Abstract
In the United States, colorectal cancer (CRC) is the second leading cause of mortality in men and women. We are now seeing an increasing number of patients with advanced-stage diagnosis and mortality from colorectal cancer before 50 years of age, which requires earlier screening. With the increasing need for CRC screening through colonoscopy, and thus endoscopists, easier and simpler techniques are needed to train proficient endoscopists. The most widely used approach by endoscopists is air insufflation colonoscopy, where air distends the colon to allow visualization of the colonic mucosa. This technique is un-comfortable for patients and requires an anesthetist to administer sedation. In addition, patients commonly complain about discomfort post-op as air escapes into the small bowel and cannot be adequately removed. Current research into the use of water insufflation colonoscopies has proved promising in reducing the need for sedation, decreasing discomfort, and increasing the visibility of the colonic mucosa. Future direction into water insufflation colonoscopies which have shown to be simpler and easier to teach may increase the number of proficient endoscopists in training to serve our aging population.
Keywords: Colorectal cancer, Water-insufflation colonoscopy, Air-insufflation colonoscopy, Adenomatous polyps, Adenoma detection rate
Core Tip: Training residents in water-insufflation colonoscopy techniques are simpler and easier to teach and lead to a reduction in patient pain, need for sedation, and increased visibility of the colonic mucosa. As more endoscopists are comfortable with this technique, more people in our growing population will be able to obtain the necessary screening colonoscopies.
INTRODUCTION
In the United States, colorectal cancer (CRC) is the second leading cause of mortality in men and women. The most effective tool for reducing the morbidity and mortality associated with CRC is the use of colonoscopy. With nearly 14.2 million procedures performed in the United States alone[1], the colonoscopy is one of the most common procedures performed. However, colonoscopies can only benefit the population with endoscopists who have proficiency in both technical and cognitive skills. The guidelines for training in colonoscopy techniques and grading proficiency continue to evolve as new advances in the tools used by endoscopists are discovered. In the 1960s, retrograde colonoscopy and endoscopic excision of polyps were developed in Japan to advance the visualization and removal of polyps from the entire large intestine[2]. Previous techniques such as the barium enema were challenging without considerable training and practice, and the presence of polypoid tumors could not be reliably excluded. As it was demonstrated that CRC did not occur de-novo but arose from a premalignant polyp, the use of the colonoscopy as a screening technique increased. Research into the use of the colonoscopy and the colonoscopy polypectomy proved that the detection of cancer at an earlier, pre-symptomatic stage was associated with better survival[3].
For a successful screening colonoscopy, partial distention of the lumen is needed to allow proper visualization and inspection of the colonic mucosa. The current standard technique for colonic distention is the use of air insufflation (AI) using an integrated air pump[4,5]. However, one of the major sources of pain and discomfort for patients undergoing a colonoscopy is the volume of air insufflated which causes significant abdominal distention and looping of the instrument. Potential risks for this procedure include perforation, bleeding, and infection. To minimize discomfort and pain during the procedure, patients undergoing colonoscopy with AI often require sedation which adds additional risks including medication side effects, higher medical costs, and longer recovery time when compared with unsedated colonoscopy[6]. At the end of the procedure, the air can only be partially removed, as some of it escapes into the small bowel. This leads to post-procedure cramping, gas, and bloating which can only be relieved by passing gas.
