Abstract
Aim:
The aim of this meta analysis was to evaluate the influence of the processing method on the marginal and internal gaps of lithium disilicate inlays/onlays.
Settings and Design:
A systematic literature review was conducted using the PubMed/Medline, Embase, Scopus, and Cochrane Library databases. This review was registered on the PROSPERO platform.
Materials and Methods:
The studies were selected according to the marginal and internal gaps of two different fabrication methods for lithium disilicate (milled and pressed).
Statistical Analysis Used:
The meta analysis was performed based on the Mantel–Haenszel and inverse variance methods, using the random effects model and a 95% confidence interval.
Results:
From all databases, 127 studies were identified. Four in vitro studies were included in the qualitative analysis and three in the meta analysis. Moreover, 197 restorations were evaluated (103 pressed and 94 milled). During the evaluation of only the internal gap, there was a statistically significant difference favoring the pressed technique (P = 0.002). There was no statistically significant difference in the analyses of the marginal gap (P = 0.530) and the total gap (P = 0.450).
Conclusion:
Both the techniques provided acceptable marginal and total gaps, although the pressed technique revealed a more favorable internal adaptation than the milled onlays/inlays.
Keywords: Computer-aided design/computer-assisted manufacturing, ceramics, dental materials, laboratory technology
INTRODUCTION
Lithium disilicate glass–ceramics have been widely used in dental practice due to their appropriate performance as a restorative material.[1,2,3] Lithium disilicate is nonmetallic inorganic ceramic material, synthetic, with a crystalline phase.[1,3] The composition includes silicon dioxide–lithium oxide (SiO2-Li2O) glass-ceramics, aluminum oxide (Al2O3), and potassium oxide (K2O) used to improve the chemical durability and phosphorous pentoxide (P2O5) and zirconium dioxide (ZrO2) that promote crystallization process.[1,3,4] The amount (% by weight) of these components is responsible for optical and mechanical properties.[3,4] The evolution of lithium disilicate provided their production of different modalities, such as heat-press or computer-aided design/computer-assisted manufacturing (CAD/CAM) manufacturing.[4] These characteristics provide an excellent chemical durability, high strength, and capacity to mimic the natural teeth' optical characteristics to lithium disilicate,[1,2,4] increasing the application in all-ceramic restorations such as veneers, inlays, onlays, anterior and posterior single crowns and multiple-unit bridges.[3]
Lithium disilicate restorations are sensitive to the processing method.[2,4,5] Therefore, the same material with the similar chemistry and microstructure may influence the final properties and clinical success, depending on the processing methodology used to produce the restoration.[4] The CAD/CAM technology came with the proposal to produce restorations with greater accuracy in a fast and reproducible way.[2,6] However, they can also cause damage to the prosthesis through the milling process.[6]
Marginal quality of the restoration is another parameter that has an influence on the clinical success and can be affected by various factors that influence directly the strength of the restoration and its life expectancy.[2,3,4,7] Discrepancy of marginal fit and internal gap in the restoration may lead to the dissolution of the luting resin facilitation, the bacterial infiltration, and altering the composition of the subgingival microflora.[6,8,9,10] In addition, these areas may weaken the restoration due to the higher concentration of stress in this region without support, leading to fracture.[11]
Although many studies have been aimed to analyze the clinical performance of lithium disilicate glass–ceramics in relation to single crowns or fixed dental prostheses and compared to other types of ceramics material, there are few researches about minimally invasive restorations. The aim of this systematic review with meta-analysis was to evaluate the influence of the processing method on the marginal and internal gap of lithium disilicate inlays/onlays. The null hypothesis was that the processing method has no difference in the marginal and internal adaption of lithium disilicate inlays or onlays.
MATERIALS AND METHODS
Research strategy and information sources
This systematic review was organized in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses criteria described by Moher et al.[12] In addition, this review was registered in the PROSPERO platform (CRD42018094020).
Criteria for selection of studies
Potentially eligible studies were selected according to the inclusion and exclusion criteria previously determined by reading summaries and complete texts. The examiners came to a consensus in any disagreement, and when necessary, a third examiner was requested.
