Abstract
One of the major concerns in the US healthcare system revolves around access to care, including specialty care. While many factors contribute to lack of access, the most common one is time (both for practices and patients). From a practice perspective, the inability to access a cardiologist for weeks if not months is usually due to an often overwhelmed clinic schedule. Leaving work, caring for a family member, transportation, parking, and other expenses are clear factors from the patient's perspective.
Now, the COVID-19 crisis has brought telemedicine to the forefront of care delivery, giving patients and physicians first-hand exposure to the technology. The broader access and simplification of technology interface has provided a nontraditional mode to care delivery in which online, “face-to-face” video, phone visits, or even two-way text communication is easily applied. Furthermore, simple everyday technology tools can provide easy and fast access to curbside consultations, quick urgent-care questions and management, up-titrating medications, and the more important but often under-delivered continuous counseling for preventive medicine. In this review, we provide an overview of telemedicine development and explain how telemedicine is the perfect vehicle to deliver many aspects of cardiovascular patient care.
Keywords: telemedicine, telehealth, remote monitoring, digital health
INTRODUCTION
The recent and ongoing COVID-19 pandemic has brought telemedicine to the front and center of medical care delivery, a development many advocates of telemedicine believe is long overdue. The urgent need to provide remote patient care precipitated a rapid introduction to telemedicine for clinicians around the world. This review provides a broad perspective of how cardiovascular care is primed for the implementation of telemedicine.
THE EVOLUTION OF TELEMEDICINE
Telemedicine is not a new concept: The vision of remote medical communication was conceptualized as early as the 1920s with the “radio doctor” via experimental television transmission.1 Since telemedicine mostly revolves around the transmission of images, it is unsurprising that teleradiology would pioneer this platform. As early as the late 1940s, there were successful attempts at transmitting radiographic images, albeit a mere 24 miles, and this spurred the development of teleradiology systems.2
In the early 1960s, anesthesiologists started working on remote patient monitoring3: a patient was described as a “radio,” and each monitoring point of data was a different radio “station” conveying different physiological information. Foreshadowing today's routine practice for communicating with emergency services, the University of Miami and the Miami Fire Department first reported the transmission of an electrocardiogram (EKG) from the field as early as 1966.4 The first transoceanic transmission of an EKG was a 1967 communication from Guinea to Miami.5
Over time, it became obvious that this platform would be useful in situations in which proper access, time and cost savings, and timely management are of high importance. For instance, prisons house a concentrated population of potential patients with chronic and acute disease processes in one large facility—a setting that could benefit from efficient telemedicine systems. Indeed, data from the University of Texas Medical Branch as early as 1995 demonstrated the potential impact of telemedicine on saving resources in prisons.6 Telemedicine offers remote physiological data review and decreases the need for referrals, thus reducing resource burdens in transportation, security personnel, and specific accommodations in different facilities where patients would otherwise seek care.
Over the years, the federal government noted the advantages in efficiency offered by this mode of medical communication and management. For example, the US Department of Veterans Affairs (VA), despite its size and widespread locations, identified that a significant percentage of patients had difficulty accessing the system due to factors such as distance, socioeconomic, and wait times. In 2003, it became one of the early adopters of telehealth. An evaluation of 5,698 telemedicine visits occurring from its inception through 2015 found that telemedicine resulted in significant travel and time savings while also saving the government thousands of dollars in travel reimbursement.7
Clearly, advances in both broadband and smartphone/tablet capabilities over the past decade have make widespread telehealth even more feasible.8 With the onset of COVID-19, the partially opened door for telemedicine has been kicked wide open.
NEW OPPORTUNITIES WITH TELEMEDICINE
Historically, the physician–patient visit has revolved around face-to-face interaction: the welcoming handshake, listening to a patient's complaints (and stories), the examination of a patient's heart and lungs, visualizing lower extremity edema or discoloration, one-onone discussion, and so on. Medicine isn't the only industry undergoing a shift to remote customer interactions. Banking, for example, has always relied heavily on face-to-face interaction. However, interpersonal financial transactions are now increasingly digital, almost eliminating the need to meet with a banker, write checks, and physically deposit money. The COVID-19 pandemic accelerated this change, decreasing coins in circulation and leading even more people to rely on digital processes for financial interactions.
