Abstract
Background
Effective recruitment of patients by health professionals is challenging but pivotal to the success of clinical trials. Many trials fail to include the required number of participants, which affects the power of the study, generalizability of results, and timely dissemination of positive outcomes. Existing research is inconclusive regarding factors influencing recruitment results, and most research does not focus on perceptions of recruiting health professionals themselves. Therefore, thorough evaluations of recruitment facilitators and barriers in trials are needed in order to optimize future patient recruitment in trials. We observed divergent recruitment results among nurses who recruited diabetes patients to our trial, which examined the effectiveness of an eHealth programme. Therefore, we aimed to describe nurses’ recruitment results and related shifts over time, and to qualitatively explore factors influencing nurses’ recruitment results.
Methods
Nurses’ recruitment results and related temporal shifts were derived from trial data (NTR6840). Based on their recruitment results, nurses were categorized as non-, low-, medium-, or high-recruiters. Subsequently, a subset of nurses per group participated in an individual semi-structured telephone interview. Interviews were analysed using NVivo software, applying an inductive coding approach.
Results
Ninety-six nurses participated in our trial and recruited on average seven patients (range: 0–32). Fifteen nurses did not recruit any patients. Most patients were recruited close to recruitment onset. Nurses who did not recruit patients close to recruitment onset generally ended up recruiting no patients. Data show a relatively high number of early recruited patients that progressively declined over time. High-recruiters were generally successful throughout the entire recruitment period. Recruitment facilitators and barriers comprised organizational, study, patient, and especially recruiter characteristics. Contrary to non- and low-recruiters, medium- and high-recruiters reported more in-depth knowledge about the study and trial requirements, expressed more personal participation-related benefits and fewer barriers, and incorporated more recruitment activities, reminders, and barrier-focused coping strategies.
Conclusion and implications
To optimize patient recruitment to clinical trials, suggested intervention targets include the continued inclusion of recruiters after initial recruitment onset and the encouragement of early recruitment success. A personalized approach may aid recruiters to become and remain successful. Primarily, it is important to provide recruiters with sufficient information on trial requirements and to address salient benefits for participation in the trial, both for themselves and for their patients. Finally, teaching recruiters skills on how to overcome barriers may further enhance motivation and recruitment capacities.
Keywords: Recruitment, nurses, randomized controlled trial, information, motivation, intention
Background/aims
Recruiting sufficient patients for randomized controlled trials (RCTs) is challenging, but pivotal to the success of research.1 Many trials do not achieve their required sample size, which can jeopardize generalizability of results and the study’s statistical power, reduce study efficiency due to extended recruitment time, and lead to premature trial discontinuation.2–6 Moreover, the dissemination of potential effective treatments to the general population may be delayed.7 Existing research highlights the paucity of conclusive evidence regarding factors influencing recruitment results.8 Researchers have been called to thoroughly evaluate their applied recruitment strategies in order to optimize future patient recruitment and timely translate positive results into practice.1
Often patient recruitment manifests through efforts of health professionals, as they are relevant contact points for patients.4,9 Whether professionals enrol a sufficient number of patients depends on multiple factors including organizational, study, patient, and recruiter factors.8,10 Organizational factors entail the number of patients seen by professionals, time constraints, and the institutional culture regarding research.2,9–11 Study factors include the strictness of trial eligibility criteria, the recruitment protocol, the informed consent procedure, and support from the research team.9,10 Patient factors comprise patients’ motivation and willingness to participate, while recruiter factors include the professionals’ enthusiasm to contribute to successful research, required knowledge and skills, their intention to implement recruitment tasks, and emotional and intellectual challenges associated with the nature of RCTs.4,9,11,12 For instance, it is well known that not all professionals who intend to recruit patients will actually succeed.9 However, most research on factors of patient recruitment by professionals relies on evidence gathered through narrative reviews or conclusions drawn by researchers, rather than on experiences of relevant professionals themselves.10,13 Perspectives of recruiting professionals themselves might provide insight into the importance of previously identified factors as well as additional factors influencing recruitment results. Moreover, these perspectives might identify how changeable these factors are and how they can best be addressed in order to enhance success.
Recently, we conducted a 6-month RCT in primary and secondary care to examine the effectiveness of a novel eHealth programme, in comparison with a control arm receiving care as usual. Both arms started with an identical online baseline questionnaire, after which they were informed of their arm allocation. Participants allocated to the control arm were not given access to the eHealth programme during the trial period, but were able to request programme access upon trial completion. The programme aimed to improve patient adherence to type 2 diabetes mellitus (T2DM) treatment recommendations, that is, healthy lifestyle changes and pharmaceutical strategies.14,15 Patients were recruited by their practice nurse or diabetes nurse which are their primary contact points of care in the Netherlands.14 After recruitment completion, we observed considerable variations in recruitment results among nurses. This triggered us to thoroughly evaluate recruitment and to explore factors possibly influencing recruitment results.
This study aimed to (1) describe nurses’ recruitment results in our trial, that is, the number of patients recruited per nurse, and temporal shifts in recruitment results and (2) qualitatively explore factors influencing recruitment results as perceived by nurses themselves, in order to define potential targets for improving patient recruitment in comparable trials.
Methods
Study design
Trial data were used to describe nurses’ recruitment results and its temporal shifts. Subsequently, an interview study was conducted among a subset of nurses who engaged in patient recruitment. The study was approved by the Medical Ethics Committee of the MUMC+(18.4.129).