Search strategy
The searches were performed in the PubMed/Medline, Embase, Scopus, and Cochrane Library databases by two reviewers, with the following keyword combinations: “Lithium disilicate AND cad-cam AND onlay OR Lithium disilicate AND cad-cam AND inlay OR Lithium disilicate AND heat-press AND onlay OR Lithium disilicate AND heat-press AND inlay.” The authors were contacted via e-mail when the complete content of the article could not be accessed. The inter-examiner (kappa) tests were performed by the selected titles and abstracts, obtaining a concordance test value of 100% (kappa = 1).
Inclusion/exclusion criteria
The inclusion criteria were retrospective, prospective, controlled, and randomized clinical studies and in vitro studies, published in English, that compared the fabrication methods of inlay/onlay in lithium disilicate (pressed and CAD/CAM). The exclusion criteria included duplicate studies, theoretical studies, duplicate data studies (previously published), systematic reviews, and a study that did not compare the two ceramic processing techniques in lithium disilicate.
Study selection and reliability of quality assessment
The studies were selected and read completely in accordance with the inclusion and exclusion criteria. The PICO criteria established by Moher et al.[12] were followed to answer the following question: “What is the best method for manufacturing lithium disilicate inlay/onlay in relation to marginal and internal adaptation?” An evaluation was performed between inlay/onlay manufactured (P) with lithium disilicate comparing (I) different ceramic processing techniques (C) for marginal and internal gaps. The primary outcome was to evaluate (O) the ceramic processing method influenced the marginal and internal gaps of lithium disilicate inlay/onlay.
Data analysis
The following data were collected from the eligible studies: main author and year of study publication, CAD/CAM System, manufacturer, type of tooth, type of preparation, marginal gap (MG) and internal adaptation evaluation, number of restorations for each processing method, groups studied, the results of the marginal and internal gaps of the different processes, and outcomes [Table 1].
Table 1.
Demographic data of all studies included
| Author, year, type of study | CAD/CAM system | Manufacturer | Type of tooth | Type of preparation | Marginal gap and internal adaptation evaluation | Number of restorations | Groups | Outcomes | Marginal gap (µm) | Internal fit (µm) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PT | MT | MT | PT | MT | PT | ||||||||
| Guess et al., 2014 - in vitro | CEREC | IPS e.max CAD (MT), IPS e.max Press (PT) | Human molar | Onlay | The replica technique, stereo microscope, and a 3 CCD-colour videocamera | 48 | 24 | Group IP: PT (IPS e.max Press) Group VP: PT (Vita-PM9) Group IC: MT (e.max CAD) |
The pressed technique resulted in significantly better internal fit values compared to the CAD/CAM technique | Before cementation 50.09 After cementation 54.05 |
Before Cementation Group IP: 45.41 Group VP: 35.30 After cementation Group IP: 62.86 Group VP: 48.55 |
103.37 | Group IP: 66.9 Group VP: 58.31 |
| Alajaji et al., 2017 - in vitro | Tizian Cut 5 | IPS e.max CAD (MT), IPS e.max Press (PT) | Acrylic tooth | MOD inlay | Micro-CT system | 15 | 30 | Group 1: MT (three-axis) Group 2: MT (five-axis) Group 3: PT |
The mean marginal gap in the pressed group was significantly lower than the mean in the other groups. However, in every group, 100% of the samples were within the clinically acceptable marginal gap limit of 100 µ |
Group 1: 67.67 (14.04) Group 2: 56.19 (12.32) |
Group 3: 35.48 (8.12) | Internal gap Group 1: 176.99 (33.39) Group 2: 160.89 (21.22) Occlusal internal gap Group 1: 210.42 (60.59) Group 2: 216.81 (34.34) Axial internal gap Group 1: 143.56 (12.44) Group 2: 104.98 (14.05) |