Thus, changes in the banking industry parallel changes in telemedicine as more and more people adopted a new banking “norm” before and during the pandemic. Although managing one's health is different from banking, the concept is not. Fast, efficient, and personalized management of patients with chronic disease does not necessarily require them to leave work, deal with traffic, or sit in a waiting room during specific hours on any given weekday.
Opportunities for Health Care
In a world where many industries are dramatically changing their delivery services, the medical community has not significantly changed its practices. Major technology companies have taken notice of this opportunity and have geared up to provide digital and remote services through new and established technology platforms. The top ten tech companies spent more than $4.7 billion on healthcare-related acquisitions from 2012 to 2018.9 Telemedicine is at the heart of many of these advances, with goals of obtaining data and communicating with patients via text, phone, or video.
Although many people think of telemedicine in terms of live, office-visit-type communication between patient and clinician, other aspects of telemedicine may prove to be of even more significant value in the future of health care. Remote monitoring is on the top of that list. Remote monitoring is readily available, reasonably simple, and relatively inexpensive, and when used with the best practices, it can be a valuable tool to help manage risk factors for cardiovascular diseases (Figure 1). More importantly, it has the potential to improve patient engagement. When patients are engaged in the biweekly or monthly report of their blood pressure monitoring, heart failure data, exercise or activity progress, or any other of the many reporting options, engagement tends to improve. Patient engagement can be a significants factor in both outcomes and healthcare costs.10
Figure 1.
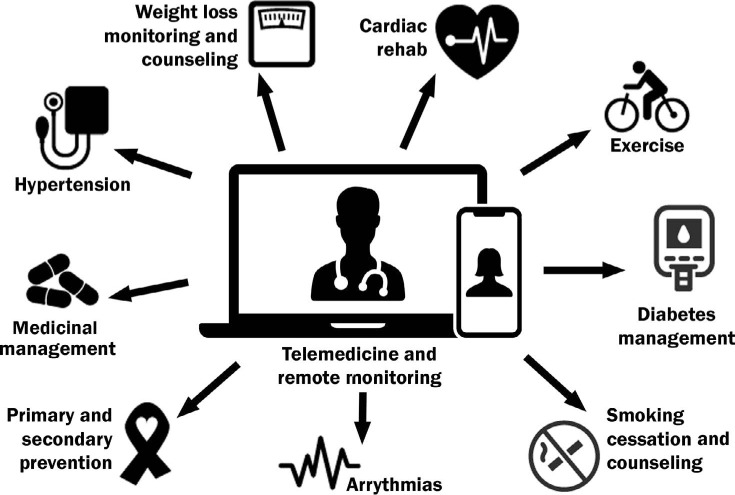
Clinical scenarios for telemedicine and remote monitoring.
There are many examples of the potential of remote monitoring with telemedicine for primary and secondary prevention,11 including cardiac rehabilitation,12, 13 obesity,14 hypertension,15, 16 and almost any major cardiovascular risk factor in need of modification.
Opportunities for Patients and Clinicians
It is no secret that the US healthcare system is riddled with inefficiencies, frustration among all parties, and excessive costs. There is a concern not just about access to care but also access to quality care. This is even more true for at-risk demographic groups that are most vulnerable to CVD and health problems overall due to a multitude of systemic inequalities.17,18 More recently, the COVID-19 pandemic and subsequent interruptions to non-COVID-related care has shone a brighter light on the need to find new ways to expand access.
