Abstract
Objective:
Depression and anxiety are comorbid conditions that are disproportionately high among American Indians (AIs) or Alaska Natives. The purpose of this study was to identify potential risk (e.g., low income, intimate partner violence [IPV], adverse childhood experiences [ACEs]) and protective factors (e.g., family resilience, social and community support) related to symptoms of depression and anxiety among AI adults.
Method:
As part of larger exploratory sequential mixed-methods research, the study focused on survey data with 127 AI adults from two Southeastern tribes (n = 117 when missing data were removed). We used the following three-stage hierarchical regression to understand factors related to depressive and anxiety symptoms: (a) demographics, including income; (b) ACEs and IPV; and (c) family resilience, along with family and community support.
Results:
Many participants experienced elevated levels of clinically significant symptoms of depression and anxiety (15% and 20%, respectively). Results indicated lower income was associated with higher depressive and anxiety symptoms. IPV and ACE variables were positively associated with depressive and anxiety symptoms. Family resilience was negatively associated with symptoms of anxiety and depression. Social and community support were associated with symptoms of anxiety.
Conclusions:
The findings provide strong preliminary support for the role of family protective and promotive factors in offsetting symptoms of anxiety and depression. This is contrary to most models of interventions for anxiety and depression focusing on individual psychotherapy rather than promoting family resilience or involvement.
Keywords: American Indians, Alaska Natives, depression, anxiety, family resilience, social support, adverse childhood experiences
Depression and anxiety are well-established comorbid conditions (Jacobson & Newman, 2017; Salcedo, 2018), and both tend to be disproportionately high among American Indians and Alaska Natives (AI/ANs). The U.S. government and sovereign AI/ANs have an established trust responsibility for the federal government to provide for the well-being of AI/AN peoples (Indian Health Services, 2019), yet these persistent and alarming disparities indicate a failure of trust obligations to these sovereign tribes (American Psychological Association, 2010; Gone & Trimble, 2012; Sarche & Spicer, 2008). In this study, we examined greater exposure to trauma and violence, along with family resilience and social support, and their associations with symptoms of anxiety and depression.
Depression and anxiety are highly connected to the psychological trauma that drives AI/AN health disparities (Brockie, Dana-Sacco, Wallen, Wilcox, & Campbell, 2015; Kenney & Singh, 2016; Warne et al., 2017). Understanding these connections is important because AI/AN mortality rates are nearly 50% higher than those of non-AI/ANs (Centers for Disease Control & Prevention, 2014). Suicide is interlinked with depression as, among the general population, two thirds of those completing suicide have documented depression (American Association of Suicidology, 2010; Penninx et al., 1999). Suicide rates among AI/ANs are nearly 50% higher than non-Hispanic Whites (Centers for Disease Control & Prevention, 2014) and have been reported at 1.7 times the rate of all other racial groups (Indian Health Services, 2018). AI/ANs diagnosed with depressive and anxiety disorders are twice as likely to experience a substance use disorder (Rieckmann et al., 2012) and are at heightened risk for hypertension, a primary cause of morbidity and mortality (Ho et al., 2015). Likewise, AI/AN populations experience posttraumatic stress disorder (PTSD) at 2–3 times that of non-AI/ANs (Gone & Trimble, 2012), with a major risk factor being trauma exposure (Beals, Belcourt-Dittloff, et al., 2013). The psychological consequences of trauma include anxiety, depression, PTSD, and suicidal thoughts, which parallel AI/AN mental health disparities (Breiding, Chen, & Black, 2014).
In addition to cited risk factors for health disparities, AI/ANs are affected by culturally distinct factors, such as historical oppression, discrimination, social determinants of health, and environmental injustices (King, Smith, & Gracey, 2009). Social determinants of health (e.g., income, education, employment, and social support; King et al., 2009) are key factors related to trauma, and AI/ANs tend to have lower income, education, employment opportunities, and social opportunities (Gone & Trimble, 2012). High-risk environments characterized by poverty, violence, and illegal substances contribute to trauma exposure (Beals, Manson, et al., 2013; Ehlers, Gizer, Gilder, & Yehuda, 2013). Exposure to adverse childhood experiences (ACEs) has been found to contribute to anxiety and depression, along with substance abuse and PTSD among AIs (Brockie et al., 2015; Warne et al., 2017).