Internal gap 75.95 (16.09) Occlusal internal gap 99.90 (23.69) Axial internal gap 52.64 (15.7) |
| Vanlıoglu et al., 2012 - in vitro | NR | IPS e.max CAD (MT), IPS e.max Press (PT)) | Human molar | MODL onlay | Silicone replica technique and light microscope | 20 | 20 | Group 1: PT Group 2: MT |
Both systems demonstrated acceptable marginal discrepancies | Marginal dentin 119.65 (27.80) Marginal enamel 112.14 (15.64) |
Marginal dentin 119.28 (25.76) Marginal enamel 99.08 (16.34) |
Internal marginal dentin 152.83 (39.82) Internal marginal enamel 174.52 (36.56) Axial 132.77 (31.32) Occlusal 196.49 (38.16) |
Internal marginal dentin 118.76 (37.88) Internal marginal enamel 119.74 (32.49) Axial 96.53 (21.54) Occlusal 134.55 (39.27) |
| Sener-Yamaner et al., 2017 - in vitro | CEREC | IPS e.max CAD (MT), IPS e.max Press (PT) | Human molar | MOD inlay | Optical microscope | 20 | 20 | Group CDL: MT Group HDL: PT |
Inlays made of milled lithium disilicate ceramic showed the lowest marginal gap values and the lowest cement thickness after cementation compared to other materials tested | Before cementation 65 (22.4) After cementation 82.6 (24.6) |
Before cementation 88.84 (15.37) After cementation 108.37 (21.25) |
NR | NR |
MT: Milled technique, PT: Pressed technique, NR: Not reported, CAD: Computer-aided design, CAM: Computer-assisted manufacturing, MOD: Mesio-occlusal-distal, MODL: Mesio-occusal-distal-lingual
Data inclusion
Data recording allowed a qualitative and quantitative comparison between the selected studies (n = 4).
Meta-analysis
The meta-analysis was based on the Mantel–Haenszel (MH) and inverse variance methods. The continuous outcome (marginal, internal, and total gap) was evaluated by mean difference (MD) and risk ratio (RR) and the corresponding 95% confidence intervals (CIs). The MD values were considered significant when P < 0.05 [Table 2]. The software Review Manager 5 (Cochrane Group) was used for meta-analysis. The heterogeneity statistic I2 was used to verify the heterogeneity by proportion, where I2 values close to 0% indicate no heterogeneity between the studies, values close to 25% represent small, 50% represent moderate, and close to 75% have been interpreted as a high level of heterogeneity.[13]
Table 2.
Mean values of total, marginal and internal gap used to perform the meta-analysis
| Author, year, type of study | Total gap (mean) | Marginal (mean) | Internal (mean) | |||
|---|---|---|---|---|---|---|
| MT | PT | MT | PT | MT | PT | |
| Alajaji et al., 2017 - in vitro | 115.43 (21.26) | 55.82 (13.3) | 61.93 (13.18) | 35.48 (8.12) | 168.94 (29.34) | 76.17 (18.49) |
| Vanlıoglu et al., 2012 - in vitro | 140.02 (29.09) | 113.28 (26.92) | 115.89 (21.72) | 109.18 (21.05) | 164.15 (36.46) | 117.39 (32.79) |
| Sener-Yamaner et al., 2017 - in vitro | 73.8 (23.5) | 98.6 (18.31) | 73.8 (23.5) | 98.6 (18.31) | NR | NR |
MT: Milled technique, PT: Press technique, NR: Not reported
RESULTS
The previous search on determined databases found a total of 127 studies. After the removal of duplicates, 88 records remained, being read all titles and abstracts. Six studies were selected according to the inclusion/exclusion criteria. No article was added from the manual searches.
Readings of the complete content of six articles were performed after the application of the inclusion and exclusion criteria. Four studies were selected for the inclusion of qualitative data[14,15,16,17] and three studies were included in quantitative analysis (meta-analysis).[14,16,17] Two studies were excluded because they did not compare the two manufacturing techniques or/and MG.[8,18] The data of the four studies included in this systematic review are given in Table 1. The search strategy details are illustrated in Figure 1.
Figure 1.