In our present in-person clinical paradigm, time is a common barrier to healthcare access19; this applies to both practices and patients. Imagine how many times a patient has had to wait weeks or months to get an appointment wedged into an overwhelmed clinic schedule, or how many have delayed seeing a cardiologist because of the time and effort involved. For many patients, the financial20 and time costs of work, caring for a family member, transportation,21 and other expenses are significant barriers to seeking care.22
The COVID-19 pandemic has added a new obstacle as patients have delayed—or been delayed from—obtaining medical care for chronic illnesses or new subacute problems. A study by the Centers for Disease Control and Prevention found that 41% of US adults delayed or avoided medical care during the first 4 months of the pandemic.23 The longer the wait, the more fragmented patient management becomes. Patients who waited longer for their specialty appointment had a higher emergency department (ED) utilization rate during the 30-day period once referred to that specialty care.24 When patients go to urgent care or the ED rather than outpatient follow-up and referrals, they tend to have lower rates of follow-up and more no-shows. Having patients seen regularly, conveniently, and expeditiously helps address care gaps and manage conditions much more effectively. Telemedicine offers this for many patients by making the process of access more feasible, quick,25 and with good data for their clinical management.
There is concern that providing remote health care could sacrifice accuracy in diagnosis or confidence in management for the sake of convenience. However, technological leaps have provided us with much better tools to work with, including Bluetooth physiological monitoring devices that can provide abundant data that, if presented in an organized and concise way, would take mere minutes to manage (Figure 2).
Figure 2.
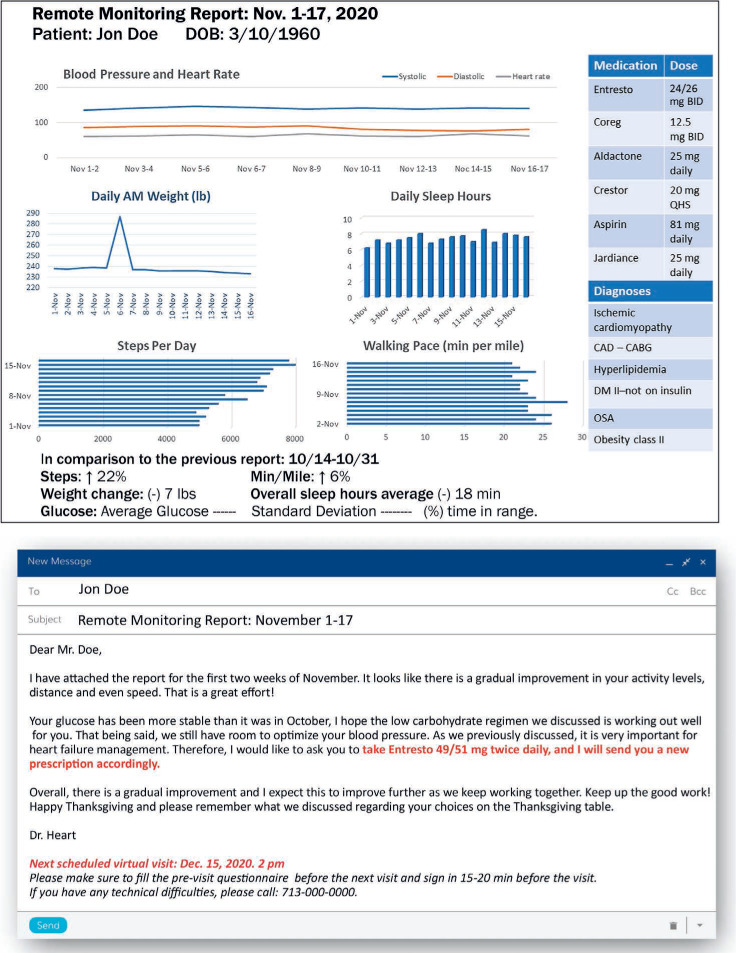
Sample remote monitoring report for a cardiovascular patient.
