Abstract
Background
The objective of this article is to assess the mental health issues of the mild condition coronavirus disease 2019 (COVID-19) patients admitted to a community treatment center (CTC) in Korea.
Methods
A total of 107 patients admitted to a CTC were included as the study population, and their mental health problems including depression (patient health questionnaire-9), anxiety (generalized anxiety disorder scale-7), post-traumatic stress disorder (PTSD) (PTSD checklist-5) and somatic symptoms (by patient health questionnaire-15) were evaluated every week during their stay. The stigma related to COVID-19 infection was evaluated with an adjusted version of the Middle East respiratory syndrome (MERS) stigma scale.
Results
During the first week of isolation, the prevalence of more-than-moderate depression was 24.3%, more-than-moderate anxiety was 14.9%, more-than-moderate somatic symptoms was 36.5% and possible PTSD was 5.6% of total population. For depression and anxiety, previous psychiatric history and stigma of COVID-19 infection were significant risk factors. For PTSD, previous psychiatric history and stigma of COVID-19 infection as well as total duration of isolation were found to be significant risk factors. Prevalence of depression, anxiety and possible PTSD remained similar across the four weeks of observations, though the prevalence of severe depression, increased after four weeks of stay. Somatic symptoms seemed to decrease during their stay.
Conclusion
The results suggest that social mitigation of COVID-19 related stigma, as well as care of patients with pre-existing mental health problems are important mental health measures during this crisis period. It is also important that clinical guidelines and public health policies be well balanced over the protection of the public and those quarantined to minimize the negative psychosocial consequences from isolation of the patients.
Keywords: COVID-19, Isolation, Depression, Anxiety, Stigma
Graphical Abstract
INTRODUCTION
In 2020, the worldwide severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection 2019 (COVID-19) epidemic resulted in large numbers of patients and shortages of medical facilities.1,2 Community treatment centers (CTCs) are innovative responses to the COVID-19 outbreak in Korea.3 The Korean government converted existing accommodation facilities into patient facilities to cope with the lack of hospital beds. COVID-19 patients with no symptoms or mild symptoms did not need intensive medical treatment, but they still needed to be quarantined until they were clear of the virus to prevent the spread of the disease.4 Further, medical monitoring is also needed to detect acute deterioration and to deal with it. The CTC is an intermediate model between hospitals and self-isolation at home.3 COVID-19 patients with minimal symptoms stayed in separate rooms in CTCs, and the medical staff of the CTCs consisted of doctors and nurses that monitored patients periodically, including using various telemedicine methods including smartphones.
The mass outbreak of a viral disease is going to cause public anxiety and subsequently lead to various mental health issues, both for the infected individuals and the general population.5,6 Despite the efforts of public health authorities and hospitals to make the quarantine more acceptable to patients, and it is legally and scientifically justified from both the individual and public health viewpoints to quarantine those patients, the quarantine itself is essentially an involuntary process that involves the restriction of basic human rights, so there is always the possibility that the quarantine becomes a traumatic experience for those involved. Indeed, one psychiatrist consulting the CTC in which the authors of this article were involved reported that patients worried about their family, especially the children that were left out; felt guilty that they might have infected their loved ones; had anxiety about uncertainty of this novel disease; worried about their own jobs and workplaces; felt frustrated about the postponement of important personal or occupational events; and experienced boredom during their isolation. Those negative psychosocial factors can combine and might lead to the deterioration of the patient's mental health. Quarantines were indeed reported to be associated with suicide, anger and other unpleasant psychological consequences in several other literatures and reviews from previous and current infectious disease outbreaks.7,8 These possible negative psychological costs should be mitigated as far as possible if the quarantine is to be successful against the viral outbreak.9 Therefore, the CTC that we have operated screened patients' mental health vigorously and tried to provide the patients with various mental health promoting programmes and activities.
The objective of this article is to assess and understand the mental health issues we observed during the operation of a CTC during the first months of the COVID-19 crisis in Korea and provide insights on the principles of operating quarantine facilities during this crisis period.
