Hypertensive urgency is a subcategory of hypertensive crisis defined as an acute increase of systolic/diastolic blood pressure exceeding 180/120 mm Hg, without signs or symptoms of acute hypertensive target organ damage.1 When there is presence of end-organ damage associated with this acute and severe rise in blood pressure, this subcategory of hypertensive crisis is referred to as hypertensive emergency.1
Hypertensive urgency is a risk factor for cardiovascular disease, end-organ damage, and death when not identified and managed.2 The majority of hypertensive urgency cases are caused by nonadherence to antihypertensive medication.3 Studies reporting prevalence and outcomes of hypertensive urgency are limited and the majority of data are found in developed countries. In Africa, the estimated prevalence of hypertension in older adults ranges from 22.3% to 90.0%.4 The prevalence of hypertensive crisis in outpatient and emergency departments ranges from 2.5% to 5%.5,6 Of all cases of hypertensive crisis, hypertensive urgency ranges from 33% to 65% and hypertensive emergency accounts for about 68%.5,6
Although data are limited in low- and middle-income countries (LMICs), this interesting study by Reis et al.7 bridges the gap and provides insight into the reality that hypertensive urgency and its outcomes are a real burden in LMICs. Reis et al. conducted a study in Tanzania where they screened 7,600 participants at a local clinic and found that the prevalence of hypertensive crisis and hypertensive urgency were 2.6% and 2.2%, respectively.7 Among those with hypertensive crisis (199), hypertensive urgency accounted for 82%, which is much higher than may have been reported in Africa.5,6
Reis et al. followed 150 out of the 164 participants with hypertensive urgency for 1 year and found that poor adherence to antihypertensive medication was the strongest predictor of hospitalization and death. In Africa, especially in the sub-Saharan region, the prevalence of nonadherence (low plus moderate adherence) to antihypertensive medications can be as high as 99%.8 Some of the factors associated with poor adherence that may lead to adverse outcomes in LMICs include availability and cost of medications, use of traditional medicine believed to treat hypertension,9 poor access and availability of health systems, and poor levels of awareness and treatment (<10%) of hypertension.10 The work by Reis et al. highlights the need for interventions toward improved adherence to antihypertensive medication especially in patients with hypertensive urgency to avoid morbidity and mortality.
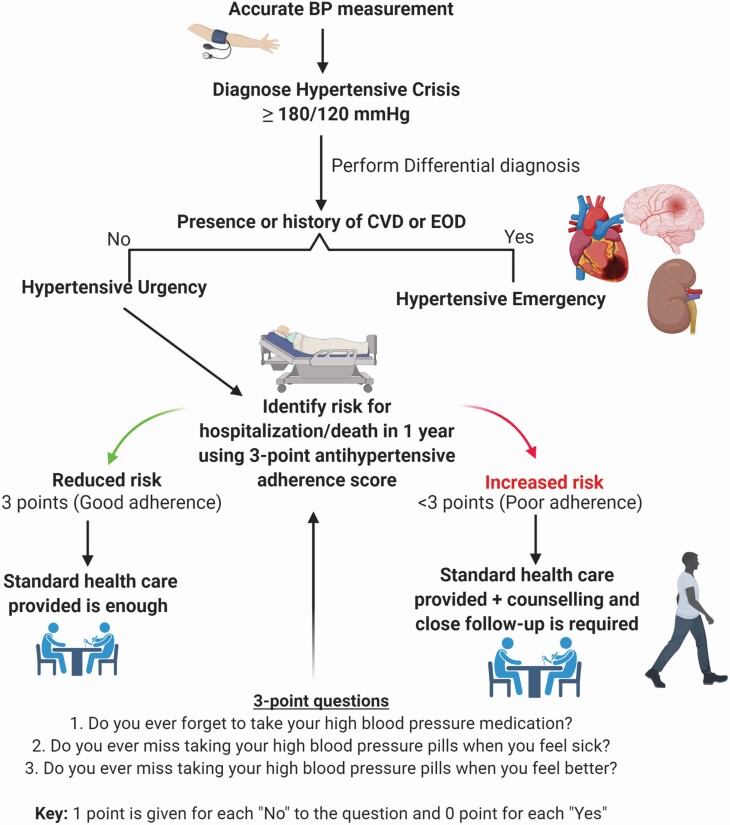
The study also demonstrates the feasibility and importance of using a simple self-reported medication adherence assessment tool to predict and identify high risk patients for hospitalization and death in 1 year. The adherence tool they used is a simple 3-question scale adopted from the Hill–Bone questionnaire.11 This tool was not only easy but also effective in identifying patients with hypertensive urgency who were at high risk of hospitalization and death. In Africa and western countries where public health institutions are usually faced with a high turnover of clients in the outpatient and emergency departments, the tool used by Reis et al. is potentially practical and efficient. We have, therefore, designed a summary algorithm to identify risk for future hospitalization and death following the data by Reis et al. (Figure 1) which can be used in the emergency and outpatient departments.
Figure 1.