On the clinician side, telemedicine could help alleviate burnout, a problem that is all too common among physicians. A simple example is blood pressure (BP) monitoring. Many of my own patients provide their BP logs in the form of application reports, excel sheet logs, handwritten on paper with comments, and typed as a message in our electronic health record system. All of these different mechanisms make it difficult to manage in an efficient manner. My practice reviews an average of 15 BP logs a day. The time it takes to review each log, enter into the patient's chart, review meds, make chart notes, and quickly check labs to verify safety (eg, a patient on chlorthalidone or an angiotensin receptor blocker) is a process that takes many extra and unnecessary minutes per patient. A simplified workflow in which all data is simply uploaded in one report that a clinician can review, act upon, and use to communicate with patients would result in significant time and cost savings. In addition, the inefficiencies that clinicians deal with on a daily basis have a significant impact on their job satisfaction. For most specialties, some of the extra time spent on many of these inefficiencies can be managed via telemedicine and the associated tools for remote monitoring.
OPTIMIZING A TELEMEDICINE VISIT
One of the most important factors to ensure a successful telemedicine visit is preparation, the key to which is proper data collection. If the clinician has already been able to efficiently review all the relevant patient data at the time of the visit, the personal interaction with the patient could be optimized, giving the clinician and patient time to review the relevant data and care plan in detail. This streamlined data collection and review process would preserve time for actual clinical care and interaction and provide objective and accurate data to inform the clinical management. Figure 3 illustrates an efficient telehealth preparation plan.
Figure 3.
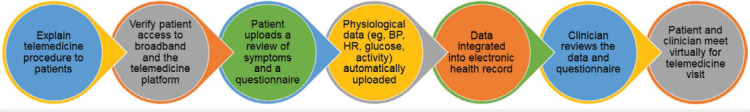
It's all in the prep: Best practices for preparing for a telemedicine visit. BP: blood pressure; HR: heart rate
TELEMEDICINE AND RESEARCH OPPORTUNITIES
The value of telemedicine in research can have a significant impact on data collection, even to the point where the “lost to follow-up” column in medical charts may become unnecessary. Many potential patients may consider enrolling (and continuing with follow-up) if the time commitment for follow-ups are not strenuous. Telemedicine and remote monitoring may offer a good solution for this, especially given that data collection is the most precious aspect of research studies.26,27
IMPACT ON CARDIOVASCULAR RISK FACTORS
A multitude of cardiovascular risk factors can be managed through telemedicine and digital health, both for primary prevention and for chronic established cardiovascular diseases. Of all the possible CV risk factors, hypertension and diabetes are among those with the largest potential impact15,28; hypertension alone is a clear risk factor for heart failure, coronary artery disease, stroke, and chronic renal disease, to name a few.
The United States has yet to reach a reasonable level of blood pressure control in the general population. In fact, recent data show that the numbers of uncontrolled hypertensive patients have been increasing over the last few years,29 and some evidence shows that more visits and interaction with clinicians is associated with better BP control.29 This highlights the need to communicate with patients more often, provide a platform for those who are not physically able to visit with their clinicians, and provide optimal data for better BP control.
Diabetes, another significant risk factor for cardiovascular disease, is also primed to be managed via telemedicine and remote monitoring.30,31 The general population is not only eagerly awaiting technological advances for better control but also bypassing the healthcare system altogether and forming its own coding systems for better glycemic control.32 The #WeAreNotWaiting movement has open-source looping systems to connect insulin pumps to continuous glucose monitoring devices in what is praised to be an artificial pancreas. They are even doing their own open-sourced research with surveys and data collection while the regulations are slow to catch up.33,34 The ability to provide better telemedicine tools for clinicians to interact with patients can result in a better outcome, again without the need for time-consuming in-person clinic visits.
CHALLENGES FACING TELEMEDICINE
Even with technological advances, patients and clinicians face multiple barriers to widespread implementation of telemedicine.
