Abstract
Background & Aims
Sickle cell disease (SCD), a genetic disorder resulting from the presence of a mutated hemoglobin S (HbS), has a worldwide distribution and causes significant morbidity and mortality in children and adults. Few studies addressed the determinants of SCD severity in adults; therefore, we investigated the impact of nutrition on the outcome of SCD and health-related quality of life (HRQoL) in adult patients.
Methods
In this longitudinal study, we recruited and prospectively followed 62 adults with SCD (aged ≥18 years) for a median of 93 months. At entry and follow-up, patients provided medical and dietary history, had a physical examination and anthropometric measurements, assessed protein-energy intake, measurement of micronutrient levels, estimation of SCD severity score, and determination of the HRQoL (SF-26v2). The study outcome was a composite of hospitalization due to SCD crises or death.
Results
At baseline, 42 (67.74%) patients had macro and, or micro-undernutrition (Group A), and 20 (32.26%) were well nourished. (Group B). The BMI and most anthropometric measurements were significantly lower in SCD patients compared to control subjects. Seventy percent of SCD patients had vitamin D, vitamin B12, and zinc deficiencies. Thirty-six under-nourished patients (86%) had gastrointestinal disorders. During follow-up, 46 patients (74.19%) developed one or more vaso-occlusive pain crises or other SCD related complications that required hospitalization. Significant differences in most SF-36v2 domains existed between well-nourished and undernourished SCD patients. Protein-energy and micronutrient deficiencies were independent predictors of severe SCD and mortality. Correction of undernutrition and hydroxyurea therapy improved SCD severity scores and HRQoL.
Conclusions
Patients with sickle cell disease have various degrees of macro and micro deficiencies, which increase SCD severity and hospitalizations and reduce the health-related quality of life. Early diagnosis and prompt correction of macro and micronutrient deficiencies need to be incorporated in the standard of care of SCD patients to improve the disease outcomes.
Keywords: Sickle cell disease, Macronutrient, Micronutrient, Health-related quality of life, Vitamin D, Zinc
Introduction
Sickle cell anemia (SCA) is a common autosomal-recessive hemoglobinopathy caused by mutations in the HBB gene resulting in the formation of pathological hemoglobin S (HbS) and ‘sickle’ shaped erythrocytes which deform under stress.1 Sickle cell anemia has a global distribution with high prevalence in Africa, Mediterranean countries, Middle Eastern countries, and India.2,3 In the United States, SCA is the most common inherited blood disorder among African Americans and Hispanics.4 Active global migration altered the epidemiology and geographical distribution of sickle cell anemia due to increased influxes of migrants from regions with high HbS prevalence towards Europe and North America.5 In the Kingdom of Saudi Arabia (KSA), 17% of Saudi adults carry the sickle-cell gene, and 3% of the population has SCD.6 Most cases of SCD cluster in southern and eastern Saudi Arabia.7
Sickle cell disease is a lifelong disorder that causes acute and chronic symptoms and signs of variable severity. Intravascular sickling of the red blood cells in smaller vessels vaso-occlusion leading to ischemia, necrosis, inflammation, and multi-organ damage.8,9 Patients with SCD are at risk of developing life-threatening complications requiring urgent care such as vaso-occlusive pain crisis, acute chest syndrome, stroke, pulmonary hypertension, and aplastic crisis.10,11 Over the past decades, the survival of children with SCD has improved substantially due to the early diagnosis and the advances in the management strategies, including blood transfusions, hydroxycarbamide, and stem cell transplantation.1,12 Thus, SCD is currently not restricted to children, but it became a chronic disease that causes morbidity and mortality in pediatric and adult populations.
Given the heterogeneity of SCD clinical manifestations and outcomes, a consensus on a specific definition for SCD severity has not yet been achieved. Several reports considered the rate of acute painful vaso-occlusive episodes requiring hospitalizations as a measurement of SCD severity. In some studies, investigators utilized different clinical events and laboratory parameters to generate measurable SCD severity indices and predictive models for identifying patients at risk of developing severe complications to initiate adequate disease-modifying therapies and prevent organ damage.13–16 However, the accuracy and predictive performance of the majority of the severity scores need to be validated.
The determinants of disease severity and outcome in patients with SCD are not well verified. Studies showed that genetic factors such as β-globin genotype, HbF, and β-globin haplotype, the co-inheritance of a-thalassemia, and glucose-6-phosphate dehydrogenase (G6PD) deficiency or polymorphisms of uridine diphosphate glucuronosyltransferase A1 (UGT1A1) promoter might influence the clinical course of SCD.17,18 To date, few studies investigated the potential role of acquired and environmental factors in modifying SCD progression and outcome.19,20 Nutrition is a critical component in the pathogenesis and course of various chronic diseases such as diabetes mellitus, cardiovascular and pulmonary diseases.21,22 Macro and micro-malnutrition, which results from insufficient food or micronutrient intake or reduced absorption, causes alterations in the body functions and composition and the impairment of the immune responses.23,24 To date, the impact of nutrition on SCD severity and the quality of life in adults with SCD is not well defined. Therefore, we conducted a comprehensive longitudinal assessment of the macro and micro-nutritional patterns in a well-characterized cohort of adults with SCD and correlated the nutritional data with SCD severity, course, outcome, and health-related quality of life.
Material and Methods
Study design and study population
We conducted this prospective study in two major hospitals (Prince Sattam Bin Abdul Aziz University Hospital and King Khaled Hospital) in Kharj, Central region of Saudi Arabia, between November 2012 and January 2020. The study enrolled males and females aged =/> 18 years with HbSS genotype sickle cell disease who had no history of acute painful crisis or recent admission to the hospital or emergency department during at least four weeks preceding enrollment (steady-state). Exclusion criteria included hemoglobin genotypes other than HbSS, concomitant thalassemia, presence of active autoimmune disorders, hematologic or solid malignancy, severe hypertension, decompensated cardiac, liver, or kidney disease., current use of immunosuppressants or anticoagulant drugs, or refusal to provide full consent. Women who were pregnant at the time of screening were not enrolled; however, women who got pregnant during follow-up were encouraged to remain in the study. However, women who got pregnant during follow-up were encouraged to remain in the study. We also enrolled healthy age, gender, and province matched individuals control subjects.
All eligible patients and control subjects provided written informed consent before enrollment in the study and before performing study-related investigations. The institutional review boards (IRB) in each participating institution approved the research protocol, informed consent forms, and study procedures that have been conducted per the Good Clinical Practice guidelines and in conformity with the ethical guidelines of the Declaration of Helsinki.
Patients provided a detailed medical history, including past and family history, therapeutic history, and dietary information (48-hour dietary recall). Whenever possible, the investigators reviewed some patients’ health records during childhood. Enrolled patients had a physical examination and laboratory tests, including complete blood count (CBC), renal function tests (creatinine, BUN), liver functions (serum bilirubin, ALT, and AST, total and direct bilirubin, alkaline phosphatase), using standard techniques. Ferritin levels were measured by a human ferritin ELISA Kit (BioSource, San Diego, CA, USA) according to the manufacturer’s instructions. Thyroid-stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), growth hormone, testosterone, estrogen, and progesterone were measured using BioSource ELISA kits (San Diego, CA, USA) according to the manufacturer’s instructions.
Patients with gastrointestinal disorders had appropriate investigations for Helicobacter pylori (H.pylori) stools antigen, celiac disease (IgA TTG, and IgG-deamidated gliadin), lactose intolerance test, upper and lower gastrointestinal endoscopies, and biopsies when necessary. At study entry, patients had hepatitis B and C screening (Human hepatitis B ELISA Kit, and human hepatitis C ELISA kit, Biosource, kits (San Diego, CA, USA) according to the manufacturer’s instructions). Patients with positive serology had further confirmatory testing. Patients had baseline and annual abdominal ultrasound examinations, while patients with viral hepatitis and, or iron overload had transient elastography as previously described.25
We estimated the enrolled patients’ energy and protein intake, measured various micro-nutrients, and determined their nutritional status (subjective global assessment). According to baseline nutritional assessment, we classified patients into two groups. Group A included patients with no under-nutrition evidence (well-nourished; SGA category A and no micro-nutrient deficiencies. Group B comprised patients with macro-and micro-nutritional deficiencies.
Macro and micro-nutritional status assessments
a. Subjective global assessment (SGA)
The study utilized the subjective global assessment tool (SGA) (validated Arabic version) to assess the patients’ nutrition and some parameters of body composition.26 Briefly, SGA is a validated nutrition assessment tool that combines patient history, recent nutrient intake, weight alterations, gastrointestinal symptoms, functional capacity, and metabolic requirements. Physical examination includes evaluating somebody’s composition parameters such as fat, wasting of muscle, and water retention. The SGA assessment classifies the patients’ nutritional status into three categories: A (well-nourished), B (moderately malnourished), and C (severely malnourished).26
b. Micronutrients measurements
according to the manufacturer, Vitamin B12 and vitamin D were measured using Diazyme vitamin B12 and 25-OH vitamin D assay kits, respectively (Diazyme Laboratories, Inc., Poway, CA, USA)’s instructions. Plasma folate levels were determined with a commercial automatic electrochemical immuno-analyzer (Roche E170, Hoffman La Roche, Basel, Switzerland) and electrochemiluminescence immunoassay (ECLIA). We used standard procedures to measure calcium, sodium, potassium, zinc, magnesium, phosphorous.
