Abstract
Background
A large number of international migrants in Malaysia face challenges in obtaining good health, the extent of which is still relatively unknown. This study aims to map the existing academic literature on migrant health in Malaysia and to provide an overview of the topical coverage, quality and level of evidence of these scientific studies.
Methods
A scoping review was conducted using six databases, including Econlit, Embase, Global Health, Medline, PsycINFO and Social Policy and Practice. Studies were eligible for inclusion if they were conducted in Malaysia, peer-reviewed, focused on a health dimension according to the Bay Area Regional Health Inequities Initiative (BARHII) framework, and targeted the vulnerable international migrant population. Data were extracted by using the BARHII framework and a newly developed decision tree to identify the type of study design and corresponding level of evidence. Modified Joanna Briggs Institute checklists were used to assess study quality, and a multiple-correspondence analysis (MCA) was conducted to identify associations between different variables.
Results
67 publications met the selection criteria and were included in the study. The majority (n=41) of studies included foreign workers. Over two-thirds (n=46) focused on disease and injury, and a similar number (n=46) had descriptive designs. The average quality of the papers was low, yet quality differed significantly among them. The MCA showed that high-quality studies were mostly qualitative designs that included refugees and focused on living conditions, while prevalence and analytical cross-sectional studies were mostly of low quality.
Conclusion
This study provides an overview of the scientific literature on migrant health in Malaysia published between 1965 and 2019. In general, the quality of these studies is low, and various health dimensions have not been thoroughly researched. Therefore, researchers should address these issues to improve the evidence base to support policy-makers with high-quality evidence for decision-making.
Keywords: statistics & research methods, public health, health services administration & management
Strengths and limitations of this study.
This study provides a comprehensive overview of migrant health research in Malaysia, including a summary table, critical assessment tables and a multiple-correspondence analysis.
Methodological contributions by creating an evidence assessment framework, including a decision tree that identifies the type of study design and corresponding level of evidence, and modified Joanna Briggs Institute checklists.
Exclusive focus on vulnerable migrants within the non-citizen population in Malaysia.
Only English peer-reviewed academic articles were included in this study, and, therefore, much relevant information that could potentially be used to inform both policies and practice may have been excluded from this review.
Introduction
Worldwide, the international migrant population accounts for approximately 272 million people, with almost one-third within Asia.1 Due to its strategic geographical location and high labour demand, Malaysia is among the top destination countries for international migrants in the Asian region.2 According to the Department of Statistics Malaysia (DOSM), the documented non-citizen population represented 3.2 million people in 2019, which accounts for 10% of Malaysia’s total population.3 DOSM defines a non-citizen as a person that resides in Malaysia for 6 months or more in the reference year.4 However, no subcategories were included in this definition. According to the Office of the United Nations High Commissioner for Human Rights, a non-citizen is an individual that does not have an effective connection with the location where the person is situated according to the host nation, and includes various types of migrants, such as foreigners with permanent residency, refugees, asylum seekers, foreign labour, international students, stateless individuals and victims of human trafficking.5 Other definitions of migrant-related terms that are used in this paper are presented in table 1.
Table 1.
Definitions of migrant-related terms
| Term | Definition |
| Regular migrant worker (documented or legal migrant worker) | ‘A migrant worker or members of his or her family authorised to enter, to stay and to engage in a remunerated activity in the State of employment pursuant to the law of that State and to international agreements to which that State is a party.’116 (p29) |
| Irregular migrant worker (undocumented or illegal migrant worker) | ‘Migrant workers or members of their families, who are not authorised to enter, to stay or to engage in employment in a State.’116 (p102) |
| Refugee | ‘A person who, owing to a well-founded fear of persecution for reasons of race, religion, nationality, membership of a particular social group or political opinions, is outside the country of his nationality and is unable or, owing to such fear, is unwilling avail himself of the protection of that country.’116 (p79) |
| Asylum seeker | ‘A person who seeks safety from persecutions or serious harm in a country other than his or her own and awaits a decision on the application for refugee status under relevant international and national instruments. In case of a negative decision, the person must leave the country and may be expelled, as may any non-national in an irregular or unlawful situation, unless permission to stay is provided on humanitarian or other related grounds.’116 (p12) |
The vast majority of non-citizens in Malaysia are migrant workers, where foreign labour can be divided according to their visa status into regular and irregular migrant workers. According to the Ministry of Home Affairs, Malaysia issued 2 million work permits to documented migrant workers in 2019.6 However, the total number of migrant workers, both documented and undocumented, is estimated to fall between 4.2 and 6.2 million people.2 Another group that contributes significantly to the non-citizen population in Malaysia is refugees and asylum seekers. The terms refugees and asylum seekers are often used interchangeably, yet, these populations differ by their legal status in destination countries and subsequent vulnerabilities (see definitions in table 1). In 2019, an approximate 178 580 refugees and asylum seekers were registered with the United Nations High Commissioner for Refugees in Malaysia, where 153 770 (86%) came from Myanmar. The remaining number (14%) came from Yemen, Syria, Afghanistan, Iraq, Palestine, Pakistan, Sri Lanka, Somalia and other countries.7
Refugees, asylum seekers and both documented and undocumented low-skilled foreign workers can be classified as vulnerable migrants in Malaysia, as these populations may face significant hardships in their new country of residence.8 9 Vulnerable migrants are more prone to being exploited and abused, have an increased need to be protected by duty bearers and are not able to fully benefit from their human rights.10 Health is among these affected human rights, as migrant workers and refugees could encounter various challenges to maintain proper health and prevent poor health outcomes, including difficulties in accessing healthcare and obtaining quality health services.10–12 According to Sweileh et al,13 assessing the current status of scientific output and identifying research gaps could positively contribute towards improving the evidence base for advocating for migrant health needs. Scoping reviews can be helpful to map the academic literature and have been used by different researchers to present the available evidence on migrant health issues in other countries.14 15
Despite the burgeoning academic literature on migrant health in Malaysia, health information on migrant-related issues is still limited, and public data remain difficult to access. Aggravating the matter, there is no overall picture currently available of the evidence base on migrant health in Malaysia, including critical appraisal of the quality of research. Therefore, this study aims to map the existing academic literature on migrant health in Malaysia since 1965 to identify the trends and gaps in this field, as well as to present an overview of the topical coverage, quality and level of evidence of these scientific studies.
Methods
General methods
A scoping review was conducted, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses—Extension for Scoping Reviews guidelines16 (online supplemental file 1). A prereview protocol was developed to guide decisions for literature selection and structure of the review, and included the review question, aim, search strategy, selection criteria and risk of bias assessment. However, the protocol was not formally registered and changed to some extent over the course of this review. The prereview protocol can be accessed on request from the first author. Data were extracted and organised using the Bay Area Regional Health Inequities Initiative (BARHII) framework.17 In addition, a decision tree was developed to classify the type of study design and level of evidence of each journal article. Subsequently, a quality assessment of the included literature was conducted by using the Joanna Briggs Institute (JBI) critical appraisal toolkit.18 Lastly, the data were analysed, and a multiple-correspondence analysis (MCA) was applied to explore existing relationships between variables, including the type of migrant, main health dimension, quality of the study and research design.
bmjopen-2020-041379supp001.pdf (1.4MB, pdf)
Patient and public involvement
Patients and the public were not involved in this study.
Conceptual framework
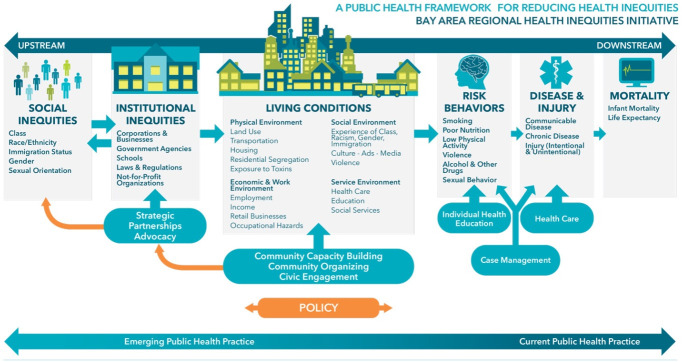
The BARHII framework was used to organise the identified literature in this scoping review into specific factors that shape equitable health outcomes (figure 1). The BARHII framework was selected due to its comprehensive nature and inclusion of various health dimensions, whereas other models focused on specific public health elements or lacked clear explanation regarding the included health-related components of the model.19 20
Figure 1.
Bay Area Regional Health Inequities Initiative framework.
The BARHII framework consists of six dimensions: (1) social inequities; (2) institutional inequities; (3) living conditions; (4) risk behaviour; (5) disease and injury; and (6) mortality. In addition, each health dimension contains various subdimensions (as presented in figure 1). Except for ‘social inequities,’ the other five categories were used to describe which health dimension the particular articles focused on. The social inequities element was incorporated by describing the population of interest, which was divided into three categories: foreign workers, asylum seekers and refugees, and unclassified migrants. The lattermost category was applied if a paper used the term ‘migrants’ or ‘immigrants’ but lacked specific information to classify the study population as foreign workers or asylum seekers/refugees.
Institutional inequities include the practices of corporations, businesses, government agencies, schools, not-for-profit organisations as well as laws, regulations and policies that could influence health outcomes (eg, a regulation that obligates companies to financially compensate an individual in case of a work incident).
Living conditions consist of the physical environment (eg, indoor air pollution), economic and work environment (eg, unemployment), social environment (eg, discrimination in the neighbourhood) and service environment (eg, healthcare) that people live in, and that play a role in determining their health outcomes (eg, denied healthcare access due to visa status).
Risk behaviour includes smoking, poor nutrition, low physical activity, violence, alcohol and other drugs and sexual behaviour. This dimension reflects the way someone acts and how that increases or decreases the risk of obtaining a particular health outcome (eg, the attitude and related behaviour towards smoking could influence an individual’s level of risk of developing lung cancer).
Disease and injury consist of communicable diseases (also known as infectious diseases; eg, chlamydia), chronic diseases (also known as non-communicable diseases; eg, cancer) and injuries (eg, fractured bone). This dimension describes the number of people or individual cases with a particular health outcome (eg, 10 out of the 100 people suffered from cancer).
Mortality was changed to ‘mortality and morbidity’ and focused on death and disease rates of the study population (eg, 10 out of 1000 live births of children under the age of 1 died) to distinguish epidemiological studies with larger samples from descriptive studies with smaller samples, where the latter were categorised as disease and injury studies.
Furthermore, some additional subdimensions were created during the data extraction stage, as these were lacking in the original BARHII framework (eg, the subdimension ‘mental health’ was added to the disease and injury dimension).
Search strategy
Based on the guidelines of the London School of Hygiene and Tropical Medicine21 and Bramer et al22 on selecting the number and types of databases that should be included in biomedical systematic searches, six databases were selected for this study: Econlit, Embase, Global Health, Medline, PsycINFO and Social Policy and Practice. This scoping review includes studies from 1965 onwards until 2019. However, all identified records were retrieved from the six databases to manually screen the data for publication date-related issues. The search process was conducted by AWdS and included a two-stage procedure to ensure that the search was exhaustive and to minimise the risk of missing potentially eligible studies. The first stage focused on identifying English-language key words and Medical Subject Headings terms for migrants (eg, immigrants, foreign workers, refugees), health (eg, disease, infection, disorder) and Malaysia (eg, Sabah, Kuala Lumpur) through reading search strategies of other review studies on migrant health as well as using medical terminology of renowned medical institutions, such as the Mayo Clinic. Subsequently, these items were combined by using Boolean operators (eg, migrant AND health AND Malaysia) in the search platform of each database (online supplemental file 2).
bmjopen-2020-041379supp002.pdf (123.4KB, pdf)
Selection criteria
Studies were eligible for inclusion if they met the following inclusion criteria: (1) conducted in Malaysia, including cross-national studies in which Malaysia was included; (2) published in peer-reviewed academic journals; (3) primary outcomes of the study included a health-related variable from at least one of the five health dimensions of the BARHII framework; (4) employment of one of the following study designs: literature synthesis (systematic review, meta-analysis, other scientific review designs), qualitative (interviews, focus group discussions) and/or quantitative (randomised controlled trial (RCT), cohort, case-control, cross-sectional, case series, case report) study design; (5) written in English; (6) inclusion of international (im)migrants, foreign workers, asylum seekers and refugees, as these groups were considered as vulnerable migrant populations in Malaysia. Articles that included both migrants and the general population were included in this study if sufficient information concerning the migrant population was available.
Studies were excluded if they were: (1) conducted or included data from 1965 or earlier, as Singapore was part of Malaysia until 1965, and this study is careful to only include Malaysia studies without Singapore; (2) grey literature; (3) opinion papers, editorials, fieldnotes of symposia, conferences and workshop abstracts; (4) focused on non-citizens and foreigners, where it was unclear whether a vulnerable migrant population was included (such as permanent residents, naturalised persons, expatriates, temporary visitors, tourists, Malaysian returnees and international students); (5) only presented migrants as a control variable and no other information regarding migrants was available.
Data extraction
Three reviewers (AWdS, ZXC and NSP) were involved in the screening process, where all had experience in the domain of public health and AWdS and NSP had practical knowledge with respect to conducting systematic reviews due to previous research work. Titles and abstracts were exported by AWdS and subsequently moved into Rayyan, an open-source software designed to support systematic reviews. AWdS and ZXC were the main reviewers, where AWdS conducted an entire screening of titles and abstracts and ZXC assessed a randomly selected 20% sample. Independent screening was carried out by using the ‘blind’ function of Rayyan, with both researchers working separately. The first stage involved screening titles and abstracts according to the inclusion criteria. Subsequently, AWdS and ZXC conducted an independent full-text screening of all potential articles and attached comments to each article on why the paper was included or excluded. After each screening stage, AWdS and ZXC compared their findings and discussed the discrepancies. In both stages, the discrepancies were about 13%–14% of the papers and were mostly around the study design and target populations. Conflicts were examined and resolved by NSP.
Following the full-text screening stage, the data were extracted by one reviewer (AWdS) and disaggregated by the different dimensions of the BARHII framework, including the type of migrant (social inequities), main health dimension (institutional inequities, living conditions, risk behaviour, disease and injury and mortality and morbidity) and health subdimensions.
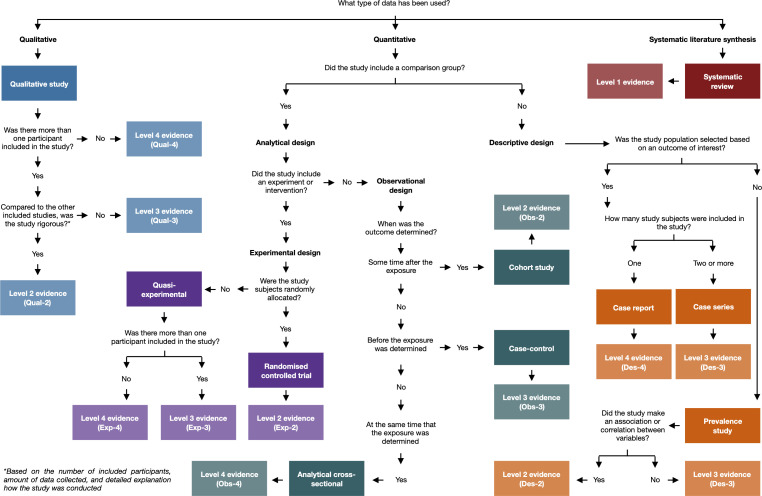
For the next stage, a decision tree was developed to ensure that the correct quality appraisal tool by study design was selected and to identify the level of evidence of the included literature (figure 2). Although various research designs were included in the decision tree, some study designs did not fit in this model, such as the mixed-method design.
Figure 2.