Patient recruitment strategy
Nurses working in primary or secondary care across the Netherlands were approached through email, telephone calls, letters, and social-media platforms, to recruit at least eight patients within a period of 6 months. Nurses were able to sign up until 2 months before the end of the patient recruitment period (November 2017 to May 2018).
Patient eligibility criteria included T2DM diagnosis ≥1 year, 40–70 years old, using at least one form of diabetes pharmacotherapy, and having no walking disability. Exclusion criteria included not speaking or understanding the Dutch language, having no access to the Internet, and applying insulin pump therapy.
The patient recruitment procedure was pilot-tested to last approximately 3 min and subsequently included programme log-on, checking the patient’s eligibility, facilitating patients to make an informed decision by informing them about the procedures of the study and explaining potential consequences, inviting the patient to participate, and (if positive) patient registration. To support this process, all nurses received an information package prior to the start of the recruitment period, which was pilot-tested to take about 15–30 minutes to read. The package included a detailed description of the study, the trial, the content of the eHealth programme, potential consequences for the patient participating in the trial, log-on data (to register patients), and a roadmap on how to register patients. Once registered, patients received log-on data, additional information, and time to consider definitive participation. If positive, consecutively the informed consent procedure, randomization, and baseline assessment occurred. The programme development and study protocol are described elsewhere16 and effectiveness results will be published separately.
The power calculation revealed that 116 patients with a completed 6-month follow-up assessment were required per trial arm to detect a clinically meaningful difference in overall patient adherence.16 As we expected patient attrition of 50% between baseline and follow-up assessment completion, we aimed to include 464 patients with a completed baseline assessment. As not all patients were expected to participate after being recruited by their nurse, we aimed to initially recruit approximately 700 patients, that is, 150% of the required 464. For these analyses, a recruited patient was defined as a patient recruited to the programme by their nurse, independent of ultimately consenting or completing the baseline or follow-up assessment.
Procedure interviews
Nurses were divided into four recruitment groups, that is, non-, low-, medium-, and high-recruiters, based on their markedly differing recruitment results. A detailed description of the division of nurses into these four groups is presented in the ‘Results’ section. Per group, all nurses were assigned numbers which were then entered in the randomization website random.org. Of the entered numbers per group, four numbers were randomly selected by the website. The nurses represented by these selected numbers were then approached by email to participate in a telephone interview. In case of non-response within 2 weeks or refusal by a particular nurse, randomly another nurse from the same group was selected through the website procedure and subsequently invited to participate. The same procedure was repeated until four nurses per group were willing to participate. Approximately eight recruiters per group had to be approached to reach the intended number of four participating nurses per group. After conducting approximately three-quarters of the initially planned interviews, data saturation was considered reached. Subsequently, no additional interviews were conducted on top of the 16 planned interviews. Interviews were scheduled from May to June 2018, lasted 15–30 min each, were conducted by S.V. and L.V., and were audio-recorded.
Measurement
The interviews were semi-structured using a one-page topic guide that was based on the grounded theory approach, reflected by a flexible and open interview structure.17 Prearranged topics included questions on demographic characteristics, and on organizational, study, recruiter, and patient factors. Organizational factors included topics such as work pressure and the organization’s attitude towards eHealth. Study factors entailed knowledge concerning trial and programme requirements. Recruiter factors included motives for signing up and the implementation, course, and facilitation of patient recruitment. Patient factors comprised their motives to accept or decline participation from the recruiter perspective.
Analyses
Recruitment results and interviewee sample characteristics were described using frequencies in SPSS software. All interviews were transcribed verbatim, anonymized, and analysed using NVivo10 software.18 Content analysis was performed by S.V. and L.V. and was guided by the coding process for inductive analyses.19 An inductive coding approach is common in qualitative data analyses, when having applied a grounded theory perspective.17 First, transcripts were closely read through and discussed among both researchers. Second, transcript segments were highlighted if considered to contain meaningful information related to the study objectives. Next, segments were labelled into over 20 categories. Subsequently, in order to limit redundancy and overlap, the number of categories was reduced to approximately 10. These categories were then entered in NVivo as ‘nodes’ to which relevant text segments were assigned. Last, the number of categories was decreased to four main topics: (1) organizational, (2) study, (3) recruiter, and (4) patient factors. Within these topics, the views of the nurses were listed and it was qualitatively described whether these views were shared by nurses from all or only specific recruitment groups. Within the recruitment groups, it was specified whether all, most, half of the nurses, or only one nurse within the recruitment group shared a particular view. S.V. coded all the interviews, while L.V. coded two randomly selected interviews from each recruitment group. Subsequently, the intercoder reliability and Cohen’s kappa were assessed using the coding comparison query. This resulted in a percent agreement of 99%, reflecting that interview passages were assigned to the same nodes by both researchers in 99% of the cases. The Cohen’s kappa showed to be 0.83, reflecting a good strength of intercoder agreement.18,20 Results of the interviews are supported by quotes (see Table 2).
Table 2.