Anthropometric measurements
At study entry and bi-annual follow-up visits, patients had anthropometric measurements with measurement of the weight, height, and BMI estimation (by dividing weight in kilograms by the square of height in meters). Based on the BMI patients’ measurements, patients with BMI values below 18.5, between 18.5–24.99, between 25.0 – 29.9, and above 30 were considered underweight, average weight, overweight, and obese, respectively.27 Other measurements included triceps, abdominal folds thickness, middle-upper arm circumference (MUAC), calf circumference (CC), waist circumference (WC), and hip circumference (HC) assessments. The waist-hip ratio (WHR) and the waist-circumference-to-height-ratio (WHtR) were calculated by dividing WC to hip circumference and height, respectively.28,29 The body fat % was measured by a Tanita TBF-400 Total Body Composition Analyzer (Tanita, Tokyo, Japan).
Assessment of SCD severity
Through the study, we used the “Sickle Cell Disease Severity Calculator” online tool available at: http://www.bu.edu/sicklecell/downloads/Projectsto assess SCD severity. This model predicts a 5-year mortality risk and assesses disease severity. This composite model includes several 25 clinical and laboratory variables such as age, gender, frequency of blood transfusion, systolic blood pressure, hemoglobin genotype, white blood cell count, reticulocyte and platelets count, clinical manifestations including pain, acute chest syndrome, priapism, sepsis, stroke, in addition to the laboratory data: bilirubin and LDH. The generated score is between 0.1 to 1 and stratifies disease severity into mild, intermediate, or high.13
Outcome measures
The study endpoint was a composite of admission to hospital with SCD related events that occurred during follow-up or death from all causes. Severe SCD constituted patients with severity scores 0.7 or more and patients who died during the study. Mild and intermediate SCD patients with severity scored 0.6 and less and survived the study.
Interventions
Patients received blood transfusion in acute hemolytic, painful vaso-occlusive crises or acute chest syndrome, stroke, or acute priapism. Some study patients received hydroxyurea (HU) before enrollment, and others initiated HU during the study, as previously indicated [30]. Patients with proven micronutrient or hormonal abnormalities detected during the study received the appropriate replacement therapies.
Health-related quality of life assessment
Patients completed the Arabic version of the Short form-36 Health Survey version 2 (SF-36v2)31 questionnaire at study entry, every six months, and in the occurrence of complications, The SF-36 questionnaire consists of eight scales yielding two summary measures: physical and mental health. The physical health measure includes four scales of physical functioning (10 items), role-physical (4 items), bodily pain (2 items), and general health (5 items). The mental health measure is composed of vitality (4 items), social functioning (2 items), role-emotional (3 items), and mental health (5 items).32 The investigators conducted the scoring according to the RAND health care instructions available at https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html.
Statistical analysis
Continuous variables were expressed as mean ± SD or median (range) as appropriate. Categorical variables were compared by Fisher’s exact test or Chi-square test as appropriate. We used Student’s t-test, Mann–Whitney U, Kruskal–Wallis tests, or analysis of variance (ANOVA) for comparing numerical variables. The incidence rate (person-time rate) is calculated by dividing the number of new events during follow-up by the sum of person-years of observation. Correlation between variables was performed by Pearson correlation for parametric and Spearman for non-parametric testing. Kaplan–Meier curves were generated to assess the association between malnutrition and the study outcomes (hospital admission due to severe SCD related complications or death). The attributable risk was calculated by subtracting the non-exposed group’s risk from the exposed group’s risk. To assess the impact of the various factors on the severity of SCD, we conducted the multivariable logistic regression analysis in which data were presented as ORs with 95% Cis and P values for the were two-sided. P<0.05 was considered statistically significant. We defined statistical significance as a P-value of less than 0.05. The statistical analysis was carried out using SPSS for Windows, version 22, and MedCalc Software Ostend, Belgium).
Results
Demographics and clinical presentations
Sixty-two SCD patients (34 males, 28 females, mean age 24.21±3.926; 95% CI: 23.21 to 25.21 years) fulfilled the inclusion criteria and provided informed consent to enroll in the study and perform the required investigations. Initially, we enrolled 62 control subjects to achieve a case/control ratio 1:1; however, only fifty age, gender-matched and province of origin healthy individuals (27 males and 23 females; mean age: 24.94± 4.01; 95% CI: 94.14 to 95.89) provided consent to join the study as a control group. The median follow-up for the entire cohort was 93 months (95% CI of the median: 92 to 94 months). At study entry, 20 patients had no macro-or micro-undernutrition (Group A), and 42 patients had under-nutrition (Group B). Table 1 summarizes the patients’ demographics, baseline clinical characteristics, and laboratory data. Although the participating centers were in the central region of KSA, 21 (33.87%), 18 (29.03%), 2 (3.23%), and 2 (3.23%) patients were initially from the Southern, Eastern, North, and Western KSA provinces respectively (Table 1). Forty-four (70.97%) patients reported parental consanguinity, and 20 patients (32.26%) reported that more than one family member had SCD. Enrolled patients presented with diverse clinical manifestations (Table 1). Significant differences in weight, height, and BMI existed between Group A and B patients. Hematologic parameters were comparable between the two patients’ groups. Abdominal (gastrointestinal) symptoms were significantly higher among undernourished patients (Table 1).
Table 1.
Demographics, baseline clinical features and laboratory data of enrolled subjects with sickle cell disease (SCD).
| Parameters | Group A (n=20) | Group B (n=42) | P-value | Control subjects N=50 |
P value (SCD vs. controls) |
|---|---|---|---|---|---|
|
| |||||
| Age (years); mean± SD | 24.25± 4.16 | 25.02± 3.59 | 0.456 | 26.32±5.37 | 0.179 |
|
| |||||
| Male:Female | 11:9 | 23:19 | 0.681 | 28: 22 | 0.731 |
|
| |||||
| Follow-up duration in months (mean±SD; 95% CI of the mean) | 93.26±2.10 (89.82 to 92.88) | 92.70±2.089 (88.38 to 92.46) | 0.329 | ||
|
| |||||
| Saudi province of origin; n (%) | |||||
|
| |||||
| North province | 2 (10) | 1 (2.38) | 0.195 | 2 (4) | 0.823 |
| Central province | 6 (30) | 13 (30.95) | 0.940 | 32 (64) | 0.002 |
| South province | 8 (40) | 22 (52.38) | 0.366 | 7 (14) | 0.0001 |
| Eastern province | 2 (10) | 5 (11.90) | 0.827 | 5 (10) | 0.864 |
| Western province | 2 (10) | 1 (2.38) | 0.195 | 4 (8) | 0.529 |
|
| |||||
| Symptoms and signs | |||||
|
| |||||
| Fatigue; n (%) | 16 (80) | 31 (73.81) | 0.598 | 3 (6) | |
|
| |||||
| Pallor; n (%) | 15 (75) | 28 (66.67) | 0.509 | 0 | |
|
| |||||
| Body pains; n (%) | 11 (55) | 23 (54.76) | 0.986 | 2 (4) | |
|
| |||||
| Anorexia/dyspepsia/nausea, vomiting; abdominal colic; n (%) | 8 (40) | 36 (85.71) | 0.0002** | 0 () | |
|
| |||||
| Diarrheal episodes; n (%) | 3 (15) | 20 (47.62) | 0.014* | 0 | |