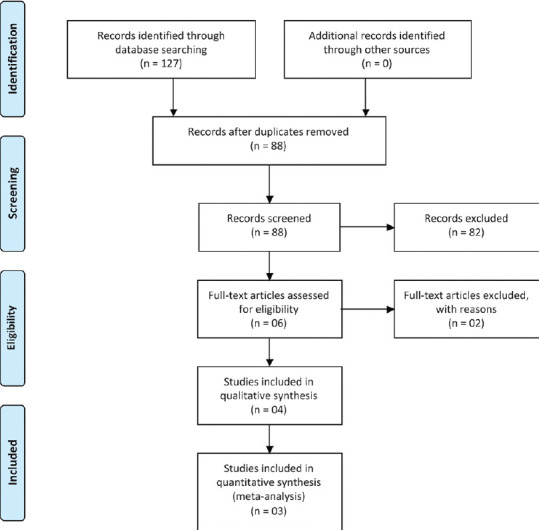
Search strategy according to the PRISMA statement
Demographic data
Of the four studies, all were in vitro studies, which created a total of 197 specimens. A “n” minimum of 40 specimens[16,17] and a “n” maximum of 72 specimens[15] were observed. Only IPS e.max CAD and IPS e.max Press (Ivoclar Vivadent) were used for specimen manufacturing.
The type of tooth of the specimens varied according to the tests performed for each study. Three studies manufactured specimens and tested on extracted human molars[15,16,17] and one tested on acrylic maxillary left first premolar tooth.[14]
Marginal and internal gap analyses
Four outcomes could be observed by studying the articles included, two of them found the MG measures clinically acceptable. However, one article[15] stated that press fabricated onlays had internal fit values significantly better than the CAD/CAM technique. On the other hand, findings by Sener-Yamaner et al.[16] indicated that inlays made by CAD/CAM technique showed lower MG and cement thickness values than the press fabricated specimens. However, Vanlıog lu et al.[17] and Alajaji et al.[14] showed that both the systems demonstrated acceptable, marginal discrepancies.
Meta-analysis
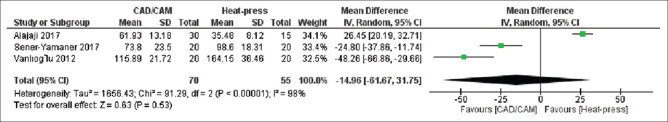
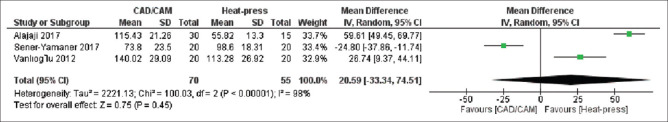
In the meta-analysis performed, when only the internal gap [Figure 2] was evaluated, there was a statistically significant difference with a favorable trend in the press technique (DM = 70.51, 95% CI: 25.45–115.58, P = 0.002). For the analysis of MG (DM = −14.96, 95% CI: −61.67–31.75, P = 0.53) [Figure 3] and total gap (DM = 20.59, 95% CI: −33, 34–74.51, P = 0.45) [Figure 4], there was no statistically significant difference in both the analyzes.
Figure 2.
Forest plot of the internal gap results
Figure 3.
Forest plot of marginal gap results
Figure 4.
Forest plot of total gap results
DISCUSSION
The minimally invasive approach allowed the use of partial-coverage adhesive ceramic restorations as an alternative to the traditional total crown on weakened or missing tooth structure.[19] To enhance the ceramic material production, various types of processing are introduced into the dental market, including the heat-press technique as well as the laboratory-side and chairside CAD/CAM systems.[20] However, the adhesive interface between the tooth/all-ceramic material is still a susceptible factor for aging processes,[15,21] which determine the clinical long-term success of bonded restorations[22] and which can be increased by the MG. The null hypothesis formulated in this study was rejected for the internal gap and accepted for MG since the press processing technique showed more favorable internal adaptation when compared to the CAD-CAM.