Decision tree to identify the type of study design and corresponding level of evidence.
The decision tree built on the study design tree from the Centre for Evidence-Based Medicine23 and essentially allowed research of varying designs to be consistently, reliably classified into one of several design families. The newly developed decision tree was created through a two-step process. First, a table was created that included definitions of various research designs, and, subsequently, specific traits of these definitions were used to develop guiding questions for the decision tree (table 2).
Table 2.
Definitions of included study designs
| Study design | Definition |
| Analytical studies | Studies that strive to quantify the relationship between a particular exposure or intervention and the outcome of interest, where these studies include a comparison group to compare the outcome rates.23 |
| Systematic review | A study that is conducted systematically to collect all published evidence—that comply with the specified inclusion criteria—and provide a summary of the results to answer a specific research question.117 |
| Randomised controlled trial (RCT) | An experimental study that includes at least two groups—treatment group and control group—to compare the outcomes between the group that received the intervention/drug and the group that received a placebo/no treatment. The participants of the group are randomly allocated to one of the groups.118 |
| Quasi-experimental study/non-RCT | An experimental study that includes at least two groups—treatment group and control group—to compare the outcomes between the group that received the intervention/drug and the group that received a placebo. The participants of the group are not randomly allocated to one of the groups.119 |
| Cohort study | A study that follows a group of people over time, where the participants are sampled based on the presence or absence of a particular exposure to compare the outcome of interest with a control group.118 |
| Case-control study | A study that includes a group of people selected on the outcome of interest (cases) and a group without the outcome of interest (controls), followed by assessing previous exposure of both groups to determine if there is a relationship between the level of exposure and outcome of interest.118 |
| Analytical cross-sectional | A study that looks at two groups—exposed and unexposed—and the outcome of interest at a particular point or period of time to compare the differences between the two groups.118 |
| Descriptive studies | Studies that do not strive to quantify a relationship between variables, but simply describe the disease outcome and characteristics within a defined population. Note that descriptive studies can still include analytic components.23 |
| Prevalence study | A study that looks at a population at a particular point or period of time to describe the prevalence of an outcome of interest.118 |
| Case series | A study where only subjects are included with a particular outcome of interest to describe the shared and diverging characteristics of this study population.120 |
| Case report | A study that describes an unfamiliar or extraordinary outcome of one individual.120 |
Second, Tomlin and Borgetto’s24 model was used to identify the level of evidence of the included literature, as the study designs that were included in their model were in line with the research designs in the definitions table. In addition, it was one of the few models that deconstructed the single-hierarchy framework and assigned study designs to different categories depending on the study objective (eg, if the study design did not aim to provide a causal relationship, but simply describe a particular outcome, the study design would be classified as descriptive research), and, therefore, valued studies with different objectives equally. Tomlin and Borgetto’s model consists of four dimensions, including descriptive research, experimental research, outcome research and qualitative research. Each of these dimensions contains four subclasses to show the level of evidence within each class, where level 1 is the highest level of evidence and level 4 the lowest. The assignment of these levels to the different study designs is based on the degree of internal validity/authenticity and external validity/transferability, where level 1 is regarded with the highest level of these two measures and level 4 ranks the lowest. Table 3 shows the different research dimensions that correspond with the included study designs and level of evidence.
Table 3.
Level of evidence for each study design
| Research design* | Level of evidence | Abbreviation |
| Descriptive research | ||
| Systematic review of descriptive studies | 1 | Des-1 |
| Prevalence study with analytical component | 2 | Des-2 |
| Case series and prevalence study without analytical component | 3 | Des-3 |
| Case report | 4 | Des-4 |
| Experimental research | ||
| Systematic review/meta-analysis of experimental studies | 1 | Exp-1 |
| Randomised controlled trial | 2 | Exp-2 |
| Group quasi-experimental study (a.k.a. non-RCT) | 3 | Exp-3 |
| Quasi-experimental study with single subject | 4 | Exp-4 |
| Observational research | ||
| Systematic review/meta-analysis of observational studies | 1 | Obs-1 |
| Cohort study | 2 | Obs-2 |
| Case-control | 3 | Obs-3 |
| Analytical cross-sectional study | 4 | Obs-4 |
| Qualitative research | ||
| Systematic review/meta-synthesis of qualitative studies | 1 | Qual-1 |
| Group qualitative studies with more rigour† | 2 | Qual-2 |
| Group qualitative studies with less rigour | 3 | Qual-3 |
| Qualitative study with a single informant | 4 | Qual-4 |
1=Highest level of evidence; 4=lowest level of evidence.
*The following terminology of Tomlin and Borgetto’s model has been modified to align with the included research designs in this study: association/correlation studies=prevalence studies with analytical component; normative/descriptive studies=prevalence studies without analytical component; individual case studies=case report; controlled-clinical trials=group quasi-experimental study; single-subject studies=quasi-experimental study with single subject; pre-existing groups comparisons with covariate analysis=cohort study; one-group pre–post studies=analytical cross-sectional study.
†Rigour was subjectively assessed and based on the number of included participants, amount of collected data and detailed explanation how the study was conducted.
RCT, randomised controlled trial.
After incorporating feedback on the questions used to identify the research design and multiple testing rounds to assess if the questions were specific enough to distinguish these designs within the full set of articles, the final version of the decision tree—as seen in figure 2—was used to extract the data.
Quality appraisal and level of evidence assessment
The quality assessment of the included studies was conducted by one reviewer (AWdS) based on the JBI critical appraisal tools, as this toolkit includes checklists for a wide variety of study designs that are most in line with the research designs included in this study. Additional objective criteria specific to migrant health studies were developed for each question of the JBI checklists to increase the reliability of the quality assessment. An example is provided in table 4.
Table 4.
Example of additional objective criteria for the Joanna Briggs Institute toolkit
| Question | ‘Were the study subjects and the setting described in detail?’121 (p3) |
| Original explanation | ‘The study sample should be described in sufficient detail so that other researchers can determine if it is comparable to the population of interest to them. The authors should provide a clear description of the population from which the study participants were selected or recruited, including demographics, location, and time period.’121 (p4) |
| Additional objective criteria | ‘Yes’ should be selected if different demographic variables are presented in absolute numbers, including age (aggregated in individual years or age categories), sex, and nationality. In addition, the setting should be described by providing the name of the location and/or a description of the location. |
| ‘No/unclear’ should be selected if a description regarding age, sex, and/or nationality in absolute numbers are lacking. Note that using only means and ratios will not be sufficient to answer this question, and no/unclear should be selected. In addition, no/unclear should be selected if the name and/or description of the location is not given. |
After discussing the additional criteria and piloting the tools, slight modifications were made for the JBI tools, and these final versions were used to assess the quality of the papers. The modified checklists can be accessed on request from the first author.
Questions were answered with ‘Yes (V)’ if the study met the criteria according to descriptions provided in the final version of the JBI toolkit. ‘No/Unclear (X)’ was selected if the study did not address the question or if information to assess the given criteria was lacking. The score concerning the quality of the study was determined by summing up all ‘Yes’ answers and dividing this number by the total number of answered questions, which differed by study design in the JBI tools. Questions that were answered with ‘Not applicable (N/A)’ were excluded from the calculation. As the JBI toolkit has no standard scoring index, the following scoring system was applied: (1) low quality=0%–50%; (2) moderate quality=above 50% and below 75%; (3) high quality=75% or higher. Although a four-band scoring system—where each category would include a 25% scoring range—was considered, a three-band scoring system was selected because the three given categories—low, moderate and high—would simplify the interpretation concerning the quality of the study. In a four-band system, the distinction and classification of the two middle categories are less straightforward compared with the three-band scoring system. Further, the first two categories in a four-band scoring system would still represent a poor-quality study, and, hence, should be used to signal more cautious interpretation of the study results among readers. The cut-off score was based on the idea that if a study could answer yes to only half or less of the questions, it would not be sufficient to transmit a reliable message to the audience. Therefore, at least more than half of the questions should be answered with yes to obtain a moderate score. The 75% cut-off was still based on the idea of having four equal scoring categories, where 75% and above would be classified as a high-quality study and would inform the audience with a more credible message.
Data analysis
Data concerning the type of migrant, health dimension, health subdimension, research design, level of evidence and quality assessment score were imported into Microsoft Excel for Mac (V.16.28). Mean quality scores were calculated for the different variables by using Microsoft Excel, including the type of migrant, health dimension, health subdimension, research design and level of evidence. RStudio (V.1.0.136; Macintosh; Intel Mac OS X 10_15) was used to conduct χ2 tests and an MCA. An MCA is a descriptive technique that can be used to visually demonstrate relationships among the levels of several categorical variables—here, these include the type of migrant, main health dimension, quality of the study and research design—in a two-dimensional (2D) space. The MCA projects categories in a 2D space with axes defined by latent dimensions (and, therefore, it is not possible to label the axes), based on weighted Euclidean distances.25 The MCA allows categories with similar profiles to be grouped together, where a closer distance of categories within the same quadrant demonstrates a stronger relationship, whereas categories that are further apart and in opposite quadrants present weaker associations.26 In addition to the MCA, χ2 tests were conducted to assess whether categorical variables were independent (eg, not associated). It should be noted that a few studies included two BARHII dimensions, yet, the analysis only allowed one dimension to be included. Therefore, only the most prominent dimension, based on the amount of attention given to the specific dimension in the article, was selected and used for the analysis.
Results
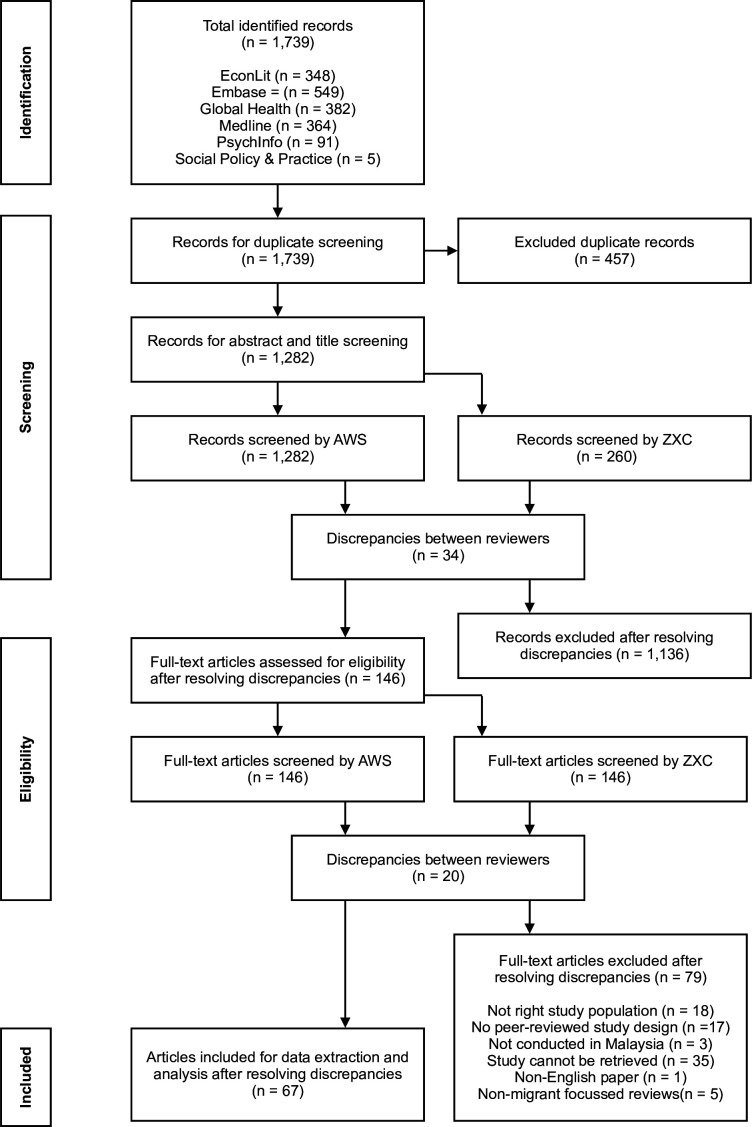
The study selection process is presented in figure 3. After removing the duplicates, 1282 original records were identified. A total of 1136 papers were excluded after the title and abstract screening stage due to focusing on another population of interest, lacking focus on a BARHII health dimension, not being a peer-reviewed academic article, and including data before 1965. As a result, 146 articles were eligible for the full-text screening stage. Subsequently, full-text articles were retrieved from these 146 records, and eventually, 67 papers met the inclusion criteria and were included in this review.
Figure 3.
Flow chart of the data selection process.
Characteristics of included papers
This section first demonstrates the findings of each BARHII dimension, followed by the results on the quality and level of evidence of the included studies. Lastly, existing relationships between the type of study design, study quality of the study, type of migrant and main health dimension are shown. Table 5 presents a descriptive summary of all included articles, including the study design and corresponding level of evidence, study period, type of migrant, sample population, main health dimension, health subdimension, quality assessment score and a short description of the study.
Table 5.
