020 versus 2019 and 2019 versus 2018 for adults with non‐respiratory diseases
Visits that were potentially deferrable or from lower risk patient populations showed greater declines across the entire state (Figure 2). Members possessing a “high‐risk” COVID risk factor reduced their non‐respiratory visits less than those at lower risk during weeks 12–17. These differences resolved by week 18. ED visits resulting in diagnoses classified as avoidable showed significantly greater declines than “not avoidable” visits, but “not avoidable” non‐respiratory visits still declined by ≈35%. Hospitals not in COVID areas experienced significantly greater declines both before and after week 10.
FIGURE 2.
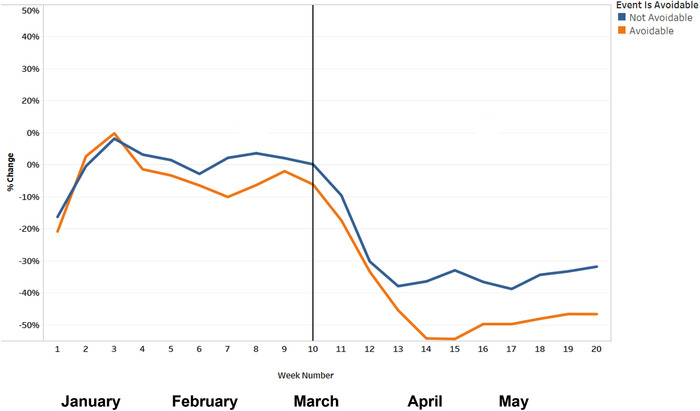
Percentage Change in ED Visits by Week 1–20 for 2020 versus 2019 for adults with non‐respiratory diseases by whether the event is avoidable or not avoidable
Figures 3 and S1 display the percentage change in ED visits by week 1–20 for 2020 versus 2019 for adults with the following selected conditions across the entire state: respiratory, cardiac, diabetes, ear conditions, gastrointestinal, headache, mental health, orthopedic, and urinary system. For respiratory conditions there was a spike of over 150% during weeks 13 and 14. Non‐respiratory conditions with the largest dips after week‐10 include orthopedics, ear conditions and headaches.
FIGURE 3.
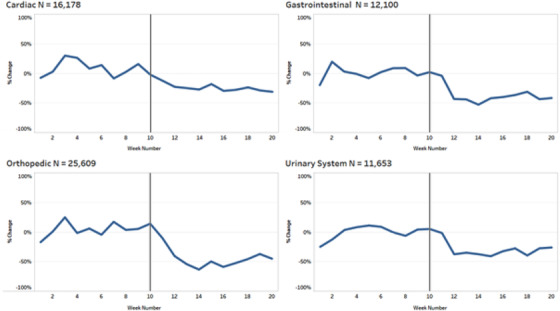
Percentage change in ED visits by week 1–20 for 2020 versus 2019 for adults with 4 most prevalent non‐respiratory conditions
3.1. Model results
The results of the adjusted DID regression models for non‐respiratory, respiratory, cardiac, diabetes, ear conditions, gastrointestinal, headache, mental health, orthopedic, and urinary system visits are shown in Table 2. The table reports the incident rate ratios. All DID model coefficients for non‐respiratory ED visits are statistically significant and negative (incident rate ratios below 1) indicating even after model adjustments for differences in member characteristics, there were significant declines in ED visits from week 10–20 in the year 2020 with the largest magnitude in decline coming from orthopedic, urinary system, and gastrointestinal visits.
TABLE 2.