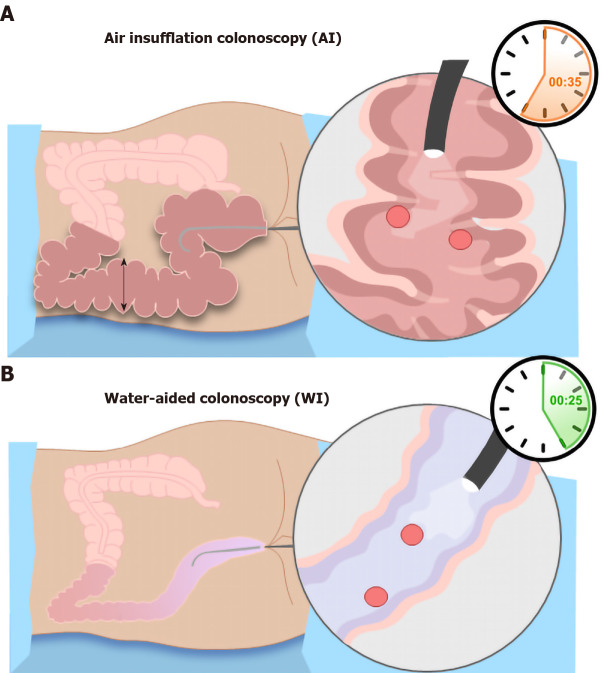
Recent clinical trials have proposed that using water infusion to distend the colon may reduce patient pain and discomfort and improve colonic visualization through difficult segments of the colon. This was first described by Falchuk and Griffin in 1984 in patients who could not undergo AI due to severe diverticular disease[7]. For water infusion colonoscopy, instead of expanding the colon, the water weighs it down utilizing gravity. It was Japanese endoscopists who evolved this technique by using syringes for water infusion and complete air suction to “collapse” the colonic lumen and continuously infusing water to advance the colonoscope[8]. This method straightens the colon and allows for better navigation of the scope through less extreme angles. As no air is left behind, this technique reduces post-procedure pain and allows for faster recovery. The first randomized control trial in 2010 showed that using the water immersion technique compared to standard AI increases the success rate of minimal sedation colonoscopy[9]. This along with other studies has shown the use of water improves the rate and time of cecal intubation, alleviates abdominal pain, and increases patients’ willingness to undergo a repeat procedure[7]. This technique is shown in Figure 1.
Figure 1.
Image of colonic distension and bowel looping in air insufflation colonoscopy vs water-aided colonoscopy. A: Air insufflation colonoscopy causes significant distention of the colon in both length and width. The air promotes looping of the bowl at the flexure points leading to difficult navigation of the colonoscope; B: Water insufflation utilizes gravity to pull the colon down while providing minimal distention and looping. AI: Air insufflation; WI: Water insufflation.
The overall effectiveness of colonoscopy is the achievement of various quality measurements. The most important quality measurement is the adenoma detection rate (ADR) which is the frequency with which adenomas are detected in asym-ptomatic, average-risk individuals in a screening colonoscopy[10]. Another quality measurement is cecal intubation or the ability to pass the colonoscope through the tip of the ileocecal valve. This ensures adequate visualization of the entire colonic mucosa. Bowel preparation is an important measure as its effectiveness rests in the hands of the patient. Without adequate bowel preparation, clear visualization of the colon is difficult and may require repeat procedures. Sedation and the use of an anesthetist decrease intra-op and post-op pain, yet it is associated with increased cost.
New advances in colonoscopy have led to the development of virtual colonoscopy and robotic colonoscopy. Virtual colonoscopies, or computed tomography colo-nography (CTC), use helical CT scanners and AI to take 3D images of the colon. This technique is non-invasive, requires no sedation, can be completed in 10-15 min, and is overall much safer[11]. However, there are some limitations to this approach. Incomplete distention of colonic segments and flat lesions can lead to false-negative diagnoses. In addition, CTC does not allow for removal or biopsy of lesions. Robotic colonoscopy has benefits over the traditional endoscope approach including better viewing of the gastrointestinal tract, decreased pain, and the ability to navigate tortuous colons successfully. Multiple models of robotic instruments are currently being studied including robotic capsules and robotically controlled advanced colonoscopies. These new advances and the ease with which they can be used may aid in the training of future endoscopists. New research shows that training residents in water insufflation colonoscopic technique leads to increased patient comfort and decreased complications with comparable success rates[12]. As the number of people needing screening colonoscopies continues to grow, so will the need for competent endoscopists and successful endoscopic techniques.