Summary table of included articles
| Reference | Study design | Study period | Type of migrant | Sample population*** | Main category | Subcategory | Quality score | Summary |
| Scheutz et al88 | Prevalence (Des-3) |
January–May 1982 | Asylum seekers and refugees | 361 Vietnamese refugees | Disease and injury | Non-communicable disease (oral health) |
Moderate (55.6) |
Dental health of refugees was examined, and the study showed a positive relationship between the average number of tooth decay and missing teeth and increase in age among younger refugees. |
| Levy89 | Prevalence (Des-2) |
July–August 1984 | Asylum seekers and refugees | 297 children (94 Filipino,104 Muruts, 99 Kadazan) |
Disease and injury | Communicable disease (parasite) |
Low (44.4) |
Three groups of children—one refugee group and two indigenous groups—were examined for six types of intestinal parasites. Among the three groups, Filipino refugee children presented significant higher rates of Trichuris trichiura and ascaris lumbricoides compared with both groups. |
| Kassim et al38 | Case series (Des-3) |
1985–1986 | Unclassified migrants* | 86 children (7 migrants,† 34 Malays, 16 Chinese, 3 mixed origin) |
Risk behaviour | Violence and abuse (Neglect) |
Moderate (60.0) |
In total, 86 children were identified as cases suffering from different types of abuse. Among this group were seven irregular migrant children, where they were identified as neglected, due to lacking nutritional and physical needs. |
| Zulkifli et al28 | Analytical cross-sectional (Obs-4) |
N/A† | Unclassified migrants | 1515 people (336 migrants,† 1075 citizens) |
Living conditions Mortality and morbidity |
Service environment (healthcare utilisation) Mortality rates (Under-five mortality) |
Low (33.3) |
A comparison between migrants and locals regarding maternal and child health outcomes were studied. Migrant women had a lower usage of contraceptives and antenatal care, but used the services of traditional birth attendants more compared with local women. In addition, migrant women had statistically significantly higher rates regarding infant mortality compared with locals. |
| Rajeswari et al48 | Prevalence (Des-3) |
N/A† | Foreign workers‡ | 456 children (10 Indonesians, 357 Malays, 78 Orang Asli, 11 Indian) |
Disease and injury | Communicable disease (parasite) |
Low (22.2) |
School children were examined for different types of helminths and protozoa, and the study showed that children from migrant workers had the highest prevalence. |
| Jeyakumar39 | Case series (Des-3) |
10 May 1993–8 July 1993 | Unclassified migrants*, §§ |
27 migrants (23 Bangladeshi, 4 Indonesians) |
Risk behaviour | Poor nutrition (nutrition deficiency) |
Low (40.0) |
Twenty-seven detained irregular migrants were sent to the hospital to treat ankle oedema, where they showed a positive response to thiamine treatment. |
| Jamaiah et al82 | Case series (Des-3) |
1983–1992 | Unclassified migrants* | 134 people (22 Indonesian, 22 Others†, ††† 40 Chinese, 37 Malays, 13 Indians) |
Disease and injury | Communicable disease (parasite) |
Low (40.0) |
A total of 134 malaria cases were admitted to University Hospital Kuala Lumpur between 1983 and 1992, including 22 irregular Indonesian migrants (16.4%) and 22 (16.4%) other foreigners (such as other irregular migrants from Bangladesh, India and Thailand, as well as Vietnamese refugees. In addition, chloroquine-resistance was found in nine irregular Indonesian migrants and six other foreigners. |
| Krahl and Hashim49 | Prevalence (Des-3) |
January 1994–June 1996 | Foreign workers‡‡‡, ¶¶¶ |
39 people (20 Indonesians, 16 Filipinos, 1 Bruneian, 1 Singaporean, 1 Thai) |
Disease and injury | Mental health (psychiatric disorders) |
High (77.8) |
Within a 2-year period, 39 foreigners were admitted to the psychiatric wards of UHKL, including 30 migrant workers that suffered from a psychiatric disorder. Domestic workers represented with 23 cases the largest group among these foreign workers. |
| Zabedah et al40 | Prevalence (Des-2) |
N/A† | Unclassified migrants | 37 people identified; 27 people included (17 Filipinos, 10 locals) |
Risk behaviour | Alcohol and other drugs (Inhalant) |
Low (22.2) |
Among the 37 suspected solvent abusers (glue sniffers) that were admitted to Bukit Padang Psychiatric Hospital, 27 children admitted using these inhalants. Almost two-third of the cases were Filipino immigrants. |
| Dony et al92 | Prevalence (Des-3) |
N/A† | Unclassified migrants | 3908 people (943 foreigners,† 2965 nationals) |
Mortality and morbidity | Morbidity rates (tuberculosis and leprosy) |
Moderate (62.5) |
An epidemiolocal study aimed to present the tuberculosis and leprosy trends in Sabah. Since 1990, at least 24% of the annual tuberculosis cases were among Indonesian and Filipino migrants, where the annual rate differed between 100 and 200 cases per 100 000 population between 1990 and 2000. Furthermore, leprosy rates among migrants differed from 4.39 cases to 6.19 cases per 100 000 population between 1996 and 2001. |
| Chandran et al50 | Case report (Des-4) |
N/A† | Foreign workers | 1 Myanmar | Disease and injury | Communicable disease (parasite) |
High (83.3) |
A Jabouley procedure was carried out to treat a 30-year-old Myanmar worker that suffered from a filarial infection. After the procedure, the patient was discharged, but did not show for the follow-up. |
| Nissapatorn et al51 | Prevalence (Des-3) |
January 2000–April 2004 | Foreign workers | 1885 patients† | Disease and injury | Communicable disease (parasite) |
Low (50.0) |
Within a 4-year period, 1885 medical records of the University of Malaya Medical Centre were reviewed to identify the prevalence of four common protozoan infections. In total, 28 malaria cases were identified, where 60.7% was among foreigners. The majority of this group consisted of foreign workers. |
| Sobri et al83 | Case series (Des-3) |
January 1995–December 2001 | Unclassified migrants | 42 people (7 Indonesians, 1 Burmese, 1 Siamese (Thai), 1 Bangladeshi, 1 Nepalese, 23 Malays, 6 Chinese, 2 Indians) |
Disease and injury | Communicable disease (bacteria) |
Low (50.0) |
In total, 42 patients were diagnosed with tuberculosis meningitis at the Kuala Lumpur Hospital during a 7-year period. Eleven (9.5%) out of the 42 tuberculosis meningitis patients were among immigrants. |
| Leong52 | Prevalence (Des-3) |
1 January 1997–31 December 2004 | Foreign workers | 3117 Indonesians | Disease and injury | Various diseases (various diseases) |
Low (44.4) |
During an 8-year period, 3117 female migrant (domestic) workers were screened at a private clinic in Johor Bahru, where 223 (7.2%) of them presented medical problems. Hypertension, pulmonary tuberculosis and hepatitis B were the top three major issues. |
| Sasidharan et al53 | Prevalence (Des-2) |
June 1999–September 2001 | Foreign workers | 697 people (26 Bangladeshi, 276 Malays, 229 Chinese, 166 Indians) |
Disease and injury | Communicable disease (bacteria) |
High (77.8) |
From 1999 to 2002, a total of 697 patients were examined for Helicobacter pylori infection. Twenty-six Bangladeshi foreign workers were among this group, and the infection was present in six of them. |
| Masitah54 | Case series (Des-3) |
N/A† | Foreign workers | N/A† | Disease and injury | Communicable disease (parasite) |
Low (22.2) |
During a 6-year period, different malaria registries were reviewed to identify the number of cases in Selangor. The number of annual malaria cases decreased from 172 people in 2001 to 90 people in 2006, while the proportion of cases among migrant workers increased from 57% to 75%, respectively. |
| Shailendra and Prepageran55 | Case report (Des-4) |
N/A† | Foreign workers | 1 Myanmar | Disease and injury | Communicable disease (parasite) |
High (75.0) |
A 38-year-old Myanmar migrant worker presented a case of oropharyngeal rhinosporidiosis. The abnormal growths were removed, and the patient did not show any recurrence of the disease after a 3-month follow-up. |
| Chan et al56 | Analytical cross-sectional (Obs-4) |
N/A† | Foreign workers* | 699 people (336 Indonesians, 45 Bangladeshi, 45 Indians, 26 Nepalese, 22 Myanmar, 17 Pakistani, 3 Africans,† 3 Sri Lankans, 3 Thai, 1 Chinese, 198 Malaysians) |
Disease and injury | Communicable disease (parasite) |
Low (0.0) |
A sample of 699 people were screened for toxoplasmosis, including 501 migrant workers. Among the migrant workers, 171 (34.1%) cases tested positive for the IgG antibodies test and 26 (5.2%) cases tested positive for the IgM antibodies test. The statistical analysis showed that the infection rate—using the IgG test—was significantly higher among local residents compared with the foreign workers. |
| Farhana et al57 | Case series (Des-3) |
1999–2008 | Foreign workers | 34 people (3 Myanmar, 1 Indonesian, 1 Pakistani, 14 Chinese, 9 Malays, 6 Indians) |
Disease and injury | Communicable disease (parasite) |
Low (60.0) |
A total of 34 amoebiasis cases were admitted to University Malaya Medical Centre during a 10-year period, including five foreign workers. |
| Chan et al58 | Analytical cross-sectional (Obs-4) |
N/A† | Foreign workers* | 699 people (336 Indonesians, 45 Bangladeshi, 45 Indians, 26 Nepalese, 22 Myanmar, 17 Pakistani, 3 Africans,† 3 Sri Lankans, 3 Thai, 1 Chinese, 198 Malaysians) |
Disease and injury | Communicable disease (parasite) |
Low (0.0) |
A sample of 699 people were screened for toxoplasmosis, including 501 migrant workers. Among the migrant workers, 171 (34.1%) cases tested positive for the IgG antibodies test and 26 (5.2%) cases tested positive for the IgM antibodies test. The statistical analysis showed that the infection rate—using the IgG test—was significantly higher among local residents compared with the foreign workers. |
| Murty59 | Case report (Des-4) |
N/A† | Foreign workers | 1 Myanmar | Disease and injury | Non-communicable disease (benign) |
High (80.0) |
A 37-year-old foreign worker was found dead, and the postmortem examination showed that the case suffered from a cystic tumour in the heart. |
| Murty et al60 | Case series (Des-3) |
1996–2005 | Foreign workers | 27 people (16 Indonesians, 1 Bangladeshi, 1 Punjabi,† 1 Bajau,† 5 Malays, 2 Indians, 1 Chinese) |
Disease and injury | Injury (physical trauma) |
Low (44.4) |
During a 10-year study period, 27 cases of fatal lightning strikes were identified. The majority of the cases were among foreign workers, where Indonesians had with 16 people (59.3%) the highest prevalence. |
| Mustafa et al61 | Prevalence (Des-2) |
August 2006–March 2009 | Foreign workers | 558 patients (34 foreign labour,† 347 Malays, 97 Indians, 80 Chinese) |
Disease and injury | Communicable disease (virus) |
Low (44.4) |
A total of 558 suspected dengue cases were identified, including 34 migrant workers. Among the foreign labour group, 20 patients presented acute dengue, 4 patients presented recent dengue and 10 patients tested negative for dengue. |
| Su et al62 | Analytical cross-sectional (Obs-4) |
3 January 2007–24 April 2007 | Foreign workers |
194 people§ (95% Indonesians, 5% Bangladeshi) |
Disease and injury | Injury (physical syndrome) |
Moderate (57.1) |
During a 4-month cross-sectional study, 234 migrant workers were examined for level of occupational vibration exposure and health outcomes. In total, 18% of the migrant workers suffered from hand–arm vibration syndrome (HAVS). In addition, different HAVS-related symptoms were significantly higher among workers with high levels of exposure compared with migrant workers with low levels of exposure. |
| Daher et al84 | Prevalence (Des-2) |
September 2009–April 2010 | Unclassified migrants | 253 Iraqi | Disease and injury | Mental health (quality of life) |
High (75.0) |
Health-related quality of life of 253 Iraqi migrants was examined, showing that their quality of life was moderate and statically significant higher levels were found among men and married people. |
| Ratnasinga et al63 | Prevalence (Des-2) |
January 2010–November 2010 | Foreign workers | 5340 people (1348 Bangladeshi, 843 Myanmar, 743 Nepalese, 217 Indonesians, 2190 Malaysians) |
Disease and injury | Injury (physical trauma) |
Low (11.1) |
A total of 5340 workers in the furniture industry were examined, where 59% of this population was foreign labour. Compared with local workers, migrant workers had less occupational accidents and a more positive work-oriented mentality. |
| Ab Rahman et al64 | Case report (Des-4) |
N/A† | Foreign workers | 1 Nepalese | Disease and injury | Communicable disease (parasite) |
High (87.5) |
A 24-year-old Nepalese migrant worker presented a long medical history of different symptoms, including fever, abdominal pain and poor appetite. Clinical examination showed that the patient suffered from a visceral leishmaniasis and malaria coinfection, and he was treated with chloroquine and amphotericin B. A follow-up was carried out after 6 months and the man remained well. |
| Taib and Baba65 | Case series (Des-3) |
2006–2009 | Foreign workers | 75 patients (38 foreigners,§ 37 locals) |
Disease and injury | Communicable disease (bacteria) |
Low (30.0) |
A total of 75 leprosy cases were detected at the Hospital Kuala Lumpur Hansen’s Clinic during a 4-year period. With 38 patients, foreign workers represented more than half of the cases. |
| Osman et al41 | Prevalence (Des-3) |
June 2012–September 2012 | Unclassified migrants | 108 Iraqi | Risk behaviour | Sexual behaviour (HPV knowledge) |
Low (50.0) |
Knowledge and awareness regarding cervical cancer and pap smear tests were assessed among 108 Iraqi migrant women. In general, this population lacks understanding regarding cervical cancer and the importance of pap smear tests. |
| Minhat et al42 | Prevalence (Des-2) |
April 2010–June 2010 | Unclassified migrants | 271 Iranians | Risk behaviour | Sexual behaviour (HPV knowledge) |
Low (25.0) |
The knowledge regarding HPV vaccination of 271 Iranian female migrants was evaluated and showed that the majority of the study population has poor knowledge regarding this matter. Marital status was the only predicative factor that was statistically significant, where married women were 3.6 times more likely to have good HPV knowledge. |
| Mendelsohn et al29 | Qualitative (Qual-2) |
July 2010–September 2010 | Asylum seekers and refugees | 14 Myanmar¶ | Living conditions | Service environment (healthcare utilisation) |
High (90.0) |
Fourteen Myanmar refugees were interviewed to explore the difficulties that this group has in accessing antiretroviral therapy (ART). Barriers to comply to ART include lack of an UNHCR identity card, fear of arrest during travelling to the hospital, corruption, financial issues and receiving small quantities of ART medication per refill. |
| Mendelsohn et al30 | Analytical cross-sectional (Obs-4) |
April 2010–July 2010 | Asylum seekers and refugees | 299 people (146 Myanmar, 5 Others,† 148 Malaysians) |
Living conditions | Service environment (healthcare utilisation) |
High (83.3) |
ART compliance and virological outcomes were compared between HIV-infected refugees and locals, where the study showed that both groups had similar rates of compliance and unsuppressed viral loads. |
| Kwan et al85 | Case series (Des-3) |
2008–2013 | Unclassified migrants | 27 people (3 Indonesians, 2 Indians, 2 Nepalese, 2 Myanmar, 1 Sri Lankan, 17 Malaysians) |
Disease and injury | Communicable disease (bacteria) |
Low (40.0) |
Between 2008 and 2013, 27 leprosy cases were identified by reviewing the Dermatology Clinic census. Out of the 27 identified leprosy cases, 37% of them were among immigrants. |
| Santos et al66 | Prevalence (Des-3) |
February 2013–June 2013 | Foreign workers |
317 people (110 Sri Lankans, 85 Indonesians, 71 Indians,§ 22 Nepalese, 20 Indians,§ 9 Myanmar) |
Disease and injury | Injury (physical syndrome) |
Moderate (55.6) |
A sample of 317 migrant workers were examined to explore the prevalence of musculoskeletal pain among this group. Almost two-third (203 people) of the surveyed migrant workers suffered from work-related musculoskeletal complaints. Pain in the knee/leg/foot area was the most common, as 85 migrant workers reported this outcome. |
| Razali et al43 | Case series (Des-3) |
2000–2012 | Unclassified migrants | 18 females (2 Indonesians, 1 Myanmar, 6 Malays, 5 Chinese, 3 Indians, 1 Punjabi) |
Risk behaviour | Violence and abuse (murder) |
High (80.0) |
Clinical records of two forensic psychiatric institutions were reviewed during 2000 and 2012. A total of 18 cases that committed maternal filicide were detected, including three immigrant women that suffered from adverse life events. |
| Elmi et al86 | Case control (Obs-3) |
January 2010–April 2014 | Unclassified migrants | 209 cases (49 migrants,† 265 locals) |
Disease and injury | Communicable disease (bacteria) |
Low (50.0) |
A case control study was conducted to identify risk factors regarding multidrug-resistant tuberculosis (MDR-TB) development. The study showed that MDR-TB was more prevalent than non-MDR-TB among foreign patients, and that MDR-TB was significantly higher among migrants compared with locals. |
| Santos et al37 | Prevalence (Des-2) |
March 2013–April 2013 | Foreign workers |
317 people (110 Sri Lankans, 85 Indonesians, 71 Indians,§ 22 Nepalese, 20 Indians,§ 9 Myanmar) |