|
| |||||
| Recent weight loss; n (%) | 3 (15) | 26 (61.90) | 0.0006 ** | 0 | |
|
| |||||
| Attacks of jaundice; n (%) | 5 (25) | 15 (35.71) | 0.403 | 0 | |
|
| |||||
| Fever episodes; n (%) | 5 (25) | 10 (23.81) | 0.919 | 0 | |
|
| |||||
| Skin lesions/hair loss | 5 (25) | 12 (28.57) | 0.770 | 1 (2) | <0.0001** |
|
| |||||
| Weigth (Kg) | 66.39 ± 7.68 | 60.57 ± 4.96 | 0.0007** | 69.84±19.75 | 0.022* |
|
| |||||
| Height (cm) | 159.87 ± 7.16 | 155.40 ± 4.13 | 0.0006** | 161.75±18.67 | 0.027* |
|
| |||||
| Body mass index (kg/m2) | 21.74±6.17 | 18.31±2.62 | 0.003** | 25.19±4.79 | <0.0001 |
|
| |||||
| Enlarged spleen; n (%) | 18 (90) | 20 (47.62) | 0.184 | 0 | |
|
| |||||
| Enlarged liver; n (%) | 5 (25) | 13 (38.24) | 0.316 | 0 | |
|
| |||||
| Comorbidities | |||||
Food intolerance; n (%)
|
2 (10) | 11 (26.19) | |||
| 1 (5) | 3 (7.14) | 0.147 | 0 | ||
| 1 (5) | 8 (19.05) | ||||
|
| |||||
| Inflammatory bowel disease (ulcerative colitis and Crohn’s disease) | 1(5) | 8 (19) | 0.146 | 0 | |
|
| |||||
| Hepatitis B (HBV) positive; n (%) | 5 (25) | 10 (23.81) | 0.919 | 0 | |
|
| |||||
| Hepatitis C (HCV) positive; n (%) | 0 | 1 (2.38) | 0.490 | 0 | |
|
| |||||
| Management | |||||
|
| |||||
| Hydroxyurea | 2 (10) | 5 (11.90) | 0.826 | NA | |
|
| |||||
| Blood transfusion (>3 times/year) | 1 (5) | 9 (21.43) | 0.103 | NA | |
|
| |||||
| History | |||||
|
| |||||
| Splenectomy prior enrollment; n (%) | 7 (35) | 12(60) | 0.068 | 0 | |
|
| |||||
| Cholecystectomy prior enrollment; n (%) | 5 (25) | 9 (21.43) | 0.755 | 0 | |
|
| |||||
| Family history | |||||
|
| |||||
| Parental consanguinty | 14 (70) | 32 (71.43) | 0.928 | 39 (78) | 0.509 |
|
| |||||
| Other family members with SCA/SCD | 4 (20) | 16 (38.09) | 0.158 | NA | |
|
| |||||
| Baseline hematological, biochemical and virologic data | |||||
|
| |||||
| Hemoglobin (g/dl); mean ±SD | 8.84 ± 2.63 | 7.49 ± 2.71 | 0.069 | 13.11 ± 3.33 | <0.0001 |
|
| |||||
| Ferritin levels (ng/mL); (Mean ± SD) | 78.26 ± 27.18 | 47.16 ± 25.37 | 0.301 | 167.83 ± 99.75 | <0.0001 |
|
| |||||
| Total bilirubin (mg/dL) (Mean ± SD) | 1.85± 1.87 | 2.97± 0.15 | 0.0003** | 0.97± 0.05 | <0.0001 |
|
| |||||
| ALT (U/L) (Mean ± SD) | 39.44 ± 12.48 | 52.37 ± 14.06 | 0.0009** | 25.61 ± 6.27 | <0.0001 |
| AST (U/L) (Mean ± SD) | 40.28 ± 11.25 | 50.53 ± 10.33 | 0.0008** | 26.38 ± 5.34 | |
|
| |||||
| Urea (mg/dl) (Mean ± SD) | 23.45 ± 19.82 | 36.17 ± 17.49 | 0.013* | 29.42 ± 8.65 | <0.0001 |
| Creatinin (mg/dL) (Mean ±SD) | 0.92 ± 0.43 | 1.06 ± 1.05 | 0.569 | 0.06 ± 0.03 | |
Group A: Well nourished SCD patients; Group B: SCD patients with macro or micro-undernutrition;: MCV-Mean cell volume, MCH Mean cell hemoglobin, MCHC-Mean cell hemoglobin concentration, AST: aspartate transaminase; ALT: alanine transaminase; WBC-White blood cells*109/l, -Platelets*109/l; reference values for ferritin: 12 to 300 ng/mL for males and 12 to 150 ng/mL for females.; TSH: Thyroid-stimulating hormone (normal range: 0.4 4 mU/l); ferritin reference:; growth hormone reference range: males: 0.5–10 ng/mL, females: 1–14 ng/mL testeteterone range: 270–1070 ng/dL; estradiol range: 30 to 400 pg/mL.
Thirteen patients (20.97%) had food intolerance (9 cases with celiac diseases and 4 cases with lactose intolerance). Ten patients with food intolerance did not comply with gluten-free or lactose-free diets and presented with bloating and diarrhea episodes. Fifteen patients (24.19%) had chronic hepatitis B (HBV), and one patient had chronic hepatitis C. Six patients with chronic viral hepatitis (37.5%) had liver stiffness scores exceeding 14 kPa with Metavit fibrosis scores of F3, suggestive of hepatic fibrosis with the expansion of most portal zones, marked bridging and occasional nodules. Five patients with chronic HBV also had iron overload. Patients received anti-viral treatment for both conditions (Table 1) with a virologic response in 11 (73.33%) and 1 (100%) patients with chronic HBV and HCV, respectively (data not shown).
Twenty-seven SCD patients (43.55%) had hypothyroidism (Table 1). Growth hormone and testosterone levels differed significantly between undernourished patients and control subjects (Supplementary table 2). Estradiol did not differ between well-nourished and undernourished patients.
Macro and micro-nutritional status and anthropometric assessments
Overall, SCD patients had significantly lower energy and protein intake than control subjects, and Group B patients showed significantly lower levels than patients in Group A (Table 2).
Table 2.
Macro and micro-nutritional status in study patients and control subjects.
| Parameter | Group A (n=20) | Group B (n=42) | P value: Group A vs. B | Control subjects (n=50) | P-value Group A, B vs. Controls |
|---|---|---|---|---|---|
|
| |||||
| Daily energy intake (kcal/day) Mean±SD |
2012.036 ± 99.098 | 1905.177 ± 66.917 | 0.0001** | 2260.94±229.21 | - Group A& B vs Controls: < 0.0001** |
|
| |||||
| Daily protein intake (g) Mean±SD |
90.89± 16.23 | 79.29±13.99 | 0.005** | 148.66±32.15 | |
|
| |||||
| Subjective global assessment of the nutritional status (SGA) | |||||
|
| |||||
| Normally nourished (SGA rating: A): n (%) | 20 (100) | 0 | < 0.0001** | 50 (100) | -Group B vs Controls: < 0.0001** |
|
| |||||
| Moderately under-nourished (SGA rating: B) | 0 | 38 (83.33) | < 0.0001** | 0 | |
|
| |||||
| Severely under-nourished (SGA rating:C) | 0 | 4 (9.52) | < 0.0001** | 0 | |
|
| |||||
| Basal metabolic rate (BMR) | |||||
|
| |||||
| -Average BMR; n (%) | 13 (65) | 20 (47.63) | 0.203 | 47 (94) | Group A vs. Controls: 0.002 Group B vs. Controls: <0.0001 |
| -Low BMR; n (%) | 2 (10) | 9 (21.43) | 0.275 | 2 (4) | |
| -High BMR; n (%) | 5 (25) | 13 (30.95) | 0.629 | 1 (2) | |
|
| |||||
| #Vitamin B12 (pg/ml); mean ± SD | 176. 20± 142.37 | 155. 45± 136.23 | 0.578 | 798.69±192.52 | - Group A & B vs. controls: < 0.0001 |
|
| |||||
| $ 25-OH-vitamin D (ng/mL); mean ± SD | 20.16± 3.148 | 14.67±3.3369 | < 0.0001** | 28.93± 8.71 | - Group A & B vs. controls: < 0.0001** |
|
| |||||
| &Plasma folate level (ng/mL); mean ± SD | 15.27±5.48 | 14.38±4.73 | 0.513 | 16.36±5.16 | -Group A vs. controls: 0.449 - Group B vs. controls: 0.070 |
|
| |||||
| Serum zinc ( mg/dl); (Mean ± SD) | 78.26 ± 27.18 | 53.36± 15.37 | <0.0001 ** | 124.34± 49.27 | -Group A& B vs. controls: <0.0001** -Group A vs. controls: 0.471 |
|
| |||||
| Calcium (mg/dl); (Mean ± SD) | 9.410±0.641 | 9.296±0.596 | 0.092 | 9.535±0.632 | - Group B vs. controls: 0.0670 |
|
| |||||
| Ferritin levels at steady state(ng\dl); (Mean ± SD) | 138.26 ± 27.18 | 94.16 ± 15.37 | 0.013* | 149.37 ± 67.63 | -Group A& B vs. controls: <0.0001 |
Group A: SCD patients without macro or micro-undernutrition; Group B: SCD patients with macro or micro-undernutrition; SGA: Subjective global assessment; Reference range of: Zinc: 60–120 μg/dL.
25-OH-vitamin D: 20 to 60 ng/mL Vitamin B12: 190 and 950 pg/mL,
Folate: 2–20 ng/mL;
Significant,
Highly significant.
Among Group B patients, 38 (83.33%) and 4 (9.52%) patients had moderate and severe undernutrition (SGA rating B and C), respectively (Table 2). The BMR was within average (−15%–+5% in 43 (69.35) patients, below average in 7 (11.29), and above average in 12 (19.35) patients with a significant difference between patient groups and control subjects (Table 2). In most under-nourished patients, sub-optimal food intake resulted from gastrointestinal complaints, including anorexia, dyspepsia, nausea, vomiting, diarrhea, and food intolerance frequent hospital admissions due to VOC attacks (data not shown).