A successful dental restoration should conform to the following criteria: marginal adaptation, biocompatibility, esthetics, and mechanical strength.[23] Among these, the presence of MG can increase plaque accumulation and contribute to a higher risk of caries lesions.[24] In addition, higher MG values reduce the fracture strength of the crown and the veneering porcelain.[25,26] Among the variety of dental ceramics, lithium disilicate has been widely used in indirect restorations[27] because it has more favorable mechanical properties compared with conventional dental porcelains, high strength, high fracture toughness,[28] and has excellent optical properties.[29] Therefore, the studies included in this systematic review[14,15,16,17] evaluate the behavior of this ceramic material.
A recent study[30] evaluated the marginal fit of lithium disilicate crowns made either by CAD/CAM or heat-press technique. The study reported that crowns manufactured by the press technique have significantly smaller MG compared with those manufactured by CAD/CAM technique. Another study[31] reported that MG no more than 100 μm are addressed clinically acceptable for ceramic crowns. However, a wide range of MG values is reported in the literature because of some factors (restoration type and location, material and technique used, etc.).[30,31] Two studies included in this review have shown lower MG values for the heat-press technique when compared to the CAD/CAM technique[14,15] whereas the study by Sener-Yamaner et al.[16] showed lower MG values for the CAD/CAM technique since only one study observed that both the systems demonstrated acceptable, marginal discrepancies.[17]
The presence of marginal inaccuracies in the conventional manufacturing process is expected due to the involvement of multiple materials, as well as clinical and laboratorial stages.[21,32,33] Therefore, the development of CAD/CAM technology optimized the process of producing restorations through creating a project by direct or indirect digitization for the manufacture (additive or subtractive) of restorations with a computer.[34] In this way, many studies compare the marginal adaptation of this processing to fixed prosthodontics,[35,36,37] but few studies compare these techniques in partial restorations.[14,15,16,17] In this systematic review, it was observed the relation to MG and total gap in inlay/onlay restorations, and both processing techniques were comparable. However, when comparing the internal fit, the press technique demonstrated better adaptation than CAD/CAM technique.
The included studies used numerous techniques to evaluate marginal and internal adaptation. The replica technique is a method that allows for long-term analysis and can be applied in clinical circumstances.[15] Meanwhile, this technique can be considered imprecise in cases of small discrepancies due to damage or distortion of the material.[38] Although X-ray computed tomography (CT) produces high-resolution imaging, there is no consensus on the ideal number of MG and internal fit measurements (20 or 50 μm).[39,40] The direct optical microscope technique did not include any inlay-array assembly. In addition, it reduces errors during the sample preparation stage;[41] however, the greatest difficulty is in discerning the color of dental structure and cement.[42] Most of the included studies used human molar teeth for inlay/onlay preparation, and only one study[14] used acrylic tooth. For in vitro studies, the use of natural human teeth is recommended because of its elasticity, adhesion, and strength characteristics that best resemble the clinical condition.[43] Since a small amount of studies met the inclusion/exclusion criteria, the study that used acrylic tooth was included, as this study used the micro-CT to evaluate the disadaptation. This technique is currently considered the most updated investigational methodology to access the adaptation of ceramic restorations.[31,44]
Some variables may influence the value of the marginal discrepancy, among them: tooth preparation, location and number of measuring points, measurement techniques, type of resin cement, and method of manufacturing restorations.[41] In the studies included, two studies evaluated the MG before and after cementation,[15,16] while two studies[14,17] did not cement the restorations since MG values may increase after cementation.[16] Recently, the use of highly led and highly viscous resin cement has been suggested to partially compensate for large cementitious spaces.[45,46] Therefore, the use of random-effects meta-analysis is justified by the discrepancy of the heterogeneity of the included studies.
In this systematic review, the variety of processing techniques, ceramic materials, CAD/CAM systems, and the use of different techniques for evaluation of marginal and internal gap impeded direct comparisons. However, most of the inlay/onlay ceramics were evaluated under in vitro conditions, which increase the potential for parameters standardization and allow better clinical assessment than oral conditions.[47] Future in vivo studies comparing the two techniques approached in this systematic review, regarding the effect on marginal and internal gaps, should cover partial ceramic restorations in addition to fixed dental restorations.