Living conditions Disease and injury |
Economic and work environment (occupational hazards) Injury (physical syndrome) |
Low (44.4) |
The study assessed overall levels of pain and identified perceived environmental hazards among a group of foreign workers. In total, 204 out of 317 migrant workers suffered from musculoskeletal pain, and noise (37.5%) and dust (37.2%) were perceived as the main environmental hazards among this group. |
| William et al87 | Prevalence (Des-2) |
4 July 2012–3 July 2014 | Unclassified migrants | 176 people (53 Filipinos, 6 Indonesians, 106 Indigenous, 10 Chinese, 1 Indian) |
Disease and injury | Communicable disease (bacteria and virus) |
High (77.8) |
During a 2-year study, 176 participants that tested positive for pulmonary tuberculosis at the Luyang Clinic in Kota Kinabalu were enrolled in the study. More than one-third of the patients (33.5%) were migrants. In addition, out of the three patients with a HIV coinfection, one was a migrant. |
| Siah et al90 | Prevalence (Des-2) |
N/A† | Asylum seekers and refugees |
89 children (39.3% Myanmar, 21.3% Somali, 22.5% Sudanese, 16.9% Others†) |
Disease and injury | Mental health (Quality of life) |
Low (11.1) |
A total of 89 refugee children were surveyed to investigate factors that influence their quality of life. Experiencing deportation, lower levels of education and unemployment of their fathers were significantly associated with a lower quality of life. |
| Guinto et al27 | Scoping review** | 2000–2014 | Foreign workers | N/A | Institutional inequities | Laws and regulations (universal health coverage (UHC)) |
N/A | The study presented implementation challenges of UHC in Southeast Asian countries. Malaysia implemented some measures regarding healthcare for migrant workers; however, government-run UHC is still lacking. |
| Vijian et al67 | Analytical cross-sectional (Obs-4) |
2010–2015 | Foreign workers | 50 people (8 Bangladeshi, 6 Nepalese, 3 Myanmar, 1 African†, §§§ 1 Pakistani, 1 Vietnamese, 14 Malays, 12 Chinese, 4 Indians) |
Disease and injury | Non-communicable disease (perforation) |
Low (16.7) |
Twenty foreign workers and 30 local patients that suffered from perforated peptic ulcers were compared with each other to assess the difference in characteristics between these two groups. Several characteristics were significantly different, where foreign workers were on average 18 years younger (mean age=30.4), suffered from smaller-sized ulcers, and experienced lower levels of postoperative complications. |
| Azian et al68 | Prevalence (Des-2) |
N/A† | Foreign workers |
2153 samples†† (1422 Bangladeshi, 349 Indians, 201 Nepalese, 78 Indonesians, 58 Vietnamese, 45 Myanmar) |
Disease and injury | Communicable disease (Parasite) |
Low (11.1) |
A total of 2153 blood samples were taken from migrant workers that were located in seven states of Peninsular Malaysia and were tested for leishmaniasis infection. More than half (55.3%) of the collected blood samples were found positive. |
| Sahimin et al69 | Prevalence (Des-2) |
September 2014–August 2015 | Foreign workers |
388 people (167 Indonesians, 81 Nepalese, 70 Bangladeshi, 47 Indians, 23 Myanmar) |
Disease and injury | Communicable disease (parasite) |
Low (33.3) |
A cross-sectional study was conducted to examine the prevalence of different intestinal parasitic infections among foreign labour. Out of the 388 migrant workers, infection rates were between 52.1% and 84%. Higher infection rates significantly associated with migrants from Nepal and India, recently arrived in the country, and less than 1-year work experience in Malaysia. |
| Noh et al31 | Prevalence (Des-2) |
N/A† | Foreign workers | 600 foreign workers† | Living conditions | Service environment (healthcare utilisation) |
Low (22.2) |
Data of 600 foreign workers were obtained to explore their healthcare utilisation. Most of them use health services occasionally (88.5%) and the majority (61.4%) goes to government hospitals. |
| Kamaludin and How46 | Analytical cross-sectional (Obs-4) |
February 2016–April 2016 | Foreign workers | 120 people† (60 foreign workers, 60 local workers) |
Risk behaviour | Hazard and safety awareness (environmental risk) |
Low (50.0) |
The study compared environmental health awareness between 60 local workers and 60 migrant workers, where the latter group showed significant lower levels of awareness. |
| Min et al70 | Prevalence (Des-3) |
January 2011–December 2013 | Foreign workers | 440 people (46 Indonesians, 37 Bangladeshi, 33 Nepalese, 17 Myanmar, 11 Pakistani, 8 Others,† 226 Malays, 32 Chinese, 20 Others,† 10 Indians) |
Disease and injury | Injury (physical trauma) |
Moderate (62.5) |
Medical records of the Hospital Sultan Ismail in Johor Bahru were reviewed between January 2011 and December 2013 to describe the prevalence of work-related ocular traumas. More than one-third of the ocular injuries were among foreign workers and contributed to two-third of the open eye traumas. |
| Woh et al71 | Prevalence (Des-3) |
N/A† | Foreign workers |
317 people (140 Indians, 80 Nepalese, 36 Indonesians, 29 Bangladeshi, 18 Myanmar, 7 Pakistani, 4 Sri Lankans, 2 Vietnamese, 1 Thai) |
Disease and injury | Communicable disease (bacteria) |
Low (44.4) |
A cross-sectional study was conducted among 317 migrant food handlers from Ipoh, Kuala Terengganu, and Shah Alam to assess the Salmonella prevalence of this group, resulting in nine (2.8%) people testing positive. Seven out of these nine cases presented multidrug resistance towards trimethoprim–sulfamethoxazole (six cases), streptomycin (seven cases), ampicillin (four cases), chloramphenicol (four cases), sulphonamides (six cases) and tetracycline (seven cases). |
| Tanabe et al32 | Mixed-method** | N/A† | Asylum seekers and refugees | Participants per method¶ (422 Myanmar—survey; 66 Myanmar—focus group; 6 people†—interviews; 4 facility assessments) |
Living conditions | Service environment (healthcare utilisation) |
N/A | A multiple-country study was conducted to explore barriers regarding family planning services among refugees, where the main challenges included lack of understanding and misinformation concerning contraceptives, language barriers, financial issues, detention concerns, and distance of service delivery points. |
| Ratnalingam et al72 | Prevalence (Des-2) |
N/A† | Foreign workers | 207 patients† | Disease and injury | Communicable disease (bacteria) |
Low (33.3) |
A total of 207 patients from four different hospitals in Malaysia were enrolled in the study to describe the characteristics and risk factors of microbial keratitis. More than one-fourth of the cases were due to work-related traumas, where 34.2% of these cases were among male migrant workers. |
| Woh et al47 | Prevalence (Des-2) |
N/A† | Foreign workers |
383 swab samples†† (Indians, Nepalese, Indonesians, Bangladeshi, Myanmar, Pakistani, Sri Lankans, Thai, Vietnamese) |
Risk behaviour | Hygiene and sanitation (food preparation) |
Low (22.2) |
A total of 383 hand swabs were obtained from migrant food handlers to investigate the prevalence of aerobic place counts, Staphylococcus aureus, and Escherichia coli, resulting in 99.5%, 64.4%, and 20.8% testing positive, respectively. In general, levels of the first two exceeded the acceptable standard. Infection rates were significantly higher among food handles from India compared food handlers from Nepal. In addition, significant higher rates were found among cooks, followed by waiters, compared with managers. |
| Noor and Shaker73 | Analytical cross-sectional (Obs-4)‡‡ |
N/A† | Foreign workers | 119 Indonesians | Disease and injury | Mental health (stress) |
High (85.7) |
A sample of 119 migrant workers were examined to explore the relationship between psychological distress and workplace discrimination, and the effect of coping strategy on stress levels. The study showed that workplace discrimination increased levels of stress. In addition, problem-oriented coping strategies were related to lower stress levels, while the emotional and avoidance coping strategy was associated to higher levels of stress. |
| Noordin et al74 | Prevalence (Des-3) |
September 2014–August 2015 | Foreign workers |
484 foreign labour (246 Indonesians, 103 Nepalese, 69 Bangladeshi, 51 Indians, 14 Myanmar, 1 Vietnamese) |
Disease and injury | Communicable disease (parasite) |
Low (33.3) |
Lymphatic filariasis prevalence among foreign labour was determined by screening 484 migrant workers, showing that 6.8% and 2.1% suffered from bancrofitian filariasis and brugian filariasis, respectively. |
| Sahimin et al75 | Prevalence (Des-2) |
September 2014–August 2015 | Foreign workers |
484 people (247 Indonesians, 99 Nepalese, 72 Bangladeshi, 52 Indians, 14 Myanmar) |
Disease and injury | Communicable disease (parasite) |
Low (44.4) |
A total of 484 foreign workers were sampled to describe the prevalence of Toxoplasma gondii and factors related to higher infection rates. In total, 278 migrant workers (57.4%) tested positive for T. gondii, where significant higher levels of infection were associated with Nepalese origin, newly arrived in Malaysia, and working in manufacturing. |
| Labao et al76 | Prevalence (Des-3) |
N/A† | Foreign workers | 60 Filipinos | Disease and injury | Injury (physical syndrome) |
Moderate (55.6) |
A cross-sectional study was conducted to investigate which body regions were presenting the most work-related musculoskeletal complaints among migrant workers. The major affected areas included the shoulder (60%), lower back (60%), upper back (48.3%) and neck (45%) regions. |
| Shaw et al91 | Randomised controlled trial (Exp-2) |
N/A† | Asylum seekers and refugees | 39 Afghans | Disease and injury | Mental health (stress) |
Low (30.8) |
In order to assess the impact of cognitive behavioural therapy on emotional distress, an 8-week intervention was conducted among 39 female refugees. As a result, the intervention significantly lowered levels of posttraumatic stress, anxiety. emotional distress and depression. |
| Abdul Rahman et al44 | Case control (Obs-3) |
N/A† | Unclassified migrants§§ |
61 people (52 Myanmar, 9 Others†) |
Risk behaviour | Poor nutrition (nutrition deficiency) |
Moderate (60.0) |
A case control study was conducted to determine the factors that were related to bilateral leg swelling among detained irregular migrants. Out of the 226 inmates, 21 Myanmar were identified as cases and were compared with 41 controls from Myanmar, Indonesia, Nepal and Vietnam. The study showed that the illness was caused due to a thiamine deficiency, as the patients lacked the consumption of meat. Intravenous and oral thiamine treatment was provided, and the patients responded well to it. |
| Sahimin et al77 | Prevalence (Des-2) |
September 2014–August 2015 | Foreign workers |
388 people (167 Indonesians, 81 Nepalese, 70 Bangladeshi, 47 Indians, 23 Myanmar) |
Disease and injury | Communicable disease (parasite) |
Low (44.4) |
A sample of 388 foreign workers was examined to describe the prevalence of Giardia duodenalis and Cryptosporidium parvum, showing that 42 people (10.8%) and 12 people (3.1%) tested positive, respectively. Indonesian nationality, work in the manufacturing and service sector, and newly arrived in Malaysia were significantly associated with G. duodenalis, while C. parvum was only significantly associated with employment in the food industry. |
| Nwabichie et al45 | Prevalence (Des-2) |
N/A† | Unclassified migrants |
320 people† (50% Nigerians, 15% Ghanaians, 35% Others (from Sudan, Tanzania, Kenya and South Africa)) |
Risk behaviour | Sexual behaviour (HPV knowledge) |
High (77.8) |
In total, 320 African female migrants were surveyed to investigate risk factors that are related to higher HPV risk behaviour. Only 27.2% of the sample obtained cervical cancer screening, where higher levels of screening were significantly associated with having knowledge regarding cervical cancer, being married, having a standard healthcare provider, and no perceived barriers when obtaining the check-up. |
| Jeffree et al78 | Case control (Obs-3) |
N/A† | Foreign workers | 470 people† | Disease and injury | Communicable disease (parasite) |
Moderate (60.0) |
A case-control study was conducted to determine the risk factors related to a malaria outbreak, where rubber tappers—including one migrant worker—presented a higher infection rate. |
| Zerguine et al79 | Analytical cross-sectional (Obs-4) |
June 2016–September 2016 | Foreign workers |
323 people (155 Bangladeshi, 126 Indonesians, 25 Pakistani, 11 Nepalese, 6 Chinese) |
Disease and injury | Injury (physical trauma) |
Moderate (57.1) |
A total of 323 migrant workers were sampled to investigate the prevalence and causes of workplace injuries, and examine the relationship between these traumas and safety commitment variables. The study showed that 22.6% of the foreign workers suffered from a work-related injury, mostly due to falls from heights (31.5%), and that there was a significant association between various injuries and different safety commitment-related variables, such as safe equipment and safety training. |
| Ya’acob et al80 | Randomised controlled trial (Exp-2) |
N/A† | Foreign workers | 54 Indonesians | Disease and injury | Injury (Physical syndrome) |
Low (38.5) |
A workplace intervention was conducted to assess the effect of Kiken Yochi training on musculoskeletal symptoms among foreign workers, where the study showed that the intervention significant decreased musculoskeletal symptoms in feet and ankle areas compared with the control group. |
| Chuah et al¶ | Qualitative (Qual-2) |
July 2016–November 2017 | Asylum seekers and refugees | 20 stakeholders¶¶ | Living conditions | Service environment (healthcare utilisation) |
High (80.0) |
Twenty stakeholders were interviewed to explore the barriers that refugees and asylum seekers encounter during healthcare utilisation, showing that cultural competency, insufficient health literacy, healthcare expenses, and not being aware of their rights were the main challenges. |
| Loganathan et al33 | Qualitative (Qual-2) |
July 2018–September 2018 | Foreign workers | 18 stakeholders¶¶ | Living conditions | Service environment (healthcare utilisation) |
High (80.0) |
A qualitative study with 18 stakeholders demonstrated that migrant workers face several complications with respect to utilising healthcare, including financial issues, discrimination, lack of valid passports and work permits, cultural competency, and physical barriers. |
| Rahman et al34 | Prevalence (Des-3) |
N/A† | Foreign workers | 314 Bangladeshi | Living conditions Disease and injury |
Service environment (healthcare utilisation) Various diseases (various diseases) |
Low (33.3) |
A group of 314 migrant workers were sampled to present the distribution of diseases and healthcare utilisation pattern. Fever and sprains were the most reported diseases among the group that suffered from an illness in the last 2 weeks, while fever and gastrointestinal diseases were the most prevalent among the group that suffered from an illness in the last month. In addition, the majority (approx. 60%) visited hospitals to seek treatment. |
| Siah et al36 | Qualitative (Qual-3) |
N/A† | Asylum seekers and refugees | 8 stakeholders (5 refugees,† 3 locals) |
Living conditions | Social environment (prejudice) |
Low (50.0) |
Eight people stakeholders were interviewed to explore the forms of discrimination that refugee children experience. The study shows that refugee children suffer from denied access to healthcare, not receiving proper education, and being judged by their social environment. |
| Sahimin et al81 | Prevalence (Des-2) |
September 2014 and August 2015 | Foreign workers |
610 people (246 Indonesians, 99 Nepalese, 72 Bangladeshi, 52 Indians, 14 Myanmar) |
Disease and injury | Communicable disease (parasite) |
Low (33.3) |
Four different diagnostic tests were applied to identify Strongyloides stercoralis among migrant workers, where prevalence rates differed between 0.8% and 35.8% |
| Chuah et al35 | Qualitative (Qual-2) |
July 2016–January 2018 | Asylum seekers and refugees | 20 stakeholders¶¶ | Living conditions | Service environment (healthcare utilisation) |
High (80.0) |
Twenty stakeholders were interviewed to identify the challenges with respect to accessing healthcare among refugees, showing that out of pocket healthcare spending, language and cultural competency barriers, and access to medication are the top healthcare challenges. |
*Includes irregular migrants.
†Data to present detailed information are lacking.
‡Includes children of migrant workers, which is according to the IOM (2011) definition still classified as migrant workers.
§Ambigious reporting of the data.
¶Includes a multiple-country study, and, therefore, subjects that were included in countries other than Malaysia are not reported in this table.
**Level of evidence and quality appraisal are not available for this study design.
††Number of samples might not be similar to the number of study participants.
‡‡Despite of lacking a comparison group, this study was identified as an analytical cross-sectional study due to the aim—testing two hypotheses—and comprehensive statistical analysis.
§§Includes detained migrants.
¶¶Representing the population of interest (as shown in the ‘type of migrant’ category).