At baseline, patients showed significantly low serum zinc, vitamin B12, and vitamin D levels than control subjects (P<0.0001). Within SCD patients, zinc and vitamin D levels were significantly lower in Group B patients compared to Group A (P= <0.0001 for both) (Table 2). Patients with zinc deficiency suffered from reduced appetite and diarrhea, which further deteriorated the undernutrition in such patients. Through the study, patients received vitamin B, vitamin D, and zinc supplementation with subsequent improvement. However, a decline in vitamins B, D, and zinc levels occurred with the onset of vaso-occlusive-related complications (data not shown). Folate and calcium levels did not differ significantly between patients and control subjects or well-nourished and undernourished patients (Table 2).
At study entry and through follow-up, anthropometric measurements were significantly lower in SCD patients than control subjects (Supplementary Table 1). The BMI, MUAC, and body fat values were lower in Group B than Group A patients (Table 1 and Supplementary Table 1). Males with SCD tend to have shorter stature (defined as s a standing height more than two standard deviations (SDs) below the mean (or below the 2.5 percentile for sex) compared to control subjects (Table 1).
SCD course, complications, survival, and outcomes during follow-up
During the year preceding enrollment, Group B patients had more frequent VOC episodes compared to Group A patients. At study entry, the baseline SCD severity scores were significantly higher in under-nourished (Group B) patients compared to well-nourished individuals (Group A) (Table 3). During follow-up, 42 undernourished and 4 well-nourished patients (74.19%) developed one or more vaso-occlusive pain crises and other SCD related complications that required hospitalization or emergency management (Table 3). The major events that required hospitalization were vaso-occlusive pain crises, acute chest syndrome, stroke, pulmonary hypertension, cardiomyopathy, acute cholecystitis, acute sickle hepatic crisis, and priapism (Table 3). Two patients in Group B developed acute cholestasis with elevated hepatic transaminases (3 times upper normal) during an acute VOC pain crisis. Renal involvement occurred in 21 (33.87%) SCD patients in the form of proteinuria, microalbuminuria (30–300 mg/g creatinine) and macroalbuminuria (>300 mg/g creatinine), in 10/21 (47.62%), 7 (33.33%) and 3 (14.29%) SCD patients respectively (Table 3).
Table 3.
Severity scores, vaso-occlusive crises, and complications before enrollment and during follow-up.
| Parameter | SCD patients with no macro or micro-nutrient deficiencies (n=20) | Macro or micro-nutrient deficiencies (n=42) | P-value |
|---|---|---|---|
|
| |||
| Number of patients who had vaso-occlusive painful episodes that required hospitalization or emergency treatment in the year prior enrollment; n (%) | |||
|
| |||
| No episodes | 18 (90) | 2 (4.76) | <0.0001** |
|
| |||
| 1–2 episodes | 2 (10) | 18 (42.86) | 0.001** |
|
| |||
| 3–5 episodes | 0 | 20 (47.62) | 0.0002** |
|
| |||
| 3–5 episodes | 0 | 20 (47.62) | 0.0002** |
|
| |||
| More than 5 episodes | 0 | 4 (9.52) | 0.157 |
|
| |||
| Baseline SCD severity score; mean±SD | 0.22± 0.01 | 0.41±0.025 | <0.0001** |
|
| |||
| Events during follow-up | |||
|
| |||
| Acute events | |||
|
| |||
| Patients who developed acute vaso-occlusive (VOC) pain crises; n (%) | 9 (45) | 42(100) | <0.0001** |
|
| |||
| 1–2 VOC attacks per person during the follow-up period; n (%) | 8 (40) | 8 (19.05) | 0.079 |
| 3–5 VOC attacks per person during the follow-up period; n (%) | 1 (5) | 20 (47.62) | 0.0009** |
| >5 VOC attacks per person during the follow-up period; n (%) | 0 | 14 (33.33) | 0.0038** |
|
| |||
| Acute chest syndrome; number of patients (%) | 1 (5) | 3 (7.14) | 0.7647 |
|
| |||
| Acute calcular cholecystitis; number of patients (%) | 3 (15) | 7 (16.67) | 0.8435 |
|
| |||
| Stroke; number of patients (%) | 0 | 3 (7.14) | 0.4376 |
|
| |||
| Acute sickle cell hepatic crises; number of patients (%) | 0 | 2 (4.76) | 0.3129 |
|
| |||
| Pneumonia; number of patients (%) | 1 (5) | 12 (28.6) | 0.03* |
|
| |||
| Myocardial infarction; number of patients (%) | 0 | 2 (4.76) | 0.3231 |
|
| |||
| Pulmonary embolism; number of patients (%) | 0 | 2 (4.76) | 0.3231 |
|
| |||
| Priapism; number of patients (%) | 1 (5) | 3 (7.14) | 0.4376 |
|
| |||
| Chronic events | |||
|
| |||
| #Choleletiasis; number of patients (%) | 12 (60) | 27 (64.29) | 0.7627 |
|
| |||
| Leg ulcers; number of patients (%) | 5 (25) | 13 (30.95) | 0.6295 |
|
| |||
| Renal complications: number of patients (%) | 1 (5) | 11 (26.2) | |
| - Proteinuria, | 0 | 3 | 0.05* |
| - Microalbuminuria | 1 | 6 | |
| - Macroalbuminuria | 0 | 2 | |
|
| |||
| Cardiomyopathy, heart failure: number of patients (%) | 1 (5) | 5 (11.9) | 0.3888 |
|
| |||
| Recurrent infections (=/>3 infections/year) ; number of patients (%) | 7 (35) | 29 (69.05) | 0.012* |
|
| |||
| Liver fibrosis/cirrhosis: number of patients (%) | 1 (5) | 7 (16.67) | 0.195 |
|
| |||
| Mean SCD severity score during follow-up; mean±SD | 0.29± 0.081 | 0.52±0.073 | <0.0001** |
|
| |||
| Incidence rate of SCD-related events that required hospitalization (cases per person-year); (95% CI) | 0.25 (0.179 to 0.340) | 0.516 (0.4399 to 0.6006) | 0.001** |
|
| |||
| Death, total (n;%) | 0 | 7 (16.67) | |
| - SCD-related | 0 | 6 (14.12) | 0. 0.05* |
| - Not SCD-related | 0 | 1 (2.94) | |
|
| |||
| Death incidence rate (cases per 100 person-year); (95% CI); | 0 (0 to 0.023) | 2.41 (0.9 to 4.97) | 0.049* |
Some patients developed more than one acute or chronic complication during follow-up.
Patients developed cholelithiasis before or after enrollment in the stud. SCD: Sickle cell disease. Sickle Cell Disease severity determined using the online calculator tool available at http://www.bu.edu/sicklecell/downloads/Projectsto assess SCD severity. The generated score is between 0.1 to 1 and stratifies disease severity into mild, intermediate, or high.13 The incidence rate calculation as follows: number of new events (SCD related hospitalizations or death total person-time of observation while at risk during the study.
Significant,
Highly significant.
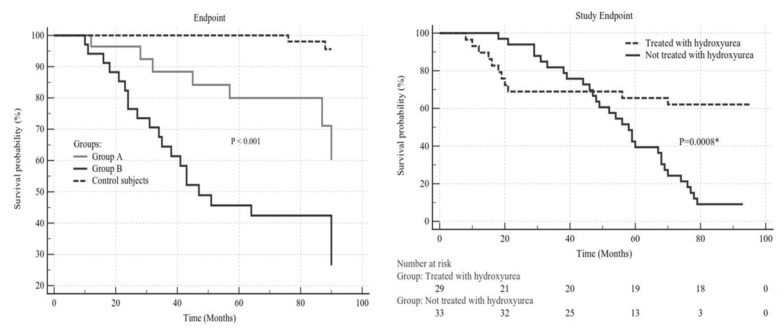
During follow-up, seven patients (11.29%) died in Group B, and no mortalities occurred either in Group A or the control group. The relative risk was 14.43 (95% CI: 0.846 to 46.2664; P= 0.05). The causes of mortality were myocardial infarction (2 patients), stroke (2 patients), pulmonary embolism (one patient), acute chest syndrome (one patient), and a patient who died in a traffic accident (Table 3; Figure 1a).
Figure 1.
Figure 1A. A Kaplan Meier curve showing the length of time from enrolment until the study’s occurrence endpoint (admission to hospital with SCD related event or death) in study groups and control subjects. There was a significant difference in times to event between the well-nourished patients (SGA: A) with no micro-nutrient deficiencies and patients with macro-(SGA: B or C) and micro-nutrient deficiencies (log-rank test P=0.001). Figure 1B: A Kaplan Meier curve showing the length of time from hydroxyurea therapy until the study’s occurrence endpoint (admission to hospital with SCD related event or death) in treated and untreated study groups. There was a significant difference in times to event and survival times between treated and untreated patients ((log-rank test P=0.0008).
