Abstract
Purpose
We aimed to compare the prevalence rates and associated symptoms of constipation and fecal incontinence in children and young adults and evaluate how these patient groups cope with these disorders.
Methods
A cross-sectional study was performed in which 212 children (8–17 years) and 149 young adults (18–29 years) from the general Dutch population completed a questionnaire about defecation disorders.
Results
Constipation occurred in 15.6% of children and 22.8% of young adults (p=0.55), while the prevalence of fecal incontinence was comparable between groups (7%, p=0.91). The symptoms associated with constipation occurred as often in children as in young adults, while most fecal incontinence symptoms occurred more often in young adults. Approximately 43% of children had constipation for more than 5 years, while 26% of young adults experienced constipation since childhood. Only 27% of constipated children and 21% of constipated young adults received treatment (mostly laxatives). For fecal incontinence, 13% of children and 36% of young adults received treatment (mostly antidiarrheal medications or incontinence pads).
Conclusion
In contrast to the general belief, the prevalence of defecation disorders and associated symptoms seem to be comparable in children and young adults. Only a few people with defecation disorders receive adequate treatment.
Keywords: Constipation, Fecal incontinence, Prevalence, Therapeutics
INTRODUCTION
Constipation and fecal incontinence are common pediatric disorders [1,2]. It is often assumed that children outgrow these defecation problems [3,4]. However, a number of studies have shown that a significant proportion of children with constipation (20–52%) still have symptoms after several years of treatment [5,6,7]. Furthermore, van Ginkel and colleagues [8] reported that constipation still occurred in 30% of patients after puberty. Moreover, even after seemingly successful treatment, 17% of the girls and 41% of the boys had a relapse of symptoms. According to Bongers and colleagues [7], the prognostic factors for poor long-term outcomes in children who experienced constipation were a long delay between the onset of symptoms and first visit to the doctor and lower defecation frequency. Even though symptoms persist in many patients despite years of treatment, the symptoms are expected to improve after the transition from childhood to adulthood. Unfortunately, it is difficult to study the development of defecation disorders across this transition period, because the criteria for diagnosing constipation and fecal incontinence in children and adults differ. As a consequence, most longitudinal studies only use certain associated symptoms to study the development of defecation disorders instead of using the complete set of diagnostic criteria. To study the actual difference in the prevalence of defecation disorders between children and young adults, and to follow patients' treatment progress during their transition from childhood to adulthood, the same diagnostic criteria must be used for both children and young adults. It is important to gain more insight into the developmental course of symptoms of constipation and fecal incontinence from childhood to adulthood. If the children have not outgrown these defecation disorders, then one should intervene as soon as possible, especially because chronic constipation and fecal incontinence are associated with reduced quality of life, psychological maladjustment, and high healthcare costs [9,10,11,12,13,14,15].
This study aimed to compare the prevalence of constipation and fecal incontinence between children and young adults. We also aimed to analyze the occurrence of symptoms associated with constipation and fecal incontinence in children and young adults. Finally, we aimed to compare how children and young adults with defecation disorders cope with their symptoms.
MATERIALS AND METHODS
Respondents
A cross-sectional study was performed in the Dutch population and was conducted in compliance with the requirements of the local Medical Ethical Committee of the University Medical Center Groningen. As we described previously, respondents were randomly selected from a database of Dutch inhabitants by the external company Survey Sampling International, in Rotterdam, the Netherlands, between September and December 2015 [16]. Participants in this database were provided with a link that allowed them to participate in the study and to complete the questionnaire online. They were able to join the study until the predetermined number of participants per demographic group was reached (based on age and sex according to the Dutch demographics). In accordance with the Dutch law, participants aged between 8 and 17 years were invited through their parents to participate in the study, and the parents were asked to assist their children in completing the survey. Respondents who completed the questionnaire received a set fee (0.30 euro per questionnaire) from the company.