ADR
ADR is the proportion of screening colonoscopies that detect at least one adenoma[13]. The goal of endoscopic screening is checking for CRC, so detection of adenoma in the large bowel can limit the advancement to larger adenomas. The recommended ADR is 20%, based on studies that showed adenoma prevalence in asymptomatic adults to be between 25% to 40%[14,15]. In a study with over 10000 patients, the overall ADR (95% confidence interval) for water insufflation was 34.4% and 30.2% for AI[16]. ADRs are inversely correlated with interval cancers which makes them an important measure in colonoscopies. Interval cancers, or post-colonoscopy CRCs, are cancers detected within the surveillance interval, or 6-36 mo post-cleared colonoscopy. The incidence of interval cancers is 3.4%-9.2%, and improving ADR and colonoscopy techniques can decrease this number substantially[17].
CECAL INTUBATION
Cecal intubation is successfully achieved when the tip of the colonoscope is passed through the ileocecal valve into the caput. This allows for a complete examination of the colonic mucosa at the medial wall of the cecum. AI distends the length of the colon, often farther than the length of the colonoscope. This attributes to the difficulty of adequate cecal intubation with AIC. Gravity allows water infusion into the sigmoid colon to open a passage through the loops and bends of the colon. In addition, abdominal compression and proper positioning of the patient facilitates the passage of the colonoscope and enhances cecal intubation. Some studies have reported that warm water insulation reduces colonic spasms which may also contribute to a higher cecal intubation rate. Some studies have shown that WIC improved cecal intubation time compared with AIC[7,18]. Increasing cecal intubation time can decrease the total OR time and thus, decrease the overall cost.
BOWEL PREP QUALITY
In order to optimize the effectiveness of colonoscopy as a screening tool, patients need to accept the procedure and the necessity of adequate bowel preparation[19]. Preparation quality affects the mucosal visualization, the ability to complete the exam, and the procedure duration. Only three-quarters of colonoscopies have adequate colon preparation[20]. Poor bowel prep can lead to lower ADRs and may force patients to undergo follow-up colonoscopies sooner. In water insufflation (WI), the suction of dirty water and infusion of clean water in the colonic lumen provides serendipitously salvage bowel cleaning in patients with suboptimal bowel preparation[21]. Ineffective bowel preparation may lead to cancelations or rescheduling procedures, which is a major contributor to costs[22].
SEDATION
Sedation for colonoscopy procedure increases the cost and post-procedure recovery time for patients. Patients who have more challenging anatomy often require more sedation as they experience more pain. Studies have shown that water exchange has minimized the requirement for sedation compared with AI. In one study, only 11.5% of patients required on-demand sedation with water exchange compared with 26% in the AI group[23]. Another benefit of limiting sedation is to decrease the risk of cardiopulmonary complications associated with anesthesia. In a study that used the Clinical Outcomes Research Initiative database, cardiopulmonary complications occurred in 0.9% of procedures and made up 67% of unplanned events in endoscopic procedures with sedation[24]. Patients with increased risk of CVP complications include those with advanced age and presence of comorbidities. These patients could benefit greatly from water insufflation colonoscopy, which requires little if any, pain management.
LIMITING PRE AND POST-PROCEDURE PAIN
Intraoperatively, AI causes more pain during colonoscopy as it elongates and distends the colon. Post-operatively, patients experience discomfort as the gas escapes the colon into the small bowel and leads to abdominal distention. Water insufflation reduces intraoperative pain by weighing down and straightening the sigmoid and decreasing colonic spasm[25]. Fewer patients require sedation with water insufflation compared with AI[26]. Several studies revealed that WIC significantly increased the number of patients who were willing to undergo another colonoscopy due to limited pain during the procedure; this was found to be significantly higher in WIC than in AIC[18,27,28]. With AI, undesired outcomes including perforation and bleeding are partly due to increased colonic distention, angulations exaggeration at flexures, and the increased looping of the instrument. The current rate of perforation is low, ranging from 0.08% to 0.3% in various studies[29]. Pain during colonoscopy indicates the risk of perforation, but sedation can mask this important warning[30]. WI colonoscopy minimizes colonic distention, improves visibility, and reduces the need for sedation, thus reducing the risk of perforation.