METHODS
Study setting–CTCs
By the end of February 2020, the Korean government decided to operate CTCs that isolate and monitor mild COVID-19 patients to cope with the shortage of hospital beds.10 The target population of CTCs were COVID-19 patients who were asymptomatic or had mild symptoms according to the criteria of the Korea Centers for Disease Control and Prevention (KCDC).11 Patients admitted to CTCs were those who were waiting to be admitted to the hospital after a COVID-19 diagnosis and those who were simply waiting for viral clearance in the hospitals. CTCs could provide symptomatic treatment for mild respiratory symptoms such as coughs, fevers, etc. However, if there was evidence of pneumonia in chest X-rays or symptomatic deterioration, patients were to be transferred to the hospital immediately. According to the guidelines of the KCDC, patients were discharged when two consequent RT-PCR tests at least 24 hours apart both failed to detect the virus.11
This study was conducted in one CTC operated by Seoul National University Hospital (SNUH). In March 5, 2020, SNUH, a teaching hospital in Korea, transformed the existing human resource development centre with 100 rooms into a CTC. The SNUH-CTC consisted of a patient center and a remote monitoring center. The patient center was where the patients were staying. They stayed in separate one- or two-bed rooms equipped with a private toilet and shower. Each room also had a small balcony or window for outside viewing. Meals and snacks were served in the room using disposable lunchbox style trays, and patients were provided with basic necessities including toiletries and other personal hygiene items, phone and Internet connections and cable TV channels. Patients were also provided with automatic blood pressure monitors, thermometers and finger-oxygenometers for self-monitoring vital signs. Patients were given instructions to measure their vital signs twice a day with those self-measured devices. They were also given chest X-ray examinations and COVID-19 tests at regular intervals. In the patient center, a minimal number of medical staff (1–2 doctors, 2 nurses and a radiographer) stayed with the patients for viral testing, X-ray screening, unavoidable in-person examinations, and emergency responses. In the remote monitoring center, doctors and nurses monitored patients at least twice a day using the telemedicine method and a smartphone. The detailed operations of SNUH-CTC were reported previously.12
Study design and data collection
As a retrospective observational study, data were obtained through reviewing medical records. All variables were collected from the electronic medical recording system of SNUH. Two of the researchers reviewed the data and cross-checked them. The medical records were composed of the following data: age, sex, date of diagnosis, date of admission, underlying disease (diabetes, hypertension, and respiratory disease), COVID-19 related symptoms (cough, sputum, fever or chill, rhinorrhoea, sore throat, dyspnea, chest pain, headache and myalgia), and the results of a weekly psychiatric evaluation.
At admission, the psychiatric history and initial psychiatric assessment were evaluated. The psychiatric history included the diagnosis of psychiatric disorders and the use of psychotropic medications. The psychiatric assessment includes the PHQ-2 (patient health questionnaire-2) and the GAD-2 (generalized anxiety disorder 2-item).13,14 During their stay at the CTC, patients reported their self-checked vital signs and symptoms to the medical staffs twice a day using the smartphone application. The doctors and nurses checked it and provided medical consultations using a video-call system. Every week after admission, the patients completed and submitted detailed psychiatric assessments that consisted of the Korean versions of the PHQ-9 (patient health questionnaire-9), GAD-7 (Generalized Anxiety Disorder Scale), P4 (suicidality screener), PCL-5 (PTSD checklist for DSM-5), PHQ-15 (patient health questionnaire-15), and COVID-19 stigma (Appendix 1).13,14,15,16,17,18,19,20,21,22 If at-risk mental status was detected from these questionnaires or at the request of the patients themselves or the monitoring staff, a psychiatric consult using a video-call interview was arranged to conduct a psychiatric assessment and supportive psychotherapy. The consulting psychiatrist offered brief psychotherapy sessions for anyone with mental health difficulties during their stay at the CTC, and prescribed antidepressants and anxiolytic medications for clinical mental health disorders.
Study population
Between 5 March and 8 April 2020, 113 COVID-19 patients who were admitted to the SNUH-CTC were included. Three pediatric patients under 18 years old and three patients who were discharged within one week of admission were excluded. A total of 107 patients were included as the study population.
Measurements
To evaluate patients' psychiatric conditions, multiple assessment tools were used. Depression was assessed with the PHQ-9, which is a 9-item scale to assess the symptoms of major depressive disorder.18 Significant depression is defined to be when the total score is ≥ 5. Anxiety was assessed with the GAD-7 scale.19 The GAD-7 consists of seven items and a total score ≥ 5 is considered to be significant anxiety. Suicidal ideas were evaluated with the P4 suicidality screener, which evaluates the suicidal attempt history and plans. Post-traumatic stress disorder (PTSD) was evaluated with the PCL-5.20 It is a 20-item scale that assesses the symptoms of stress, and PTSD is defined to be when the total score is ≥ 31. The PHQ-15 evaluated the severity of 15 somatic symptoms.22 The COVID-19 stigma was evaluated with an adjusted version of the MERS stigma scale. It is an 8-item scale assessing the four domains of stigma with a four-point Likert-type scale (from “strongly disagree” to “strongly agree”): personalized stigma, disclosure concerns, negative self-image, and public attitude concerns.21,23 Concurrent validity was assessed by examining the relationship of stigma index with other validated questionnaires. COVID-19 stigma index has a statistically significant positive correlation with PHQ-9, GAD-7, PHQ-15 and PCL-5 (Appendix 2).