Patient Factors
Internet access. As telemedicine programs become more widely available, they are likely to unmask a significant socioeconomic obstacle: “fair” internet access. According to Pew Research, in 2018 there were clear disparities in home broadband access based on race (61% of Hispanic adults, 66% of black adults, 80% of white adults had broadband access) and income (56% of adults making < $30,0000/yr had broadband access; 72% making $30,000-50,000; 87% making $50,000–75,000; 92% making > $75,000). Community also plays a difference: 63% of adults in rural areas report using home broadband compared with 79% in suburban areas (one wonders if this speaks to the variation in broadband bandwidth quality). Pew estimated that about 17% of US adults are “smartphone dependent” in that they do not have home broadband and are completely dependent on their smartphones for internet access).35 The monopoly of neighborhood internet service providers is also a significant factor to access. These statistics are indicative of significant racial and socioeconomic disparities that must be addressed for the successful implementation of telemedicine and associated digital health tools. Improving access requires a combination of federal- and state-level legislation.
Culture change. As with some physicians, many patients cannot envision a relationship via live video and e-mail communication. Medicine has always been about building relationships with patients, so the adoption of telemedicine, like many other aspects of evolving care practices, requires patient education and discussion to manage expectations. For instance, clinics could create a video explaining the process of telemedicine and what a clinician can (and cannot) manage via remote data collection and video visits. The clinical team should also have a role in clearly explaining this to patients.
Patient awareness. Building on the above point of culture change, awareness of the patient-clinician relationship is a significant factor. Part of that culture shift is building awareness that telemedicine is an accessible and affordable option. If patients are unaware that telemedicine is offered, many might not think to ask. It is important to clearly explain to patients how this service can and cannot provide the care they need.
Payment. Subsidies to help patients with telemedicine copays could help encourage virtual follow-up visits. There are transportation subsidies for some patients to attend their in-person appointments, and these may be available to subsidize copayments for virtual follow-up visits.
Privacy. This is a significant concern for both patients and clinicians. Legislative guidelines should establish minimum security requirements for platforms to be licensed to offer telemedicine and remote monitoring services and for this to be tied to reimbursements. During the COVID-19 crisis, regulations were loosened for these visits. However, as new regulations and codes are implemented in the near future, privacy and security requirements should be included, with the flexibility to change as the technology changes.
Language. Language barriers are often a barrier to care, whether in person or via telemedicine. Live video platforms offering three- and four-way services could help address this issue to offer translation services during video visits. Furthermore, on-demand translation services should be a part of reimbursement.
Technical skills. Simplification of platforms is already underway. Much like smartphones have become ubiquitous and easy-to-use technology for the general public, telemedicine platforms must become simple and intuitive to encourage patients to take full advantage of telehealth opportunities. The Centers for Medicare & Medicaid Services (CMS) has acknowledged this and provided reimbursement codes to set up devices for proper patient follow-up. This, in turn, encourages clinicians and their office staff to make sure the process is simple and easy.36
Clinician Factors
Reimbursement. At the time of this writing, reimbursement for telehealth visits during the COVID-19 crisis nearly mirrors that of an in-office visit.37–39 However, this is not expected to continue. It is expected that new regulations and codes, primarily from CMS and subsequently other health insurers, would be offered for telemedicine visits. Before COVID-19 upended the healthcare business, there was already a CMS directive moving toward expanding telemedicine services, albeit at a much slower pace. Remote monitoring codes established before the pandemic could be used for telemedicine.
Technical skills. Patients may require minor assistance with occasional technical glitches. Although clinicians should not be trained in full technical support, they should be able to address simple mishaps to ensure smooth patient experiences. Supporting office staff should also be aware of the basic mishaps that may require an intervention and how to assist telehealth users.
Culture change. Many well-established physicians and practices may find it difficult to envision this change in healthcare delivery. However, as with many changes in practice norms—such as the adoption of radial access techniques—adaptation is feasible when the end result is better patient care. This might take time for some clinicians to adopt, but the technological move has been and will continue to be fast, so we need to understand and welcome these changes.
Expenses and finances. Initial expenses are required to set up virtual platforms, acquire resources, and hire and train personnel. Currently, there are many platforms and companies offering these services, and prices overall are relatively reasonable, especially with the current reimbursement rates. Many electronic health record systems have built-in telemedicine systems, but even for smaller institutions and practices, platforms such as Doximity have offered 2- and 3-way secured video conferencing for virtual care at reasonable prices. However, if reimbursement rates drop as expected, it may affect budgets for these services. Notably, since a significant portion of telemedicine visits are for established patients, this could create room in the clinic schedule for revenue-generating new patient referrals, potentially offsetting any losses from telehealth visits.