TEACHING ENDOSCOPY TECHNIQUES IN TRAINING PROGRAMS
There are multiple different methods currently used for colonoscopy training, including mechanical simulators, virtual reality simulators, computer-simulating endoscopy, magnetic endoscopic imaging, and composite and explanted animal organ simulators. One of the main factors that leads to a lack of polyp discovery is the inexperience of the endoscopist[30,31]. However, there have been some limitations to colonoscopy instruction, including time management and potential trauma to patients involved. Endoscopists in training may benefit from learning the water insufflation technique, as the scope becomes easier to navigate through a minimally looped colon. In addition, detorsion becomes easier for trainees with water insufflation as there is a decreased risk of perforation from AI. Studies have shown that WIC has significantly shorter cecal intubation time for endoscopists in training compared with AIC[7]. The increasing need for colonoscopy screening has increased the demand for high-quality training. Stimulation models are a key tool that many programs use to ease the learning curve of colonoscopy techniques. Another tool that should be introduced into training programs is the use of water insufflation colonoscopy. Trainees may benefit from training with the water insufflation technique as there is the ease of insertion, reduced cecal intubation time, more comfort for the patient, and less looping of the bowel[12]. The strengths and weaknesses of these two techniques are shown in Table 1.
Table 1.
Strengths and weaknesses of air insufflation vs water insufflation
|
AI: Strengths
|
AI: Weaknesses
|
WI: Strengths
|
WI: Weaknesses
|
| Distended bowel allows for better visualization | Increased pain on insertion | Increased ADR | Decreased visualization through fluid |
| More widely accepted | Increased postoperative pain | Decreased looping of bowel | Longer insertion time |
| Current teaching method | Increased sedation requirement | Decreased sedation requirement | Not widely accepted or utilized |
| Current patient preference | Increased risk of perforation | Increased cecal intubation rate |
AI: Air insufflation; WI: Water insufflation; ADR: Adenoma detection rate.
CONCLUSION
Colorectal cancer is the second leading cause of mortality in men and women in the United States. Since the onset of screening colonoscopies, the conventional colo-noscope has not changed much since its development. Many colonoscopy practices use deep sedation to provide comfort for the patients, which adds to the overall cost of the procedure. There is still a lack of widespread acceptance of the use of colonoscopies (vs other non-invasive screening techniques), as up to 75% of patients diagnosed with colon cancer present with locally advanced disease[32]. In addition, 1 in 10 patients has developed interval cancers after clear colonoscopies. Beyond the water insufflation technique, there have been new advances in the use of robotic endoscopic techniques for screening colonoscopies. These devices can give a more in-depth view of the gastrointestinal tract, decrease pain associated with endoscopy, and perform well in more challenging colons[33]. Future directions should aim at getting a true 360-degree view of the colon with minimal pain, sedation, and total procedure time. In addition, colonoscopy practices should be geared toward practices that can be safely done during the COVID pandemic without the risk of aerosolizing viral particles.
Footnotes
Conflict-of-interest statement: Chelsea V Hayman and Dinesh Vyas have nothing to disclose.
Manuscript source: Unsolicited manuscript
Peer-review started: October 16, 2020
First decision: October 27, 2020
Article in press: December 11, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mizukami T S-Editor: Liu M L-Editor: A P-Editor: Ma YJ
Contributor Information
Chelsea V Hayman, College of Medicine, California Northstate University, Elk Grove, CA 95757, United States.