Statistical analysis
The PHQ-9, GAD-7, P4 suicidality screener, PCL-5 and COVID-19 stigma scale were scored according to each questionnaire's scoring manual. The descriptive statistics are described for the sociodemographic variables, the changes in the proportion of patients with psychiatric distress during the isolation period in the CTC and the intensity of the somatic symptoms of the mild COVID-19 patients in the CTC. We analysed the relationships between sociodemographic factors with the COVID-19 stigma with the χ2 test or ANOVA; we assessed the associations between depression, anxiety, PTSD and clinical characteristics using odds ratios (ORs), which were calculated using multiple logistic regression analyses; and the 95% confidence intervals (CIs) were calculated using maximum likelihood methods. All tests were two-tailed, and P < 0.05 was considered statistically significant. All analyses were performed using the Stata software, version 14.1 (Stata Corp., College Station, TX, USA).
Ethics statement
The study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB No. H-2003-163-1112). Informed consent was exempted as this study was a retrospective medical record review study and did not obtain patient personal information.
RESULTS
Demographic characteristics of COVID-19 patients and the relationship with COVID-19 stigma
The basic characteristics in this study population are shown in Table 1. Of the 107 residents, 52.3% were female and 68.2% of them were no more than 30 years old. Approximately 10.3% of the patients had a previous psychiatric history and 4.7% of them had an underlying disease. 39.3% did not have COVID-19 symptoms, and the mean isolation period at the time of the evaluation was 11.58 ± 0.81 days. There were no significant differences between the subjects with high levels and low levels of COVID-19 stigma regarding their sociodemographic characteristics, COVID-19 symptoms, and total duration of isolation.
Table 1. Characteristics of the mild COVID-19 patients admitted to a CTC in Korea, according to the level of perceived COVID-19 stigma.
| Characteristics | Total | Perceived stigma | P valuea | ||
|---|---|---|---|---|---|
| Upper 25% | 25%–100% | ||||
| Sex | 0.302 | ||||
| Male | 51 (47.7) | 11 (21.6) | 40 (78.4) | ||
| Female | 56 (52.3) | 17 (30.4) | 39 (69.6) | ||
| Age, yr | 0.720 | ||||
| < 30 | 73 (68.2) | 19 (26.0) | 54 (74.0) | ||
| 30–49 | 19 (17.8) | 4 (21.0) | 15 (79.0) | ||
| ≥ 50 | 15 (14.0) | 5 (33.3) | 10 (66.7) | ||
| Previous psychiatric history | 0.417 | ||||
| Yes | 11 (10.3) | 24 (25.0) | 72 (75.0) | ||
| No | 96 (89.7) | 4 (36.4) | 7 (63.6) | ||
| Underlying diseaseb | 0.748 | ||||
| Yes | 5 (4.7) | 1 (20.0) | 4 (80.0) | ||
| No | 102 (95.3) | 27 (26.5) | 75 (73.5) | ||
| COVID-related symptoms | 0.997 | ||||
| Yes | 65 (60.7) | 17 (26.2) | 48 (73.8) | ||
| No | 42 (39.3) | 11 (26.2) | 31 (73.8) | ||
| Total duration of isolation, day | 0.061 | ||||
| 0–10 | 49 (45.8) | 13 (26.5) | 36 (73.5) | ||
| > 10 | 58 (54.2) | 15 (25.9) | 43 (74.1) | ||
Values are presented as number (%).
COVID-19 = coronavirus disease 2019, CTC = community treatment center.
aP value by χ2 test; bUnderlying disease includes: hypertension, diabetes and asthma.
The relationships between depression, anxiety, PTSD and clinical characteristics
To identify the relationships between depression, anxiety, PTSD and clinical characteristics among the participants, sex-and age-adjusted logistic regression models were applied for analysis (Table 2). Previous psychiatric history was significantly associated with a depressed mood in the PHQ-9 scale (adjusted OR [aOR], 11.76; 95% CI, 2.67–51.92). COVID-19 stigma was also related to a depressed mood (aOR, 7.66; 95% CI, 2.76–21.29). Similar results were observed for the relationship between anxiety and clinical characteristics. A previous psychiatric history and COVID-19 stigma were significantly associated with the anxiety of patients (aOR, 10.15; 95% CI, 2.43–42.40, and aOR, 10.43; 95% CI, 3.04–35.75, respectively). In the case of PTSD, the participants with a previous psychiatric history were more likely to have PTSD (aOR, 11.88; 95% CI, 1.83–77.20). COVID-19 stigma and the total duration of isolation were significantly associated with PTSD (aOR, 8.77; 95% CI, 1.40–55.01, and aOR, 8.94; 95% CI, 1.41–56.60, respectively).