The response rates were 23% for children and 54% for adults. In total, 240 children aged between 8 and 17 years and 187 young adults aged between 18 and 29 years were included in the study. In accordance with the Rome IV criteria for functional disorders, 28 children and 50 young adults with a history of anorectal or pelvic surgery, with a diagnosed comorbidity, or who used medications as treatment for their comorbidities that could influence their bowel habits were excluded. Respondents who underwent the following types of anorectal or pelvic surgery were also excluded: intestinal resection surgery (n=7), surgery for Hirschsprung's disease (n=3), surgery for sacrococcygeal teratoma (n=2), perianal fistula surgery (n=2), anal sphincter surgery (n=4), hemorrhoidectomy (n=4), and prostate surgery (n=1). Moreover, respondents with the following comorbidities were excluded: inflammatory bowel disease (n=3), irritable bowel disorder (n=27), slow transit constipation (n=1), rectal prolapse (n=2), congenital anorectal malformation (n=1), Hirschsprung's disease (n=3), sacrococcygeal teratoma (n=2), neurological disorder such as spinal cord injury or multiple sclerosis (n=3), spina bifida (n=2), and diabetes mellitus (n=7). Finally, 212 children and 149 young adults were included in the analyses.
Data analysis and criteria for defecation disorders
In this study, young adults completed the Groningen Defecation and Fecal Continence questionnaire, while children filled in the pediatric version of the questionnaire (Supplementary Files 1, 2), possibly with the help of their parent(s). The feasibility, reproducibility, and validity of this questionnaire have been tested in the adult Dutch population [17]. The questionnaires contained questions on bowel habits, symptoms of defecation disorders, and how these disorders are dealt with. In addition, multiple validated scoring systems for diagnosing constipation and fecal incontinence were used in the questionnaires. In order to provide a comparison between children and young adults, we used the same diagnostic criteria for defecation disorders. Therefore, we used the adult Rome IV criteria for diagnosing constipation and fecal incontinence in both children and young adults. In contrast to the adult Rome IV criteria, it was unethical and not feasible to use the pediatric Rome IV criteria for both disorders as they require physical examination or additional investigation [18]. In our opinion, it would have been unethical to carry out physical examinations or additional investigations because our study involved the general population instead of patients who had voluntarily consulted a doctor. Hence, we used the following criteria for diagnosing constipation: straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal blockage, manual maneuvers to facilitate defecation, and fewer than three spontaneous bowel movements a week. Questions related to straining, obstruction, and incomplete evacuation were simplified as they were too difficult for children to answer if these symptoms occurred in at least 25% of the defecation attempts. If respondents had at least two of the aforementioned symptoms and rarely had loose stools without using laxatives, they met the Rome IV criteria for constipation [19]. In addition, participants should not meet the suggested criteria for irritable bowel syndrome in order to fulfill the diagnostic criteria for constipation. The possible diagnosis of irritable bowel syndrome was excluded when questions related to abdominal pain were asked, since the participants did not undergo additional investigations for this study. Fecal incontinence was defined as recurrent, uncontrolled passage of fecal material for the last 3 months, in an individual with a developmental age of at least 4 years [20]. Of note, since the adult Rome criteria were used to diagnose defecation disorders in children, we were unable to differentiate fecal incontinence due to constipation (overflow fecal incontinence) from fecal incontinence without constipation. In the analyses on associated symptoms and coping with defecation disorders, only the symptoms that occurred or treatments that were used at least several times a month were taken into account.
Statistical analysis
IBM SPSS Statistics for Windows, Version 23.0 (IBM Co., Armonk, NY, USA) was used for the statistical analysis. Normally distributed continuous data were expressed as means and standard deviations and analyzed using an independent sample Student's t-test. Categorical data were expressed as numbers and percentages and analyzed using a chi-square or Fisher's exact test. The p-values of less than 0.05 were considered significant.
RESULTS
Respondents' characteristics
The characteristics of 212 children and 149 young adults are described in Table 1. No significant differences were observed between the respondents in terms of sex, body mass index, and living environment.
Table 1. Respondents' characteristics.
| Characteristics | Children (n=212) | Young adults (n=149) | p-value | |
|---|---|---|---|---|
| Age | 13.1 (2.81) | 24.1 (3.28) | <0.001 | |
| Sex | 0.14 | |||
| Male | 119 (56.1) | 72 (48.3) | ||
| Female | 93 (43.9) | 77 (51.7) | ||
| BMI category* | 0.57 | |||
| Underweight | 17 (8.0) | 9 (6.0) | ||
| Normal weight | 145 (68.4) | 102 (68.5) | ||
| Overweight | 23 (10.8) | 23 (15.4) | ||
| Obesity | 24 (11.3) | 15 (10.1) | ||
| Living environment | 0.32 | |||
| Rural | 85 (40.1) | 52 (34.9) | ||
| Urban | 127 (59.9) | 97 (65.1) | ||
Values are presented as mean (standard deviation) or number (%).