***Sample population in italic represents the migrant population.
†††Includes refugees, international students, expats and unclassified migrants.
‡‡‡Includes three expats.
§§§Includes an international student.
¶¶¶Includes six transnational marriage migrants.
HPV, human papilloma virus; N/A, data not available; UNHCR, United Nations High Commissioner for Refugees.
Health dimension and type of migrant
The literature was first assessed to understand the trends and topical coverage of research against the six dimensions of the BARHII public health framework. The first dimension, social inequities, was used to describe the population of interest and refers to the type of migrant (eg, foreign workers, asylum seekers and refugees, or unclassified migrants). The other five dimensions focused on elements that influence the health status of the population of interest, including institutional inequities, living conditions, risk behaviour, disease and injury and mortality and morbidity. These latter five categories are outlined below and include results on the types of migrants researched within these dimensions. Figures 4 and 5 present overviews of the number of studies disaggregated by health dimension and type of migrant, respectively.
Figure 4.
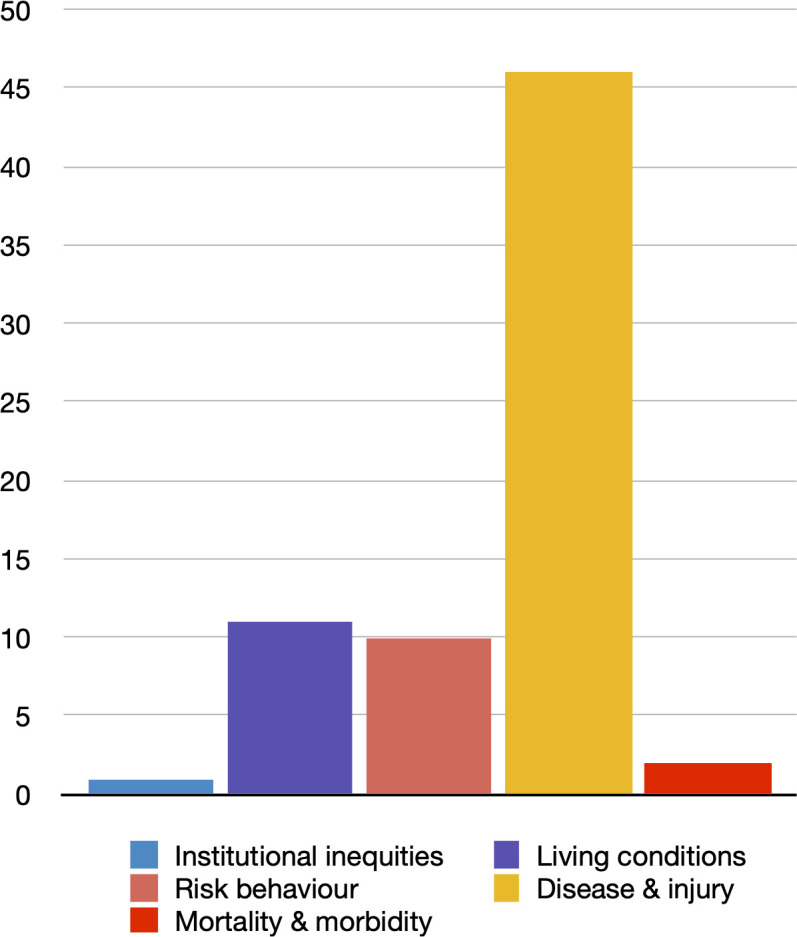
Number of studies disaggregated by health dimension.
Figure 5.
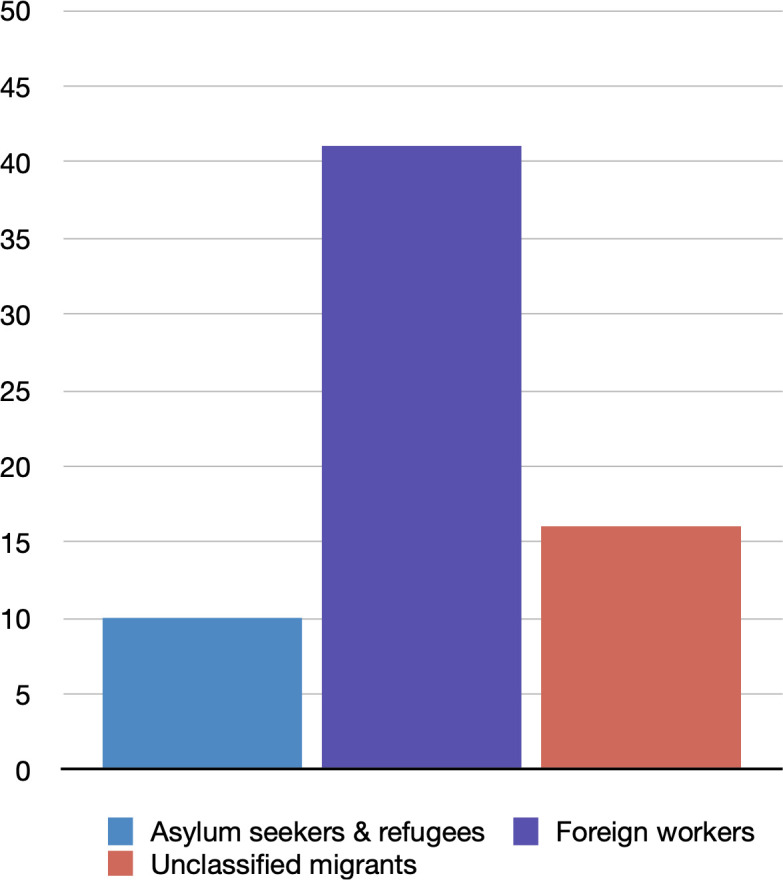
Number of studies disaggregated by type of migrant.
Institutional inequities
One paper addressed the institutional inequities dimension27 by exploring the inclusion of migrant workers into national universal health coverage (UHC) policies in five countries of the Association of Southeast Asian Nations: Indonesia, Philippines, Malaysia, Thailand and Singapore. The researchers stated that Malaysia has implemented a medical insurance policy for foreign labour by obligating documented migrant workers to be enrolled in private insurance schemes, as non-citizens have no access to UHC at public facilities.
Living conditions
Eleven papers were classified under the living conditions dimension, where most articles (n=9/11) addressed the service environment subdimension.8 28–35All of these papers studied the asylum seeker and refugee population, except for one article that focused on migrant workers.33 Half the studies used qualitative methods to explore barriers to healthcare utilisation and showed that language difficulties, discrimination, insufficient health literacy and cultural differences were common issues. One study focused on the social environment subdimension and showed that refugee children experienced discrimination by locals and other refugees of different ethnicities and national origins, such as stereotyping them as criminals.36 Santos et al37 assessed elements related to the work environment subdimension by investigating perceived environmental hazards among foreign workers, demonstrating that noise and dust were perceived as the greatest occupational health threats.
Risk behaviour
Ten studies researched the risk behaviour dimension, with most articles (n=8/10) conducted on general migrant populations without clear identification of which migrant categories were included in their study.38–45 Three of these articles focused on the sexual behaviour subdimension, exploring risk behaviour related to human papillomavirus (HPV). The studies showed that a significant number of migrant women have high HPV risk behaviour due to lack of understanding with respect to cervical cancer, the screening process, and poor knowledge concerning HPV vaccination.41 42 45 Two papers, classified within the poor nutrition subdimension, showed poor health outcomes among detained migrants due to nutrition deficiencies.39 44 The other articles among unclassified migrants included two studies on violence and abuse, exploring maternal filicide43 and neglecting children38; and one study on alcohol and other drugs, pertaining to inhalants’ usage.40 These three studies simply showed that migrants represent a certain proportion of the identified cases. Only the study on the use of inhalants presented more cases among migrants than locals. Two final studies included foreign workers and explored the hygiene and sanitation and hazard and safety awareness subdimensions.46 47 Kamaludin and How46 stated that migrant workers had significantly less knowledge regarding environmental health, such as air quality, natural hazards, sanitation and industrial hazards, compared with local workers. Woh et al47 investigated the level of hygiene among migrant food handlers and argued that personal hygiene and sanitation measures should be improved among this population.
Disease and injury
With a total of 46 studies, the disease and injury dimension presented the largest study field of interest related to the BARHII framework. Most articles (n=36/46) studied foreign workers,34 37 48–81 while only six and four articles included unclassified migrants82–87 and refugee populations,88–91 respectively. The majority (n=27/46) of the articles studied communicable diseases, where 18 of these studies focused on parasites,48 50 51 54–58 64 68 69 74 75 77 78 81 82 89 eight on bacteria,53 65 71 72 83 85–87 and two on viruses.61 87 Most of the studies were descriptive and presented that migrants, irrespective of the defined type, represented a significant share among the study populations. Non-communicable diseases were studied far less compared with communicable diseases and were only specifically addressed in three articles.59 67 88 Scheutz et al88 found high numbers of different non-communicable oral complications among Vietnamese refugees, such as tooth decay and missing teeth. Kugan et al67 compared the difference in characteristics between foreign workers and Malaysian patients with perforated peptic ulcers, showing that the treated foreign labour population were younger, experienced fewer postoperative complications, and had smaller-sized ulcers compared with locals. Murty59 reported a case study, presenting a deceased migrant worker due to a cystic tumour in the heart region.
In addition to the studies that focused on single disease outcomes, two studies were conducted that presented distributions of various diseases among foreign workers, including communicable and non-communicable disorders.34 52 Five studies focused on the mental health subdimension, where these studies concentrated on describing psychiatric disorders,49 determining quality of life-related risk factors,84 90 and testing the effect of different coping mechanisms and therapy sessions on the level of stress.73 91 Nine studies explored the injury subdimension, where nearly all (n=8/9) studies focused on work-related injuries. Most of these studies examined the prevalence of particular injuries and traumas, including fatal lightning strikes,60 ocular traumas,70 and musculoskeletal pain.37 66 76 Ratnasinga et al63 compared the number of occupational incidents between local workers and migrant workers, where foreign workers had less accidents. In addition, two papers described risk factors for work-related injuries, such as high machine-related vibration exposure62 and low levels of the company’s safety commitment (as assessed by foreign workers themselves).79 Ya’acob et al80 conducted an RCT to evaluate the impact of a specific workplace intervention on musculoskeletal symptoms (MMS) among foreign labour and showed that the intervention reduced MMS in the foot and ankle regions significantly compared with the control group.
Mortality and morbidity
Two papers addressed the mortality and morbidity dimension by showing incidence rates among general cohorts of migrants. Zulkifli et al28 conducted a study on maternal and child health in Sabah and identified that infant mortality rates were significantly higher for migrants compared with locals. Dony et al92 also conducted a study in Sabah and showed that at least 24% of new tuberculosis cases detected since 1990 were among migrants and that leprosy incidence rates among migrants were on average 3.7 times higher than incidence rates among Malaysians.
Level of evidence and quality of the study
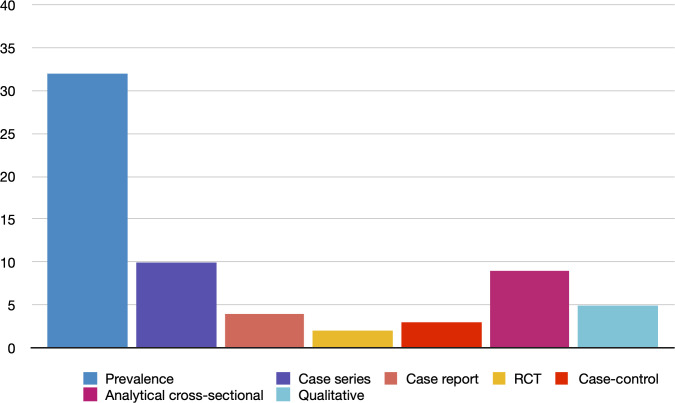
In total, 65 articles were included in the quality assessment; tables 6 and 7 show the mean quality scores of the papers disaggregated by BARHII dimension and level of evidence, respectively. Two articles—representing a scoping review27 and mixed-method design32—were excluded from this assessment, as the JBI toolkit does not accommodate these study designs. The quality assessment scores can be found in online supplemental file 3. In addition, figure 6 shows an overview of the number of studies disaggregated by research design.
Table 6.
Number and average quality of included articles disaggregated by type of migrant and Bay Area Regional Health Inequities Initiative (BARHII) dimensions
| Category | Number of studies per study design with level of evidence* | Total # studies | Mean quality | References | ||||||||
| CR-4 | AC-4 | QL-3 | CS-3 | PR-3 | CC-3 | QL-2 | PR-2 | RC-2 | ||||
| Type of migrant | ||||||||||||
| Asylum seekers and refugees | – | 1 | 1 | – | 1 | – | 3 | 2 | 1 | 10† | 58.4% | 8 29 30 32 35 36 88–91 |
| Foreign workers | 4 | 7 | – | 4 | 10 | 1 | 1 | 12 | 1 | 41‡ | 45.7% | 27 31 33 34 37 46–81 |
| Unclassified migrants | – | 1 | – | 6 | 2 | 2 | – | 5 | – | 16 | 52.7% | 28 38–45 82–87 92 |
| Dimension of BARHII framework | ||||||||||||
| Institutional inequities | – | – | – | – | – | – | – | – | – | 1‡ | – | 27 |
| Living conditions | – | 2 | 1 | – | 1 | – | 4 | 2 | – | 1† | 59.7% | 8 28–37 |
| Risk behaviour | – | 1 | – | 3 | 1 | 1 | – | 4 | – | 10 | 48.7% | 38–47 |
| Disease and injury | 4 | 6 | – | 7 | 11 | 2 | – | 14 | 2 | 46 | 46.3% | 34 37 48–91 |
| Mortality and morbidity | – | 1 | – | – | 1 | – | – | – | – | 2 | 47.9% | 28 92 |
| Subdimensions of institutional inequities | ||||||||||||
| Laws and regulations | – | – | – | – | – | – | – | – | – | 1‡ | – | 27 |
| Subdimensions of living conditions | ||||||||||||
| Social environment | – | – | 1 | – | – | – | – | – | – | 1 | 50.0% | 36 |
| Economic and work environment | – | – | – | – | – | – | – | 1 | – | 1 | 44.4% | 37 |
| Service environment | – | 2 | – | – | 1 | – | 4 | 1 | – | 9‡ | 62.8% | 8 28–35 |
| Subdimensions of risk behaviour | ||||||||||||
| Poor nutrition | – | – | – | 1 | – | 1 | – | – | – | 2 | 50.0% | 39 44 |
| Violence and abuse | – | – | – | 2 | – | – | – | – | – | 2 | 70.0% | 38 43 |
| Alcohol and other drugs | – | – | – | – | – | – | – | 1 | – | 1 | 22.2% | 40 |
| Sexual behaviour | – | – | – | – | 1 | – | – | 2 | – | 3 | 50.9% | 41 42 45 |
| Hygiene and sanitation | – | – | – | – | – | – | – | 1 | – | 1 | 22.2% | 47 |
| Hazard and safety awareness | – | 1 | – | – | – | – | – | – | – | 1 | 50.0% | 46 |
| Subdimensions of disease and injury | ||||||||||||
| Communicable disease | 3 | 2 | – | 6 | 4 | 2 | – | 10 | – | 27 | 44.2% | 48 50 51 53–58 61 64 65 68 69 71 72 74 82 83 85–87 89 |
| Non-communicable disease | 1 | 1 | – | – | 1 | – | – | – | – | 3 | 50.8% | 75 77 78 81 |
| Injury | – | 2 | – | 1 | 3 | – | – | 2 | 1 | 9 | 47.4% | 59 67 88 |
| Mental health | – | 1 | – | – | 1 | – | – | 2 | 1 | 5 | 56.1% | 37 60 62 63 66 70 76 79 80 |
| Various diseases | – | – | – | – | 2 | – | – | – | – | 2 | 38.9% |
49 73 84 90 91 34 52 |
| Subdimensions of mortality and morbidity | ||||||||||||
| Mortality rates | – | 1 | – | – | – | – | – | – | – | 1 | 33.3% | 28 |
| Morbidity rates | – | – | – | – | 1 | – | – | – | – | 1 | 62.5% | 92 |
| Total | 4 | 9 | 1 | 10 | 13 | 3 | 4 | 19 | 2 | 67†, ‡ | 49.2% | 8 27–92 |
*Level of evidence ranks from 1 to 4, where 1 is the highest level of evidence and 4 is the lowest level.
