Abstract
Background and Aims:
Healthcare workers (HCW's) who have contracted the disease while working in the hospital may have a deep psychological impact in the form of depression and anxiety, along with the stress of passing the infection to their family members. This study attempts to highlight the risk factors and psychological impact on doctors who have tested positive for coronavirus disease-2019 (COVID-19).
Material and Methods:
This online cross-sectional survey-based study enrolled all level doctors of all specialities of in Mumbai, India, who had tested positive for novel coronavirus. The survey questionnaire was a 26-item self-administered anonymous set of questions in English language only. This validated questionnaire was distributed by a link via Google forms for 1 week.
Results:
We received 51 completed responses. Most of them were (67%) postgraduate students. Forty-three (85%) respondents were working in a COVID-19 center. Twenty-three (45%) had a history of contact with these patients without proper personal protective equipment (PPE) with unknown COVID-19 status of the patient at the time of contact. Ten percent regretted their decision of becoming a doctor. Only half (51%) had family support during their illness and 45% relied on friends and colleagues in the hospital. Twenty-six percent mentioned having a low mood throughout the illness. A major portion of people (32%) having fear of severe illness and death.
Conclusion:
Medical doctors working in direct contact with confirmed cases of COVID-19 are at increased risk of contracting the infection and it has a major impact on physical and mental health of medical doctors.
Keywords: COVID-19, healthcare workers, mental health, psychological impact, risk factors
Introduction
The world is currently facing an outbreak of the Coronavirus disease (COVID-19) pandemic, after the first case detected in Wuhan, China on November 17, 2019 and spread to almost every country of the world.[1] Healthcare workers (HCWs) are working at the front line in response to this pandemic and as such are exposed to hazards that put them at risk of infection with the SARS-CoV-2 virus. Many procedures causing exposure to respiratory droplets or aerosols from the patient's airways[2] during their interactions in emergency departments, wards and operation theatres, performance of airway related procedures, and care of critically ill patients increase the risk of HCWs contracting the COVID-19. It is highly important to acknowledge not just the physical but also the psychological impact on HCWs who are braving this highly infectious disease and treating patients with often limited resources and constantly changing guidelines as the world struggles to cope with the burden of this disease. Many frontline HCWs are contracting with the COVID-19 around the world and it is important to know the exact nature of exposure, associated risk factors, and their attitude and mental status after they contracted the disease.
This study was designed to highlight the risk factors and psychological impact on front line medical doctors who have tested positive for COVID-19 as confirmed by reverse transcription-polymerase chain reaction (RT-PCR) testing.
Material and Methods
This online cross-sectional survey-based study enrolled medical graduates, postgraduate students of all specialties, junior or attending consultants, and senior consultants of various public or private medical colleges, postgraduate institutions, and private/corporate hospitals in the metro city of Mumbai in India, who had tested positive for novel coronavirus. Mumbai is a one of the major hotspot of the COVID-19 outbreak in the world. This study was conducted over one week from June 7, 2020 to June 14, 2020.
This study was conducted anonymously maintaining the privacy of participants. None of the investigators were aware of who were the participants. Anonymity was maintained by contacting a common contact (usually a resident doctor or/and faculty member in respective colleges/institutes/accredited institutes) who is not supposed to disclose the names of the COVID-19 positive medical doctors. Faculties from various departments of tertiary institutes were contacted in Mumbai who were willing to share the questionnaire with their known COVID-19 positive doctors without revealing their identities. The survey link was sent via WhatsApp freeware with a request to forward the same link to the participants’ personal WhatsApp numbers or Email. The survey questionnaire is a 26-item self-administered anonymous set of questions in English language only. The questionnaire comprised of two parts: the first part was pertaining the demographic details and known risk factors which may lead to transmission of COVID-19, and the second part consisted questions related to the stigma, fear and anxiety faced. This questionnaire was developed by a consultant physician who was diagnosed as COVID-19 positive, in consultation with other doctor working in COVID-19 facility. This Questionnaire was internally validated for simplicity, clarity, ambiguity, and relevance of each question. Preliminary part of the questionnaire consisted of demographic data of the participants. Majority of the 26 questions offered single best response answers. Few questions allowed the multiple responses. Successfully completing the questionnaire was considered as consent for participation in the survey. This validated questionnaire was distributed by a link via Google forms [Appendix]. Google form is an online survey cloud based software with the capability to input answers and validate them. After the study period of one week elapsed, the total number of responses which were recorded were collated. These responses were subsequently screened for completeness and the completed responses were included in the final analysis. Data was collated from the survey forms and analyzed. Frequencies were used to describe the demographic data. Data analysis for comparisons was done using Chi-square or Fisher's exact test with P < 0.05 considered as significant. Statistics were done using SPSS version 23.