Dinesh Vyas, College of Medicine, California Northstate University, Elk Grove, CA 95757, United States. dineshvyas@yahoo.com; Department of Surgery, San Joaquin General Hospital, French Camp, CA 95231, United States.
References
- 1.Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS, Dong FB, Winges LD, McKenna MT. How many endoscopies are performed for colorectal cancer screening? Gastroenterology. 2004;127:1670–1677. doi: 10.1053/j.gastro.2004.09.051. [DOI] [PubMed] [Google Scholar]
- 2.Wolff WI. Colonoscopy: history and development. Am J Gastroenterol. 1989;84:1017–1025. [PubMed] [Google Scholar]
- 3.Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer. 1975;36:2251–2270. doi: 10.1002/cncr.2820360944. [DOI] [PubMed] [Google Scholar]
- 4.Phaosawasdi K, Cooley W, Wheeler J, Rice P. Carbon dioxide-insufflated colonoscopy: an ignored superior technique. Gastrointest Endosc. 1986;32:330–333. doi: 10.1016/s0016-5107(86)71877-4. [DOI] [PubMed] [Google Scholar]
- 5.Janssens F, Deviere J, Eisendrath P, Dumonceau JM. Carbon dioxide for gut distension during digestive endoscopy: technique and practice survey. World J Gastroenterol. 2009;15:1475–1479. doi: 10.3748/wjg.15.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stock C, Ihle P, Sieg A, Schubert I, Hoffmeister M, Brenner H. Adverse events requiring hospitalization within 30 days after outpatient screening and nonscreening colonoscopies. Gastrointest Endosc. 2013;77:419–429. doi: 10.1016/j.gie.2012.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Hafner S, Zolk K, Radaelli F, Otte J, Rabenstein T, Zolk O. Water infusion vs air insufflation for colonoscopy. Cochrane Database Syst Rev. 2015;26:CD009863. doi: 10.1002/14651858.CD009863.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mizukami T, Yokoyama A, Imaeda H, Kumai K. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Digest Endosc . 2007;19:43–48. [Google Scholar]
- 9.Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Water immersion vs standard colonoscopy insertion technique: randomized trial shows promise for minimal sedation. Endoscopy. 2010;42:557–563. doi: 10.1055/s-0029-1244231. [DOI] [PubMed] [Google Scholar]
- 10.Rex DK, Schoenfeld PS, Cohen J, Pike IM, Adler DG, Fennerty MB, Lieb JG 2nd, Park WG, Rizk MK, Sawhney MS, Shaheen NJ, Wani S, Weinberg DS. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81:31–53. doi: 10.1016/j.gie.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 11.Heiken JP, Peterson CM, Menias CO. Virtual colonoscopy for colorectal cancer screening: current status. Cancer Imaging. 2005;5 Spec No A:S133–S139. doi: 10.1102/1470-7330.2005.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vyas D, Chang J, Goyal M, Obad N, Ramdass P, Sodavarapu S. Training surgery residents in underwater colonoscopies is more effective than training them in air-insufflation colonoscopies. medRxiv . 2020:Epub ahead of print. [Google Scholar]
- 13.Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD, Church J, Marshall JB, Riddell RH U. S. Multi-Society Task Force on Colorectal Cancer. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 15.Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000;343:169–174. doi: 10.1056/NEJM200007203430302. [DOI] [PubMed] [Google Scholar]
- 16.Fuccio L, Frazzoni L, Hassan C, La Marca M, Paci V, Smania V, De Bortoli N, Bazzoli F, Repici A, Rex D, Cadoni S. Water exchange colonoscopy increases adenoma detection rate: a systematic review with network meta-analysis of randomized controlled studies. Gastrointest Endosc 2018; 88: 589-597. :e11. doi: 10.1016/j.gie.2018.06.028. [DOI] [PubMed] [Google Scholar]