Interviewee quotes.
| Quote number | Respondent | Quote |
|---|---|---|
| 1 | NR3_PN | ‘It’s been initiated in some other practices, [apps and such things] … but well, it’s just neither a relevant nor a urgent issue here, I’m already satisfied if they’re willing to fill in an email survey’. |
| 2 | HR4_DN | ‘Well, we were asked by the physician who was quite enthusiastic. And by coincidence, my colleague – another physician – and me were conducting some innovation work, digitalization and eHealth, so we thought it would fit really well, and that’s why we collaborated in recruitment’. |
| 3 | NR1_PN | ‘Because then I concluded that I had a lot of people who just don’t fit the criteria, and I wasn’t aware of that in advance’. |
| 4 | NR3_PN | ‘I got it [the request to participate] from a colleague and the physician, who already signed-up for us, and then you are in the middle of it. I thought, well let’s see what I can do, but in the end it turns out it wasn’t the same willingness [to participate] … then it doesn’t work, there is not much time’. |
| 5 | HR3_PN | ‘Because I think that eHealth is the key to success of the treatment, particularly for the so-called younger generation … So I think it can have a beneficial effect on health, but also on the work pressure in the general practice’. |
| 6 | LR1_PN | ‘I thought, well that should be easy, we are just going to do this on spec, and that doesn’t work. I think I was insufficiently aware of what was needed so actually I might’ve said “yes” too enthusiastically … and afterwards I invested way too little to make it successful’. |
| 7 | MR4_DN | ‘I say: “Well, there’s a new tool, which may have a positive contribution to better regulation [of your diabetes]”. And I say that it’s not that much work at all. People are generally scared that it will take a lot of time, so I indicated that the time investment is quite relative and that they can do it from home’. |
| 8 | NR3_PN | ‘In the end we’re the ones who carry it out, recruiting people, and that’s time consuming. I mean, that’s time that’s taken from your patients … that’s time I cannot spend on direct patient care’. |
| 9 | LR2_PN | ‘If you continuously hear from people: “I don’t want to participate,” or they just don’t fit the [eligibility] profile, then you’ll forget to ask it more easily’. |
| 10 | NR1_PN | ‘Because in the beginning I asked them and they said: “No I don’t feel like participating … such a hassle.” So at a given moment the threshold to ask it becomes higher, it becomes less prioritized and you forget it’. |
| 11 | NR2_PN | ‘In our practice we are used to high rates of employee turnover, so I worked at a fast pace with very little space to think … we have had a very hectic six months and at a given moment it became less prioritized and too much for me … it was no longer automatic … I’m not only involved in diabetes and then for me it [recruitment] moved to the background and did not get priority, sorry’. |
| 12 | LR3_PN | ‘When I had too little time to explain it or if the consultation session was over, then I didn’t bring it up’. |
| 13 | MR2_PN | ‘Well sometimes a bright moment like “yes,” here we go again, we are going for it. And then I thought … then I had one or two people who I could’ve asked. Then you are more alert and you go for it, and then there are a couple [of patients] who say no or who don’t have Internet … and then [the alertness] goes down, it goes up and down’. |
| 14 | HR3_PN | ‘Well, [recruitment] during consultations was difficult, I had to be aware of it, because at the end of the consultation I thought: “Ah I totally forgot to ask …,” so I called them afterwards … I preferred the experience of working with a list so I wouldn’t forget anyone, and then I could also schedule my time to invite patients’. |
| 15 | MR1_PN | ‘So, I put the [instruction] card in my sight. Moreover, in my agenda … I see patients from 8:30 AM till 4:00 PM, and the first line [in the agenda] was “MDP,” My Diabetes Profile’. |
| 16 | MR3_DN | ‘There were a lot of people who didn’t want it … the time factor and partly motivation, that it was too much [for them], you know, people with diabetes just don’t want to be reminded of their diabetes that often’. |
| 17 | HR4_DN | ‘While explaining I noticed in patients that they were quickly scared: “Am I stuck to this [study]?” or “Am I forced to do certain things?” and I noticed a lot of reluctance there … But when I started to explain … that they were not obliged to check it weekly or reach certain goals, that it was merely for themselves and that it didn’t have to be carried out in a certain pace … and that’s something the people liked’. |
NR: non-recruiter; LR: low-recruiter; MR: medium-recruiter; HR: high-recruiter; PN: practice nurse; DN: diabetes nurse.
Results
Absolute recruitment results
Ninety-six nurses from across the Netherlands signed up for participation, of which 66 were practice nurses and 30 were diabetes nurses. In total, these 96 nurses recruited 669 patients. Seventy-four nurses were involved immediately from the start, the other 22 enrolled later and had an average recruitment period of 2.8 months. The 74 nurses who participated for the entire recruitment period recruited 538 patients (80%), while the 22 nurses who enrolled later recruited 131 patients (20%). For those nurses who were involved from the start, the absolute recruitment result ranged between 0 and 32 patients, as shown in Figure 1, and on average nurses recruited seven patients (standard deviation (SD) = 7.2). About one-third (36%) reached the target of at least eight patients and 14 nurses (15%) did not recruit any patients.
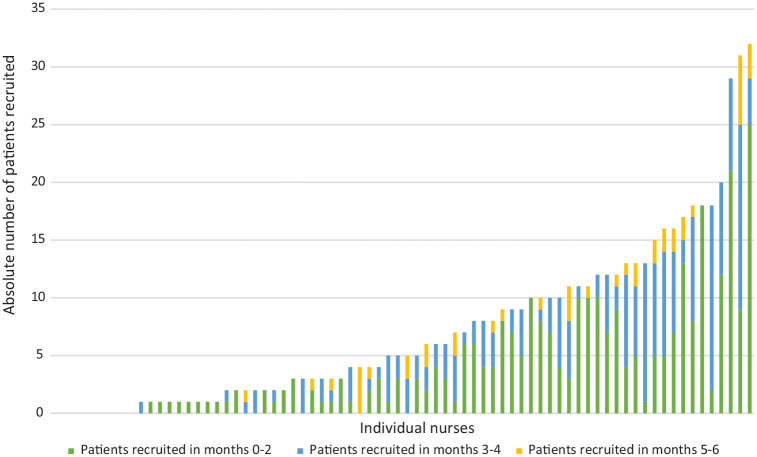
Figure 1.