BMI: body mass index.
*Variable contains missing data.
Prevalence of defecation disorders
In our pediatric study population, 33 children (15.6%) had constipation, of whom a quarter also had co-existing fecal incontinence; meanwhile, 34 young adults (22.8%) had constipation, of whom 15% also had co-existing fecal incontinence. No significant difference was observed in the prevalence rate between children and young adults (p=0.55). Fecal incontinence occurred as often in children as in young adults (15 [7.1%] and 11 [7.4%], respectively, p=0.91).
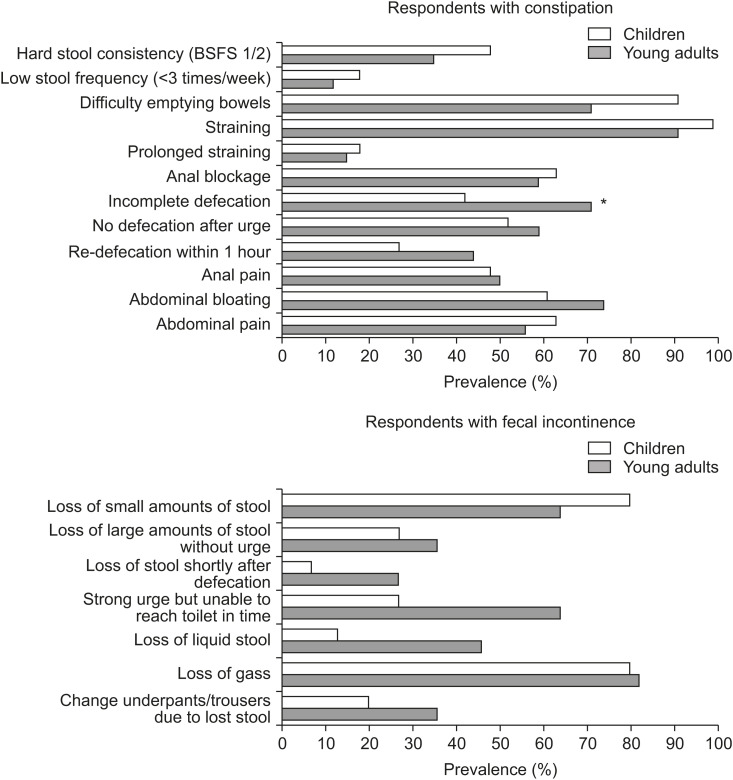
Symptoms associated with defecation disorders
Furthermore, we compared the symptoms associated with constipation in 33 children and 34 young adults (Fig. 1). The “feeling of incomplete defecation” was significantly more often reported in young adults than in children (71% vs. 42%, p=0.027). The prevalence of other associated symptoms of constipation was comparable between children and young adults. Approximately 43% of the children with constipation had symptoms for more than 5 years, 30% for 1–5 years, and 27% for less than 1 year. Furthermore, 26% of young adults experienced constipation symptoms since childhood, while 41% experienced these symptoms for less than 1 year.
Fig. 1. Symptoms associated with defecation disorders. *p<0.05 when comparing children with young adults. BSFC: Bristol Stool Form Scale.
With regard to the prevalence of symptoms associated with fecal incontinence, 15 children were compared with 11 young adults with fecal incontinence (Fig. 1). Although most symptoms associated with fecal incontinence occurred more often in young adults than in children, this difference was not statistically significant.
Coping with defecation disorders
Finally, we compared how respondents coped with symptoms of constipation and fecal incontinence (Tables 2 and 3). Laxative was the most common treatment in constipated children and young adults (21.2% vs. 11.8%, p=0.24, respectively). Irrespective of age, other adequate treatments, such as enemas, special diets, or rectal irrigation using water, were only used by a few respondents (Table 2). In total, only 27% of the constipated children and 21% of the constipated young adults received certain forms of treatment. Furthermore, 18.2% of the children and 11.8% of the young adults used their fingers or hands to evacuate the stools (p=0.61). This was mostly performed by pressing the abdomen with their hands or pressing the area between the buttocks just in front of the anus. Moreover, 9% of the constipated children and 6% of the constipated young adults performed a manual stool extraction, by gently inserting a finger inside the anus and manually removing the stool.