Incidence rate ratios from Negative Binomial Count Models (DID) for all non‐respiratory ED visits and the 9 selected conditions in Figure 3 and S1
| All Non‐Respiratory | Respiratory | Cardiac | Diabetes | Ear condition | Gastrointestinal | Headache | Mental health | Orthopedic | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Differences‐in‐differences | 0.621** | 0.896 | 0.700** | 0.665* | 0.529** | 0.687** | 0.551** | 0.646** | 0.507** | 0.735** |
| (0.025) | (0.066) | (0.092) | (0.114) | (0.065) | (0.064) | (0.080) | (0.099) | (0.055) | (0.073) | |
| Female | 1.482** | 1.321** | 1.005 | 0.995 | 1.367** | 1.340** | 2.717** | 1.231** | 1.425** | 1.676** |
| (0.029) | (0.047) | (0.064) | (0.083) | (0.081) | (0.061) | (0.192) | (0.091) | (0.075) | (0.085) | |
| Age 45–64 | 0.819** | 0.800** | 1.477** | 1.537** | 1.165* | 1.031 | 0.657** | 0.539** | 1.068 | 0.93 |
| (0.022) | (0.037) | (0.120) | (0.165) | (0.086) | (0.061) | (0.054) | (0.052) | (0.074) | (0.060) | |
| Age 65–79 | 0.306** | 0.313** | 0.772** | 0.730** | 0.503** | 0.456** | 0.147** | 0.178** | 0.357** | 0.489** |
| (0.009) | (0.016) | (0.072) | (0.084) | (0.042) | (0.030) | (0.015) | (0.019) | (0.027) | (0.035) | |
| Age 80 and over | 0.173** | 0.197** | 0.537** | 0.240** | 0.236** | 0.303** | 0.0627** | 0.131** | 0.218** | 0.422** |
| (0.005) | (0.011) | (0.058) | (0.033) | (0.024) | (0.022) | (0.008) | (0.015) | (0.018) | (0.032) | |
| Avoidable | 0.213** | 1.225** | 0.0170** | 4.055** | 0.701** | 0.253** | 1.647** | 0.000582** | 0.120** | 0.403** |
| (0.004) | (0.047) | (0.001) | (0.403) | (0.043) | (0.012) | (0.123) | (0.000) | (0.007) | (0.021) | |
| COVID Risk | 1.013 | 0.985 | 1.679** | 566.1** | 0.616** | 0.725** | 0.525** | 0.633** | 0.667** | 0.836** |
| (0.021) | (0.038) | (0.118) | (285.300) | (0.037) | (0.035) | (0.038) | (0.050) | (0.037) | (0.043) | |
| COVID Area | 0.815** | 0.860** | 0.811** | 0.911 | 0.932 | 0.801** | 1.049 | 0.847* | 0.851** | 0.818** |
| (0.016) | (0.031) | (0.053) | (0.076) | (0.055) | (0.036) | (0.073) | (0.064) | (0.045) | (0.040) | |
| 2019 | 12,1397 | 14,909 | 9004 | 1279 | 2588 | 6043 | 3383 | 3694 | 16,695 | 6834 |
| 2020 | 97326 | 17472 | 8193 | 1110 | 1974 | 5103 | 2467 | 3343 | 13163 | 5761 |
| Both Years Combined | 21,8723 | 32,381 | 17,197 | 2389 | 4562 | 11,146 | 5850 | 7037 | 29,858 | 12,595 |
P < 0.01, *P < 0.05, Standard errors in parentheses; controlling for year and week of the year fixed‐effects.
When looking at all non‐respiratory visits combined in the DID regression, we see visits during COVID‐19 became 39% less likely. Compared to the 18–44 age group, people aged 45 to 64 were 22.1% less likely to visit the ED, people aged 65 to 79 were 69.4% times less likely to visit the ED, and people 80 and over were 82.7% times less likely to visit the ED. Females were 48.2% more likely to visit the ED than males after adjustment for all other model covariates. In the same model, people residing in an area with high prevalence of COVID‐19 were 22.7% less likely to visit the ED. The magnitude was greater for those visits that contained a potentially avoidable diagnosis with a decline of 78.7%, controlling for all other model covariates. Individuals with comorbid conditions associated with higher risk if contracting COVID‐19 were equally likely to visit the ED.
4. LIMITATIONS
These analyses have a few limitations. First, this is a retrospective database analysis and therefore we cannot account for potential differences that are unobservable. Second is the generalizability of the findings. Although we included members employed in a variety of industries and regions, Louisiana is our sample, so our results reflect only one state and patients without insurance are not considered. As a result, our analysis likely underestimates effects owing to job loss given previous evidence that health insurance increases ED visits. 16
5. DISCUSSION
Using a large database of insurance claims in a state with an early COVID‐19 outbreak, we use differential intrastate timing to demonstrate the magnitude and composition of non‐respiratory ED visits during the COVID‐19 pandemic. Most notably, we demonstrate that visits that were potentially deferrable or from lower risk patient populations showed greater declines, but even high‐risk patients and non‐avoidable visits experienced large declines in non‐respiratory ED visits. Non‐respiratory visits overall declined by almost 40%, with certain more deferrable categories such as orthopedic visits declining by up to 60%.
These unprecedented declines in ED visits likely affected patient health, hospital capacity, and health system finances. The decline in visits has caused substantial financial losses for health systems and particularly their EDs 17 , 18 limiting resources for preparedness for this pandemic and future pandemics. 19 Unlike during outbreaks of influenza, 20 this decline in visits created excess capacity and in so doing may have helped reduce COVID‐19 mortality. Although the initial advisory to avoid hospitals may have been appropriate, given evidence that delays in emergency care can increase mortality, 21 in future pandemics, public health experts should monitor aggressively for a transition point when a call for a return to acute medical care should be issued.