Absolute recruitment result per 2-month period per nurse (n = 74).
Temporal shifts in absolute recruitment results
As shown in Figure 1, the absolute recruitment results are further subdivided into 2-month periods to indicate in which part of the recruitment period patients were registered by their nurse. These data show a high early recruitment success that progressively declined over time. Of the 538 patients recruited by these nurses, 56% (n = 302) was recruited in the first 2 months. Within the third and fourth month, this number declined to 32% (n = 174) and in the last 2 months to 12% (n = 62). Of the 74 nurses, 15 did not recruit any patients within the first 2 months, of which 9 did not recruit any patients throughout the entire recruitment period. Nurses without recruitment success in the first 2 months recruited 17 patients in total, accounting for 3% of the total number of patients recruited.
Figure 1 shows that nurses with a relatively low absolute recruitment result mainly recruited their limited number of patients in the first 2 months, followed by a progressive decline. In addition, Figure 1 shows that nurses with a relatively medium absolute recruitment result largely recruited their patients in the first 4 months, of which the largest share in the first 2 months. Most nurses with a relatively high absolute recruitment result remained successful throughout the entire recruitment period. Besides recruiting a large share of their patients in the first 2 months, some of those latter nurses showed substantial results in months 3–4.
Standardized recruitment results
The total recruitment period of nurses varied from 2–6 months. Consequently, we standardized nurses’ recruitment results to an average monthly number of recruited patients as shown in Figure 2. When standardized, nurses recruited an average number of 1.4 patients (range: 0–9.5) per month. The standardized recruitment result did not differ between practice nurses and diabetes nurses (p = .51).
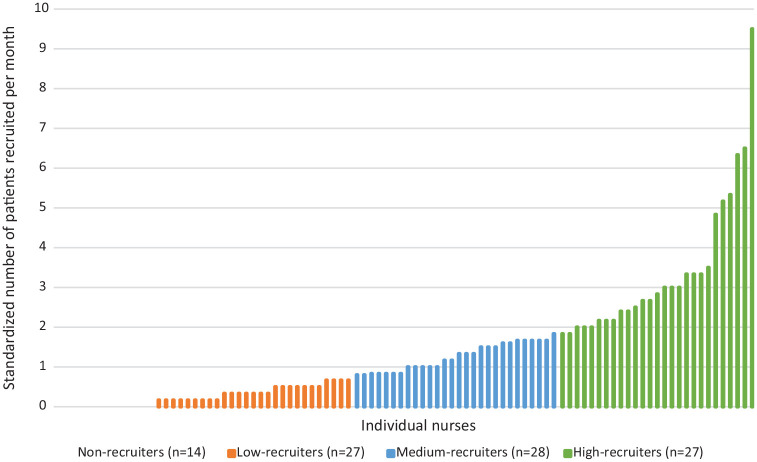
Figure 2.
Standardized recruitment result per month per nurse (n = 96).
The division of nurses in four groups for the interviews was both pragmatic and statistical in nature and was derived from the standardized number of recruited patients per nurse. The first group consisted of nurses who did not recruit any patients (non-recruiters, n = 14). The remaining nurses were divided into three fairly equal sized groups recruiting an average monthly number of 0.2–0.7 patients (low-recruiters, n = 27), 0.8–1.8 patients (medium-recruiters, n = 28), and 1.8–9.5 patients (high-recruiters, n = 27). The standardized average number of 1.4 patients per month was approximately the middle of the range of the medium-recruiters (0.8–1.8 patients). The recruitment groups are depicted with different colours in Figure 2.
Retention of recruited patients
Of the 57 patients recruited by all low-recruiters, 74% (n = 42) went on to consent, of which 86% (n = 36) completed the baseline assessment and in turn 50% (n = 18) completed the follow-up assessment. Of the 182 patients recruited by all medium-recruiters, 73% (n = 132) went on to consent, of which 89% (n = 118) completed the baseline assessment and in turn 60% (n = 71) completed the follow-up assessment. While slightly higher retention percentageswere observed for patients included by high-recruiters with regard to consent and follow-up completion, these differences have not been tested for significance. Of the 430 patients initially included by high-recruiters, 78% (n = 335) went on to consent, of which 88% (n = 295) completed the baseline assessment and in turn 67% (n = 197) completed the follow-up assessment.
Results of the interviews
Sample characteristics of the interviewed nurses are presented in Table 1. Most nurses were female (n = 14), reported extensive working experience, and were employed as practice nurses working in primary care (n = 11). Diabetes nurses, working in secondary care (n = 5), only provided healthcare to patients with diabetes.
Table 1.