Results
At the end of 1 week we received 51 completed responses. Among the respondents, 33 (64%) were males and 18 (36%) were females. Thirty-six (70%) participants were less than 30 years, 14 (28%) were between 30-50 years and one (2%) was above 50 years of age. As per position in their workplace maximum, 34 (67%) respondents were postgraduate students, 8 were junior consultants (15%), 5 were medical undergraduates who just completed their medical degree (10%) and 4 were senior consultants (8%) [Table 1].
Table 1.
Demographics and professional status
| Demographics | Number of people |
|---|---|
| Male:Female | 33 (64%):18 (36%) |
| Age groups (Years) | |
| <30 | 36 (70%) |
| 30-50 | 14 (28%) |
| >50 | 1 (2%) |
| Professional status | |
| Medical Interns | 5 (10%) |
| Postgraduate students | 34 (67%) |
| Junior consultants | 8 (15%) |
| Senior consultants | 4 (8%) |
Eighteen (35%) participants belonging to Internal Medicine, Pulmonary Medicine and Paediatrics, 13 (25%) from para-clinical specialities like community medicine and pathology and 10 (20%) from anaesthesia and intensive care [Figure 1].
Figure 1.
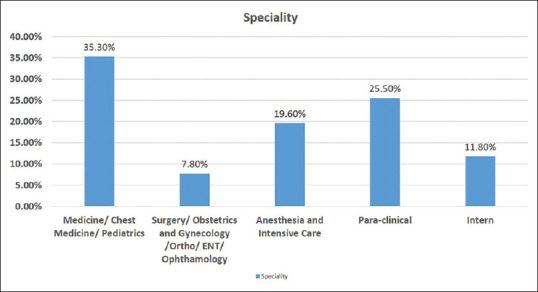
Speciality distribution among health care workers diagnosed with COVID-19
Majority (86%) of the respondents had no comorbidities, the most common comorbidity was hypothyroidism in 4% of the respondents. The other comorbidities were hypertension, diabetes mellitus, hyperparathyroidism, asthma, and beta-thalassemia.
Forty-three (85%) respondents were working in a COVID-19 dedicated center with separate wards, operation theatres, and intensive care units (ICU) for COVID-19 positive patients. Thirty-five (68%) respondents were working on the frontline caregivers with direct COVID-19 positive patient contact. Twenty-three (45%) had a history of contact with these patients without proper personal protective equipment (PPE) with unknown COVID-19 status of the patient at the time of contact. Ten percent of respondents claimed that adequate PPE was unavailable at their place of work. With regards to prophylaxis against the disease, 34 (66%) respondents had taken Hydroxychloroquine recommended by the Indian Council of Medical Research, New Delhi, Indiaprior to their diagnosis.[3] With respect to the nature of their duties/exposure, 21 (41%) were involved in aerosol-generating procedures such as intubation, extubation, suctioning, and endoscopy. Thirty-five (68%) were also in close contacts in the form of co-habitants who were working in COVID-19 dedicated centers, thus increasing their chances of exposure to the disease [Figure 2].
Figure 2.
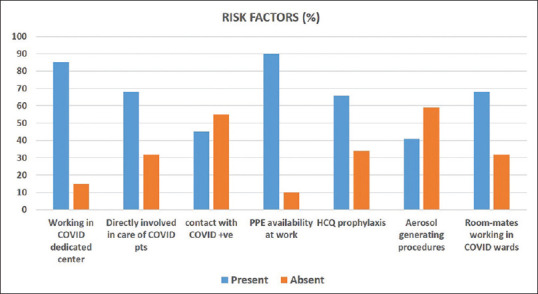
Risk factors among health care workers diagnosed with COVID-19
The most common symptoms were fever (66%), sore throat (49%), loss of sense of smell and taste (39%). Six doctors (12%) were asymptomatic. Other less common symptoms were cough, diarrhea, throat irritation, myalgia, and runny nose. Most of them were provided with hospital isolation (59%), while the rest were isolated in home (21%) and hotels (20%). The duration of the isolation was mostly 2 weeks (80%) and the maximum duration of isolation was 4 weeks.