For this study, we used the framework of historical oppression, resilience, and transcendence (FHORT; see Figure 1), an AI-based approach to frame risk and protective factors within this cultural context (Burnette & Figley, 2017). This framework was developed with the focal tribes through 10 years of preliminary research (Burnette & Figley, 2017). According to the FHORT, historical oppression, which includes contemporary oppression such as exposure to psychological trauma and economic inequalities, has undermined Indigenous communities and families through the imposition of historical traumas (e.g., boarding schools that stripped families’ ability to socialize and transmit culture and language to their children), impairing the healthy transmission of affection and love and replacing such beliefs with antagonistic and oppressive social norms (Burnette, 2015). Consequently, social problems such as psychological trauma and violence have increased, and over time, these social ills may give rise to various health disparities, such as depression and anxiety (Burnette, 2015). Historical oppression is inclusive of massive traumas that are historical in nature and contemporary forms of oppression (e.g., low income, intimate partner violence [IPV], and ACEs, which AIs tend to disproportionately experience; Breiding et al., 2014; Brockie et al., 2015; Burnette et al., 2017; Kenney & Singh, 2016; Mersky & Janczewski, 2018; Roh et al., 2015; Warne et al., 2017).
Figure 1.
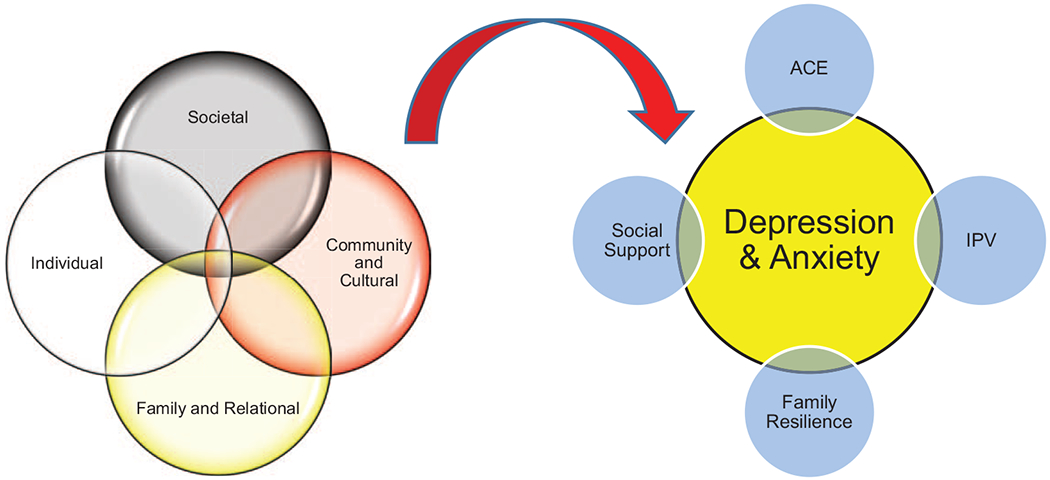
Overlapping ecological risk and protective factors for depression and anxiety according to the framework of historical oppression, resilience, and transcendence (FHORT). See the online article for the color version of this figure.
Yet AI/ANs also experience resilience, or recovery from oppression, and transcendence, or greater growth, despite experiencing chronic oppression; these strengths and protective factors must be documented. The ecological FHORT expands on the prominent concept of historical trauma yet is distinct in that it is localized to specific contexts and is inclusive of the proximal factors that continue to perpetuate oppression (Burnette & Figley, 2017). The balance of risk and protective factors across multiple ecological levels explains whether a person experiences resilience and wellness (balance across physical, mental, emotional, and spiritual health; Burnette & Figley, 2017). Family resilience describes how the family collectively adapts to challenges and promotes family members’ wellness and the wellness of the family as a whole (Masten & Monn, 2015). Despite AI/ANs experiencing elevated mental health problems compared to the general population (Gone & Trimble, 2012), research is limited on the topic. The purpose of this article is to identify potential risk (e.g., low income, IPV, ACEs) and protective factors (e.g., family resilience, social and community support) related to symptoms of depression and anxiety.