Sample characteristics of interviewees (n = 16).
| Nurse characteristics | n (%) | Mean (SD) |
|---|---|---|
| Gender | ||
| Male | 2 (12) | |
| Female | 14 (88) | |
| Nurse type | ||
| Practice nurse | 11 (69) | |
| Diabetes nurse | 5 (31) | |
| Patient population | ||
| Diabetes type 1 and/or 2 | 5 (31) | |
| Chronic patientsa | 11 (69) | |
| Age | 44.9 (9.7) | |
| Years of working as a nurse | 9.4 (6.4) | |
| Weekly consultation hours | 24.3 (6.7) | |
SD: standard deviation.
Including patients with diabetes, chronic obstructive pulmonary disease, asthma, and cardiovascular risk management.
Organizational factors
The majority of all nurses were experienced in recruiting patients to research. Approximately half of all nurses were engaged in parallel research activities during our trial; however, most activities were unrelated to our trial population. In contrast to high-recruiters, half of the non-recruiters mentioned that research involving digital interventions seemed to be neither a relevant nor an urgent topic within their organizations as they described their patient population as largely non-digital oriented (Quote_#1, Quote_#2) (Table 2).
Time and work pressure were expressed by almost all non-, low-, and medium-recruiters and only sporadically by high-recruiters as barriers to recruitment efforts. All nurses, but especially non-recruiters, described their overall patient population as not eligible to participate; patients were commonly characterized as being too old and not digitally oriented (Quote_#3).
Study factors
The study design and procedure were insufficiently clear to most non- and low-recruiters, reflected by little knowledge regarding the eligibility criteria, the programme’s content, the study design, and the randomization procedure. By contrast, all medium- and high-recruiters provided a highly detailed description of the programme, its content, and the randomization procedure. In general, nurses from all groups were pleased with the available support from the research team. Periodic email reminders were valued as helpful and necessary to stay alert.
Recruiter factors
Motives to sign-up
One non-recruiter stated that the decision to participate in the study was made by her physician (Quote_#4). However, all other nurses of all groups expressed their willingness to participate, which was largely supported by positive attitudes about, for example, the importance of research and the novelty of the innovation. Besides, most low-to-high-recruiters argued that the programme could potentially yield personal benefits for their patients and themselves (Quote_#5). In addition, most high-recruiters labelled participation as fitting in their organization’s vision and mentioned that eHealth could serve as a medium to support self-management initiatives.
Implementation of recruitment
All nurses of all groups initially approached their patients through consultations sessions. Most non- and low-recruiters shaped their efforts by expressing their involvement in research without extensively informing and explaining potential study consequences to their patients. Furthermore, most low-recruiters mentioned to execute recruitment efforts without a concrete plan (Quote_#6). By contrast, almost all medium- and high-recruiters indicated to have made efforts to recruit patients by providing information, offering support, being enthusiastic, answering patients’ questions, expressing conviction of the programme’s importance, and addressing positive attributes of eHealth and the programme (Quote_#7). Some high-recruiters stated that providing study information and explaining potential study advantages and disadvantages to patients took 5–10 minutes.
All nurses except high-recruiters stated to prioritize standard discussion topics within their consultations, such as the patient’s well-being and glycaemic control, over introducing patients to the study (Quote_#8). Most of these nurses reported to value the programme as less important because it did not yield immediate benefits for themselves or their patients. In addition, some nurses were reluctant to invest in potential future health improvements related to the programme, as they were unsure about its outcome. Furthermore, for non- and low-recruiters, potential explanatory factors for their poor recruitment result were their, in the view of the research team, unrealistic expectations of the efforts needed and the feasibility of the recruitment process.
The magnitude of patients declining the invitation to participate evoked negative emotional and practical responses in most non- and low-recruiters and half of the medium-recruiters. Examples of negative emotions entailed guilt for not recruiting patients, disappointment, and discouragement, while in practice this resulted in shifting study recruitment to a lower priority and forgetting recruitment (Quote_#9 and Quote_#10). By contrast, all high-recruiters emphatically expressed being unaffected by patient rejections as they perceived it completely normal if patients would decline participation.
Course of recruitment
All non- and low-recruiters and most of the medium- and high-recruiters forgot patient recruitment at a certain point. In addition, most non- and low-recruiters indicated often not to manage recruiting patients or that the study became of inferior priority (Quote_#11). In most non- and low-recruiters, this process of forgetting and not managing recruitment seemed irreversible, that is, at a certain point they invited no more patients to participate. A lack of time to extensively explain study details and potential study consequences were frequently mentioned reasons for forgetting and not managing recruitment (Quote_#12). One medium-recruiter described the recruitment process as fluctuating, that is, if patients accepted participation, alertness and motivation to recruit would increase, if patients declined participation, alertness would decrease (Quote_#13). One medium-recruiter coped with forgetting recruitment in consultations by telephoning patients afterwards. The majority of the high-recruiters expressed their awareness of forgetting recruitment and coped with this by applying alternative recruitment strategies. For example, two nurses complemented consultation recruitment with telephone calls while another applied telephone calls and email contact instead, because of time constraints during consultations (Quote_#14). Although telephone recruitment was considered practical, most high-recruiters preferred face-to-face recruitment given the possibility to personally inform patients.