†Includes a mixed-method design, which was not appraised for level of evidence nor quality of the study.
‡Includes a scoping review design, which was not appraised for level of evidence nor quality of the study.
AC-4, analytical cross-sectional study; CC-3, case control; CR-4, case report; CS-3, case series; PR-2, prevalence study with analytical component; PR-3, prevalence study without analytical component; QL-2, qualitative study with more rigour; QL-3, qualitative study with less rigour; RC-2, randomised controlled trial.
Table 7.
Number and average quality of included articles disaggregated by research design category
| Research design | Level of evidence | Included studies | Mean quality | References |
| Descriptive research | ||||
| Systematic review of descriptive studies | 1 | – | – | – |
| Prevalence study with analytical component | 2 | 19 | 39.7% | 31 37 40 42 45 47 53 61 63 68 69 72 75 77 81 84 87 89 90 |
| Case series | 3 | 10 | 46.7% | 38 39 43 54 57 60 65 82 83 85 |
| Prevalence study without analytical component | 3 | 13 | 49.8% | 34 41 48 49 51 52 66 70 71 74 76 88 92 |
| Case report | 4 | 4 | 81.5% | 50 55 59 64 |
| Total | 46 | 47.7% | 31 34 37–43 45 47–55 57 59–61 63–66 68–72 74–77 81–85 87–90 92 | |
| Experimental research | ||||
| Systematic review/meta-analysis of experimental studies | 1 | – | – | – |
| Randomised controlled trial | 2 | 2 | 34.7% | 80 91 |
| Group quasi-experimental study (non-randomised) | 3 | – | – | – |
| Quasi-experimental study with single subject | 4 | – | – | – |
| Total | 2 | 34.7% | 80 91 | |
| Observational research | ||||
| Systematic review/meta-analysis of observational studies | 1 | – | – | – |
| Cohort study | 2 | – | – | – |
| Case-control | 3 | 3 | 56.7% | 44 78 86 |
| Analytical cross-sectional study | 4 | 9 | 42.6% | 28 30 46 56 58 62 67 73 79 |
| Total | 12 | 46.1% | 28 30 44 46 56 58 62 67 73 78 79 86 | |
| Qualitative research | ||||
| Systematic review/meta-synthesis of qualitative studies | 1 | – | – | – |
| Group qualitative studies with more rigour | 2 | 4 | 82.5% | 8 29 33 35 |
| Group qualitative studies with less rigour | 3 | 1 | 50.0% | 36 |
| Qualitative study with a single informant | 4 | – | – | – |
| Total | 5 | 76.0% | 8 29 33 35 36 | |
| Total | 67* | 49.2% | 8 27–92 | |
*Includes a mixed-method design and a scoping review, which were both not assessed for the level of evidence nor quality appraisal.
Figure 6.
Number of studies disaggregated by research design.
bmjopen-2020-041379supp003.pdf (84.6KB, pdf)
In general, the quality of the evidence base on migrant health in Malaysia is low (49.2%) and consists mostly of level 3 evidence papers (n=27/65). Level 2 evidence represents 38.5% of the evidence base (n=25/65), followed by level 4 evidence papers (n=13/65). No level 1 evidence studies (systematic reviews or meta-analyses) were identified. The majority of the papers (n=41/65) focused on foreign workers; however, studies that included asylum seekers and refugees have the highest mean quality (58.4%). Furthermore, only four out of five BARHII health dimensions were included in the quality assessment. The living conditions dimension has the highest average score (59.7%), followed by the risk behaviour dimension (48.7%), mortality and morbidity dimension (47.9%), and the disease and injury dimension (46.3%). Moreover, the descriptive research category represents the majority (70.8%) of the evidence base with a mean quality of 47.7%. The qualitative research category has the highest mean quality and is the only research category with a high-quality score (76%).
Associations between different variables
Figure 7 presents the results of the MCA, showing different associations between four dimensions: (1) type of study design; (2) quality of the study; (3) type of migrant; and (4) main health dimension. χ2 test results were used to assess whether categorical variables were independent.
Figure 7.
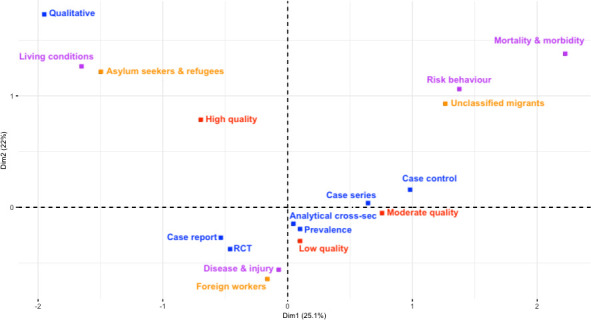
Results of the multiple-correspondence analysis.
High-quality studies tend to include refugees and asylum seekers (χ2=17.005, df=4, p=0.001928), focus on living conditions (χ2=131.94, df=6, p<0.001), and have a qualitative research design (χ2=656.35, df=12, p<0.001). Moreover, studies that included foreign workers tend to focus on diseases and injuries (χ2=374.52, df=6, p<0.001) and contain a case report study design (χ2=576.87, df=12, p<0.001). Furthermore, research that included the unclassified migrant population tend to study the risk behaviour, and mortality and morbidity dimensions (χ2=374.52, df=6, p<0.001). Lastly, prevalence studies, and, to a lesser extent, analytical cross-sectional studies, tend to have a low-quality score (χ2=656.35, df=12, p<0.001).
Discussion
Key findings
This study mapped the existing academic literature on migrant health in Malaysia and assessed the quality and level of evidence of these scientific studies. The majority of these studies focus on the ‘disease and injury’ dimension, especially infectious diseases, and includes mostly foreign workers. Two health dimensions (institutional inequality, and morbidity and mortality) as well as various subdimensions of each health dimension are lacking substantial research. In addition, only a few papers include the asylum seeker and refugee population, and a vast amount do not provide any details to classify the type of migrant. The average quality of the papers was low, yet quality differed significantly among the studies. High-quality studies were mostly qualitative designs that included refugees and focused on living conditions, while prevalence and analytical cross-sectional studies were mostly low quality. In terms of research trends, no specific changes in type of migrant, health dimension or quality of the study have been observed over the last six decades. However, it should be noted that qualitative research made its entry in the early 2010s and made up a vast amount of the papers published in recent years. Future research priorities based on the existing evidence and identified gaps are summarised in box 1.
Box 1. Main recommendations to improve future research on migrant health.
Recommendation
Improve the description of the target migrant population by including information regarding the type of migrant (eg, foreign worker, refugee), visa status (eg, regular, irregular), country of origin, socioeconomic variables (eg, level of education, income), mode of transport during migration journey (eg, boat, car) and the existence of forced entry (eg, human trafficking, forced marriage).
Create associations between different stages of migration (predeparture, travel, destination, interception and return phase) and health outcomes.
More research output concerning governance and institutional inequities and mortality and morbidity, and, consequently, conduct a time series analysis between these two dimensions to identify and possible relationships.
More research output regarding non-communicable diseases, especially on the main causes of death in Malaysia; cardiovascular diseases, chronic respiratory diseases and diabetes.
More research output concerning several subdimension of risk behaviour, especially on smoking, physical inactivity, and alcohol abuse.
Evaluate the impact of health and non-health policies on migrant health.
Explore living conditions regarding the physical environment, such as housing and environmental conditions, and the impact on migrant health outcomes.
Promotion of guidelines on study conduct and reporting among researchers.
Among the five BARHII health dimensions, institutional inequities, and mortality and morbidity were the least represented. Yet, studies concerning the influence of governance on migrant health are of utmost importance, as overarching governance can affect health outcomes of the other BARHII dimensions.93 94 Similarly, epidemiological research on mortality and morbidity rates is necessary for population health statistics, to identify disease patterns, document changes over time and inform plans of action to tackle these health issues.95 Further research should focus on migrant health governance, as well as epidemiological research on morbidity and mortality among both migrants and non-migrants, to better understand the effects of policies on migrant health, which is particularly relevant in low-income and middle-income countries where the evidence gap is so acute.96 Furthermore, a recent systematic review on the effects of non-health-targeted policies on migrant health in high-income countries showed that non-health policies (eg, restrictive immigration policies) were associated with poor health outcomes.97 It is therefore important that policies in other sectors (potentially including, eg, immigration, labour, education) are also assessed for their potential consequences for migrant health.
Living conditions were represented in 11 studies and focused mainly (n=9/11) on the service environment by addressing the healthcare setting. However, there is scarce information on the social and economic environments that different categories of migrants must navigate and no data on the physical environment at all. Research conducted in other countries demonstrates the importance of these three subdimensions on migrant health.98–100 Shao et al98 argued that inequalities regarding the level of income (economic environment) influenced health outcomes among internal migrant workers in China. He and Wong99 stated that poor mental health among female migrant workers in China was related to gender-specific stressors (social environment). Al-Khatib et al100 demonstrated that poor housing conditions (physical environment) in a refugee camp were directly associated with various upper respiratory tract diseases. These studies underscore the importance of different environments on migrant health, motivating a focus of future research on the health impact of living conditions other than healthcare utilisation.
Ten studies were conducted on risk behaviour with different subdimensions, from hygiene and sanitation to violent and abusive behaviour. However, all of these subdimensions were under-researched, as only limited elements of each subdimension were discussed. For instance, three studies focused on sexual behaviour by addressing HPV knowledge.41 42 45 Yet, no attention was given to other sexual behaviour-related topics, such as condom use, HIV knowledge and birth control. Although these studies have been conducted in Malaysia, this research is lacking in the migration context.101–103 Therefore, future research should focus on broader aspects of each subdimension, as demonstrated in research elsewhere. For example, Renzaho and Burns104 addressed the poor nutrition subdimension by showing that dietary patterns among African migrants changed negatively after arriving in Australia due to the increased intake of fast food and processed food. Ganle et al105 concentrated on the sexual risk behaviour subdimension and stated that 71% of the sampled refugees in Ghana had transactional sex, and only 12% used contraceptives. Bosdriesz et al106 compared smoking between migrants and non-migrants in the USA and showed that migrants smoked less than US citizens. As a significant number of migrants in Malaysia come from Indonesia, a population that smokes almost twice as much as Malaysians, smoking behaviour among this migrant group may differ from locals.107 Therefore, future research should further explore the differences in other risk behaviours, such as smoking, between Malaysians and migrants in Malaysia.
Disease and injury was the most researched dimension, representing more than two-thirds of the evidence base on migrant health in Malaysia. Despite the strong representation, over half the research papers concentrated on communicable diseases, while only a few examined non-communicable diseases, consistent with global research output on international migrant workers.108 As the WHO109 states that approximately 74% of all deaths in Malaysia are attributable to non-communicable disease, in particular cardiovascular disease, chronic respiratory disease and diabetes, there is a need to expand research on non-communicable disease trends and outcomes among the migrant population in Malaysia.
We found that the majority of studies involved foreign workers (n=41/67), and only 10 studies examined asylum seekers and refugees as the primary population of interest. Our findings, therefore, offer useful synthesis on migrant worker’s health specifically, which is lacking relative to studies on asylum seekers and refugees in global migration health research.13 Furthermore, 11 studies did not specify the included migrant population. This issue could have occurred due to missing information on the type of migrant in the dataset that the researchers used for their studies. For example, the Ministry of Health (MOH) will not report anything more detailed than ‘non-Malaysian,’ as no further information on non-citizens are collected during patient registration at MOH facilities. Ideally, all research on migrants should clearly specify the type of migrants being studied and not omit crucial details, such as gender, visa status and country of origin. Also, human trafficking could significantly affect a person’s health and vulnerability, yet, there is very little known about the health issues experienced by trafficked persons in Malaysia.110 While the vulnerabilities experienced by trafficked persons intersect with other migration-related vulnerabilities like gender, ethnicity or documentation status, victims of human trafficking should be categorised separately, to reflect their own unique status and vulnerability. The travel routes or modes of transportation used by migrants to come to Malaysia may influence migrant health in different ways a well, as different routes or modes of transportation may be linked with specific hazards. Related to this issue is the lack of evidence on migrant health with specific stages of migration, including predeparture, travel, destination interception and return, where health outcomes might differ between these stages.111
Lastly, this scoping review revealed that the average quality of studies on migrant health in Malaysia is poor (49.2%) and that most of these studies have level 3 (n=27/65) or level 2 (n=25/65) evidence. Only qualitative studies with more rigour (level 2 evidence) and those that focus on living conditions and include the refugee and asylum seeker populations, tend to have a high-quality score. Therefore, there is a clear need to conduct research that will provide strong evidence to support practices and policies that will positively impact migrant health. Creating standard research design-specific guidelines, if not existing already, and, subsequently, promoting these materials among academics and research institutions, could increase the quality of future research work. Furthermore, researchers should follow study design specific reporting guidelines, to ensure that all relevant information is captured in publications for further evidence synthesis, such as this review.
Limitations
This study is the first systematic literature synthesis and scoping review on migrant health in Malaysia and presents a comprehensive overview of all identified peer-reviewed articles that met the inclusion criteria. Specific recommendations based on this research are provided to improve the evidence base on migrant health in Malaysia. Furthermore, we used a self-developed decision tree and modified JBI checklists to help identify the type of study design and corresponding level of evidence of the included studies. We found this evidence assessment framework to be useful for the quality assessment of migrant health-related studies, and it might be useful for other research fields as well. Yet, our review has several limitations. As this paper focuses exclusively on vulnerable migrants within the non-citizen population in Malaysia, we excluded other non-citizen groups, such as expatriates and international students, based on the assumption that these groups are less vulnerable (eg, expatriates in Malaysia have more privileges in terms of recognition regarding their roles in society, receive better financial compensation and tend to have access to many other benefits compared with foreign workers). However, we acknowledge that other non-citizen groups may face challenges in obtaining proper healthcare in Malaysia as well, such as issues related to cultural competency among foreign students and retirees.112 113 In addition, papers including non-citizens without further description were excluded, although these studies may have included the vulnerable migrant population.
Only academic peer-reviewed studies were included, thus excluding grey literature, editorials and opinion papers. Also, only English language articles were included, resulting in the exclusion of one identified paper in Bahasa Malaysia (the Malay language).114 Aggravating the issue, other Malaysian articles might not have been identified due to the lack of Malaysian keywords in the search strategy. As a result, much relevant information that could potentially be used to inform both policies and practice, as well as to make this review more comprehensive, may have been excluded from this review.
Inter-rater reliability was limited to a 20% sample of the records in the first (abstract and title) screening stage, and no data extraction nor quality assessment was verified by a second reviewer due to time and resource constraints. Yet, we anticipate low selection bias as the health dimensions in the BARHII framework present clear distinctions between each other, and most of the included papers used objective indictors. For example, when a paper was measuring the knowledge and awareness regarding the pap smear test among female migrants, it would be classified as a ‘risk behaviour’ study. Furthermore, we believe that the development of the decision tree and additional objective criteria for the JBI tools—an example was given earlier in table 4—reduced the subjectivity of this study, and, hence, increases the reliability. Yet, future research is needed to validate both the decision tree and modified JBI toolkit.