Regulations. Although regulations are more of a healthcare system factor than a clinician factor, clinicians can and should play a role in shaping more favorable regulations for patients and providers alike. For instance, implementing federal regulations to allow telemedicine and remote monitoring services across state lines will offer not just access to healthcare for patients who are in need but would also offer a broader choice for healthcare services.
CONCLUSION
Rapid advances in digital technology coupled with the sudden need for remote healthcare solutions during the COVID-19 pandemic have thrust telemedicine into the forefront of remote healthcare delivery. Although replacing in-person visits with telemedicine or remote monitoring is clearly not appropriate for all patients, it can be implemented in much of our patient population for primary and secondary cardiovascular disease management and, in some instances, for triaging acute cardiovascular disease processes.
Many major tech companies are betting on the digital medical future, and so should we. With the right tools, and taking the time and steps to optimize the process, telemedicine could become a powerful equalizer for patient care. Pandora's box has been opened, and we, as clinicians, should be prepared and play active roles in ensuring that telemedicine implementation and regulation are optimized to serve our patients and our professional community.
KEY POINTS
The need for remote care options during the COVID-19 pandemic has accelerated adoption of telemedicine.
Telemedicine offers opportunities to better integrate remote monitoring into clinical care, improve patient engagement, save time and money for patients and healthcare providers, and alleviate physician burnout.
Cardiovascular risk factors, particularly hypertension and diabetes, can be managed through telemedicine.
There are still significant barriers to widespread implementation, including inequities in internet access, patient awareness, privacy and reimbursement regulations, and cultural change away from reliance on in-person visits.
Footnotes
Conflict of Interest Disclosure:
The author has completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1.Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington (DC): National Academies Press (US); 1996. DOI. [DOI] [PubMed] [Google Scholar]
- 2.Gershon-Cohen J, Cooley AG. Telognosis. Radiology. 1950 Oct;55(4):582–7. doi: 10.1148/55.4.582. doi. [DOI] [PubMed] [Google Scholar]
- 3.Davis DA, Thornton W, Grosskreutz DC, Sugioka K, McKnight R. Radio telemetry in patient monitoring. Anesthesiology. 1961 Nov-Dec;22:1010–3. doi: 10.1097/00000542-196111000-00024. doi. [DOI] [PubMed] [Google Scholar]
- 4.Nagel EL, Hirschman JC, Mayer PW, Dennis F. Telemetry of physiologic data: an aid to fire-rescue personnel in a metropolitan area. South Med J. 1968 Jun;61(6):598–601. doi: 10.1097/00007611-196806000-00009. doi. [DOI] [PubMed] [Google Scholar]
- 5.Hirschman JC, Baker TJ, Schiff AF. Transoceanic radio transmission of electrocardiograms. Dis Chest. 1967 Aug;52(2):186–90. doi: 10.1378/chest.52.2.186. doi. [DOI] [PubMed] [Google Scholar]
- 6.Brecht RM, Gray CL, Peterson C, Youngblood B. The University of Texas Medical Branch–Texas Department of Criminal Justice Telemedicine Project: findings from the first year of operation. Telemed J. 1996 Spring;2(1):25–35. doi: 10.1089/tmj.1.1996.2.25. doi. [DOI] [PubMed] [Google Scholar]
- 7.Russo JE, McCool RR, Davies L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed J E Health. 2016 Mar;22(3):209–15. doi: 10.1089/tmj.2015.0055. doi. [DOI] [PubMed] [Google Scholar]