Facilitation of recruitment
Half of the non- and low-recruiters, and all medium- and high-recruiters set a target regarding the number of patients they aimed to recruit, which in all cases was higher than the study target set by the research team. In addition, the majority of the participating nurses applied self-initiated reminders to facilitate their recruitment process. Half of the non-recruiters and almost all other recruiters indicated they had put their received instruction materials on their desk as a visual cue. One non-recruiter wrote a reminder note in her agenda, while similar notes were applied by most medium- and high-recruiters (Quote_#15). A shortcut to the programme website was made by some low-recruiters, while most high-recruiters opened the programme website prior to their consultations. Checking patients’ eligibility on appointment lists prior to consultations was frequently applied by medium- and high-recruiters and infrequently by low-recruiters. In addition, a minority of the high-recruiters put up a poster in their practice to raise study awareness and cognitive processing of patients.
Patient factors
Almost all non- and low-recruiters stated that all or the majority of their patients declined study participation, while this occurred to a lesser extent in medium- and high-recruiters. Motivational issues such as no interest or not seeing the purpose of participation, and participation being considered confronting to their disease, were reasons of patients not to participate that all nurses mentioned. Patient barriers to participating were having no time or priority, and insufficient digital skills (Quote_#16).
Generally, nurses characterised most patients who agreed to participate as intrinsically enthusiastic and open to digital innovations. Almost all medium- and high-recruiters stated to have effectively informed and motivated initially reluctant patients (Quote_#17).
Conclusion
This study aimed to (1) describe nurses’ recruitment results and related temporal shifts in a recent trial and (2) explore factors influencing recruitment results as perceived by the nurses themselves.
In our study, 15% of the nurses were non-recruiters which was lower than the 25% reported in other studies. However, in these other studies, recruitment was performed by physicians.4,9,10 Although nurses are considered to play a key role in recruiting patients to clinical trials, figures on nurses’ recruitment results seem to be lacking, which hampers clear comparisons.21 A study comparing recruitment results of nurses to physicians indicated that nurses were as effective and more cost-effective recruiters and suggested a more explicit role of nurses in patient recruitment.22 Compared to existing figures of physician recruitment, our nurses seem to be somewhat more successful in recruiting patients, but further comparative research is required.
Most T2DM patients visit their nurse every 3–6 months;14 our 6-month recruitment period therefore provided sufficient opportunity for patients to be exposed to their nurses’ recruitment efforts. Periodic reminders, available support from the research team, and the brief recruitment procedure may also have contributed to a lower non-recruiter percentage. A similar trial on an intervention to improve medication adherence also showed that about one-third of the physicians reached their set patient target, and that longer time to enrol the first patient was associated with poor recruitment results.10 Initial recruitment failure negatively affects recruiters’ motivation and beliefs about the study’s feasibility, which in turn could slow down or prematurely terminate recruitment efforts.23 In that light, recruiters should aim for early success to maintain motivation and sustain study efficacy beliefs.
From the interview data, we observed a clear dichotomy between non-/low-recruiters compared to medium-/high-recruiters regarding factors influencing recruitment results.
Recruitment process of non- and low-recruiters
The recruitment process of non-/low-recruiters appeared to be similar. Nurses from these recruitment groups showed poor study, programme, and procedure-specific knowledge. This possibly resulted in informing and motivating their patients to an insufficient degree to participate. Generally, all nurses in our trial characterized their patient population as both ineligible and unwilling to participate in our study, which previously also emerged as a barrier for positive recruitment results.4,10,24 Therefore, the insufficient informing and motivating of patients may explain why patients of non-/low-recruiters generally rejected participation. Socio-cognitive models posit that patients’ willingness to participate could be improved by transferring study and programme knowledge and exploring benefits to initiate a patient’s cognitive processing of the decision to participate in a trial.25,26 Furthermore, non-/low-recruiters might benefit from learning coping skills on how to respond to patient rejections, given their subsequent lack of recruitment effort.23 Especially for professionals with little practical recruiting experience, it might be beneficial to apply guided practice in which they are offered demonstrations and training on how to address the study in consultations, and empowered to rehearse recruitment behaviour and overcome challenges.27–29
Non-/low-recruiters viewed the study as less important compared to regular healthcare work and as not immediately rewarding, factors which emerged as recruitment barriers earlier.5,23 In addition, nurses’ time and work pressure were mainly brought-up as barriers to introduce the study to patients. Competing demands and time pressure are also commonly reported barriers to positive recruitment results and hamper fitting research into daily practice.11,23,30,31 Hence, personal benefits and barrier-focused coping strategies need to be incorporated in recruitment enhancing interventions.
Differences between non- and low-recruiters
A non-digital-oriented working environment, unrealistic effort, and feasibility expectations may have contributed negatively to recruitment results of non-recruiters. A lack of empowerment due to practice policy or culture and recruitment efforts taking more time than expected, also emerged as barriers elsewhere.10 Despite acknowledging the value of research, which generally substantiates initial participation,23 no personal benefits for signing-up were brought-up by non-recruiters contrary to low-recruiters, which may explain low-recruiters’ slightly higher results.25,32,33
Recruitment process of medium- and high-recruiters
The recruitment process of medium- and high-recruiters also showed similarities. These nurses expressed various personal benefits of signing up, substantiating their willingness to participate.25 Contrary to non-/low-recruiters, these nurses expressed their enthusiasm in making efforts to inform and motivate patients to participate, which contributes to successful trial recruitment.9 Together with more extensive study knowledge, their enthusiasm may have positively affected confidence and willingness to recruit patients.23
High- and some medium-recruiters applied alternative recruitment strategies to cope with forgetfulness and to overcome time constraints. Recruitment during daily care may be difficult if standard discussion topics leave insufficient room for the introduction of a study.23 Substituting recruitment during consultations by more suitable strategies in case of time constraints, such as email or telephone recruitment is important to increase the likelihood of successful recruitment efforts.34 Moreover, medium-/high-recruiters frequently applied self-initiated reminders, which may have facilitated recruitment efforts, alertness in response to anticipated forgetfulness, and overcoming barriers.35
Differences between medium- and high-recruiters
High-recruiters perceived that participating in the study was in line with their organization’s vision and attitude towards research activities and eHealth initiatives. Favourable organizational circumstances such as a research and innovation-oriented culture have shown to result in fruitful recruitment results earlier.13 Furthermore, high-recruiters did not prioritize standard discussion topics over inviting patients to participate, which may have resulted in discussing the study more frequently. In addition, it seemed that high-recruiters remained consistent recruiters throughout the entire recruitment period, contrary to medium-recruiters whose success seemed to decrease in the final recruitment months. Finally, self-initiated reminders were more often employed by high-recruiters.