Ten percent of doctors mentioned that because of contacting COVID-19 as a professional hazard they regretted their decision of becoming a doctor and they probably would have been safer in other professions. Fifty-one percent had immediate family support during their illness and 45% relied on friends and colleagues in the hospital.
On a scale of 1–10 with 1 being utterly depressed, 5 being stable/balanced, and 10 being normal mood, most of them marked their mood as average (rating of 5). Twenty-six percent mentioned having a low mood throughout the illness. A major portion of people (32%) reported having fear of severe illness and death. To maintain stable mental health during their isolation period the most popular activities that people indulged in were chatting with family and friends, online recreation, meditation, academic work, and exercise in that order. Two percent of doctors mentioned that they could not focus on anything. Eighty-two percent of doctors mentioned that they were less confident about the current infection control measures. Majority of the participants (62%) feared re-infection after re-joining work to the extent that 21% of the participants have strongly considered quitting their job or applying for extended leave at their place of work due to COVID-19 [Figure 3].
Figure 3.
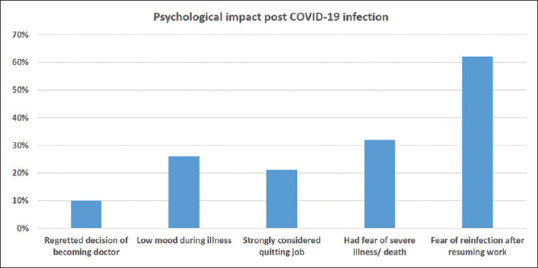
Psychological impact of COVID-19 on affected healthcare workers
Discussion
During a pandemic, HCWs are expected to work long hours under significant pressure with often inadequate or inappropriate resources, while accepting the dangers of close interaction with sick patients. HCWs are vulnerable both to the disease itself and to the misinformation that may increase their anxiety levels.[4] The National Health Commission of the People's Republic of China reported that as of February 24, 2020, a total of 3387 of 77,262 patients with COVID-19 (4.4%) in China were HCWs or others who worked in medical facilities.[5]
In the COVID-NET study done across the USA, 54% of COVID-19-associated hospitalizations occurred in males and 46% occurred in females.[6] According to Wei-Jei Guan et al., who elaborated on the clinical characteristics of COVID-19 in China, 59% of the affected patients were males.[7] Our study also validates their findings that males are at higher risk (64% in our study) of contracting COVID-19 as compared to females.
The median age of the patients was >65 years in COVID-NET study (6) and 47 years in the study by Wei-Jei Guan et al.,[7] In our study however 70% of the afflicted were <30 years of age. This may be because of the number of duties, clinical responsibilities, hours of exposure, and direct contact by junior doctors (especially those doing their residency) as compared to senior doctors. This is also shown by the fact that 67% of the respondents were residents from various medical colleges across the city.
In a study by Wang J et al.,[8]25% of the doctors affected in China with COVID-19 were belonging to the Pulmonary Medicine and Critical Care Medicine. Our study showed that most of the respondents (45%) belonged to clinical specialities of Internal Medicine, Pulmonary Medicine, Paediatrics, and Anaesthesiology and Intensive Care. This may be because of active participation of these specialities in wards, intensive care unit management and exposure to patients’ droplets during aerosol-generating procedures like tracheal intubation, extubation, bag-mask ventilation, and suctioning.
In our study, 68% of the respondents were frontline caregivers at a dedicated COVID admitting hospital. China's National Health Commission showed that 3300 HCWs were infected as of early March 2020 and in Italy, 20% of responding HCWs were infected.[5,9] In our study, we approached only to medical doctors and not all HCWs, so numbers are less than other studies. Access to PPE for HCWs is of utmost concern and should be used during confirmed COVID-19 patient contact or unknown COVID-19 status, because in our study, 45% of the participants had a history of exposure to patients without PPE and that is because of unknown COVID-19 status at the time of contact.