Table 2. Coping with constipation.
| Coping methods | Children (n=33) | Young adults (n=34) | p-value |
|---|---|---|---|
| Using laxatives | 7 (21.2) | 4 (11.8) | 0.24 |
| Using enemas | 1 (3.0) | 0 (0.0) | 0.49 |
| Using special diets | 0 (0.0) | 3 (8.8) | 0.24 |
| Irrigating the rectum with water | 1 (3.0) | 2 (5.9) | 0.99 |
| Using fingers/hands when evacuating the stool | 6 (18.2) | 4 (11.8) | 0.61 |
Values are presented as number (%).
Table 3. Coping with fecal incontinence.
| Coping methods | Children (n=15) | Young adults (n=11) | p-value |
|---|---|---|---|
| Using antidiarrheal medications | 1 (6.7) | 2 (18.2) | 0.56 |
| Using special diets | 1 (6.7) | 0 (0.0) | 0.99 |
| Irrigating the rectum with water | 1 (6.7) | 0 (0.0) | 0.99 |
| Using incontinence pads | 0 (0.0) | 4 (36.4) | 0.022 |
| Rearrange activities | 2 (13.3) | 4 (36.4) | 0.18 |
Values are presented as number (%).
In case of fecal incontinence, young adults used antidiarrheal medications more often than children (18.2% vs. 6.7%, p=0.56). Special diets or rectal irrigation using water was rarely adopted by respondents with fecal incontinence, as shown in Table 3. Significantly more young adults used incontinence pads than children (36.4% vs. 0.0%, p=0.022). Only 13% of the children and 36% of young adults received certain forms of (symptomatic) treatment. In addition, fecal incontinence seemed to have a larger influence on the daily activities of young adults; approximately 36.4% of young adults had to rearrange their activities more than once a month compared with 13.3% of the children (p=0.18).
DISCUSSION
It is often assumed that children outgrow constipation and fecal incontinence [3,4]. In this study, we demonstrated that, unfortunately, the magnitude of these defecation problems seemed to be comparable between young adults and children. The prevalence rates did not decrease, nor did the symptoms associated with constipation and fecal incontinence occur less frequently in young adults than in children. The prevalence rates of constipation were 23% in young adults and 16% in children, and this difference was not significantly different. Fecal incontinence occurred in 7% of the children and young adults who participated in this survey. The prevalence of constipation and especially fecal incontinence in our study population is relatively high compared with those in other studies [1,2,21,22,23], possibly due to the inclusion of the general population instead of a subpopulation of children with severe symptoms that require the assistance of a general practitioner or a medical specialist. In our study, the children and young adults with fecal incontinence had both fecal incontinence without constipation and overflow fecal incontinence, which can be a symptom of (more severe) constipation [24,25]. Both types were included as they can only be differentiated using the pediatric Rome criteria based on the findings of patients' physical or additional examinations. Besides the prevalence rates, the occurrence rate of symptoms associated with constipation and fecal incontinence did not decline in young adults compared with that in children. Many symptoms associated with constipation or fecal incontinence appear to occur more often in young adults or at least did not occur significantly less often. Additionally, fecal incontinence seemed to be more severe in young adults as 36% needed to change their underpants/and or trousers due to accidental stool loss, in comparison to 20% of the children. This finding could also be explained by the fact that children may not have had the opportunity to change their clothes while at school even if they wanted to. Moreover, 43% of the children had constipation for more than five years, while 26% of young adults had this disorder since childhood. This finding indicates that not all children who experience constipation improve after a number of years or after the transition from childhood to adulthood, as supported by various studies [5,6,7,8]. Because our study was based on the general population instead of a selected population of patients who already consulted the gastroenterologist or other doctors and received treatment, it was further clarified that the defecation disorder in a relatively large proportion of children did not improve spontaneously even after reaching adulthood.
In our study population, only a few respondents who had a defecation disorder were treated for their symptoms. Both children and young adults who experienced constipation mostly used laxatives to soften their stools. A relatively large proportion of the children and young adults needed to use their fingers or hands to evacuate the stool, probably because they did not receive adequate treatment or the treatment was insufficient. In case of fecal incontinence, more young adults received symptomatic treatment, such as antidiarrheal medications or incontinence pads, than children. This is not only due to the higher prevalence rates and number of symptoms, but also due to the more independent position of young adults. Children depend largely on their parents when it comes to purchasing over-the- counter medications or using other devices. As previously shown, very few children with defecation disorders seek medical help [16,26]. This implies that many children do not receive any forms of treatment or practice “self-treatment” instead of seeking professional help. This study demonstrated that the symptoms do not seem to disappear spontaneously later in life; therefore, parents and doctors should pay more attention to managing these defecation problems and breaking the taboo surrounding this topic. Hence, it is important to raise the public's awareness regarding this problem, because constipation and fecal incontinence can decrease the quality of life and lead to psychological maladjustment [9,10,11].