Background Literature
Trauma in the forms of IPV (Duran et al., 2004; Libby et al., 2005) and ACEs (Brockie et al., 2015; Kenney & Singh, 2016; Mersky & Janczewski, 2018; Warne et al., 2017) are documented risk factors for depression and anxiety, while social support (Duran et al., 2004; Libby et al., 2005), particularly from families (Burnette, 2017), is a documented protective factor for depression and anxiety among AI/AN individuals. The focus now turns to focal risk and protective factors.
Depression, Anxiety, and Trauma
In 2015, 6.7% of individuals in the U.S. population experienced a major depressive incident, whereas this rate was 8.9% for AI/ANs—the highest of any racial or ethnic group (National Institute of Mental Health, 2015). The limited research on symptoms of anxiety (particularly generalized anxiety disorder) and depression among AI/ANs is growing, and rates have ranged between 10% and 30% (Evans-Campbell, Walters, Pearson, & Campbell, 2012; Gone & Trimble, 2012; Ho et al., 2015). AI/ANs tend to be exposed to trauma and violence at elevated rates (Sarche & Spicer, 2008). Psychological trauma also increases symptoms of depression and anxiety (Moghaddam, Dickerson, Yoon, & Westermeyer, 2014; Rieckmann et al., 2012).
Researchers have reported a strong relationship between trauma—including IPV and childhood trauma—and depression and anxiety (Libby et al., 2005). AI/AN women tend to be more likely than their male counterparts to have been exposed to trauma (i.e., IPV and child maltreatment; Beals, Belcourt-Dittloff, et al., 2013), and IPV is associated with anxiety and depression among AI/ANs (Duran et al., 2009). An estimated 46% of AI/AN women report experiencing IPV victimization, which is the highest rate of IPV among any racial or ethnic group in the United States (Breiding et al., 2014).
With respect to child trauma in the form of child maltreatment, AI/AN children have the highest rate of victimization at 14.3 per 1,000 children compared to African American (13.9 per 1,000), White (8.1 per 1,000), Hispanic (8.0 per 1,000), and Asian (1.6 per 1,000) children (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau, 2019). ACEs—which include childhood abuse, neglect, and household dysfunction (Dube, Felitti, Dong, Giles, & Anda, 2003)—have been found to be risk factors for AI/AN depression. In a sample of 233 AI older adults, approximately three quarters of the sample (75.6%) experienced at least one trauma, and almost one third (31.8%) experienced three or more traumas, which is disproportionately higher than rates reported for the general U.S. population (Brockie et al., 2015; Burnette et al., 2017; Kenney & Singh, 2016; Mersky & Janczewski, 2018; Roh et al., 2015; Warne et al., 2017). Researchers have reported that as ACEs increase, the likelihood of depression and anxiety increases (Felitti, 2002). ACEs also have been identified as risk factors for suicide and violence (Brockie et al., 2015; Whitfield, Anda, Dube, & Felitti, 2003), both of which are elevated among AI/ANs (American Psychological Association, 2010; Gone & Trimble, 2012; Sarche & Spicer, 2008).
Social Support and Resilience
Strong social support, especially from families, has been found to protect against anxiety and depression (Burnette et al., 2017; Çayır, Burke, Spencer, Schure, & Goins, 2017; Roh et al., 2015; Schure & Goins, 2017). Close-knit families and communities are culturally relevant examples of social support and aspects of family resilience, which may be especially applicable in the lives of AI/ANs. Within the FHORT, resilience focuses on recovering and adapting well after experiences of adversity (Fleming & Ledogar, 2008). In some cases, adversity may serve as a turning point, fueling greater levels of life satisfaction and liberation (Tedeschi & Calhoun, 2004). According to Masten (2018), interconnections, interactions, and amassing of risk factors (those that exacerbate or worsen outcomes), protective factors (those that buffer against negative outcomes or enhance positive outcomes), and promotive factors (those that are strengths regardless of the level of adversity or risk) determine whether a system experiences wellness (harmony across the mind, body, spirit, and environment) after adversity or strain (Burnette & Figley, 2017). Indeed, the balance across ecological levels of factors (e.g., individual, family, community) is in constant tension, shifting in interaction with the environment. Because of limitations on how many constructs can be tested with the sample size in one article, we focused on measures of resilience rather than transcendence.