There is increasing evidence that suggests that COVID-19 can be an independent risk factor for stress in HCWs. Nearly 26% of our participants showed a low mood during their period of disease detection and isolation. In a study in Hubei province of China, frontline workers and medical staff showed various degrees of anxiety and depression mainly attributed to personal safety and concerns of viral transmission to their families.[10] Another study in China, involving 1257 HCWs from 34 hospitals with a fever clinic or COVID-19 treating facility, studied the degree of symptoms of depression, anxiety, insomnia, and distress was assessed by various scales and questionnaires. A major proportion of respondents reported symptoms of depression (50.4%), anxiety (44.6%), insomnia (34.0%), and distress (71.5%). Female staff, Nurses, frontline HCWs, and those working in Wuhan city of China, reported more severe degrees of mental health symptoms than other HCWs.[11] In our study, 31% of participants were often worried about the spread of illness to their family members through themselves. Lai et al. have shown that during infectious disease epidemics, support from family and friends, as well as a positive attitude, have previously been shown to reduce stress.[12] More than half (51%) of our participants mentioned that they had family support during their disease detection and recovery period.
As the pandemic continues, essential clinical and administrative strategies are needed to support HCWs. Our study focused on a particularly vulnerable group susceptible to psychological distress. Mohindra et al.,[13] conducted an interview-based study among HCWs working in COVID-19 treating institute, to find out the perceived motivations influencing morale amongst HCWs. The interview includes positive motivational factors for intellectuals and emotional factors that need to be strengthened; negatives, frustrations associated with patient care and personal fears and annoyances experienced by doctors. Special care should be focused on giving psychological support like counseling services, adequate remuneration and development of support systems among colleagues. Also mandatory insurance of frontline HCWs and reassurance by the governing authorities that the family needs of HCWs will be taken care. It would also help to better community awareness to reduce social stigma related to frontline HCWs.[13] Elderly HCWs and those with significant comorbidities or on immunosuppressive medications can be spared from working if possible or they should be allowed to work in nonpatient area.[14] Mental health issues in COVID-19 afflicted HCWs should be treated by preferably psychotherapeutic means based on the stress adaptation model.[15] Other options that should be explored are setting of psychological intervention teams and online medical advice based platforms to help battle the psychological impact of this disease on frontline HCWs.
Our survey has few limitations, this study was conducted amongst tertiary care HCW's in Mumbai which was badly affected by the pandemic, our results may not be representative of the doctors’ population at large. Our study has focused only on the HCWs who have contracted the disease and not all HCWs working on the frontline. We were unable to calculate the sample size because number of physicians diagnosed with COVID-19 were not known to us because of privacy concerns and lastly mental health questions were not formulated in consultation with a trained clinical psychologist or other mental health expert and it only indicates the general mental health of the respondent.
Conclusion
Medical doctors working in direct contact with confirmed cases of COVID-19 are at increased risk of contracting the infection and it has a major impact on physical and mental health of medical doctors who diagnosed as COVID-19 positive.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix: Survey Questionnaire
Survey of risk factors and post-exposure attitude among physicians diagnosed with COVID-19
Hello all, this study is aimed at evaluating the possible exposure sources, isolation patterns and mental health wellbeing of doctors who have tested positive for COVID-19. The response to these questions will remain anonymous and will be used purely for academic purposes. Thank you for your kind participation.