Associations between nutritional parameters and SCD severity and outcome
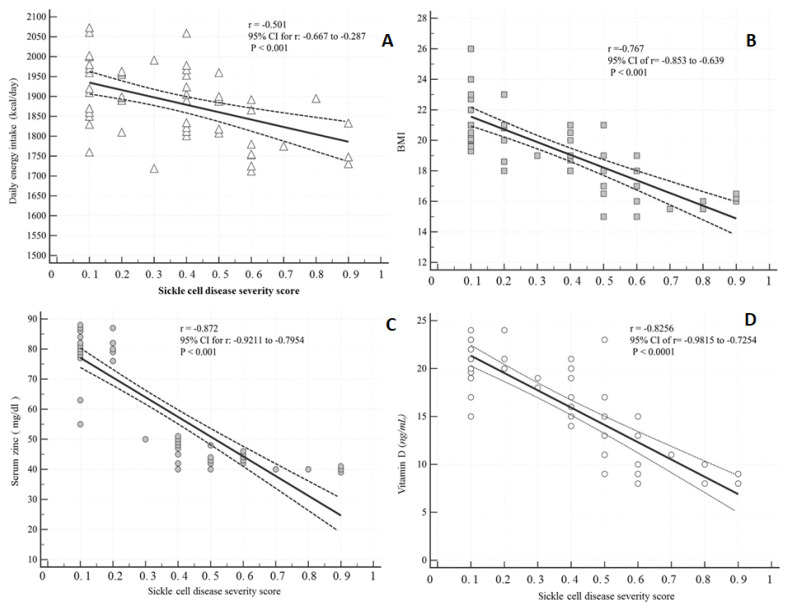
A significant inverse correlation existed between each of daily energy intake, BMI, serum zinc levels, vitamin D levels, and SCD severity scores (P<0.001) (Figure 2a,b,c,d). We calculated the attributable risk and attributable risk percent to estimate how much of this study outcome was attributable to undernutrition. The attributable risk was 0.598, and the attributable risk percent was 88.28%, suggesting that malnutrition may be responsible for 88% of the severe outcomes of SCD. Multivariate logistic regression analysis showed that being a male with energy intake less than 1600, SGA scores B or C, a BMI less than 18, hemoglobin levels less than 6 gm/dl, vitamin D levels less than 16 ng/mL, and zinc levels less than 60 ng/dl were independent risk factors for a more severe SCD score and worse outcome (Table 4).
Figure 2.
Correlation between nutritional variables and SCD severity index. Daily.
Figure 2a: Energy intake with SCD severity scores: A significant inverse correlation between daily energy intake (kcal/day) was negatively correlated with SCD severity score (correlation coefficient=−0.501; P=0.001). Dotted lines represent 95% CI.
Figure 2b: The relationship between BMI and SCD severity: A significant negative correlation existed between BMI and SCD severity score (correlation coefficient= − 0.767; P =0.001). Dotted lines represent 95% CI.
Figure 2c: The relationship between vitamin D and SCD severity: A significant negative correlation existed between vitamin D levels D (ng/mL) and SCD severity score (correlation coefficient= − 0.826; P < 0.001). Dotted lines represent 95% CI.
Figure 2d: The relationship between serum zinc and SCD severity: A significant negative correlation existed between serum zinc levels (ng/mL) and SCD severity score (correlation coefficient= − 0.872; P < 0.001). Dotted lines represent 95% CI.
Table 4.
Risk factors associated with severe sickle cell disease.
| Predictor | Regression coefficient | Chi-square | OR (95% CI) | P | |
|---|---|---|---|---|---|
| Referant Group (Mild or moderate SCD, survivors | Severe SCD and non-survivors | ||||
| Intercept | −5.785 | 21.694 | 0.001 | ||
| Male | 1.326 | 5.185 | 1 | 3.848 (1.274–10.254) | 0.02 |
| Age ( years) | 0.579 | 1.893 | 1 | 1.686 (0.478, 4.316) | 0.195 |
| Energy intake < 1600 kcal per day >1600Kcal/day |
0.073 | 3.972 | 1 | 1.072 (1.005, 1.153) | 0.0341 |
| Hemoglobin <6gm/dl >6gm/dl |
0.536 | 1.126 | 1 | 1.729 (0.759, 4.135) | 0.393 |
| SGA score - B,C -A |
2.174 | 9.630 | 1 | 8.736 (2.548, 17.385) | 0.004 |
| BMI <17 >17 |
3.067 | 1.521 | 1 | 0.543 (0.361, 0.818) | 0.0034 |
|
Vitamin D < 16 ng/mL >16 mg/mL |
1. 841 | 6.543 | 1 | 2.417 (1.463, 4.140) | 0.0007 |
| Zinc < 60 mg/dl) |
3.482 | 3.419 | 1 | 5.061 (1.462, 16.471) | 0.0087 |
Vitamin B12
|
1.632 | 5.651 | 1 | 4.145 (1.849 – 9.291) | 0.0006 |
Sickle Cell Disease severity determined using the online calculator tool available at http://www.bu.edu/sicklecell/downloads/Projectsto assess SCD severity. The generated score is between 0.1 to 1 and stratifies disease severity into mild, intermediate, or high.13 Patients with severe SCD (patients with high severity scores (0.7–1) and patients who died during the study) were compared to patients with mild and moderate severity scores and survived the study. BMI, body mass index; 95% CI, 95% confidence interval.; OR, odds ratio.
Influence of nutritional supplementation and management of gastrointestinal complaints on SCD manifestations
During follow-up, patients with energy-protein and micro-undernutrition had a nutritional consultation with correction of energy deficit and vitamin D and zinc supplementation, which was followed by improved symptoms and signs. However, VOC crises were associated with a decline in vitamin D and zinc in some patients (Supplementary figure 1). Patients with gastrointestinal disorders such as Helicobacter pylori infection, inflammatory bowel disease received proper pharmacologic therapy, and those with celiac disease and lactose intolerance complied with gluten and dairy-free diets resulting in improvement of food intake amelioration of macro-and micro-nutritional parameters, and improvement of body composition. (Figure 3).
The outcome of disease-modifying measures
Seven patients (2 in group A and 5 in group B) were receiving hydroxyurea before enrollment, and 20 patients initiated HU therapy during the study (Supplementary Table 2). Hydroxyurea therapy was associated with a significant reduction in VOC episodes’ frequency and improvement in the SCD severity scores. The decrease in SCD severity resulted in a tangible enhancement in macro and micronutrition (Figure 2b and supplementary table 2).
Ten patients (one in group A and 9 in group B) received three or more blood transfusions in the year before study entry (Table 1). Three (4.84%) patients who received =/> three transfusions per year due to repeated complications developed iron overload after (Table 3) (Figure 3c).
Health-related quality of life assessment
Table 5 demonstrates the mean ± SD scores of SF-36 in well-nourished (Group A), undernourished SCD patients (Group B), and control subjects. Compared to controls, SCD patients had inferior self-reported quality of life, with a significant decrease in the total SF-26 scores and subdomains. Through follow-up, improving the patients’ nutrition and supplementation of zinc and vitamin D significantly improved the HRQoL scores (data not shown).
Table 5.
Means (SD) of baseline SF-361 quality of life scores in SCD patients without and with macro and micro nutritional deficiencies versus control subjects.
| Scores (norm) | SCD patients with no macro or micro-nutrient deficiencies (n=20) | SCD patients with macro or micro-nutrient deficiencies (n=42) | P-value | Control subjects (n=50) | P value between SCD patients and controls |
|---|---|---|---|---|---|
| PF | 84.05 ± 2.81 | 80.50 ± 3.19 | <0.0001 | 90.10 ± 2.40 | <0.0001** |
| RP | 88.21± 1.71 | 86.83 ± 1.34 | 0.0013 | 90.48 ± 3.4 | 0.0008 |
| BP | 82.13 ± 2.42 | 80.21 ±2.25 | <0.0001 | 84.63± 3.36 | 0.0002 |
| GH | 52.89 ± 2.37 | 50.25± 1.75 | <0.0001 | 54.24± 3.11 | 0.0377* |
| VT | 55.34 ± 2.33 | 53.21 ± 1.56 | <0.0001 | 59.35 ± 3.617 | 0.0001** |
| SF | 88.29 ± 2.18 | 86.83 ± 1.52 | <0.0001 | 91.47 ± 3.9 | <0.0001** |
| RE | 83.97 ± 3.31 | 81.83 ± 3.76 | 0.006 | 88.53 ± 8.56 | <0.0001** |
| MH | 72.09 ± 3.18 | 71.79 ± 2.67 | 0.058 | 72.10 ± 4.3 | 0.3112 |
| PCS | 43.74 ± 1.54 | 41.04± 1.73 | <0.0001 | 47.81 ± 2.7 | <0.0001** |
| MCS | 49.21 ± 1.72 | 49.01 ± 1.82 | 0.062 | 50.07 ± 1.11 | 0.0255 |
SF-36, short-form quality of life score with 36 questions. HRQoL: health- related quality of life. AC, activity; BP, bodily pain; EF, emotional function; FA, fatigue; GH, general health; MCS, Mental Component Summary Score; MH, mental health; PCS, Physical Component Summary Score; PF, physical functioning; RE, Role Emotional; RP, role physical; SF, social functioning; SS, systemic symptoms; VT, vitality; WO, worry.