From the perspective of the individuals’ health who stayed at home, the implications of these patients staying at home are unclear. Previous research has identified that 13% to 27% of ED visits share ICD codes with urgent care clinics, indicating they could potentially be seen in a lower‐cost setting. 8 Other research examines similar lists and finds that a small percentage of these visits potentially would experience delayed or worsened care for serious illnesses. 22 , 23 The substantial increase in telemedicine during COVID‐19 may have increased the accuracy of patient self‐triage for those patients who consulted their physician. The accuracy of patients choosing an appropriate site of care is likely not homogeneous and may vary by age, health literacy, messaging received from their community and leadership, reported risk factors for COVID‐19 (eg, hypertension, which was initially reported to be a significant risk), societal disadvantage, 24 and individual heterogeneity. Other patients, such as those staying home with diabetes‐related visits, may be instead being more closely managed by their regular physican or nurse practitioner in order to avoid ED visits, providing a promising model for more coordinated care post‐pandemic. Once outcome data are available for analysis, future research can use the experience we document to design a layered triage system that can keep patients safe while lowering costs through reduced ED use for low acuity visits.
There are numerous potential pathways by which the decline in ED visits we observe could occur, with differential impacts on public health. 25 The incidence or severity of disease could decrease, promoting health, as with fewer pedestrians hit by cars causing a decline in orthopedic visits, or fewer surgical procedures leading to fewer complications. Patients could change their care‐seeking behavior, either staying home or seeking care from their usual primary care physician or nurse practitioner rather than ED services. Similarly, outpatient surveillance and diagnostic intensity may have changed, as outpatient physicians and nurse practitioners seek to keep patients out of the ED.
6. CONCLUSION
ED visits declined precipitously in the first months of the COVID‐19 pandemic in the United States. ED visits for care potentially amenable to other care settings experienced greater declines than non‐avoidable visits. However, even high‐risk ED visits and visits from high‐risk patients declined substantially. This may have contributed to the increase in non‐coronavirus‐related deaths in the United States during this period. 26 Health systems should continue efforts to make patients feel safe during this pandemic so that patients seek evaluation and care in all appropriate settings. 27
AUTHOR CONTRIBUTIONS
ABF, DB, GD, TD, CG, and SCN conceived of the presented idea. GD, CG, ML, BVV, RZ, and YZ conducted the statistical analyses. ABF, DB, GD, TD, CG, and SCN wrote the manuscript.
Supporting information
Supporting Information
Biography
Ari B. Friedman, MD, PhD, is an Assistant Professor of Emergency Medicine at the University of Pennsylvania, holds a secondary appointment in the Department of Medical Ethics and Health Policy, is Core Faculty at the Center for Emergency Care Policy and Research, and is a Senior Fellow of the Leonard Davis Institute of Health Economics.
Friedman AB, Barfield D, David G, et al. Delayed emergencies: The composition and magnitude of non‐respiratory emergency department visits during the COVID‐19 pandemic. JACEP Open. 2021;2:e12349 10.1002/emp2.12349
Supervising Editor: Chadd K. Kraus, DO, DrPH
Funding and support: Deidre Barfield, Thomas Diller, Miao Li, Benjamin V. Vicidomina, Ruthann Zhang, and Yuan Zhang are employed by Blue Cross and Blue Shield of Louisiana. Candace Gunnarson is employed by Gunnarsson Consulting. The authors have no further conflicts of interest to declare. This analysis was not grant supported.
REFERENCES
- 1. Society for Cardiovascular Angiography & Intervention. New Data Confirms Doctors' Fear: majority of Americans avoiding treatment for heart attack and stroke due to COVID‐19. GlobeNewsWire. 2020. https://www.globenewswire.com/news-release/2020/05/29/2040871/0/en/New-Data-Confirms-Doctors-Fear-Majority-of-Americans-Avoiding-Treatment-for-Heart-Attack-and-Stroke-Due-to-COVID-19.html [Google Scholar]
- 2. Hartnett KP, Kite‐Powell A, DeVies J, et al. Impact of the COVID‐19 pandemic on emergency department visits —United States, January 1, 2019–May 30, 2020. Morbidity Mortality Weekly Report. 2020; 69(23): 699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Koziol‐McLain J, Price DW, Weiss B, Quinn AA, Honigman B. Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J Emerg Nurs JEN Off Publ Emerg Dep Nurses Assoc. 2000; 26(6): 554‐563. [DOI] [PubMed] [Google Scholar]
- 4. Uscher‐Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013; 19(1): 47‐59. [PMC free article] [PubMed] [Google Scholar]