- 8.Serrano KJ, Thai CL, Greenberg AJ, Blake KD, Moser RP, Hesse BW. Progress on Broadband Access to the Internet and Use of Mobile Devices in the United States. Public Health Rep. 2017 Jan-Feb;132(1):27–31. doi: 10.1177/0033354916679365. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CBInsights [Internet]. New York, NY: CB Information Services, Inc.; c2020. Where Big Tech Is Placing Bets In Healthcare; 2018 Sep 13 [cited 2020 Nov 12]. Available from: cbinsights.com. https://www.cbinsights.com/research/top-tech-companies-healthcare-investments-acquisitions/ [Google Scholar]
- 10.Carman KL, Dardess P, Maurer M et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood) 2013 Feb;32(2):223–31. doi: 10.1377/hlthaff.2012.1133. doi. [DOI] [PubMed] [Google Scholar]
- 11.Widmer RJ, Collins NM, Collins CS, West CP, Lerman LO, Lerman A. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc. 2015 Apr;90(4):469–80. doi: 10.1016/j.mayocp.2014.12.026. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maddison R, Rawstorn JC, Stewart RAH et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019 Jan;105(2):122–9. doi: 10.1136/heartjnl-2018-313189. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torri A, Panzarino C, Scaglione A et al. Promotion of Home-Based Exercise Training as Secondary Prevention of Coronary Heart Disease: A PILOT WEB-BASED INTERVENTION. J Cardiopulm Rehabil Prev. 2018 Jul;38(4):253–8. doi: 10.1097/HCR.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 14.Batsis JA, Pletcher SN, Stahl JE. Telemedicine and primary care obesity management in rural areas - innovative approach for older adults? BMC Geriatr. 2017 Jan;517(1):6. doi: 10.1186/s12877-016-0396-x. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milani RV, Lavie CJ, Bober RM, Milani AR, Ventura HO. Improving Hyper-tension Control and Patient Engagement Using Digital Tools. 2017 Jan;130(1):14–20. doi: 10.1016/j.amjmed.2016.07.029. DOI. [DOI] [PubMed] [Google Scholar]
- 16.Yatabe MS, Yatabe J, Asayama K et al. The rationale and design of reduction of uncontrolled hypertension by Remote Monitoring and Telemedicine (REMOTE) study. Blood Press. 2018 Apr;27(2):99–105. doi: 10.1080/08037051.2017.1406306. [DOI] [PubMed] [Google Scholar]
- 17.Bell CN, Thorpe RJ, Bowie JV, LaVeist TA. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Ann Epidemiol. 2018 Mar;28(3):147–152. doi: 10.1016/j.annepidem.2017.12.007. doi. [DOI] [PubMed] [Google Scholar]
- 18.Doshi T, Smalls BL, Williams JS, Wolfman TE, Egede LE. Socioeconomic Status and Cardiovascular Risk Control in Adults With Diabetes. Am J Med Sci. 2016 Jul;352(1):36–44. doi: 10.1016/j.amjms.2016.03.020. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelly SA, Schesing KB, Thibodeau JT, Ayers CR, Drazner MH. Feasibility of Remote Video Assessment of Jugular Venous Pressure and Implications for Telehealth. JAMA Cardiol. 2020 Jul 1;5(10):1194–1195. doi: 10.1001/jamacardio.2020.2339. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007 Mar 14;297(10):1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 21.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013 Oct;38(5):976–93. doi: 10.1007/s10900-013-9681-1. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for U.S. adults. Health Serv Res. 2012 Feb;47(1 Pt 2):462–85. doi: 10.1111/j.1475-6773.2011.01308.x. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC [Internet] Atlanta, GA: U.S. Department of Health & Human Services; c2020. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns — United States, June 2020; 2020 Sep 11 [cited 2020 Nov 12]. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm. [Google Scholar]
- 24.Ryu J, Lee TH. The Waiting Game - Why Providers May Fail to Reduce Wait Times. N Engl J Med. 2017 Jun 15;376(24):2309–11. doi: 10.1056/NEJMp1704478. doi. [DOI] [PubMed] [Google Scholar]
- 25.Dullet NW, Geraghty EM, Kaufman T et al. Impact of a University-Based Out-patient Telemedicine Program on Time Savings, Travel Costs, and Environmental Pollutants. Value Health. 2017 Apr;20(4):542–546. doi: 10.1016/j.jval.2017.01.014. doi. [DOI] [PubMed] [Google Scholar]