* Required
-
1. Gender *
- Male
- Female
-
2. Age group *
- < 30 years
- 30-50 years
- > 50 years
-
3. Kindly mark if you have any of the co-morbidities. *
- Diabetes Mellitus
- Hypertension
- COPD
- Thyroid disorders
- IHD
- Liver disease
- Kidney disease
- None
- Other:
-
4. What is your position at your workplace? *
- Intern
- Resident
- Junior consultant
- Senior consultant
-
5. Primary specialty *
- Medicine/ Chest Medicine/ Pediatrics etc. Surgery/ Obstetrics and Gynecology / Ortho/ ENT/ Ophthalmology etc. Anesthesia and Intensive Care Non -clinical / Para-clinical specialty:
- Other

Please attend all questions
-
6. Is your Workplace a dedicated / admitting COVID center? *
- yes
- No
-
7. Were you in contact with a confirmed COVID + case without Personal protective equipment (PPE)? *
- Yes
- No
-
8. Have you been working on the frontline (OT/ ICU/Ward) treating COVID patients? *
- Yes
- No
-
9. What was the reason of testing? *
- Symptoms
- Exposure
-
10. Were you involved in aerosol generating procedures like intubation / extubation/ suctioning / endoscopy? *
- Yes
- No
-
11. Is PPE adequately available at your place of work? *
- Yes
- No
-
12. Were you taking HCQS prophylaxis? *
- Yes
- No
-
13. Were your co-habitants working for COVID patients at time of detection? *
- Yes
- No
- I was staying alone
-
14. What symptoms did you have? *
- Cough
- Fever
- Diarrhea
- Sore throat
- Loss of sense of smell/ taste
- None
- Other:
-
15. Place of Quarantine *
- Home
- Hotel
- Hospital
-
16. Duration of quarantine *
- 2 weeks
- 3 weeks
- More than 3 weeks
-
17. Since you tested positive have you ever regretted becoming a doctor? *
- Yes
- No
-
18. What support system did you have during your illness? *
- Family
- Friends / colleagues
- None
-
19. Are you happy with the support system you have/ had during your illness? *
- Yes
- No
- Somewhat
-
20. On the scale of 1-10 how do you rate your general mood at time of illness (5- stable / balanced) *
- Very depressed 1 2 3 4 5 6 7 8 9 10 Positive and happy
-
21. Are you worried about your family members getting infected because of you? *
- Not at all
- Often
- Most of the time
- Always
-
22. Do you feel under confident about the spread of the infection with the current infection control measures? *
- Yes
- No
-
23. Do you fear re-infection after joining back work after recovery? *
- Yes
- No
-
24. Have you strongly considered quitting/ applying for extended leave at work because of COVID-19? *
- Yes
- No
-
25. Do you have fear of severe illness or death? *
- Yes
- No
-
26. How are you keeping good mental health during your isolation period? (Tick all applicable) *
- Chatting with friends and family
- Watching movies / web series
- meditation/ Yoga
- Exercise
- Prayers Academic work
- Other:
-
References
- 1.World Health Organisation: WHO announces COVID-19 outbreak a pandemic. [Last accessed on 2020 Jun 24]. Available from: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic .
- 2.Dost B, Koksal E, Terzi Ö, Bilgin S, Ustun YB, Arslan HN. Attitudes of anesthesiology specialists and residents toward patients infected with the novel coronavirus (COVID-19): A national survey study. Surg Infect (Larchmt) 2020;21:350–6. doi: 10.1089/sur.2020.097. [DOI] [PubMed] [Google Scholar]
- 3.Indian Council of Medical Research advisory on the use of Hydroxychloroquine as prophylaxis for SARS-CoV2 infection. [Last accessed on 2020 Jun 24]. Available from: https://www.mohfw.gov.in/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxisforSARSCoV2infection.pdf .
- 4.Schwartz J, King C-C, Yen M-Y. Protecting healthcare workers during the coronavirus disease 2019 (COVID-19) outbreak: Lessons from Taiwan's severe acute respiratory syndrome response. Clin Infect Dis. 2020;71:858–60. doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Health Commission of the People's Republic of China. Transcript of the press conference of the China-WHO Joint Expert Investigation Team on Covid-19 on February 25, 2020. [Last accessed on 2020 Jun 24]. Available from: https://www.who.int/docs/default-source/coronaviruse/transcripts/joint-mission-press-conference-script-english-final.pdf?sfvrsn=51c90b9e_2 .
- 6.Garg S, Kim L, Whitaker M, O’Halloran L, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019-COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–64. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100–1. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19: Protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological impact and coping strategies of frontline medical staff in hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei, China. Med Sci Monit. 2020;26:e924171. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020;258:1049–55. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohindra R, R R, Suri V, Bhalla A, Singh SM. Issues relevant to mental health promotion in frontline health care providers managing quarantined/isolated COVID19 patients. Asian J Psychiatr. 2020;51:102084. doi: 10.1016/j.ajp.2020.102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solanki SL, Thota RS, Garg R, Pingle AA, Goswami J, Rangnath N, et al. Society of onco-anesthesia and perioperative care (SOAPC) advisory regarding perioperative management of onco-surgeries during COVID-19 pandemic. Indian J Anaesth. 2020;64(Suppl S2):97–102. doi: 10.4103/ija.IJA_447_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folkman S, Greer S. Promoting psychological well-being in the face of serious illness: When theory, research and practice inform each other. Psychooncology. 2000;9:11–9. doi: 10.1002/(sici)1099-1611(200001/02)9:1<11::aid-pon424>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]