- 5. Bean M. COVID‐19 fears still keeping Americans away from hospitals, survey finds. Beckers Hosp Rev. 2020. https://www.beckershospitalreview.com/public-health/covid-19-fears-still-keeping-americans-away-from-hospitals-survey-finds.html. [Google Scholar]
- 6. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐Segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol. 2020; 75(22): 2871‐2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid‐19. N Engl J Med. 2020; 382(18): 1679‐1681. [DOI] [PubMed] [Google Scholar]
- 8. Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff. 2010; 29(9): 1630‐1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Evaniew N, Files C, Smith C, et al. The fragility of statistically significant findings from randomized trials in spine surgery: a systematic survey. Spine J. 2015; 15(10): 2188‐2197. [DOI] [PubMed] [Google Scholar]
- 10. Searing L. Five kinds of health appointments you should consider keeping, despite the pandemic [Internet]. Washington Post. https://www.washingtonpost.com/lifestyle/wellness/five-kinds-of-health-appointments-you-should-consider-keeping-despite-the-pandemic/2020/07/01/d04f5848-bbc4-11ea-80b9-40ece9a701dc_story.html. 2020. [cited Aug 24]. [Google Scholar]
- 11. US Burden of Disease Collaborators , Mokdad AH, Ballestros K, et al, US Burden of Disease Collaborators . The state of US health, 1990‐2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018; 319(14): 1444‐1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The COVID Tracking Project. Louisiana Overview [Internet]. Atlantic. 2020. [cited Aug 24]. https://covidtracking.com/data/state/louisiana#historical [Google Scholar]
- 13. Swenson D. Louisiana coronavirus cases and deaths: a daily snapshot graphic [Internet]. Nolacom. 2020. https://bloximages.newyork1.vip.townnews.com/nola.com/content/tncms/assets/v3/editorial/b/19/b19afd82-71ee-11ea-bc2f-a3b35078a17f/5f43f7474eeb5.pdf.pdf. [cited Aug 24]. Available from. [Google Scholar]
- 14. NYU Center for Health and Public Service Research. Ambulatory Care Sensitive Conditions. 2014. [cited 2020 Oct 29]. https://wagner.nyu.edu/faculty/billings/nyued-background [Google Scholar]
- 15. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID‐19‐related death using OpenSAFELY. Nature. 2020; 584(7821): 430‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Finkelstein AN, Taubman SL, Allen HL, Wright BJ, Baicker K. Effect of medicaid coverage on ED use — further evidence from Oregon's Experiment. New England J Med. 2016; 375(16): 1505‐1507. [DOI] [PubMed] [Google Scholar]
- 17. Mellnik T, Karklis L, Tran AB. Americans are delaying medical care, and it's devastating health‐care providers. Washington Post. 2020. https://www.washingtonpost.com/nation/2020/06/01/americans-are-delaying-medical-care-its-devastating-health-care-providers/. [Internet]. cited 2020 Jun 2]. [Google Scholar]
- 18. Khullar D, Bond AM, Schpero WL. COVID‐19 and the Financial Health of US Hospitals. JAMA. 2020. https://jamanetwork.com/journals/jama/fullarticle/2765698. [Internet]. cited 2020 May 11]. [DOI] [PubMed] [Google Scholar]
- 19. Terwiesch C, Mahoney K, Volpp K. Payment for staying empty? Reimbursing hospitals for Covid‐19 readiness. NEJM Catalyst. 2020; 10 https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0232. [Google Scholar]
- 20. Sivey P, McAllister R, Vally H, Burgess A, Kelly A‐M. Anatomy of a demand shock: quantitative analysis of crowding in hospital emergency departments in Victoria, Australia during the 2009 influenza pandemic. PLoS ONE. 2019; 14(9): e0222851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jena AB, Mann NC, Wedlund LN, Olenski A. Delays in emergency care and mortality during major U.S. Marathons. N Engl J Med. 2017; 376(15): 1441‐1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lowe RA, Bindman AB, Ulrich SK, et al. Refusing care to emergency department of patients: evaluation of published triage guidelines. Ann Emerg Med. 1994; 23(2): 286‐293. [DOI] [PubMed] [Google Scholar]
- 23. Raven MC, Lowe RA, Maselli J, Hsia RY. Comparison of presenting complaint vs discharge diagnosis for identifying “ nonemergency” emergency department visits. JAMA. 2013; 309(11): 1145‐1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Owen WF, Carmona R, Pomeroy C. Failing another National Stress Test on health disparities. JAMA. 2020; 323(19): 1905. [DOI] [PubMed] [Google Scholar]
- 25. Kocher KE, Macy ML. Emergency department patients in the early months of the Coronavirus disease 2019 (COVID‐19) pandemic—what have we learned? JAMA Health Forum. 2020; 1(6): e200705‐e200705. [DOI] [PubMed] [Google Scholar]
- 26. Lu D. There has been an increase in other causes of deaths, not just Coronavirus. N Y Times. 2020. https://www.nytimes.com/interactive/2020/06/01/us/coronavirus-deaths-new-york-new-jersey.html. Internet]. cited 2020 Jun 1]. [Google Scholar]
- 27. Asch DA. Opening Hospitals to More Patients During the COVID‐19 pandemic—making it safe and making it feel safe. JAMA Intern Med. 2020. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2766560. Internet]. cited 2020 May 27]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