Table 2. Multivariate logistic regression analysis on relationship between depression, anxiety, PTSD and clinical characteristics among the patients in the CTC.
| Variables | Total | Depression (PHQ-9) | Anxiety (GAD-7) | PTSD (PCL-5) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |||
| Sex | 0.425 | 0.539 | 0.100 | |||||
| Male | 51 (47.7) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| Female | 56 (52.3) | 1.46 (0.58–3.67) | 1.42 (0.46–4.35) | 0.16 (0.02–1.43) | ||||
| Age, yr | 0.103 | 0.125 | 0.675 | |||||
| < 30 | 73 (68.2) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| ≥ 30 | 34 (31.8) | 2.16 (0.85–5.46) | 2.36 (0.79–7.05) | 1.47 (0.24–8.94) | ||||
| Previous psychiatric history | 0.001 | 0.001 | 0.010 | |||||
| No | 96 (89.7) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| Yes | 11 (10.3) | 11.76 (2.67–51.92) | 10.15 (2.43–42.40) | 11.88 (1.83–77.20) | ||||
| COVID-related symptoms | 0.732 | 0.952 | 0.278 | |||||
| No | 42 (39.3) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| Yes | 65 (60.7) | 1.18 (0.46–3.04) | 0.97 (0.31–2.98) | 3.42 (0.37–31.45) | ||||
| Perceived stigma | < 0.001 | < 0.001 | 0.020 | |||||
| 25%–100% | 79 (73.8) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| Upper 25% | 28 (26.2) | 7.66 (2.76–21.29) | 10.43 (3.04–35.75) | 8.77 (1.40–55.01) | ||||
| Total duration of isolation, day | 0.139 | 0.206 | 0.020 | |||||
| 0–10 | 49 (45.8) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| > 10 | 58 (54.2) | 2.48 (0.75–8.28) | 2.39 (0.62–9.21) | 8.94 (1.41–56.60) | ||||
PTSD = post-traumatic stress disorder, CTC = community treatment center, PHQ-9 = patient health questionnaire-9, GAD-7 = generalized anxiety disorder-7, PCL-5 = PTSD checklist for DSM-5, OR = odds ratio, CI = confidence interval, COVID = coronavirus disease.
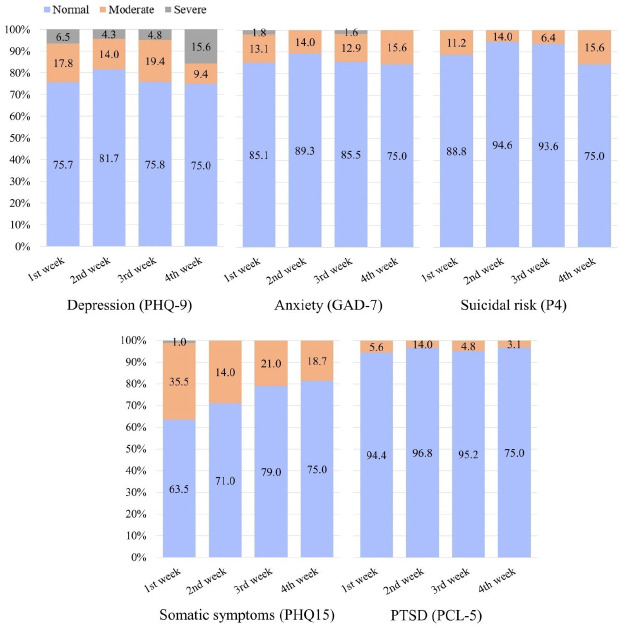
Trends in the psychiatric distress during the isolation period in the CTC
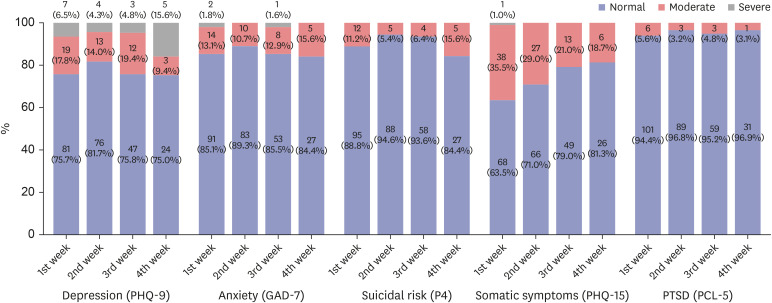
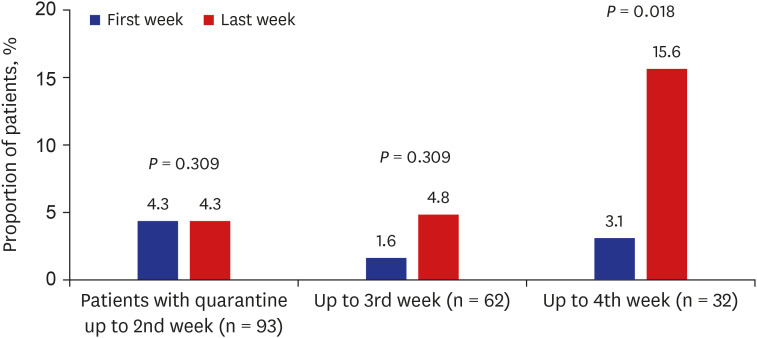
The psychiatric distress in the residents showed no significant trend change except for depression and somatic symptoms (Fig. 1). In the case of depression, the proportion of people with severe depression (PHQ-9 ≥ 10) was 15.6% at week 4, which increased significantly (P = 0.018) (Fig. 2). There was no significant difference over time in anxiety, and the proportion of patients with moderate suicide risk was the highest at week 4, but it also did not show a significant difference over time. In the case of somatic symptoms, rather, it tended to decrease with time (P = 0.014), and there was no significant difference in PTSD over time.