Significant difference between the study groups (P<0.05).
Highly significant difference between the two study groups (P<0.01, 0.001).
Significant differences existed between patients with SCD and control subjects as well as well-nourished and undernourished SCD patients in all SF-36v2 domains except MH and MCs.
Discussion
Due to the improvement in the diagnosis and management of SCD, the survival rates of children with SCD have increased, and SCD is currently a chronic disease that causes considerable morbidity and mortality in adults.1,33,34 The impact of nutrition on the course and severity of SCD is not clarified; therefore, this longitudinal study enrolled and prospectively followed a well-characterized cohort of adult patients in steady-state SCD. The current study showed that a considerable percentage of the enrolled patients suffered from degrees of macro-and micronutrient deficiencies, which contribute to increased SCD severity, more complications, worse prognosis, and low quality of life.
The malnourished study group’s childhood medical records showed that those patients had body composition abnormalities, inadequate nutrition, and endocrinal disturbances since childhood that persisted into adulthood; thus, our results lend further credence to previous studies on pediatric cohorts.33,34 The malnutrition in this cohort was not due to food deprivation or shortage resulting from financial constraints since the economic status and household income did not differ significantly between the two SCD patients and control subjects. The etiology of the quantitative and qualitative malnutrition observed in a subset of this study’s SCD patients is multifactorial, resulting from lack of intake or uptake of macro or micronutrients triggered by SCD increased nutritional demands, concomitant chronic gastrointestinal diseases and infections, socio-demographic and lifestyle factors. Before enrollment and follow-up, most SCD study patients had frequent hospitalizations due to vaso-occlusive crises and SCD-related complications, including infections. As shown by several reports,35 hospitalized patients show a high malnutrition rate; however, this was not the sole cause of inadequate nutrition in this study. The study demonstrated that several SCD patients suffered from chronic gastrointestinal and hepatic disorders such as gastroesophageal reflux, IBD, celiac disease, and chronic viral hepatitis, which result in malnutrition due to malabsorption, altered nutrient metabolism, hypermetabolism, and anorexia.36,37,38 In the current study, the frequency of CD and IBD among the SCD was higher than in the control group and in the general population;39,40 furthermore, some patients had more than one family member suffering from concomitant SCD and either celiac or IBD. The high frequency of celiac disease and inflammatory bowel disease among SCD malnourished was intriguing, and to our knowledge, has not been reported before. Consanguinity, which is frequent in the Kingdom of Saudi Arabia, may play a role in such association since the three disorders, SCD, celiac disease, and IBD, have genetic determinants. The potential association of SCD with either CD or IBD requires further studies to investigate if such associations exist in other patients with other ethnic backgrounds.
In agreement with previous reports on pediatric cohorts,41,42,43 this study demonstrated that adults with SCD had deficiencies of zinc and vitamins B12 and D that contributed to the severity of SCD. Vitamin D deficiency is highly prevalent in Saudi Arabia due to decreased sun exposure because of the hot climate and traditional wear, covering the entire body.41 The large-scale economic growth and social development in KSA were associated with alterations in the dietary patterns and food choices with increased consumption of fast-foods that lack important nutritive constituents resulting in nutrient deficiencies. The concomitant SCD and H.pylori infection or celiac disease or IBD observed in this study played a role in micronutrient malabsorption. In the current study, SCD patients’ clinical manifestations and health-related quality of life significantly improved after personalized micronutrient integration, further supporting the findings of studies,44,45 which demonstrated early recognition of nutritional insufficiencies and nutrient supplementation is crucial for improving SCD outcomes not only in children but also in adult patients.
The present study has several strengths, including its prospective design, which enabled us to longitudinally assess the clinical, nutritional, and endocrinal parameters complications and health-assess related quality of life and outcome of the disease over eight years. The study provided insight on the etiology of malnutrition in SCD patients and the impact of integrating nutritional management into the SCD standard of care to improve the disease outcomes. Nevertheless, the study also has limitations. This study enrolled Saudi patients and control subjects without including other ethnicities. Given that disorders such as vitamin D deficiency and hypothyroidism are frequent in the Saudi population, we could not specify the actual incidence and clinical implications of such disorders on SCD. The study enrolled a relatively young population (median of 25 years) and followed them for almost eight years; however, it is crucial to conduct more longitudinal studies to investigate the effect of aging on SCD progression rates, morbidities, and mortality rates. Initially, we attempted to enroll 62 matched healthy control subjects to achieved a case-control ratio of 1:1. However, twelve control subjects were excluded due to the failure to provide consent to join the study or non-compliance to clinical visits.
Conclusions
Our results show that adults with sickle cell disease have multifactorial macro and micro-malnutrition, which are associated with severe disease, increased hospital admissions, and lower HRQoL. Integrating the diagnosis and correction of macro and micronutrient deficiencies into the standard management of SCD is critical for improving clinical outcomes and the patient’s quality of life.
Supplementary Files
Supplementary Table 1.
Anthropometric measurements in SCD patients and control subjects.
| Parameter | Group A (n=20) | Group B (n=42) | P-value Group A vs B |
Control subjects (n=50) | P-value Group A &B vs. Controls: |
|---|---|---|---|---|---|
| Middle upper arm circumference (MUAC) (cm) | 21.85±1.73 | 19.65±1.03 | <0.0001** | 23.97±2.95 | Group A & B vs. Controls <0.0001** |
| Triceps skinfold thickness (TSK) (mm) | 6.73 ±3.06 | 5.67 ±2.95 | 0.196 | 8.37 ±4.39 | Group A vs. Controls: 0.084 Group B vs. Controls:0.0024** |
| Abdominal skinfold (mm) | 14.48±3.5 | 12.97±2.1 | 0.038 | 17.65±3.34 | Group A vs. Controls: 0.0003 Group B vs. Controls: <0.0001** |
| Waist circumference (WC) (cm) | 70.43 ±5.56 | 68.36±3.27 | 0.074 | 77.53±6.04 | Group A & B vs. Controls <0.0001** |
| Hip Circumference (HC) (cm.) | 80.14 ± 7.56 | 78.36± 3.27 | 0.074 | 84.73 ±9.38 | Group B vs. Controls: 0.035 Group A & B vs. Controls: 0.0003 |
| Body Fat (%) | |||||
| Low fat % (< 20% ); n (%) | 4(20) | 21 (50) | 0.026 | 1 (2) | Group B vs. Controls: 0.035 Group A & B vs. Controls: <0.0001 |
| Normal fat % (21–33%); n (%) | 16 (80) | 21 (50) | 0.026 | 45 (90) | Group A vs. Controls: 0.124 Group B vs Controls: 0.003 |
| Over fat% (34–39%); n (%) | 0 | 0 | 4 (28) | Group A & B vs. Controls 0.002 | |
| Obese (> 39) ; n (%)(82.14) | 0 | 0 | 0 | ||
Supplementary Table 2.
Parameters of patients treated with hydroxyurea versus those not treated.
| Parameter | Patients receiving HU (n=27) | Patients not receiving HU (n=35) | P-value |
|---|---|---|---|
|
| |||
| Hemoglobin (g/dl) ) mean ± SD | 9.074± 0.569 | 8.011±0.698 | <0.0001 |
|
| |||
| Ferritin levels at steady state(ng\dl); (Mean ± SD) | 171.89±54.48 | 152.51±51.63 | 0.158 |
|
| |||
| Energy intake (kcal/day); (Mean ± SD) | 1889.953±104.726 | 1724.158±92.551 | < 0.0001 |
|
| |||
| Daily protein intake (g); mean ± SD | 50.42±13.48 | 46.16±11.94 | 0.192 |
|
| |||
| Plasma folate level (ng/mL); mean ± SD | 14.86±2.98 | 13.28±3.11 | 0.048* |
|
| |||
| Serum zinc ( mg/dl ; mean ± SD | 70.68±12.59 | 61.65±14.02 | 0.011* |
|
| |||
| Vitamin B12 (pg/ml) ; mean ± SD | 339.894±84.474 | 287.651±82.173 | 0.017* |
|
| |||
| 25-OH-vitamin D (ng/mL); mean ± SD | 20.94±4.82 | 16.16±3.21 | < 0.0001** |
|
| |||
| - Growth hormone (ng/ml); mean±SD | 6.79± 2.12 | 4.24±2.52 | 0.402 |
|
| |||
| - Hypothyroid, n (%) | 5 (25) | 17 (40.48). | 0.223 |
| - Euothyroid, n (%) | 10 (50) | 14 (33.33) | 0.21 |
| - Hyperthyroid; n (%) | 5 (25) | 11 (26.19) | 0.921 |
|
| |||
| - Testesterone (ng/dL) (in men); mean ±SD | 656.12±205.84 | 603.91±185.49 | 0.321 |
|
| |||
| Estradiol (pg/mL) - (in women) |
200.29±66.72 | 189.68±71.53 | 0.579 |
|
| |||
| Mean number of SCD-related crises that needed hospitalization/person/during the entire follow-up | 4.33±1.65 | 8.76±2.44 | <0.0001** |
|
| |||
| Incidence rate of SCD-related events that required hospitalization (cases per person-year); (95% CI); | 0.328 (0.258 to 0.410) | 0.508 (0.425 to 0.601) | 0.0021** |
|
| |||
| Mean SCD severity score during follow-up | 0.215±0.116 | 0.440±0.177 | < 0.0001** |
Macro and micronutrient levels before and after supplementation and during VOC crises. A significant improvement in nutrients was observed between baseline levels and after supplementation. During crises, the level of nutrients declined though it was higher than baseline levels.