Some limitations of this study need to be addressed. There is a high risk of selection bias due to the relatively low response rates, especially in the pediatric group. We may have included more people with defecation-related complaints, since they are more likely to respond to questions related to their problems [27]. Furthermore, our sample of respondents with defecation disorders was small, which had a large influence on the p-value of several analyses. Repeating this study in another country, using the translated version of the Groningen Defecation and Fecal Continence, would contribute to increasing the sample size and strengthening the results. Finally, it is not possible to compare the prevalence rates of defecation disorders in children in our study with those in other studies, as the adult Rome IV criteria for diagnosing constipation and fecal incontinence were used in this study.
In conclusion, in contrast to the general belief that children outgrow defecation disorders, the prevalence and occurrence rates of associated symptoms seem to be comparable between children and young adults. Since many children do not outgrow their disorders, constipation and fecal incontinence should be treated as early as possible. Currently, only a small proportion of children and young adults with defecation disorders receive adequate (symptomatic) treatment.
ACKNOWLEDGEMENTS
The authors would like to thank T. van Wulfften Palthe, PhD for editing the English manuscript.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest: The authors have no financial conflicts of interest.
SUPPLEMENTARY MATERIALS
The Groningen Pediatric Defecation & Fecal Continence Questionnaire
The Groningen Defecation & Fecal Continence Questionnaire
References
- 1.Rajindrajith S, Devanarayana NM, Crispus Perera BJ, Benninga MA. Childhood constipation as an emerging public health problem. World J Gastroenterol. 2016;22:6864–6875. doi: 10.3748/wjg.v22.i30.6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rouster AS, Karpinski AC, Silver D, Monagas J, Hyman PE. Functional gastrointestinal disorders dominate pediatric gastroenterology outpatient practice. J Pediatr Gastroenterol Nutr. 2016;62:847–851. doi: 10.1097/MPG.0000000000001023. [DOI] [PubMed] [Google Scholar]
- 3.Bellman M. Studies on encopresis. Acta Paediatr Scand. 1966;(Suppl 170):1+. [PubMed] [Google Scholar]
- 4.Abrahamian FP, Lloyd-Still JD. Chronic constipation in childhood: a longitudinal study of 186 patients. J Pediatr Gastroenterol Nutr. 1984;3:460–467. doi: 10.1097/00005176-198406000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Procter E, Loader P. A 6-year follow-up study of chronic constipation and soiling in a specialist paediatric service. Child Care Health Dev. 2003;29:103–109. doi: 10.1046/j.1365-2214.2003.00319.x. [DOI] [PubMed] [Google Scholar]
- 6.Michaud L, Lamblin MD, Mairesse S, Turck D, Gottrand F. Outcome of functional constipation in childhood: a 10-year follow-up study. Clin Pediatr (Phila) 2009;48:26–31. doi: 10.1177/0009922808320599. [DOI] [PubMed] [Google Scholar]
- 7.Bongers ME, Benninga MA. Long-term follow-up and course of life in children with constipation. J Pediatr Gastroenterol Nutr. 2011;53(Suppl 2):S55–6. [PubMed] [Google Scholar]
- 8.van Ginkel R, Reitsma JB, Büller HA, van Wijk MP, Taminiau JA, Benninga MA. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003;125:357–363. doi: 10.1016/s0016-5085(03)00888-6. [DOI] [PubMed] [Google Scholar]
- 9.Filho HS, Mastroti RA, Klug WA. Quality-of-life assessment in children with fecal incontinence. Dis Colon Rectum. 2015;58:463–468. doi: 10.1097/DCR.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 10.Kovacic K, Sood MR, Mugie S, Di Lorenzo C, Nurko S, Heinz N, et al. A multicenter study on childhood constipation and fecal incontinence: effects on quality of life. J Pediatr. 2015;166:1482–1487.e1. doi: 10.1016/j.jpeds.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 11.Ranasinghe N, Devanarayana NM, Benninga MA, van Dijk M, Rajindrajith S. Psychological maladjustment and quality of life in adolescents with constipation. Arch Dis Child. 2017;102:268–273. doi: 10.1136/archdischild-2016-310694. [DOI] [PubMed] [Google Scholar]