Study Hypotheses
In this study, we connected symptoms of depression and anxiety to exposures to trauma and violence, exploring whether family resilience and social support are promising pathways toward greater wellness. Following the ecological framework of the FHORT, we focused on risk and protective factors at the family (ACEs, family resilience, household income), relational and community (social and community support, IPV), and individual (symptoms of anxiety and depression) ecological levels. More information on the potential role of strength and protective factors is needed to understand buffers and pathways out of adversity and adverse mental health consequences of psychological trauma (in the forms of IPV and ACEs). We explored the following hypotheses: (a) higher income will be negatively associated with symptoms of depression and anxiety, (b) IPV and ACEs will be positively associated with symptoms of depression and anxiety, and (c) family resilience and social support will be negatively associated with symptoms of depression and anxiety. Mapping predictors to the FHORT, low income, IPV, and ACEs were measures of proximal oppression; family resilience and social support were measures of protective and promotive factors (aspects of resilience; Burnette & Figley, 2017).
Method
Study Design and Procedures
Data for this study were part of a larger exploratory sequential mixed-methods research study aimed at exploring culturally specific risk and protective factors for alcohol abuse, family violence, and related mental health outcomes (depression and anxiety). The exploratory mixed-methods design begins with qualitative research, which builds to quantitative data collection and analysis, leading to overall interpretations (Creswell & Plano Clark, 2017). For qualitative data, 436 people across two tribes participated in individual, family, and focus-group interviews. Included within qualitative data were subsamples of elders ages 55 and older (n = 105), adults (n = 147), professionals (n = 70), and youth (n = 114) within each type of interview.
Two Southeastern tribes participated in this study, with tribal members initially coming up with the idea to focus on trauma and resilience in this long-term research that began a decade ago. In the larger study, data were collected through field notes; individual and group interviews with youth, adults, elders, and professionals; family interviews; administrative data; and a survey to understand and identify culturally relevant risk and protective factors related to social, psychological, and health disparities (Burnette, Boel-Studt, et al., 2019; Burnette, Renner, et al., 2019; McKinley et al., 2020, 2019). The current study focused exclusively on the survey data. All study procedures were approved by the Tulane University Institutional Review Board and the tribal councils of the focal tribes, whose identities are protected due to tribal agreements. Results were provided to tribes prior to publication on more than 10 occasions.
Data Collection and Sample
Members from two Southeastern U.S. tribes participated in this study. Both tribes have enrolled populations of over 10,000 members. Tribe A is federally recognized and located further inland from the Gulf of Mexico. It has experienced significant economic development, with its own schools; health care and medical services; and police, fire, land management, and health and human services facilities. Tribe B is state recognized and located in proximity to water and the Gulf Coast. Tribe B has fewer economic resources, and the absence of federal recognition has undermined its ability to provide tribal infrastructure for its members. Tribe B offers employment as well as educational and other individual programs for youth and tribal members. All federally recognized tribal members from Tribe A are eligible for health care locally through Indian Health Services, whereas Tribe B does not have access to these services. Survey data were collected between April and October 2016. The survey was open to any member of Tribe A or Tribe B over the age of 18, including but not limited to those who participated in the interviews or focus groups that were part of the larger study. This convenience sample was recruited through community newsletters, word of mouth, and participants from the qualitative portion. Participants had the option to complete the survey in three ways: (a) online using Qualtrics (2014) software; (b) by hard copy (mailed to the participant and returned in a self-addressed envelope); or (c) over the phone, with a research team member reading items and recording participants’ answers. Participants entered a drawing for $50 gift cards, and approximately 1 in 2 (n = 70, 55%) received a gift card as compensation for their participation. Participant names were supplied only for the purpose of participant compensation.