Acknowledgments
The authors like to thank the Deanship of Scientific Research, Prince Sattam Bin Abdul Aziz University, for supporting the study. We would also like to thank Dr. Maysa Moustafa for her assistance in conducting hormonal assays.
Footnotes
Competing interests: The authors declare no conflict of Interest.
References
- 1.Piel FB, Steinberg MH, Rees DC. Sickle Cell Disease. N Engl J Med. 2017 Apr;376(16):1561–1573. doi: 10.1056/NEJMra1510865. [DOI] [PubMed] [Google Scholar]
- 2.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86:480–487. doi: 10.2471/BLT.06.036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macharia AW, Mochamah G, Uygoga S, Ndia CM, et al. The clinical epidemiology of sickle cell anemia In Africa. Am J Hematol. 2018 Mar;93(3):363–370. doi: 10.1002/ajh.24986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hassell KL. Population estimates of sickle cell disease in the US. Am J Prev Med. 2010;38(4 suppl):S512–S521. doi: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Piel FB, Talem AJ, Huang Z, Gupta S, Williams TN, Weatherall DJ. Global migration and the changing distribution of sickle haemoglobin: a quantitative study of temporal trends between 1960 and 2000. Lancet Glob Health. 2014 Feb;2(2):e80–e89. doi: 10.1016/S2214-109X(13)70150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elsayid Mohieldin, Al-Shehri Mohammed Jahman, Alkulaibi Yasser Abdullah, Alanazi Abdullah, Qureshi Shoeb. Frequency distribution of sickle cell anemia, sickle cell trait and sickle/beta-thalassemia among anemic patients in Saudi Arabia. J Nat Sci Biol Med. 2015 Aug;6(Suppl 1):S85–S88. doi: 10.4103/0976-9668.166093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jastaniah W. Epidemiology of sickle cell disease in Saudi Arabia. Ann Saudi Med. 2011 May-Jun;31(3):289–293. doi: 10.5144/0256-4947.2011.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sundd P, Gladwin MT, Novelli EM. Pathophysiology of sickle cell disease. Annu Rev Pathol. 2019 Jan 24;14:263–292. doi: 10.1146/annurev-pathmechdis-012418-012838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manwani D, Frenette PS. Vaso-occlusion in sickle cell disease: Pathophysiology and novel targeted therapies. Blood. 2013 Dec 5;122(24):3892–8. doi: 10.1182/blood-2013-05-498311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn CT. Clinical severity in sickle cell disease: The challenges of definition and prognostication. Exp Biol Med. 2016 Apr;241(7):679–88. doi: 10.1177/1535370216640385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. acute care utilization and re-hospitalizations for sickle cell disease. JAMA. 2010;303:1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 12.Miller ST, Sleeper LA, Pegelow CH, Enos LE, Wang WC, Weiner SJ, Wethers DL, Smith J, Kinney TR. Prediction of adverse outcomes in children with sickle cell disease. N Engl J Med. 2000;342:83–9. doi: 10.1056/NEJM200001133420203. [DOI] [PubMed] [Google Scholar]
- 13.Sebastiani P, Nolan VG, Baldwin CT, Abad-Grau MM, Wang L, Adewoye AH, Lillian C, McMahon, Farrer L, Taylor J, Kato GJ, Gladwin MT, Steinberg MH. A network model to predict the risk of death in sickle cell disease. Blood. 2007 Oct 1;110(7):2727–35. doi: 10.1182/blood-2007-04-084921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burke L, Hobart JC, Fox C, Lehrer-Graiwer J, Bridges K, Kraus M, Rames F. The 10-Item sickle cell disease severity measure (SCDSM-10): A novel measure of daily SCD symptom severity developed to assess benefit of GBT440, an experimental HbS polymerization inhibitor. Blood. 2016;128(22):4760. doi: 10.1182/blood.V128.22.4760.4760. [DOI] [Google Scholar]
- 15.Cameron BF, Christian E, Lobel JS, Gaston MH. Evaluation of clinical severity in sickle cell disease. J Natl Med Assoc. 1983 May;75(5):483–7.13. [PMC free article] [PubMed] [Google Scholar]
- 16.Day SW. Development and evaluation of a sickle cell assessment instrument. Pediatr Nurs. 2004 Nov;30(6):451–8. [PubMed] [Google Scholar]
- 17.Adekile A, Kutlar F, McKie K, Addington A, Elam D, Holley L, Clair B, Kutlar A. The influence of uridine diphosphate glucuronosyl transferase 1A promoter polymorphisms, beta-globin gene haplotype, co-inherited alpha-thalassemia trait and Hb F on steady-state serum bilirubin levels in sickle cell anemia. Eur J Haematol. 2005;75:150–5. doi: 10.1111/j.1600-0609.2005.00477.x. [DOI] [PubMed] [Google Scholar]
- 18.Miller ST, Milton J, Steinberg MH. G6PD deficiency and stroke in the CSSCD. Am J Hematol. 2011;86:331–331. doi: 10.1002/ajh.21958. [DOI] [PubMed] [Google Scholar]
- 19.Piel FB, Tewari S, Brousse V, Analitis A, Font A, Menzel S, Chakravorty S, Thein SL, Inusa B, Telfer P, de Montalembert M, Fuller GW, Katsouyanni K, Rees DC. Associations between environmental factors and hospital admissions for sickle cell disease. Haematologica. 2017 Apr;102(4):666–675. doi: 10.3324/haematol.2016.154245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mekontso Dessap A, Contou D, Dandine-Roulland C, Hemery F, Habibi A, Charles-Nelson A, Galacteros F, Brun-Buisson C, Maitre B, Katsahian S. Environmental influences on daily emergency admissions in sickle-cell disease patients. Medicine (Baltimore) 2014 Dec;93(29):e280. doi: 10.1097/MD.0000000000000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cano N, Melchior JC. Malnutrition in chronic diseases. Rev Prat. 2003;53(3):268–73. [PubMed] [Google Scholar]
- 22.Von Ruesten A, Feller S, Bergmann MM, Boeing H. Diet and risk of chronic diseases: results from the first 8 years of follow-up in the EPIC-Potsdam study. European Journal of Clinical Nutrition. 2013;67:412–419. doi: 10.1038/ejcn.2013.7. [DOI] [PubMed] [Google Scholar]
- 23.Saunders J. Malnutrition: causes and consequences. Clin Med (Lond) 2010 Dec;10(6):624–627. doi: 10.7861/clinmedicine.10-6-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bourke CD, Berkley JA, Prendergast AJ. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol. 2016 Jun;37(6):386–398. doi: 10.1016/j.it.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foucher J, Chanteloup E, Vergniol J, Castéra L, Bail B, Adhoute X, et al. Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut. 2006;55(3):403–8. doi: 10.1136/gut.2005.069153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Subjective global assessment form (Internet) [Accessed on: 14/2/2020]. available at: https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html.