Fig. 1. Changes in the proportion of patients with psychiatric distress during the isolation period in the community treatment center.
PHQ-9 = patient health questionnaire-9, GAD-7 = generalized anxiety disorder-7, P4 = suicidality screener, PHQ-15 = patient health questionnaire-15, PTSD = post-traumatic stress disorder, PCL-5 = PTSD checklist for DSM-5.
Fig. 2. Changes in the proportion of patients with depressive mood according to the isolation period in the community treatment center.
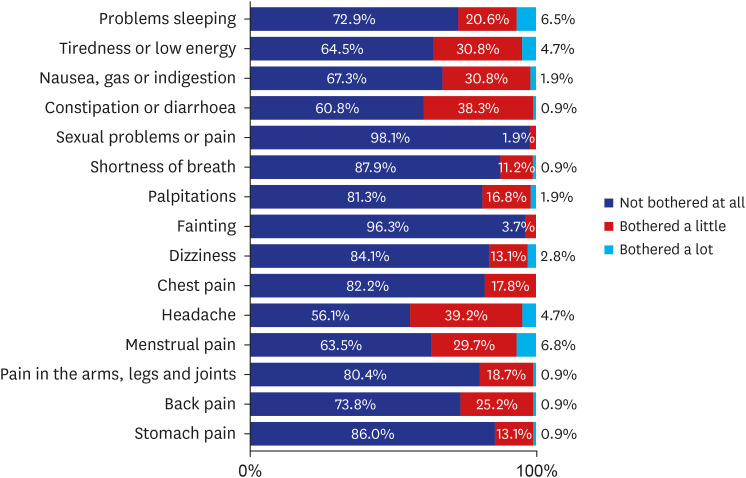
Intensity of somatic symptoms of the mild COVID-19 patients in the CTC
As shown in Fig. 1, the psychiatric distress most frequently reported by residents in the first week of admission was somatic symptoms. For each somatic symptom, the most frequent complaint was a headache (Fig. 3), followed by constipation or diarrhoea. The somatic symptoms most rarely reported by residents were sexual problems or pain.
Fig. 3. Intensity of somatic symptoms of the mild coronavirus disease 2019 patients in the community treatment center.
Symptoms are measured by patient health questionnaire 15.
Psychiatric intervention during the isolation period in the CTC
At the time of admission, all patients completed the PHQ-2 and GAD-2, and psychiatric intervention was offered if each scale was 3 or higher. During patients’ stays in the CTC, psychiatric consultation was offered for patients who showed symptoms on their weekly mental health assessments or who complained of emotional distress to the monitoring medical staff of the CTC. A total of 29 patients were provided with 30-minute sessions of general supportive psychotherapy via video-calls with the counselling psychiatrist, with an average of 2.8 counselling sessions for each patient (Appendix 3). In addition, 7 of those patients were also prescribed psychotropic medications. The average number days of the psychotropic prescription was 8.14 ± 6.69 days.
DISCUSSION
During the patients' first week of stay in the CTC, depression did not seem to be more prevalent than that of the general population in Korea. The prevalence of depression with PHQ-9 ≥ 10 was 6.5% among the study subjects for first week stay in the CTC, while in the general Korean population, the prevalence of PHQ-9 ≥ 10 depression was 6.7% (Shin, 2017). For the GAD-7, there are no population level data in Korea, but PTSD is possibly more prevalent among the patients in the CTC than the estimates from general population, though the data are not directly comparable due to different measures (Cho 2015, Jeon 2007). One literature from China reporting the mental health status among those quarantined as having close contacts with COVID-19 and frontline medical personnel showed a 22.1% prevalence of depression with PHQ-9 ≥ 5 and a 22.2% prevalence of anxiety with the GAD-7 ≥ 5.24 Our study sample showed more depression and less anxiety (24.3% PHQ-9 ≥ 5 depression and 14.9% GAD-7 ≥ 5 anxiety) since our subjects are not close contacts or medical personnel under surveillance, but rather are confirmed mild cases; therefore, these results are not comparable. The prevalence of more-than-moderate depression (PHQ-9 ≥ 5), anxiety (GAD-7 ≥ 5) and possible PTSD remained similar across the four weeks of observations, though the prevalence of severe depression (PHQ-9 ≥ 10), which can be regarded as clinical depressive disorder, increased after four weeks of stay. In contrast, somatic symptoms measured by the PHQ-15 seemed to decrease during their stay.