CONCLUSION
Within the limitations of this study, it can be concluded that the pressed fabrication technique showed a more favorable internal adaptation when compared to the milled process. However, regarding the marginal and total gaps, both the techniques proved to be acceptable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gracis S, Thompson VP, Ferencz JL, Silva NR, Bonfante EA. A new classification system for all-ceramic and ceramic-like restorative materials. Int J Prosthodont. 2015;28:227–35. doi: 10.11607/ijp.4244. [DOI] [PubMed] [Google Scholar]
- 2.Boitelle P, Mawussi B, Tapie L, Fromentin O. A systematic review of CAD/CAM fit restoration evaluations. J Oral Rehabil. 2014;41:853–74. doi: 10.1111/joor.12205. [DOI] [PubMed] [Google Scholar]
- 3.Song XF, Ren HT, Yin L. Machinability of lithium disilicate glass ceramic in in vitro dental diamond bur adjusting process. J Mech Behav Biomed Mater. 2016;53:78–92. doi: 10.1016/j.jmbbm.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Giordano R, McLaren EA. Ceramics overview: Classification by microstructure and processing methods. Compend Contin Educ Dent. 2010;31:682–4. 686, 688 passim. [PubMed] [Google Scholar]
- 5.Arora A, Yadav A, Upadhyaya V, Jain P, Verma M. Comparison of marginal and internal adaptation of copings fabricated from three different fabrication techniques: An in vitro study. J Indian Prosthodont Soc. 2018;18:102–7. doi: 10.4103/jips.jips_327_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rekow ED, Silva NR, Coelho PG, Zhang Y, Guess P, Thompson VP. Performance of dental ceramics: Challenges for improvements. J Dent Res. 2011;90:937–52. doi: 10.1177/0022034510391795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhaskaran E, Azhagarasan NS, Miglani S, Ilango T, Krishna GP, Gajapathi B. Comparative evaluation of marginal and internal gap of Co-Cr copings fabricated from conventional wax pattern, 3D printed resin pattern and DMLS tech: An in vitro study. J Indian Prosthodont Soc. 2013;13:189–95. doi: 10.1007/s13191-013-0283-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yildiz C, Vanlıoǧlu BA, Evren B, Uludamar A, Kulak-Ozkan Y. Fracture resistance of manually and CAD/CAM manufactured ceramic onlays. J Prosthodont. 2013;22:537–42. doi: 10.1111/jopr.12037. [DOI] [PubMed] [Google Scholar]
- 9.Hamza TA, Ezzat HA, El-Hossary MM, Katamish HA, Shokry TE, Rosenstiel SF. Accuracy of ceramic restorations made with two CAD/CAM systems. J Prosthet Dent. 2013;109:83–7. doi: 10.1016/S0022-3913(13)60020-7. [DOI] [PubMed] [Google Scholar]
- 10.Groten M, Girthofer S, Pröbster L. Marginal fit consistency of copy-milled all-ceramic crowns during fabrication by light and scanning electron microscopic analysis in vitro. J Oral Rehabil. 1997;24:871–81. doi: 10.1046/j.1365-2842.1997.00592.x. [DOI] [PubMed] [Google Scholar]
- 11.Zarone F, Ferrari M, Mangano FG, Leone R, Sorrentino R. “Digitally Oriented Materials”: Focus on Lithium Disilicate Ceramics. Int J Dent. 2016;2016:9840594. doi: 10.1155/2016/9840594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT Evaluation of ceramic inlays: Comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017;29:49–58. doi: 10.1111/jerd.12271. [DOI] [PubMed] [Google Scholar]
- 15.Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014;42:199–209. doi: 10.1016/j.jdent.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sener-Yamaner ID, Sertgöz A, Toz-Akalın T, Ozcan M. Effect of material and fabrication technique on marginal fit and fracture resistance of adhesively luted inlays made of CAD/CAM ceramics and hybrid materials. J Adhes Sci Technol. 2017;31:55–70. [Google Scholar]