Strengths and limitations
First, we provided a thorough evaluation of factors affecting recruitment results. Second, perspectives of recruiters were examined, rather than findings gathered from reviews or perceptions from research teams. Still, as a single study using in-depth methods, the results may not be generalizable to other interventions or settings. Furthermore, the findings are based on comparisons between groups which could also have been divided otherwise. For example, a better division might have been against the targets set by the research team, that is, non-recruiters, up to and including the target of eight patients, and over eight patients. Finally, observational research designs are required to possibly invigorate current findings statistically.
Implications and conclusion
First, if feasible, researchers should continue including recruiters after initial recruitment onset, as we showed that 20% of the patients were enrolled by later entrants. Second, early recruitment success is encouraged as recruiters that recruit patients from the outset are likely to continue to recruit compared with those who do not succeed early on. Third, recruitment results seem to be partly influenced by an integration of recruiter factors such as knowledge, motivation, intention, and self-regulatory capacities.25,26,34,36–38 Although other factors may provide relevant intervention targets to improve results, recruiter factors may be the most viable and changeable domain to intervene in according to Sabaté.39
The intention a professional expresses to recruit patients generally builds on the information provided by the research team, and the motivation a professional has to carry out recruitment activities.38 While nurses are recruited, they should primarily be informed on the study’s content, procedure, feasibility, and benefits to substantiate and enhance their willingness to participate. Furthermore, nurses should be made aware that patient recruitment will require a short-term investment, that is, informing and motivating patients, to ensure that patients have all the information and understanding they need to make a decision whether or not to join the trial. Sufficient motivation of nurses to recruit patients does not necessarily warrant that recruitment activities will take place and that positive results will be achieved.9,34,37 Hence, recruiters should be prepared, skilled, and confident to optimally deliver recruitment efforts, in terms of when, where, and how to act, and how to cope with barriers such as patient rejections, time constraints, and forgetfulness.40 Reminders may facilitate the likelihood of intentions being actually translated into recruitment efforts. However, these may only suit recruiters who have a high intention towards patient recruitment, unintentionally forget recruitment, or perceive recruitment barriers such as time pressure, contrary to nurses who deliberately terminate recruitment.35,41 Nurses who deliberately slow-down or terminate recruitment, or nurses without recruitment results yet, should primarily be approached by informative and motivational messages rather than barrier-focused coping messages or reminders. In sum, in order to optimize patient recruitment in prospective trials, we suggest a personalized approach which addresses specific recruiter needs as this may aid them to become and remain successful.
Acknowledgments
We would like to thank the participating nurses for their valuable time investment in this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the MUMC+ Strategy 2020 fund. The funding source had no involvement in preparing or conducting the research or research article.
ORCID iD: Stan Vluggen  https://orcid.org/0000-0001-6870-5347
https://orcid.org/0000-0001-6870-5347
References
- 1. Newington L, Metcalfe A. Factors influencing recruitment to research: qualitative study of the experiences and perceptions of research teams. BMC Med Res Methodol 2014; 14: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tooher RL, Middleton PF, Crowther CA. A thematic analysis of factors influencing recruitment to maternal and perinatal trials. BMC Pregnancy Childbirth 2008; 8: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carter RE. Application of stochastic processes to participant recruitment in clinical trials. Control Clin Trials 2004; 25(5): 429–436. [DOI] [PubMed] [Google Scholar]
- 4. Page MJ, French SD, McKenzie JE, et al. Recruitment difficulties in a primary care cluster randomised trial: investigating factors contributing to general practitioners’ recruitment of patients. BMC Med Res Methodol 2011; 11: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pringle M, Churchill R. Randomised controlled trials in general practice. BMJ 1995; 311(7017): 1382–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McDonald AM, Knight RC, Campbell MK, et al. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006; 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Watson JM, Torgerson DJ. Increasing recruitment to randomised trials: a review of randomised controlled trials. BMC Med Res Methodol 2006; 6: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ngune I, Jiwa M, Dadich A, et al. Effective recruitment strategies in primary care research: a systematic review. Qual Prim Care 2012; 20(2): 115–123. [PubMed] [Google Scholar]
- 9. Fukui T, Rahman M, Shimbo T, et al. Recruitment of patients for a clinical trial: factors on the physician side and reasons on the patient side. Intern Med 2006; 45(8): 511–514. [DOI] [PubMed] [Google Scholar]
- 10. Foster JM, Sawyer SM, Smith L, et al. Barriers and facilitators to patient recruitment to a cluster randomized controlled trial in primary care: lessons for future trials. BMC Med Res Methodol 2015; 15: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ross S, Grant A, Counsell C, et al. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol 1999; 52(12): 1143–1156. [DOI] [PubMed] [Google Scholar]
- 12. Donovan JL, de Salis I, Toerien M, et al. The intellectual challenges and emotional consequences of equipoise contributed to the fragility of recruitment in six randomized controlled trials. J Clin Epidemiol 2014; 67(8): 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Foy R, Parry J, Duggan A, et al. How evidence based are recruitment strategies to randomized controlled trials in primary care? Experience from seven studies. Fam Pract 2003; 20(1): 83–92. [DOI] [PubMed] [Google Scholar]
- 14. Nederlandse Diabetes Federatie. NDF Zorgstandaard diabetes – Type 2 volwassenen, 2013, http://www.zorgstandaarddiabetes.nl/type-2/ (accessed 12 October 2017).