The stigma of the COVID-19 infection and previous psychiatric history were two important risk factors for depression and anxiety, as well as possible PTSD during the first week of stay in the CTC. It is of note that the total duration of isolation until the first mental health assessment (that is, the sixth day of stay in the CTC), which would include the self-isolation period at home and 6 or 7 days in the CTC, was not a significant risk factor for possible depression and anxiety, while it was a significant risk factor for possible PTSD.
The stigma of the COVID-19 infection is indeed an important societal concern. The current COVID-19 outbreak has provoked the social stigma of those infected, as well as discriminatory behaviors towards foreigners, certain ethnic groups or other minority populations including LGBTQs worldwide, almost to the level of xenophobia in some countries.25,26,27,28 Even the necessary public health measures would have created tensions leading to social stigma if they were not carefully prepared and conducted.29 As UNICEF clarified in their guide for social stigma associated with COVID-19, the situation itself - the newness of the disease, the fear of the unknown, and the ease of associating that fear with “others” in this COVID-19 situation30 - looks very volatile. There is a plethora of hatred responses from the media and SNS that can be observed every day. However, stigmatizing and labelling others potentially lead to deviant behaviours, which might include the concealment of the infection, the delay of immediate treatment, or the refusal of healthy behaviors, and might ultimately undermine the much needed social cohesion and solidarity during the crisis. Of course, on an individual level, stigma and labelling will lead to unnecessary suffering and possible mental health problems for COVID-19 patients and their families. In these regards, the public health system should also concern itself with mitigating the stigma of the COVID-19 infection if COVID-19 containment efforts are to truly be successful. Stigma mitigation programmes such as anti-stigma education, advocacy for patients and their families and media monitoring will be important in this regard, but more importantly, careful, balanced attention to human rights should be given by government and public health authorities, as well as medical institutions providing treatment and quarantining.
On the individual level, the important risk of mental health issues such as depression, anxiety and PTSD can be found in one's previous psychiatric history. It can be expected that personal vulnerability poses as an important risk factor for mental health problems during any social crisis, and several studies involving disaster and refugee settings31,32 indicated that one's previous psychiatric history was a major mental health risk. In addition to the fact that quarantine and isolation inevitably place infected persons in a closed space, the stress of a sudden life change, be it as short as a month, and the degree of uncertainty regarding the prognosis or when they are going to be clear of the virus would contribute to the aggravation or recurrence of existing mental disorders among the patients placed in quarantine. Additionally, in these prolonged disaster equivalent situations, many patients with chronic illnesses including mental disorders will find it difficult to obtain the necessary medications or psychosocial supports both because of their own isolation and the shut-down of healthcare facilities such as clinics and pharmacies, and this would make the already dire situation much worse. Therefore, special care should be given to existing mental disorders for those admitted with mild COVID-19 symptoms. Vigorous screening for mental health symptoms and assessment of patients' past psychiatric history should be mandatory during admission, and possibly at regular intervals during their stay; and counselling psychiatrists or psychologists should be on hand for further assessment and intervention. Additionally, the isolation duration before first mental health assessment (during the first week of admission) did not affect the risk of depression or anxiety, though it did affect the risk of PTSD symptoms. Most of the patients admitted to the CTC were self-isolated in their own houses before coming to the CTC. The fear and anxiety of the unknown viral disease, the feeling of containment, adequate medical care not being readily available while all the media warned about the seriousness of the disease, and the self-isolation period might be traumatic, even if patients had minimal symptoms from the virus.
However, the consulting psychiatrist of the center reported that many of the people who requested counselling on admission but did not have a past psychiatric history expressed quick relief of their worries and anxiety after a few days of stay in the CTC because they felt that now they were placed in professional and adequate care. The gradual decrement of patients with significant somatic symptoms according to the PHQ-15 might also be explained by this factor since stress and emotional distress would cause vague physical symptoms, even without the presence of the formal somatoform disorder.
Another result of note regarding the isolation period was that although the majority of the people admitted to this CTC were discharged in less than 4 weeks, the prevalence of a possible depressive disorder (that is, severe depressive symptoms according to the PHQ-9) was seen to increase after 4 weeks of stay. The consulting psychiatrist reported that the sense of isolation, deprivation and uncertainty started to take over the sense of security among those individuals whose stay extended beyond four weeks. One study from China during the H1N1 pandemic of 2009 reported that a short quarantine of 7 days did not have a negative psychological effect on those quarantined.33 Therefore, care should be taken for not to prolong the isolation without the appropriate clinical necessity, and the viral test scheduling and discharge guidelines should be well balanced over the protection of the general public and those quarantined.