- 17.Vanlioglu BA, Evren B, Yildiz C, Uludamar A, Ozkan YK. Internal and marginal adaptation of pressable and computer-aided design/computer-assisted manufacture onlay restorations. Int J Prosthodont. 2012;25:262–4. [PubMed] [Google Scholar]
- 18.Homsy FR, Özcan M, Khoury M, Majzoub ZAK. Marginal and internal fit of pressed lithium disilicate inlays fabricated with milling, 3D printing, and conventional technologies. J Prosthet Dent. 2018;119:783–90. doi: 10.1016/j.prosdent.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 19.van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. 2010;26:929–39. doi: 10.1016/j.dental.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Kelly JR, Benetti P. Ceramic materials in dentistry: Historical evolution and current practice. Aust Dent J. 2011;56(Suppl 1):84–96. doi: 10.1111/j.1834-7819.2010.01299.x. [DOI] [PubMed] [Google Scholar]
- 21.Beier US, Kapferer I, Burtscher D, Giesinger JM, Dumfahrt H. Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth. Int J Prosthodont. 2012;25:395–402. [PubMed] [Google Scholar]
- 22.Heintze SD. Systematic reviews: I The correlation between laboratory tests on marginal quality and bond strength II The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9(Suppl 1):77–106. [PubMed] [Google Scholar]
- 23.Karlsson S. The fit of Procera titanium crowns.An in vitro and clinical study. Acta Odontol Scand. 1993;51:129–34. doi: 10.3109/00016359309041158. [DOI] [PubMed] [Google Scholar]
- 24.Lang NP, Kiel RA, Anderhalden K. Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J Clin Periodontol. 1983;10:563–78. doi: 10.1111/j.1600-051x.1983.tb01295.x. [DOI] [PubMed] [Google Scholar]
- 25.Wiskott HW, Belser UC, Scherrer SS. The effect of film thickness and surface texture on the resistance of cemented extracoronal restorations to lateral fatigue loading. Int J Prosthodont. 1999;12:255–62. [PubMed] [Google Scholar]
- 26.Rekow D, Thompson VP. Near-surface damage--a persistent problem in crowns obtained by computer-aided design and manufacturing. Proc Inst Mech Eng H. 2005;219:233–43. doi: 10.1243/095441105X9363. [DOI] [PubMed] [Google Scholar]
- 27.Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: A systematic review. J Prosthet Dent. 2014;112:22–30. doi: 10.1016/j.prosdent.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 28.Höland W, Rheinberger V, Apel E, van 't Hoen C, Höland M, Dommann A, et al. Clinical applications of glass-ceramics in dentistry. J Mater Sci Mater Med. 2006;17:1037–42. doi: 10.1007/s10856-006-0441-y. [DOI] [PubMed] [Google Scholar]
- 29.Schultheis S, Strub JR, Gerds TA, Guess PC. Monolithic and bi-layer CAD/CAM lithium-disilicate versus metal-ceramic fixed dental prostheses: Comparison of fracture loads and failure modes after fatigue. Clin Oral Investig. 2013;17:1407–13. doi: 10.1007/s00784-012-0830-1. [DOI] [PubMed] [Google Scholar]
- 30.Azar B, Eckert S, Kunkela J, Ingr T, Mounajjed R. The marginal fit of lithium disilicate crowns: Press vs.CAD/CAM. Braz Oral Res. 2018;32:e001. doi: 10.1590/1807-3107/2018.vol32.0001. [DOI] [PubMed] [Google Scholar]
- 31.Riccitiello F, Amato M, Leone R, Spagnuolo G, Sorrentino R. In vitro evaluation of the marginal fit and internal adaptation of zirconia and lithium disilicate single crowns: Micro-CT comparison between different manufacturing procedures. Open Dent J. 2018;12:160–72. doi: 10.2174/1874210601812010160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christensen GJ. Will digital impressions eliminate the current problems with conventional impressions? J Am Dent Assoc. 2008;139:761–3. doi: 10.14219/jada.archive.2008.0258. [DOI] [PubMed] [Google Scholar]