- 26.Reuters Events Pharma [Internet] London: Reuters Events; c2020. Tele-medicine: The future of clinical trials; 2019 Dec 13 [cited 2020 Nov 12]. Available from: https://social.eyeforpharma.com/clinical/telemedicine-future-clinical-trials. [Google Scholar]
- 27.Reuters Events Pharma [Internet] London: Reuters Events; c2020. How Telehealth & Remote Care Enable Faster, More Efficient Virtual Clinical Trials; 2020 [cited 2020 Nov 12]. Available from: https://news.careinnovations.com/blog/telehealth-remote-care-faster-more-efficient-virtual-clinical-trials. [Google Scholar]
- 28.McManus RJ, Mant J, Franssen M et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018 Mar 10;391(10124):949–59. doi: 10.1016/S0140-6736(18)30309-X. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muntner P, Hardy ST, Fine LJ et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999–2000 to 2017–2018. JAMA. 2020 Sep 22;324(12):1190–1200. doi: 10.1001/jama.2020.14545. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bergenstal RM, Layne JE, Zisser H Diabetes Technol Ther. 2020. Nov 5, Remote Application and Use of Real-Time Continuous Glucose Monitoring by Adults with Type 2 Diabetes in a Virtual Diabetes Clinic. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dixon RF, Zisser H, Layne JE et al. A Virtual Type 2 Diabetes Clinic Using Continuous Glucose Monitoring and Endocrinology Visits. J Diabetes Sci Technol. 2020 Sep;14(5):908–11. doi: 10.1177/1932296819888662. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marshall DC, Holloway M, Korer M, Woodman J, Brackenridge A, Hussain S. Do-It-Yourself Artificial Pancreas Systems in Type 1 Diabetes: Perspectives of Two Adult Users, a Caregiver and Three Physicians. Diabetes Ther. 2019 Oct;10(5):1553–64. doi: 10.1007/s13300-019-00679-y. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The OPEN Survey [Internet] Dublin, Ireland: The OPEN Project; c2020. Diabetes open looping systems; 2020 [cited 2020 Nov 12]. Available from: https://open-diabetes.eu/en/open-survey/ [Google Scholar]
- 34.SmartCompany [Internet] Melbourne, Austrailia: Smart Company; c2020. A DIY approach to personal healthcare devices is changing the way people manage disease — but regulation is falling behind; 2020 Nov 2 [cited 2020 Nov 12]. Available from: https://www.smartcompany.com.au/industries/health/iot-healthcare-devices-regulation/ [Google Scholar]
- 35.Pew Research Center [Internet] Washington, DC, USA: Pew Research Center; c2020. Internet/Broadband Fact Sheet; 2019 Jun 12 [cited 2020 Nov 12]. Available from: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ [Google Scholar]
- 36.Centers for Medicare & Medicaid Services [Internet] Baltimore, MD: U.S. Centers for Medicare & Medicaid Services; c2020. President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak; 2020 Mar 17 [cited 2020 Nov 12]. Available from: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak. [Google Scholar]
- 37.Hartnett KP, Kite-Powell A, DeVies J et al. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020 Jun 12;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Office of the Texas Governor [Internet] Austin, TX: Office of the Texas Governor; c2020. Governor Abbott Waives Certain Regulations for Tele-medicine Care in Texas; 2020 Mar 17 [cited 2020 Nov 12]. Available from: https://gov.texas.gov/news/post/governor-abbott-waives-certain-regulations-for-telemedicine-care-in-texas. [Google Scholar]
- 39.Commonwealth of Massachusetts [Internet] Boston, MA: Commonwealth of Massachusetts; c2020. Order Expanding Access to Telehealth Services and to Protect Health Care Providers; 2020 Mar 10 [cited 2020 Nov 12]. Available from: https://www.mass.gov/doc/march-15-2020-telehealth-order/download. [Google Scholar]