A recent review emphasizes that information & communication, the provision of supplies, minimal duration of isolation and voluntary quarantine rather than required quarantine are key factors for psychological mitigation during the COVID-19 crisis.9 Various international organizations also emphasize that the first step in mental health promotion during the disaster would be providing basic services (food, shelter, water, basic health care, and the control of communicable diseases), security, the restoring of communication (telephone lines, etc.) and providing relevant information for those affected.34,35 This means that providing a sense of safety with the fulfilment of basic needs, communication with their important ones, and a sense of what happened and what will happen in the future are important disaster management principles, especially for the promotion of mental health and psychosocial well-being. From this perspective, the stay in the CTC was likely seen as humane, caring, and secure by the individuals admitted here and not as a traumatic isolation forced by this unprecedented and unexpected disaster. The authors believe that sufficient human and medical resources deployed for medical surveillance and caring, individual and spacious spaces, the basic sense of privacy, and maintained connectivity to the outside with various IT technologies would be the important factors in the successful operation of containment facilities during a viral outbreak crisis, both for the containment of the virus and the protection of the psychosocial well-being and mental health of patients.
We found that the CTC model would be one effective innovation to counter a mass outbreak such as the current COVID-19 crisis. The CTC can take care of the patients with minimal viral symptoms and enable the hospitals to focus on more serious cases; furthermore, the CTC is able to provide much needed psychosocial support for the victims of COVID-19. The CTC seems to change the possible traumatic experience of quarantine into a more humane and cared-for experience. The authors expect that establishing well-provided CTCs for an infectious outbreak such as the current COVID-19 crisis possibly decreases the total social cost of the situation. This decrease occurs not only by making the whole containment system more efficient but also by making the quarantine experience more acceptable to the public than simple isolation facilities.
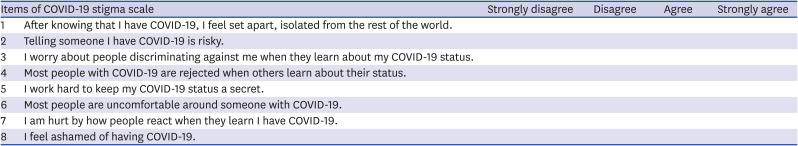
Appendix 1
COVID-19 stigma scale
The COVID-19 stigma is an adjusted version of the Middle East respiratory syndrome stigma scale,21 which is derived by the modification of short version of the human immunodeficiency virus stigma scale.23 Responses to each statement are rated on a four-point Likert scale from “strongly disagree” to “strongly agree,” where higher scores indicate higher level of stigma.
COVID-19 = coronavirus disease 2019.
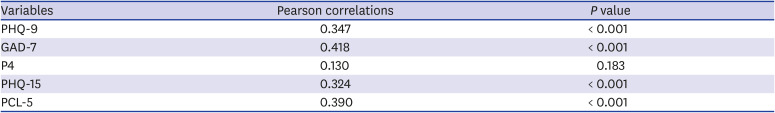
Appendix 2
Pearson correlations of stigma index with other validated questionnaires
Cronbach's α = 0.935.
PHQ-9 = patient health questionnaire-9, GAD-7 = generalized anxiety disorder-7, P4 = suicidality screener, PHQ-15 = patient health questionnaire-15, PCL-5 = PTSD checklist for DSM-5.
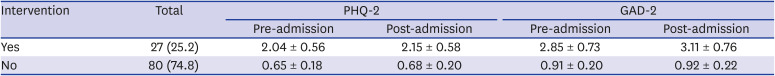
Appendix 3
Pre and post admission PHQ-2, GAD-2 scores according to psychiatric intervention
Values are presented as number (%) or mean ± standard deviation.
PHQ-2 = patient health questionnaire-2, GAD-2 = generalized anxiety disorder-2.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Sohn JH, Park HW, Lee YJ, Cho B.
- Data curation: Sohn JH, Kang E.
- Formal analysis: Kang E, Lee SY.
- Investigation: Kang E, Lee SY, Kim MS, Jung H, Kim KH, Kim KN.
- Methodology: Sohn JH, Park HW, Lee YJ, Cho B.
- Writing - original draft: Kang E, Lee SY, Sohn JH.
- Writing - review & editing: Kang E, Lee SY, Kim MS, Jung H, Kim KH, Kim KN, Cho B, Sohn JH.