- 33.Olivera AB, Saito T. The effect of die spacer on retention and fitting of complete cast crowns. J Prosthodont. 2006;15:243–9. doi: 10.1111/j.1532-849X.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- 34.Baroudi K, Ibraheem SN. Assessment of chair-side computer-aided design and computer-aided manufacturing restorations: A review of the literature. J Int Oral Health. 2015;7:96–104. [PMC free article] [PubMed] [Google Scholar]
- 35.Castillo de Oyagüe R, Sánchez-Jorge MI, Sánchez Turrión A, Monticelli F, Toledano M, Osorio R. Influence of CAM vs.CAD/CAM scanning methods and finish line of tooth preparation in the vertical misfit of zirconia bridge structures. Am J Dent. 2009;22:79–83. [PubMed] [Google Scholar]
- 36.de França DG, Morais MH, das Neves FD, Barbosa GA. Influence of CAD/CAM on the fit accuracy of implant-supported zirconia and cobalt-chromium fixed dental prostheses. J Prosthet Dent. 2015;113:22–8. doi: 10.1016/j.prosdent.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 37.Zeng L, Zhang Y, Liu Z, Wei B. Effects of repeated firing on the marginal accuracy of Co-Cr copings fabricated by selective laser melting. J Prosthet Dent. 2015;113:135–9. doi: 10.1016/j.prosdent.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 38.May KB, Russell MM, Razzoog ME, Lang BR. Precision of fit: The Procera All Ceram crown. J Prosthet Dent. 1998;80:394–404. doi: 10.1016/s0022-3913(98)70002-2. [DOI] [PubMed] [Google Scholar]
- 39.Gassino G, Barone Monfrin S, Scanu M, Spina G, Preti G. Marginal adaptation of fixed prosthodontics: A new in vitro 360-degree external examination procedure. Int J Prosthodont. 2004;17:218–23. [PubMed] [Google Scholar]
- 40.Lee KB, Park CW, Kim KH, Kwon TY. Marginal and internal fit of all-ceramic crowns fabricated with two different CAD/CAM systems. Dent Mater J. 2008;27:422–6. doi: 10.4012/dmj.27.422. [DOI] [PubMed] [Google Scholar]
- 41.Nawafleh NA, Mack F, Evans J, Mackay J, Hatamleh MM. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J Prosthodont. 2013;22:419–28. doi: 10.1111/jopr.12006. [DOI] [PubMed] [Google Scholar]
- 42.White SN, Yu Z, Tom JF, Sangsurasak S. In vivo marginal adaptation of cast crowns luted with different cements. J Prosthet Dent. 1995;74:25–32. doi: 10.1016/s0022-3913(05)80224-0. [DOI] [PubMed] [Google Scholar]
- 43.Chitmongkolsuk S, Heydecke G, Stappert C, Strub JR. Fracture strength of all-ceramic lithium disilicate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur J Prosthodont Restor Dent. 2002;10:15–22. [PubMed] [Google Scholar]
- 44.Kim JH, Jeong JH, Lee JH, Cho HW. Fit of lithium disilicate crowns fabricated from conventional and digital impressions assessed with micro-CT. J Prosthet Dent. 2016;116:551–7. doi: 10.1016/j.prosdent.2016.03.028. [DOI] [PubMed] [Google Scholar]
- 45.Hahn P, Attin T, Gröfke M, Hellwig E. Influence of resin cement viscosity on microleakage of ceramic inlays. Dent Mater. 2001;17:191–6. doi: 10.1016/s0109-5641(00)00067-1. [DOI] [PubMed] [Google Scholar]
- 46.Gemalmaz D, Kükrer D. In vivo and in vitro evaluation of marginal fit of class II ceromer inlays. J Oral Rehabil. 2006;33:436–42. doi: 10.1111/j.1365-2842.2005.01562.x. [DOI] [PubMed] [Google Scholar]
- 47.Kern M, Strub JR, Lü XY. Wear of composite resin veneering materials in a dual-axis chewing simulator. J Oral Rehabil. 1999;26:372–8. doi: 10.1046/j.1365-2842.1999.00416.x. [DOI] [PubMed] [Google Scholar]