- 17.Jang HJ. Training in Endoscopy: Colonoscopy. Clin Endosc. 2017;50:322–327. doi: 10.5946/ce.2017.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, Aharonian HS, Guth PH, Mann SK, Leung JW. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 19.McLachlan SA, Clements A, Austoker J. Patients' experiences and reported barriers to colonoscopy in the screening context--a systematic review of the literature. Patient Educ Couns. 2012;86:137–146. doi: 10.1016/j.pec.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003;58:76–79. doi: 10.1067/mge.2003.294. [DOI] [PubMed] [Google Scholar]
- 21.Ramirez FC, Leung FW. A head-to-head comparison of the water vs. air method in patients undergoing screening colonoscopy. J Interv Gastroenterol. 2011;1:130–135. doi: 10.4161/jig.1.3.18512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rex DK, Imperiale TF, Latinovich DR, Bratcher LL. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol. 2002;97:1696–1700. doi: 10.1111/j.1572-0241.2002.05827.x. [DOI] [PubMed] [Google Scholar]
- 23.Cadoni S, Gallittu P, Sanna S, Fanari V, Porcedda ML, Erriu M, Leung FW. A two-center randomized controlled trial of water-aided colonoscopy vs air insufflation colonoscopy. Endoscopy. 2014;46:212–218. doi: 10.1055/s-0033-1353604. [DOI] [PubMed] [Google Scholar]
- 24.Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66:27–34. doi: 10.1016/j.gie.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 25.Rapelli S, Montorfano G, Gornati R, Berra B. Tissue and serum gangliosides determination in patients with meningiomas. Ital J Biochem. 1989;38:289A–291A. [PubMed] [Google Scholar]
- 26.Chaubal A, Pandey V, Patel R, Poddar P, Phadke A, Ingle M, Sawant P. Difficult colonoscopy: air, carbon dioxide, or water insufflation? Intest Res. 2018;16:299–305. doi: 10.5217/ir.2018.16.2.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ransibrahmanakul K, Leung J, Mann S Siao-Salera R; Lim B; Hasyagar C; Yen D; Nastaskin I; Leung F. Water Infusion in Lieu of Air Insufflation (Water Method) Diminished Discomfort in Patients Undergoing Minimal Sedation Colonoscopy in the Hands of Supervised Trainees. Am J Gastroenterol . 2009;104:S509–S510. [Google Scholar]
- 28.Hsieh YH, Lin HJ, Tseng KC. Limited water infusion decreases pain during minimally sedated colonoscopy. World J Gastroenterol. 2011;17:2236–2240. doi: 10.3748/wjg.v17.i17.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ASGE Standards of Practice Committee, Fisher DA, Maple JT, Ben-Menachem T, Cash BD, Decker GA, Early DS, Evans JA, Fanelli RD, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Malpas PM, Sharaf RN, Shergill AK, Dominitz JA. Complications of colonoscopy. Gastrointest Endosc. 2011;74:745–752. doi: 10.1016/j.gie.2011.07.025. [DOI] [PubMed] [Google Scholar]
- 30.Leung FW, Aljebreen AM, Brocchi E, Chang EB, Liao WC, Mizukami T, Schapiro M, Triantafyllou K. Sedation-risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc. 2010;2:81–89. doi: 10.4253/wjge.v2.i3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Papanikolaou IS, Karatzas PS, Varytimiadis LT, Tsigaridas A, Galanopoulos M, Viazis N, Karamanolis DG. Effective colonoscopy training techniques: strategies to improve patient outcomes. Adv Med Educ Pract. 2016;7:201–210. doi: 10.2147/AMEP.S99617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnston PG. The Colorectal Cancer Coalition: reflections on the future. Oncologist. 2006;11:970–972. doi: 10.1634/theoncologist.11-9-970. [DOI] [PubMed] [Google Scholar]
- 33.Cater D, Vyas A, Vyas D. Robotics in Colonoscopy. Am J Robot Surg. 2014;1:48–54. doi: 10.1166/ajrs.2014.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]