- 12.McKenna C, Bartlett L, Ho YH. Fecal incontinence reduces quality of life more than you may think. Dis Colon Rectum. 2017;60:e597–8. doi: 10.1097/DCR.0000000000000832. [DOI] [PubMed] [Google Scholar]
- 13.Vriesman MH, Rajindrajith S, Koppen IJN, van Etten-Jamaludin FS, van Dijk M, Devanarayana NM, et al. Quality of life in children with functional constipation: a systematic review and meta-analysis. J Pediatr. 2019;214:141–150. doi: 10.1016/j.jpeds.2019.06.059. [DOI] [PubMed] [Google Scholar]
- 14.Park R, Mikami S, LeClair J, Bollom A, Lembo C, Sethi S, et al. Inpatient burden of childhood functional GI disorders in the USA: an analysis of national trends in the USA from 1997 to 2009. Neurogastroenterol Motil. 2015;27:684–692. doi: 10.1111/nmo.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sommers T, Corban C, Sengupta N, Jones M, Cheng V, Bollom A, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572–579. doi: 10.1038/ajg.2015.64. [DOI] [PubMed] [Google Scholar]
- 16.Timmerman MEW, Trzpis M, Broens PMA. The problem of defecation disorders in children is underestimated and easily goes unrecognized: a cross-sectional study. Eur J Pediatr. 2019;178:33–39. doi: 10.1007/s00431-018-3243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meinds RJ, Timmerman MEW, van Meegdenburg MM, Trzpis M, Broens PMA. Reproducibility, feasibility and validity of the Groningen Defecation and Fecal Continence questionnaires. Scand J Gastroenterol. 2018;53:790–796. doi: 10.1080/00365521.2018.1465993. [DOI] [PubMed] [Google Scholar]
- 18.Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional disorders: children and adolescents. Gastroenterology. 2016;150:1456–1468.e2. doi: 10.1053/j.gastro.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 19.Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, et al. Bowel disorders. Gastroenterology. 2016;150:1393–1407.e5. doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 20.Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Functional anorectal disorders. Gastroenterology. 2016;150:1430–42.e4. doi: 10.1053/j.gastro.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koppen IJN, Vriesman MH, Saps M, Rajindrajith S, Shi X, van Etten-Jamaludin FS, et al. Prevalence of functional defecation disorders in children: a systematic review and meta-analysis. J Pediatr. 2018;198:121–30.e6. doi: 10.1016/j.jpeds.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 22.Nelson RL. Epidemiology of fecal incontinence. Gastroenterology. 2004;126(Suppl 1):S3–S7. doi: 10.1053/j.gastro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 23.Chanpong A, Osatakul S. Laxative choice and treatment outcomes in childhood constipation: clinical data in a longitudinal retrospective study. Pediatr Gastroenterol Hepatol Nutr. 2018;21:101–110. doi: 10.5223/pghn.2018.21.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee G, Son JS, Bae SH. Clinical features of severely constipated children: comparison of infrequent bowel movement and fecal soiling groups. Pediatr Gastroenterol Hepatol Nutr. 2020;23:26–34. doi: 10.5223/pghn.2020.23.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nurko S, Scott SM. Coexistence of constipation and incontinence in children and adults. Best Pract Res Clin Gastroenterol. 2011;25:29–41. doi: 10.1016/j.bpg.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajindrajith S, Devanarayana NM, Benninga MA. Children and adolescents with chronic constipation: how many seek healthcare and what determines it? J Trop Pediatr. 2012;58:280–285. doi: 10.1093/tropej/fmr096. [DOI] [PubMed] [Google Scholar]
- 27.Choung RS, Locke GR, Schleck CD, Ziegenfuss JY, Beebe TJ, Zinsmeister AR, et al. A low response rate does not necessarily indicate non-response bias in gastroenterology survey research: a population-based study. J Public Health. 2013;21:87–95. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Groningen Pediatric Defecation & Fecal Continence Questionnaire
The Groningen Defecation & Fecal Continence Questionnaire