- 27.World Health Organization. WHO Global Database on Body Mass Index. WHO-BMI ; 2018. [Internet]. Retrieved from http://apps.who.int/bmi/index.jspon 16/1/2020. [Google Scholar]
- 28.Jackson AS, Pollock M. Practical assessment of body composition. Physician Sport Med. 1985;13:76–90. doi: 10.1080/00913847.1985.11708790. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. Use and interpretation of anthropometric indicators of nutritional status. Bull World Health Organ. 1986;64:929–941. [PMC free article] [PubMed] [Google Scholar]
- 30.Nevitt SJ, Jones AP, Howard J. Hydroxyurea (hydroxycarbamide) for sickle cell disease. Cochrane Database Syst Rev. 2017 Apr 20;4(4):CD002202. doi: 10.1002/14651858.CD002202.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The 36-Item Short Form Survey (SF-36) (Internet) available at: https://www.physio-pedia.com/36-Item_Short_Form_Survey_(SF-36)
- 32.Coons S, Abdulmohsin SA, Draugalis JR, Hays RD. Reliability of an Arabic Version of the RAND-36 Health Survey and Its Equivalence to the US-English Version. Medical Care. 1998;36(3):428–43. doi: 10.1097/00005650-199803000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Hankins JS, Estepp JH, Hodges JR, Villavicencio MA, Robison LL, Weiss MJ, Kang G, Schreiber JE, Porter JS, Kaste SC, Saving KL, Bryant PC, Deyo JE, Nottage KA, King AA, Brandow AM, Lebensburger JD, Adesina O, Chou ST, Zemel BS, Smeltzer MP, Wang WC, Gurney JG. Sickle Cell Clinical Research and Intervention Program (SCCRIP): A lifespan cohort study for sickle cell disease progression from the pediatric stage into adulthood. Pediatr Blood Cancer. 2018 Sep;65(9):e27228. doi: 10.1002/pbc.27228. [DOI] [PubMed] [Google Scholar]
- 34.Oyedeji C, Strouse JJ, Crawford RD, Garrett ME, Ashley-Koch AE, Telen MJ. A multi-institutional comparison of younger and older adults with sickle cell disease. Am J Hematol. 2019 Apr;94(4):E115–E117. doi: 10.1002/ajh.25405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruiz AJ, Buitrago G, Rodríguez N, Gómez G, Sulo S, Gómez C, Partridge J, Misas J, Dennis R, Alba MJ, Chaves-Santiago W. Araque Clinical and economic outcomes associated with malnutrition in hospitalized patients. J Clin Nutr. 2019 Jun;38(3):1310–1316. doi: 10.1016/j.clnu.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 36.Lebwohl B, Sanders DS, Green PHR. Coeliac Disease. Lancet. 2018;391:70–81. doi: 10.1016/S0140-6736(17)31796-8. [DOI] [PubMed] [Google Scholar]
- 37.Pulley J, Todd A, Flatley C, Begun J. Malnutrition and quality of life among adult inflammatory bowel disease patients. Journal Gastentol Hepatol (JGH) 2020;4(3):454–460. doi: 10.1002/jgh3.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huisman EJ, Trip EJ, Siersema PD, van Hoek B, van Erpecum KJ. Protein-energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol. 2011;23:982–989. doi: 10.1097/MEG.0b013e32834aa4bb. [DOI] [PubMed] [Google Scholar]
- 39.Saeed A, Assir Ai, Assiri H, Ullah A, Rashid M. Celiac disease in Saudi children: Evaluation of clinical features and diagnosis. Saudi Med J. 2017;38(9):895–899. doi: 10.15537/smj.2017.9.20808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fadda A, Peedikayil MC, Kagevi I, Al Kahtani K, Ben Mousa A, Al Ashgar HI, Al Sohaiban Hi Al, Quaiz M, Abdulla A, Khan MQ, Helmy A. Inflammatory bowel disease in Saudi Arabia: a hospital-based clinical study of 312 patients. Ann Saudi Med. 2012;32(3):276–282. doi: 10.5144/0256-4947.2012.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee MT, Licursi M, McMahon DJ. Vitamin D deficiency and acute vaso-occlusive complications in children with sickle cell disease. Pediatr Blood Cancer. 2015;62(4):643–7. doi: 10.1002/pbc.25399. [DOI] [PubMed] [Google Scholar]
- 42.Ajayi OI, Bwayo-Weaver S, Chirla S, Serlemitsos-Day M, Daniel M, Nouraie M, Edwards K, Castro O, Lombardo F, Gordeuk VR. Cobalamin status in sickle cell disease. Int J Lab Hematol. 2013 Feb;35(1):31–7. doi: 10.1111/j.1751-553X.2012.01457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Antwi-Boasiako C, Dankwah GB, Aryee R, Hayfron-Benjamin C, Doku A, N‘guessan BB, Asiedu-Gyekye IJ, Campbell AD. Serum iron levels and copper-to-zinc ratio in sickle cell disease. Medicina. 2019;55(5):180. doi: 10.3390/medicina55050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martyres DJ, Vijenthira A, Barrowman N, Harris-Janz S, Chretien C, Klaassen RJ. Nutrient insufficiencies/deficiencies in children with sickle cell disease and its association with increased disease severity. Pediatr Blood Cancer. 2016;63(6):1060–4. doi: 10.1002/pbc.25940. [DOI] [PubMed] [Google Scholar]
- 45.Mandese V, Marotti F, Bedetti L, Bigi E, Palazzi G, Iughetti L. Effects of nutritional intake on disease severity in children with sickle cell disease. Nutr J. 2016 Apr 30;15(1):46. doi: 10.1186/s12937-016-0159-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Anthropometric measurements in SCD patients and control subjects.
| Parameter | Group A (n=20) | Group B (n=42) | P-value Group A vs B |
Control subjects (n=50) | P-value Group A &B vs. Controls: |
|---|---|---|---|---|---|
| Middle upper arm circumference (MUAC) (cm) | 21.85±1.73 | 19.65±1.03 | <0.0001** | 23.97±2.95 | Group A & B vs. Controls <0.0001** |
| Triceps skinfold thickness (TSK) (mm) | 6.73 ±3.06 | 5.67 ±2.95 | 0.196 | 8.37 ±4.39 | Group A vs. Controls: 0.084 Group B vs. Controls:0.0024** |
| Abdominal skinfold (mm) | 14.48±3.5 | 12.97±2.1 | 0.038 | 17.65±3.34 | Group A vs. Controls: 0.0003 Group B vs. Controls: <0.0001** |
| Waist circumference (WC) (cm) | 70.43 ±5.56 | 68.36±3.27 | 0.074 | 77.53±6.04 | Group A & B vs. Controls <0.0001** |
| Hip Circumference (HC) (cm.) | 80.14 ± 7.56 | 78.36± 3.27 | 0.074 | 84.73 ±9.38 | Group B vs. Controls: 0.035 Group A & B vs. Controls: 0.0003 |
| Body Fat (%) | |||||
| Low fat % (< 20% ); n (%) | 4(20) | 21 (50) | 0.026 | 1 (2) | Group B vs. Controls: 0.035 Group A & B vs. Controls: <0.0001 |
| Normal fat % (21–33%); n (%) | 16 (80) | 21 (50) | 0.026 | 45 (90) | Group A vs. Controls: 0.124 Group B vs Controls: 0.003 |
| Over fat% (34–39%); n (%) | 0 | 0 | 4 (28) | Group A & B vs. Controls 0.002 | |
| Obese (> 39) ; n (%)(82.14) | 0 | 0 | 0 | ||
Supplementary Table 2.
Parameters of patients treated with hydroxyurea versus those not treated.
| Parameter | Patients receiving HU (n=27) | Patients not receiving HU (n=35) | P-value |
|---|---|---|---|
|
| |||
| Hemoglobin (g/dl) ) mean ± SD | 9.074± 0.569 | 8.011±0.698 | <0.0001 |
|
| |||
| Ferritin levels at steady state(ng\dl); (Mean ± SD) | 171.89±54.48 | 152.51±51.63 | 0.158 |
|
| |||
| Energy intake (kcal/day); (Mean ± SD) | 1889.953±104.726 | 1724.158±92.551 | < 0.0001 |
|
| |||
| Daily protein intake (g); mean ± SD | 50.42±13.48 | 46.16±11.94 | 0.192 |
|
| |||
| Plasma folate level (ng/mL); mean ± SD | 14.86±2.98 | 13.28±3.11 | 0.048* |
|
| |||
| Serum zinc ( mg/dl ; mean ± SD | 70.68±12.59 | 61.65±14.02 | 0.011* |
|
| |||
| Vitamin B12 (pg/ml) ; mean ± SD | 339.894±84.474 | 287.651±82.173 | 0.017* |
|
| |||
| 25-OH-vitamin D (ng/mL); mean ± SD | 20.94±4.82 | 16.16±3.21 | < 0.0001** |
|
| |||
| - Growth hormone (ng/ml); mean±SD | 6.79± 2.12 | 4.24±2.52 | 0.402 |
|
| |||
| - Hypothyroid, n (%) | 5 (25) | 17 (40.48). | 0.223 |
| - Euothyroid, n (%) | 10 (50) | 14 (33.33) | 0.21 |
| - Hyperthyroid; n (%) | 5 (25) | 11 (26.19) | 0.921 |
|
| |||
| - Testesterone (ng/dL) (in men); mean ±SD | 656.12±205.84 | 603.91±185.49 | 0.321 |
|
| |||
| Estradiol (pg/mL) - (in women) |
200.29±66.72 | 189.68±71.53 | 0.579 |
|
| |||
| Mean number of SCD-related crises that needed hospitalization/person/during the entire follow-up | 4.33±1.65 | 8.76±2.44 | <0.0001** |
|
| |||
| Incidence rate of SCD-related events that required hospitalization (cases per person-year); (95% CI); | 0.328 (0.258 to 0.410) | 0.508 (0.425 to 0.601) | 0.0021** |
|
| |||
| Mean SCD severity score during follow-up | 0.215±0.116 | 0.440±0.177 | < 0.0001** |
Macro and micronutrient levels before and after supplementation and during VOC crises. A significant improvement in nutrients was observed between baseline levels and after supplementation. During crises, the level of nutrients declined though it was higher than baseline levels.