Besides the BARHII framework, various conceptual public health models are available, and these models may include different (sub)dimensions. For instance, the WHO Commission on Social Determinants of Health framework includes material circumstances, such as food availability, whereas this dimension is not included in the BARHII framework.115 Similarly, critical appraisal tools other than the JBI toolkit are available, which could address different points to determine the quality of the study. Therefore, it would be helpful to assess other public health models and critical appraisal tools to see if they include additional elements (eg, food availability) that would be beneficial for future studies.
Likewise, a decision tree was developed by using the characteristics of the used definitions of different research designs as well as the specific traits of Tomlin and Borgetto’s24 level of evidence model. Using other definitions and level of evidence models could result in a different level of evidence categorisation. However, we believe this review makes a strong methodological contribution by combining study designs and level of evidence in a unified decision tree, which can be used by researchers conducting systematic or scoping reviews where accurate classification of the study design and associated evidence level, is important.
In order to conduct the MCA, the dataset could only include one unit per dimension for each paper. As some studies included multiple BARHII dimensions, only the most prominent dimension was included in the analysis. As a result, the analysis may suffer from some selection bias and present slightly different outcomes compared with an analysis that includes the other BARHII dimensions.
Lastly, no adjustments were made for outliers in the quality assessment. Therefore, some papers with extremely high or low scores could have influenced specific dimensions and might not reflect the quality of those dimensions perfectly.
Conclusion
Migrant health remains an issue in Malaysia, yet, the quality of the evidence needed to inform policies is currently lacking. Research-specific reporting guidelines should be followed to improve the credibility and quality of the evidence base. Furthermore, future research should focus more on evidence gaps in the mortality and morbidity, and institutional inequities dimensions, and certain subdimensions, such as non-communicable diseases, housing conditions and physical inactivity, to provide a comprehensive picture of migrant health in Malaysia. Apart from demonstrating the research gaps, this paper also makes methodological contributions to migrant health research by providing a modified JBI toolkit and a decision tree that identifies the type of study design and corresponding level of evidence, both of which can be used in other research fields as well.
Supplementary Material
Acknowledgments
The authors would like to thank Andrew Seko for granting them permission on behalf of the Bay Area Regional Health Inequities Initiative (BARHII) for the use of their public health framework in this scoping review. They would also like to thank Norhayati Binti Yahya for providing them with the definition for non-citizens on behalf of the Department of Statistics Malaysia (DOSM). Furthermore, they would like to thank the editor and four independent reviewers for their helpful feedback. Lastly, they would like to thank the United Nations University – International Institute for Global Health for its continuous support throughout this project.
Footnotes
Contributors: AWdS, NSP, MV and ZXC created the study protocol. AWdS and ZXC conducted abstract and full-text screening and NSP solved undisputed conflicts. AWdS extracted the data, drafted the decision tree and modified the JBI tools, and NSP, MV, ZXC and CAL provided feedback during these processes. CAL and AWdS conducted the data analysis. AWdS drafted the initial version of the manuscript and AWdS, NSP, MV, CAL, TL and ZXC critically revised and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. The prereview protocol and modified JBI checklists can be accessed on request from the first author.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.International Organization for Migration World migration report 2020. Geneva: International Organization for Migration, 2019. [Google Scholar]
- 2.International Organization for Migration Malaysia. Kuala Lumpur: International Organization for Migration, 2020. https://www.iom.int/countries/malaysia [Google Scholar]
- 3.Department of Statistics Malaysia Population quick info. Putrajaya: Department of Statistics Malaysia, 2020. https://www.dosm.gov.my/v1/index.php?r=column/cone&menu_id=b2RVUmEyZ2ZZYXhaUzUrdnpsaWozdz09 [Google Scholar]
- 4.Department of Statistics Malaysia Current population estimates Malaysia. Putrajaya: Department of Statistics Malaysia, 2019. [Google Scholar]
- 5.Office of the United Nations High Commissioner for Human Rights The rights of non-citizens. Geneva: United Nations, 2006. [Google Scholar]
- 6.Ministry of Home Affairs Malaysia Statistik pekerja asing terkini mengikut negeri DAN sektor. Putrajaya: Ministry of Home Affairs Malaysia, 2019. http://www.data.gov.my/data/ms_MY/dataset/statistik-pekerja-asing-terkini-mengikut-negeri-dan-sektor [Google Scholar]
- 7.United Nations High Commissioner for Refugees Figures at a glance in Malaysia. Kuala Lumpur: United Nations High Commissioner for Refugees, 2019. https://www.unhcr.org/en-my/figures-at-a-glance-in-malaysia.html [Google Scholar]
- 8.Chuah FLH, Tan ST, Yeo J, et al. The health needs and access barriers among refugees and asylum-seekers in Malaysia: a qualitative study. Int J Equity Health 2018;17:120 10.1186/s12939-018-0833-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devadason ES, Meng CW. Policies and laws regulating migrant workers in Malaysia: a critical appraisal. J Contemp Asia 2014;44:19–35. 10.1080/00472336.2013.826420 [DOI] [Google Scholar]
- 10.International Organization for Migration Iom Handbook: protection and assistance for migrants vulnerable to violence, exploitation and abuse. Geneva: International Organization for Migration, 2018. [Google Scholar]
- 11.Pocock NS, Suphanchaimat R, Chan CK, et al. Reflections on migrant and refugee health in Malaysia and the ASEAN region. BMC Proc 2018;12:4 10.1186/s12919-018-0100-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lasimbang HB, Tong WT, Low WY. Migrant workers in Sabah, East Malaysia: the importance of legislation and policy to uphold equity on sexual and reproductive health and rights. Best Pract Res Clin Obstet Gynaecol 2016;32:113–23. 10.1016/j.bpobgyn.2015.08.015 [DOI] [PubMed] [Google Scholar]
- 13.Sweileh WM, Wickramage K, Pottie K, et al. Bibliometric analysis of global migration health research in peer-reviewed literature (2000–2016). BMC Public Health 2018;18:777 10.1186/s12889-018-5689-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villarroel N, Hannigan A, Severoni S, et al. Migrant health research in the Republic of ireland: a scoping review. BMC Public Health 2019;19:324 10.1186/s12889-019-6651-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanlou N, Haque N, Skinner A, et al. Scoping review on maternal health among immigrant and refugee women in Canada: prenatal, intrapartum, and postnatal care. J Pregnancy 2017;2017:1–14. 10.1155/2017/8783294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 17.Bay Area Regional Health Inequities Initiative Framework. Oakland, CA: Bay Area Regional Health Inequities Initiative, 2015. http://barhii.org/framework/ [Google Scholar]
- 18.Aromataris E, Munn Z, Joanna briggs institute reviewer’s manual. Adelaide, Australia: Joanna Briggs Institute, 2017. https://wiki.joannabriggs.org/display/MANUAL/JBI+Reviewer%27s+Manual [Google Scholar]
- 19.National Academies of Sciences, Engineering, and Medicine A framework for educating health professionals to address the social determinants of health. Washington, DC: The National Academies Press, 2016. [PubMed] [Google Scholar]
- 20.Public Health England Public health outcomes framework 2019/20: a consultation. London: Public Health England, 2019. [Google Scholar]
- 21.London School of Hygiene & Tropical Medicine Which databases should I search? A guide to the most popular resources. London: London School of Hygiene & Tropical Medicine, 2014. [Google Scholar]
- 22.Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 2017;6:245 10.1186/s13643-017-0644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centre for Evidence-Based Medicine Study designs. Oxford: Centre for Evidence-Based Medicine, 2019. https://www.cebm.net/2014/04/study-designs/ [Google Scholar]
- 24.Tomlin G, Borgetto B. Research pyramid: a new evidence-based practice model for occupational therapy. Am J Occup Ther 2011;65:189–96. 10.5014/ajot.2011.000828 [DOI] [PubMed] [Google Scholar]
- 25.Greenacre M. Correspondence analysis in practice. 2nd ed. Boca Raton, FL: Chapman & Hall/CRC, 2007. [Google Scholar]
- 26.Le Roux B, Rouanet H. Multiple correspondence analysis. London: Sage, 2010. [Google Scholar]
- 27.Guinto RLLR, Curran UZ, Suphanchaimat R, et al. Universal health coverage in ‘One ASEAN’: are migrants included? Glob Health Action 2015;8:25749 10.3402/gha.v8.25749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zulkifli SN, U KM, Yusof K, et al. Maternal and child health in urban Sabah, Malaysia: a comparison of citizens and migrants. Asia Pac J Public Health 1994;7:151–8. 10.1177/101053959400700302 [DOI] [PubMed] [Google Scholar]
- 29.Mendelsohn JB, Rhodes T, Spiegel P, et al. Bounded agency in humanitarian settings: a qualitative study of adherence to antiretroviral therapy among refugees situated in Kenya and Malaysia. Soc Sci Med 2014;120:387–95. 10.1016/j.socscimed.2014.06.010 [DOI] [PubMed] [Google Scholar]
- 30.Mendelsohn JB, Schilperoord M, Spiegel P, et al. Is forced migration a barrier to treatment success? similar HIV treatment outcomes among refugees and a surrounding host community in Kuala Lumpur, Malaysia. AIDS Behav 2014;18:323–34. 10.1007/s10461-013-0494-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noh NA, Wahab HA, Bakar Ah SHA, et al. Public health services for foreign workers in Malaysia. Soc Work Public Health 2016;31:419–30. 10.1080/19371918.2015.1125321 [DOI] [PubMed] [Google Scholar]
- 32.Tanabe M, Myers A, Bhandari P, et al. Family planning in refugee settings: findings and actions from a multi-country study. Confl Health 2017;11:9 10.1186/s13031-017-0112-2 [DOI] [Google Scholar]
- 33.Loganathan T, Rui D, Ng C-W, et al. Breaking down the barriers: understanding migrant workers' access to healthcare in Malaysia. PLoS One 2019;14:e0218669. 10.1371/journal.pone.0218669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rahman MM, Arif MT, Safii R, et al. Care seeking behaviour of Bangladeshi migrant workers in Sarawak, Malaysia. Bangladesh Med Res Counc Bull 2019;45:47–53. 10.3329/bmrcb.v45i1.41808 [DOI] [Google Scholar]
- 35.Chuah FLH, Tan ST, Yeo J, et al. Health system responses to the health needs of refugees and asylum-seekers in Malaysia: a qualitative study. Int J Environ Res Public Health 2019;16:1584 10.3390/ijerph16091584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siah PC, Low SK, Lee WY, et al. Discrimination perceived by child refugees in Malaysia: from the views of representatives from refugees’ community service centres and non-government service. Vulnerable Child Youth Stud 2019;18:1–4. 10.1080/17450128.2019.1662149 [DOI] [Google Scholar]
- 37.Santos A, Ramos HM, Ramasamy G. Musculoskeletal pain among migrant workers in the Malaysian manufacturing industry: the impact of the physical environment, workload and work patterns. Pertanika Journal of Social Sciences & Humanities 2015;23:315–24. [Google Scholar]
- 38.Kassim MS, George R, Kassim K, et al. Child abuse and neglect as seen in General Hospital, Kuala Lumpur--a two year study. Med J Malaysia 1989;44:111–21. [PubMed] [Google Scholar]
- 39.Jeyakumar D. Thiamine responsive ankle oedema in detention centre inmates. Med J Malaysia 1995;50:17–20. [PubMed] [Google Scholar]
- 40.Zabedah MY, Razak M, Zakiah I, et al. Profile of solvent abusers (glue sniffers) in East Malaysia. Malays J Pathol 2001;23:105–9. [PubMed] [Google Scholar]
- 41.Osman MT, Al-Naggar RA, Taha BI. Knowledge and awareness of cervical cancer screening among Iraqi immigrant women living in Malaysia. World J Med Sci 2013;8:123–9. [Google Scholar]
- 42.Minhat HS, Mustafa J, Sarabi S. Sociodemographic determinants of knowledge on HPV vaccination among Iranian women living in Malaysia. Academic Journal of Cancer Research 2013;6:8–12. [Google Scholar]
- 43.Razali S, Salleh RM, Yahya B, et al. Maternal filicide among women admitted to forensic psychiatric institutions in Malaysia: case series. East Asian Arch Psychiatry 2015;25:79. [PubMed] [Google Scholar]
- 44.Abdul Rahman S, Jeffree MS, Kamaludin F, et al. Beriberi outbreak among unauthorised immigrants in a detention cAMP in Malaysia. J Immigr Minor Health 2018;20:1294–7. 10.1007/s10903-017-0674-5 [DOI] [PubMed] [Google Scholar]
- 45.Nwabichie CC, Manaf RA, Ismail SB. Factors affecting uptake of cervical cancer screening among African women in Klang Valley, Malaysia. Asian Pac J Cancer Prev 2018;19:825. 10.22034/APJCP.2018.19.3.825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kamaludin NA, How V. The inequality of environmental health awareness among foreign immigrants and local blue-collar workers in Kuala Lumpur, Malaysia. Environ Justice 2016;9:181–7. 10.1089/env.2016.0020 [DOI] [Google Scholar]
- 47.Woh PY, Thong KL, Lim YAL, et al. Microorganisms as an indicator of hygiene status among migrant food handlers in Peninsular Malaysia. Asia Pac J Public Health 2017;29:599–607. 10.1177/1010539517735856 [DOI] [PubMed] [Google Scholar]
- 48.Rajeswari B, Sinniah B, Hussein H. Socio-Economic factors associated with intestinal parasites among children living in Gombak, Malaysia. Asia Pac J Public Health 1994;7:21–5. 10.1177/101053959400700104 [DOI] [PubMed] [Google Scholar]
- 49.Krahl W, Hashim A. Psychiatric disorders in ASEAN-migrants in Malaysia--a university hospital experience. Med J Malaysia 1998;53:232–8. [PubMed] [Google Scholar]
- 50.Chandran PA, Jayaram G, Mahmud R, et al. Microfilaria in hydrocele fluid cytology. Malays J Pathol 2004;26:119–23. [PubMed] [Google Scholar]
- 51.Nissapatorn V, Lim YAL, Jamaiah I, et al. Parasitic infections in Malaysia: changing and challenges. Southeast Asian J Trop Med Public Health 2005;36 Suppl 4:50–9. [PubMed] [Google Scholar]
- 52.Leong CC. Pre-Employment medical examination of Indonesian domestic helpers in a private clinic in Johor Bahru – an eight year review. Medical Journal of Malaysia 2006;61:592. [PubMed] [Google Scholar]
- 53.Sasidharan S, Uyub AM, Azlan AA. Further evidence of ethnic and gender differences for Helicobacter pylori infection among endoscoped patients. Trans R Soc Trop Med Hyg 2008;102:1226–32. 10.1016/j.trstmh.2008.05.006 [DOI] [PubMed] [Google Scholar]