Hypertensive urgency algorithm to identify risk for future hospitalization and death. Blood pressure (BP) was measured accurately to diagnose hypertensive crisis by having participants sit with their back supported and legs uncrossed with their feet flat on the floor for 5 minutes before the measurement. Hypertensive urgency was diagnosed based on absence of cardiovascular disease (CVD) and end-organ damage (EOD) in patients with hypertensive crisis. Using 3 adherence questions, they identified the risk for hospitalization and death. Participants with 3 points had reduced risk while those with <3 points had increased risk for hospitalization/death in 1 year. Additional close follow-up is highly recommended for patients with poor adherence (<3 points). Created with BioRender.com.
Indeed, the study by Reis et al. highlights the need for more studies and interventions in LMICs that are tailored toward mitigating the prevalence and incidence of hypertensive crisis. Though data may be lacking, hypertensive crisis, and hypertensive urgency are very common in LMICs.9,12 Data on physical activity, lifestyle, sociodemographic, and clinical outcomes associated with hypertensive urgency are warranted.
ACKNOWLEDGMENTS
We thank Professor Fernando Elijovich and Assistant Professor Dr Annet Kirabo for assisting with editing.
FUNDING
This work was supported by the Fogarty International Center of the National Institutes of Health grant D43 TW009337 and D43 TW009744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. van den Born BH, Lip GYH, Brguljan-Hitij J, Cremer A, Segura J, Morales E, Mahfoud F, Amraoui F, Persu A, Kahan T, Agabiti Rosei E, de Simone G, Gosse P, Williams B. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur Heart J Cardiovasc Pharmacother 2019; 5:37–46. [DOI] [PubMed] [Google Scholar]
- 2. Wani-Parekh P, Blanco-Garcia C, Mendez M, Mukherjee D. Guide of hypertensive crisis pharmacotherapy. Cardiovasc Hematol Disord Drug Targets 2017; 17:52–57. [DOI] [PubMed] [Google Scholar]
- 3. Paini A, Aggiusti C, Bertacchini F, Agabiti Rosei C, Maruelli G, Arnoldi C, Cappellini S, Muiesan ML, Salvetti M. Definitions and epidemiological aspects of hypertensive urgencies and emergencies. High Blood Press Cardiovasc Prev 2018; 25:241–244. [DOI] [PubMed] [Google Scholar]
- 4. Bosu WK, Reilly ST, Aheto JMK, Zucchelli E. Hypertension in older adults in Africa: a systematic review and meta-analysis. PLoS ONE 2019; 14:e0214934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shao PJ, Sawe HR, Murray BL, Mfinanga JA, Mwafongo V, Runyon MS. Profile of patients with hypertensive urgency and emergency presenting to an urban emergency department of a tertiary referral hospital in Tanzania. BMC Cardiovasc Disord 2018; 18:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nakalema I, Kaddumukasa M, Nakibuuka J, Okello E, Sajatovic M, Katabira E. Prevalence, patterns and factors associated with hypertensive crises in Mulago hospital emergency department; a cross-sectional study. Afr Health Sci 2019; 19:1757–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reis KG, Wilson R, Kalokola F, Wajanga B, Lee MH, Safford M, Peck RN. Hypertensive urgency in Tanzanian adults: a one-year prospective study. Am J Hypertens 2020; 33:1087–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Oluwole EO, Osibogun O, Adegoke O, Adejimi AA, Adewole AM, Osibogun A. Medication adherence and patient satisfaction among hypertensive patients attending outpatient clinic in Lagos University Teaching Hospital, Nigeria. Niger Postgrad Med J 2019; 26:129–137. [DOI] [PubMed] [Google Scholar]
- 9. Macquart de Terline D, Kane A, Kramoh KE, Ali Toure I, Mipinda JB, Diop IB, Nhavoto C, Balde DM, Ferreira B, Dèdonougbo Houenassi M, Ikama MS, Kingue S, Kouam Kouam C, Takombe JL, Limbole E, Mfeukeu Kuate L, N’guetta R, Damorou JM, Sesso Z, Sidy Ali A, Perier M-C, Azizi M, Empana JP, Jouven X, Antignac M. Factors associated with poor adherence to medication among hypertensive patients in twelve low and middle income Sub-Saharan countries. PLoS ONE 2019; 14:e0219266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nulu S, Aronow WS, Frishman WH. Hypertension in sub-Saharan Africa: a contextual view of patterns of disease, best management, and systems issues. Cardiol Rev 2016; 24:30–40. [DOI] [PubMed] [Google Scholar]
- 11. Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs 2000; 15:90–96. [DOI] [PubMed] [Google Scholar]
- 12. Mandi DG, Yaméogo RA, Sebgo C, Bamouni J, Naibé DT, Kologo KJ, Millogo GRC, Yaméogo NV, Thiam-Tall A, Samadoulougou AK, Zabsonré P. Hypertensive crises in sub-Saharan Africa: clinical profile and short-term outcome in the medical emergencies department of a national referral hospital in Burkina Faso. Ann Cardiol Angeiol (Paris) 2019; 68:269–274. [DOI] [PubMed] [Google Scholar]