- 15. Garcia-Perez LE, Alvarez M, Dilla T, et al. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther 2013; 4(2): 175–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vluggen S, Hoving C, Schaper NC, et al. A web-based program to improve treatment adherence in patients with type 2 diabetes: development and study protocol. Contemp Clin Trials 2018; 74: 38–45. [DOI] [PubMed] [Google Scholar]
- 17. Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks, CA: SAGE, 1998. [Google Scholar]
- 18. Mortelmans D. Kwalitatieve analyse met Nvivo. Leuven; Den Haag: Acco, 2011. [Google Scholar]
- 19. Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval 2006; 27(2): 237–246. [Google Scholar]
- 20. Altman DG. Practical statistics for medical research. London: Chapman & Hall; CRC Press, 1991. [Google Scholar]
- 21. Sadler GR, Lantz JM, Fullerton JT, et al. Nurses’ unique roles in randomized clinical trials. J Prof Nurs 1999; 15(2): 106–115. [DOI] [PubMed] [Google Scholar]
- 22. Donovan JL, Peters TJ, Noble S, et al. Who can best recruit to randomized trials? Randomized trial comparing surgeons and nurses recruiting patients to a trial of treatments for localized prostate cancer (the ProtecT study). J Clin Epidemiol 2003; 56(7): 605–609. [DOI] [PubMed] [Google Scholar]
- 23. Mason V, Shaw A, Wiles N, et al. GPs’ experiences of primary care mental health research: a qualitative study of the barriers to recruitment. Fam Pract 2007; 24(5): 518–525. [DOI] [PubMed] [Google Scholar]
- 24. Donovan JL, Paramasivan S, de Salis I, et al. Clear obstacles and hidden challenges: understanding recruiter perspectives in six pragmatic randomised controlled trials. Trials 2014; 15: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50(2): 179–211. [Google Scholar]
- 26. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984; 11(1): 1–47. [DOI] [PubMed] [Google Scholar]
- 27. McAlister A, Perry C, Parcel G. How individuals, environments, and health behaviors interact: social cognitive theory. In: Glanz K, Rimer B, Viswanath K. (eds) Health behavior and health education. 4th ed. San Francisco, CA: Jossey-Bass, 2008, pp. 169–188. [Google Scholar]
- 28. Lawton J, Kirkham J, White D, et al. Uncovering the emotional aspects of working on a clinical trial: a qualitative study of the experiences and views of staff involved in a type 1 diabetes trial. Trials 2015; 16: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Townsend D, Mills N, Savovic J, et al. A systematic review of training programmes for recruiters to randomised controlled trials. Trials 2015; 16: 432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fletcher B, Gheorghe A, Moore D, et al. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2012; 2(1): e000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Spaar A, Frey M, Turk A, et al. Recruitment barriers in a randomized controlled trial from the physicians’ perspective: a postal survey. BMC Med Res Methodol 2009; 9: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dormandy E, Kavalier F, Logan J, et al. Maximising recruitment and retention of general practices in clinical trials: a case study. Br J Gen Pract 2008; 58(556): 759–766, i–ii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pearl A, Wright S, Gamble G, et al. Randomised trials in general practice: a New Zealand experience in recruitment. N Z Med J 2003; 116(1186): U681. [PubMed] [Google Scholar]
- 34. Sniehotta FF, Schwarzer R, Scholz U, et al. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol 2005; 35(4): 565–576. [Google Scholar]
- 35. Bell-Syer SE, Moffett JA. Recruiting patients to randomized trials in primary care: principles and case study. Fam Pract 2000; 17(2): 187–191. [DOI] [PubMed] [Google Scholar]
- 36. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983; 51(3): 390–395. [DOI] [PubMed] [Google Scholar]
- 37. Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health 2005; 20(2): 143–160. [Google Scholar]
- 38. De Vries H. An integrated approach for understanding health behavior; the I-Change Model as an example. Psychol Behav Sci Int J 2017; 2(2), https://juniperpublishers.com/pbsij/pdf/PBSIJ.MS.ID.555585.pdf [Google Scholar]
- 39. Sabaté E. Adherence to long-term therapies: evidence for action. Geneva: WHO, 2003. [PubMed] [Google Scholar]
- 40. Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychol 1999; 54(7): 493–503. [Google Scholar]
- 41. Bower P, Wallace P, Ward E, et al. Improving recruitment to health research in primary care. Fam Pract 2009; 26(5): 391–397. [DOI] [PubMed] [Google Scholar]