References
- 1.Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35(10):e112. doi: 10.3346/jkms.2020.35.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Truog RD, Mitchell C, Daley GQ. The toughest triage—allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973–1975. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 3.Park PG, Kim CH, Heo Y, Kim TS, Park CW, Kim CH. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Korean Med Sci. 2020;35(13):e140. doi: 10.3346/jkms.2020.35.e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gammon J. The psychological consequences of source isolation: a review of the literature. J Clin Nurs. 1999;8(1):13–21. doi: 10.1046/j.1365-2702.1999.00201.x. [DOI] [PubMed] [Google Scholar]
- 6.Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 7.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbisch D, Koenig KL, Shih FY. Is there a case for quarantine? perspectives from SARS to Ebola. Disaster Med Public Health Prep. 2015;9(5):547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim SW, Lee KS, Kim K, Lee JJ, Kim JY Daegu Medical Association. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. 2020;35(15):e152. doi: 10.3346/jkms.2020.35.e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korea Centers for Disease Control and Prevention. COVID-19 Response Guideline. 8th ed. Cheongju: Korea Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 12.Kang E, Lee SY, Jung H, Kim MS, Cho B, Kim YS. Operating protocols of a community treatment center for isolation of patients with coronavirus disease, South Korea. Emerg Infect Dis. 2020;26(10):2329–2337. doi: 10.3201/eid2610.201460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Dube P, Kroenke K, Bair MJ, Theobald D, Williams LS. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Prim Care Companion J Clin Psychiatry. 2010;12(6):PCC.10m00978. doi: 10.4088/PCC.10m00978blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Washington D.C.: U.S. Department of Veterans Affairs; 2013. [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 18.An JY, Seo ER, Lim KH, Shin JH, Kim JB. Standardization of the Korean version of screening tool for depression (patient health questionnaire-9, PHQ-9) J Korean Soc Biol Ther Psychiatry. 2013;19(1):47–56. [Google Scholar]
- 19.Ahn JK, Kim Y, Choi KH. The psychometric properties and clinical utility of the Korean version of GAD-7 and GAD-2. Front Psychiatry. 2019;10:127. doi: 10.3389/fpsyt.2019.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim JW, Chung HG, Choi JH, So HS, Kang SH, Kim DS, et al. Psychometric properties of the Korean version of the PTSD checklist-5 in elderly Korean veterans of the Vietnam War. Anxiety Mood. 2017;13(2):123–131. [Google Scholar]
- 21.Park HY, Park WB, Lee SH, Kim JL, Lee JJ, Lee H, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020;20(1):605. doi: 10.1186/s12889-020-08726-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lyoo YC, Ju S, Kim E, Kim JE, Lee JH. The patient health questionnaire-15 and its abbreviated version as screening tools for depression in Korean college and graduate students. Compr Psychiatry. 2014;55(3):743–748. doi: 10.1016/j.comppsych.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Wiklander M, Rydström LL, Ygge BM, Navér L, Wettergren L, Eriksson LE. Psychometric properties of a short version of the HIV stigma scale, adapted for children with HIV infection. Health Qual Life Outcomes. 2013;11(1):195. doi: 10.1186/1477-7525-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu S, Wu Y, Zhu CY, Hong WC, Yu ZX, Chen ZK, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun. 2020;87:56–58. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stop the coronavirus stigma now. Nature. 2020;580(7802):165. doi: 10.1038/d41586-020-01009-0. [DOI] [PubMed] [Google Scholar]
- 26.Sternlicht A. With new COVID-19 outbreak linked to gay man, homophobia on rise in South Korea. [Updated May 12, 2020]. https://www.forbes.com/sites/alexandrasternlicht/2020/05/12/with-new-covid-19-outbreak-linked-to-gay-man-homophobia-on-rise-in-south-korea/?sh=71c422149099.
- 27.Shin H, Cha S. South Koreans call in petition for Chinese to be barred over virus. [Updated January 28, 2020]. https://www.reuters.com/article/us-china-health-reaction-southkorea/south-koreans-call-in-petition-for-chinese-to-be-barred-over-virus-idUSKBN1ZR0QJ.
- 28.Kuo L, Davidson H. They see my blue eyes then jump back' – China sees a new wave of xenophobia. [Updated March 29, 2020]. https://www.theguardian.com/world/2020/mar/29/china-coronavirus-anti-foreigner-feeling-imported-cases.
- 29.Logie CH, Turan JM. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. 2020;24(7):2003–2006. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.UNICEF. Social stigma associated with COVID-19: a guide to preventing and addressing social stigma. [Updated March 2020]. https://www.unicef.org/documents/social-stigma-associated-coronavirus-disease-covid-19.
- 31.Acarturk C, Cetinkaya M, Senay I, Gulen B, Aker T, Hinton D. Prevalence and predictors of posttraumatic stress and depression symptoms among Syrian refugees in a refugee camp. J Nerv Ment Dis. 2018;206(1):40–45. doi: 10.1097/NMD.0000000000000693. [DOI] [PubMed] [Google Scholar]
- 32.Alpak G, Unal A, Bulbul F, Sagaltici E, Bez Y, Altindag A, et al. Post-traumatic stress disorder among Syrian refugees in Turkey: a cross-sectional study. Int J Psychiatry Clin Pract. 2015;19(1):45–50. doi: 10.3109/13651501.2014.961930. [DOI] [PubMed] [Google Scholar]
- 33.Wang Y, Xu B, Zhao G, Cao R, He X, Fu S. Is quarantine related to immediate negative psychological consequences during the 2009 H1N1 epidemic? Gen Hosp Psychiatry. 2011;33(1):75–77. doi: 10.1016/j.genhosppsych.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Inter-Agency Standing Committee. IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Geneva: IASC; 2007. [DOI] [PubMed] [Google Scholar]
- 35.International Federation Reference Centre for Psychosocial Support. Psychosocial interventions A handbook. Copenhagen: International Federation Reference Centre for Psychosocial Support; 2009. [Google Scholar]