- 54.Masitah M. Malaria among foreign workers in Selangor, Malaysia. Journal of Health and Translational Medicine 2008;11:53–8. [Google Scholar]
- 55.Shailendra S, Prepageran N. Oropharyngeal rhinosporidiosis in a migrant worker: a delayed presentation. Medical Journal of Malaysia 2008;63:65. [PubMed] [Google Scholar]
- 56.Chan BTE, Amal RN, Hayati MIN, Noor Hayati MI, et al. Seroprevalence of toxoplasmosis among migrant workers from different Asian countries working in Malaysia. Southeast Asian J Trop Med Public Health 2008;39:9. [PubMed] [Google Scholar]
- 57.Farhana F, Jamaiah I, Rohela M, et al. A ten year (1999-2008) retrospective study of amoebiasis in University Malaya medical centre (UMMC), Kuala Lumpur, Malaysia. Tropical Biomedicine 2009;Dec 1;26:262–6. [PubMed] [Google Scholar]
- 58.Chan BT, Amal RN, Noor Hayati MI. Comparative study of seroprevalence of toxoplasmosis between local workers and migrant workers in Malaysia. Archives of Medical Science 2009;5:255. [Google Scholar]
- 59.Murty OP. Cystic tumor of papillary muscle of heart: a rare finding in sudden death. Am J Forensic Med Pathol 2009;30:201–3. 10.1097/PAF.0b013e31819d9af5 [DOI] [PubMed] [Google Scholar]
- 60.Murty OP, Kian CK, Husin MH. Fatal lightning strikes in Malaysia: a review of 27 fatalities. The American Journal of Forensic Medicine and Pathology 2009;30:246–51. [DOI] [PubMed] [Google Scholar]
- 61.Mustafa B, Hani AWA, Chem YK, Mariam M, et al. Epidemiological and clinical features of dengue versus other acute febrile illnesses amongst patients seen at government polyclinics. Med J Malaysia 2010;65:291–6. [PubMed] [Google Scholar]
- 62.Su TA, Hoe VCW, Masilamani R, et al. Hand-arm vibration syndrome among a group of construction workers in Malaysia. Occup Environ Med 2011;68:58–63. 10.1136/oem.2009.052373 [DOI] [PubMed] [Google Scholar]
- 63.Ratnasinga J, Ioras F, Mohd Karee I. Migrant contract workers and occupational accidents in the furniture industry. J Appl Sci 2011;11:2646–51. 10.3923/jas.2011.2646.2651 [DOI] [Google Scholar]
- 64.Ab Rahman AK, Abdullah FH, leishmaniasis V. Visceral leishmaniasis (kala-azar) and malaria coinfection in an immigrant in the state of Terengganu, Malaysia: a case report. J Microbiol Immunol Infect 2011;44:72–6. 10.1016/j.jmii.2011.01.014 [DOI] [PubMed] [Google Scholar]
- 65.Taib T, Baba R. Clinical characteristics of patients with leprosy in hospital Kuala Lumpur. Malaysian Journal of Dermatology 2013;31:30–6. [Google Scholar]
- 66.Santos A, Ramos HM, Ramasamy G, et al. Prevalence of musculoskeletal pain in a sample of migrant workers in the manufacturing industry in Malaysia. Public Health 2014;128:759–61. 10.1016/j.puhe.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 67.Kugan V, Mahadevan DT, Kandasami P, Vijian K, Tata MD, Palayan K. Comparison of features and outcomes of perforated peptic ulcer between Malaysians and foreigners. Med J Malaysia 2016;71:13. [PubMed] [Google Scholar]
- 68.Azian MN, Hakim SL, Khadri MS. Leishmaniasis in Peninsular Malaysia: the role of immigrant workers and the vector. Southeast Asian Journal of Tropical Medicine and Public Health 2016;47:607–16. [Google Scholar]
- 69.Sahimin N, Lim YAL, Ariffin F, et al. Migrant workers in Malaysia: current implications of sociodemographic and environmental characteristics in the transmission of intestinal parasitic infections. PLoS Negl Trop Dis 2016;10:e0005110 10.1371/journal.pntd.0005110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Min NN, Vasudevan SK, Jasman AA, et al. Work-Related ocular injuries in Johor Bahru, Malaysia. International Eye Science 2016;16:416–22. [Google Scholar]
- 71.Woh PY, Thong KL, Behnke JM, et al. Characterization of nontyphoidal Salmonella isolates from asymptomatic migrant food handlers in Peninsular Malaysia. J Food Prot 2017;80:1378–83. 10.4315/0362-028X.JFP-16-342 [DOI] [PubMed] [Google Scholar]
- 72.Ratnalingam V, Umapathy T, Sumugam K. Microbial keratitis in West and East Malaysia. Internal Eye Science 2017;17:1989–92. [Google Scholar]
- 73.Noor NM, Shaker MN. Perceived workplace discrimination, coping and psychological distress among unskilled Indonesian migrant workers in Malaysia. International Journal of Intercultural Relations 2017;57:19–29. 10.1016/j.ijintrel.2017.01.004 [DOI] [Google Scholar]
- 74.Noordin R, Mohd Zain SN, Yunus MH, et al. Seroprevalence of lymphatic filariasis among migrant workers in Peninsular Malaysia. Trans R Soc Trop Med Hyg 2017;111:370–2. 10.1093/trstmh/trx062 [DOI] [PubMed] [Google Scholar]
- 75.Sahimin N, Lim YAL, Ariffin F, et al. Socio-Demographic determinants of Toxoplasma gondii seroprevalence in migrant workers of Peninsular Malaysia. Parasit Vectors 2017;10:238 10.1186/s13071-017-2167-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Labao HC, Faller EM, Bacayo MFD. ‘Aches and pains’ of Filipino migrant workers in Malaysia: A profile of work-related musculoskeletal disorders. Annals of Global Health 2018;84:474–80. 10.29024/aogh.2331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sahimin N, Douadi B, Yvonne Lim AL, Lim AL, et al. Distribution of Giardia duodenalis (assemblages A and B) and Cryptosporidium parvum amongst migrant workers in Peninsular Malaysia. Acta Trop 2018;182:178–84. 10.1016/j.actatropica.2018.02.033 [DOI] [PubMed] [Google Scholar]
- 78.Jeffree SM, Mihat O, Hassan R, Ahmed K, Safian N, et al. Falciparum malaria outbreak in Sabah linked to an immigrant rubber tapper. Am J Trop Med Hyg 2018;98:45–50. 10.4269/ajtmh.17-0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zerguine H, Tamrin SBM, Jalaludin J. Prevalence, source and severity of work-related injuries among “foreign” construction workers in a large Malaysian organisation: a cross-sectional study. Ind Health 2018;56:264–73. 10.2486/indhealth.2017-0205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ya’acob NA, Abidin EZ, Rasdi I, et al. Reducing work-related musculoskeletal symptoms through implementation of Kiken Yochi training intervention approach. Work 2018;60:143–52. 10.3233/WOR-182711 [DOI] [PubMed] [Google Scholar]
- 81.Sahimin N, Lim YA, Noordin R. Epidemiology and Immunodiagnostics of Strongyloides stercoralis infections among migrant workers in Malaysia. Asian Pacific Journal of Tropical Medicine 2019;12:250. [Google Scholar]
- 82.Jamaiah I, Anuar AK, Najib NA. Imported malaria: a retrospective study in university Hospital, Kuala Lumpur, a ten-year experience. Medical Journal of Malaysia 1998;53:6–9. [PubMed] [Google Scholar]
- 83.Sobri M, Merican JS, Nordiyana M. Neuroimaging features of tuberculous meningitis. Medical Journal of Malaysia 2006;61:36–40. [PubMed] [Google Scholar]
- 84.Daher AM, Ibrahim HS, Daher TM, et al. Health related quality of life among Iraqi immigrants settled in Malaysia. BMC Public Health 2011;11:407 10.1186/1471-2458-11-407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kwan Z, Pailoor J, Leng Tan L, Tan LL, et al. Leprosy – an imported disease. Lepr Rev 2014;85:170–6. 10.47276/lr.85.3.170 [DOI] [PubMed] [Google Scholar]
- 86.Elmi OS, Hasan H, Abdullah S, et al. Multidrug-Resistant tuberculosis and risk factors associated with its development: a retrospective study. The Journal of Infection in Developing Countries 2015;9:1076–85. 10.3855/jidc.6162 [DOI] [PubMed] [Google Scholar]
- 87.William T, Parameswaran U, Lee WK, et al. Pulmonary tuberculosis in outpatients in Sabah, Malaysia: advanced disease but low incidence of HIV co-infection. BMC Infect Dis 2015;15:32 10.1186/s12879-015-0758-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Scheutz F, Heidmann J, Poulsen S. Dental health of Vietnamese boat people on Pulau Bidong, Malaysia. Community Dent Oral Epidemiol 1983;11:255–8. 10.1111/j.1600-0528.1983.tb01888.x [DOI] [PubMed] [Google Scholar]
- 89.Levy J. Epidemiological survey of intestinal parasitic infections in children of Sabah, Malaysia. J Public Health 1988;10:240–9. 10.1093/oxfordjournals.pubmed.a042413 [DOI] [PubMed] [Google Scholar]
- 90.Siah P-C, Lee W-Y, Goh L-Y. Quality of life among refugee children in Malaysia – a brief report. Vulnerable Child Youth Stud 2015;6:1–6. 10.1080/17450128.2015.1092624 [DOI] [Google Scholar]
- 91.Shaw SA, Ward KP, Pillai V. A group mental health randomized controlled trial for female refugees in Malaysia. American Journal of Orthopsychiatry 2018. [DOI] [PubMed] [Google Scholar]
- 92.Dony JF, Ahmad J, Khen Tiong Y, Tiong YK. Epidemiology of tuberculosis and leprosy, Sabah, Malaysia. Tuberculosis 2004;84:8–18. 10.1016/j.tube.2003.08.002 [DOI] [PubMed] [Google Scholar]
- 93.Vearey J, Orcutt M, Gostin L, et al. Building alliances for the global governance of migration and health. BMJ 2019;366:l4143 10.1136/bmj.l4143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.World Health Organization Regional Office for Europe Strategy and action plan for refugee and migrant health in the who European region. Copenhagen: World Health Organization Regional Office for Europe, 2016. [Google Scholar]
- 95.Reidpath DD, Allotey P. Infant mortality rate as an indicator of population health. Journal of Epidemiology Community Health 2003;57:344–6. 10.1136/jech.57.5.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vijayasingham L, Rhule E, Asgari-Jirhandeh N, et al. Restrictive migration policies in low-income and middle-income countries. The Lancet Global Health 2019;7:e843–4. 10.1016/S2214-109X(19)30196-2 [DOI] [PubMed] [Google Scholar]
- 97.Juárez SP, Honkaniemi H, Dunlavy AC, et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. The Lancet Global Health 2019;7:e420–35. 10.1016/S2214-109X(18)30560-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shao C, Meng X, Cui S, et al. Income-Related health inequality of migrant workers in China and its decomposition: an analysis based on the 2012 China Labor-force dynamics survey data. J Chin Med Assoc 2016;79:531–7. 10.1016/j.jcma.2016.02.009 [DOI] [PubMed] [Google Scholar]
- 99.He X, Wong DFK. A comparison of female migrant workers’ mental health in four cities in China. Int J Soc Psychiatry 2013;59:114–22. 10.1177/0020764011423467 [DOI] [PubMed] [Google Scholar]
- 100.Al-Khatib I, Ju'ba A, Kamal N, et al. Impact of housing conditions on the health of the people at al-Ama'ri refugee cAMP in the West bank of Palestine. Int J Environ Health Res 2003;13:315–26. 10.1080/09603120310001616092 [DOI] [PubMed] [Google Scholar]
- 101.Mutalip MH, Mishkin K, Paiwai F, et al. Factors associated with sexual intercourse, condom-use, and perceived peer behaviors among adolescents in Malaysia: a school-based cross-sectional study. Malaysian Journal of Social Sciences & Humanities 2019;4:8–18. [Google Scholar]
- 102.Khan MA, Rosly NA, Majeed AB. Knowledge of modes of HIV transmission among public secondary school students in urban and rural areas in Malaysia. Pakistan Journal of Pharmaceutical Sciences 2018;31:1985–90. [PubMed] [Google Scholar]
- 103.Mohamad Shakir SM, Wong LP, Lim Abdullah K, Shakir M, Mahavera S, et al. Online STI information seeking behaviour and condom use intentions among young Facebook users in Malaysia. Health Promot Int 2020;35:1116–24. 10.1093/heapro/daz108 [DOI] [PubMed] [Google Scholar]
- 104.Renzaho AMN, Burns C. Post-migration food habits of sub-Saharan African migrants in Victoria: a cross-sectional study. Nutrition & Dietetics 2006;63:91–102. 10.1111/j.1747-0080.2006.00055.x [DOI] [Google Scholar]
- 105.Ganle JK, Amoako D, Baatiema L, et al. Risky sexual behaviour and contraceptive use in contexts of displacement: insights from a cross-sectional survey of female adolescent refugees in Ghana. Int J Equity Health 2019;18:127. 10.1186/s12939-019-1031-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bosdriesz JR, Lichthart N, Witvliet MI, et al. Smoking prevalence among migrants in the US compared to the US-Born and the population in countries of origin. PLoS One 2013;8:e58654 10.1371/journal.pone.0058654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ritchie H, Roser M. Smoking. Oxford: Our World Data, 2019. https://ourworldindata.org/smoking [Google Scholar]
- 108.Sweileh WM. Global output of research on the health of international migrant workers from 2000 to 2017. Global Health 2018;14:105 10.1186/s12992-018-0419-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.World Health Organisation Noncommunicable diseases (NCD) country profiles. Malaysia: World Health Organisation, 2018. [Google Scholar]
- 110.Zimmerman C, Hossain M, Watts C. Human trafficking and health: a conceptual model to inform policy, intervention and research. Soc Sci Med 2011;73:327–35. 10.1016/j.socscimed.2011.05.028 [DOI] [PubMed] [Google Scholar]
- 111.Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med 2011;8:e1001034 10.1371/journal.pmed.1001034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Par M, Hassan SA, Uba I, et al. Perceived stress among international postgraduate students in Malaysia. Int J Psychol Stud 2015;7:1 10.5539/ijps.v7n4p1 [DOI] [Google Scholar]
- 113.Kohno A, Nik Farid ND, Musa G, et al. Factors affecting Japanese retirees’ healthcare service utilisation in Malaysia: a qualitative study. BMJ Open 2016;6:e010668 10.1136/bmjopen-2015-010668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Asits S, Noorhidayah I, Osman A. Migrasi bermusim: Pengaruhnya terhadap kawalan malaria di Sabah. Medical Journal of Malaysia 1999;54:200–9. [PubMed] [Google Scholar]
- 115.World Health Organization A conceptual framework for action on the social determinants of health. Geneva: World Health Organization, 2010. [Google Scholar]
- 116.International Organization for Migration Glossary on migration. 2nd ed. Geneva: International Organization for Migration, 2011. [Google Scholar]
- 117.Centre for Cognitive Ageing and Cognitive Epidemiology Systematic reviews and meta-analyses: a step-by-step guide. Edinburgh: Centre for Cognitive Ageing and Cognitive Epidemiology, 2013. https://www.ccace.ed.ac.uk/research/software-resources/systematic-reviews-and-meta-analyses [Google Scholar]
- 118.Alexander LK, Lopes B, Ricchetti-Masterson K. ERIC notebook. 2nd ed. Chapel Hill: Epidemiologic Research and Information Center, 2015. [Google Scholar]
- 119.Cochrane Childhood Cancer Non-Randomised controlled study (NRS) designs. London: Cochrane Childhood Cancer, 2021. https://childhoodcancer.cochrane.org/non-randomised-controlled-study-nrs-designs [Google Scholar]
- 120.Peacock JL, Peacock PJ. Oxford Handbook of medical statistics. Oxford: Oxford University Press, 2011. [Google Scholar]
- 121.Moola S, Munn Z, Tufanaru C. Chapter 7: systematic reviews of etiology and risk : Aromataris E, Munn Z, JBI manual for evidence synthesis. Adelaide, Australia: JBI, 2017. 10.46658/JBIMES-20-08 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-041379supp001.pdf (1.4MB, pdf)
bmjopen-2020-041379supp002.pdf (123.4KB, pdf)
bmjopen-2020-041379supp003.pdf (84.6KB, pdf)