A total of 161 individuals began the survey, and 79% completed the survey (n = 127). The total sample included 80 members of Tribe A and 47 members of Tribe B. Table 1 presents demographic statistics for the sample. Ten participants had data missing from some of the key variables and were removed from the sample, resulting in a final analytic sample of 117. Prior to all publications, comprehensive results were reported to the tribes on over 10 presentations.
Table 1.
Survey Demographics
| Quantitative follow-up survey | n (%) | M (SD) |
|---|---|---|
| Tribe A | 80 (63.0) | |
| Tribe B | 47 (37.0) | |
| Male | 23 (19.1) | |
| Female | 104 (81.9) | |
| Age (range = 21–80 years) | 46.2 (14.9) | |
| Married | 51 (40.2) | |
| Number of children (range = 0–14) | 3.77 (2.4) | |
| Household type | ||
| Single (live by self) | 15 (11.8) | |
| Couple (no children) | 20 (15.7) | |
| Single parent | 25 (19.7) | |
| Two parent | 49 (38.6) | |
| Extended/blended family | 18 (14.2) | |
| Education | ||
| Less than high school | 12 (9.5) | |
| High school or equivalent | 18 (14.2) | |
| Some college/vocational degree | 28 (22.1) | |
| Associate degree | 27 (21.3) | |
| Bachelor’s degree or higher | 26 (20.5) | |
| Working full-time | 85 (66.0) | |
| Somewhat difficult to pay bills/economically | 69 (54.3) | |
| Annual household income | ||
| <$15,000 | 18 (14.2) | |
| $15,001–25,000 | 21 (16.5) | |
| $25,001–50,000 | 39 (30.7) | |
| $50,001–75,000 | 22 (17.3) | |
| >$75,001 | 27 (21.3) | |
| Type of community | ||
| Reservation/tribal communities | 105 (82.7) | |
| Nearby/off-reservation | 15 (11.8) | |
| Out of state | 7 (5.5) | |
| Intimate partner violence victimization (PVS) | 2.0 (2.2) | |
| ACES | 2.7 (2.5) | |
| Family Resilience Inventory (FRI) | 18 (3.2) | |
| Social Support Index | 47.1 (8.0) |
Note. N = 127. PVS = Partner Victimization Scale; ACES = Adverse Childhood Experiences Scale; FRI = Family Resilience Index. Percentages are rounded up to the nearest 10th percent. Extended families include grandparents, aunts, uncles, cousins, etc. Blended families include stepparents and/or stepchildren. Regarding type of communities, one tribe is federally recognized (has reservation communities), and the other is state recognized (has tribal communities but not the federal trust land of reservations). These distinctions are noted by the reservation/tribal communities’ label. Although some of the communities are rural < 2,500, the majority of communities are considered urban clusters, which have populations between 2,500 and 50,000 (U.S. Census Bureau, 2016).
Measures
See Table 2 for a description of measures. Independent variables included age, gender, household income, marital status, partner victimization, childhood adversity, family resilience, and social support. Included as controls/covariates were age, gender, income, and marital status.
Table 2.
Table of Measures
| Variable and measure | # Items | Response set | Example items | Scoring | Reliability | Citation |
|---|---|---|---|---|---|---|
| Depressive symptoms: Patient Health Questionnaire-9 | 9 | 0 = not at all, 3 = nearly every day | Loss of interest or pleasure, trouble falling asleep, feeling tired or having little energy | Added: total scores 0–27 (0–4 = none/minimal, 5–9 = mild, 10–14 = moderate, 15–19 = moderately severe, 20–27 = severe) | (α = .89) | Kroenke, Spitzer, and Williams (2001) |
| Anxiety: Generalized Anxiety Disorder-7 | 7 | 0 = not at all, 3 = nearly every day | Feeling nervous, anxious, or on edge, not being able to stop or control worrying, and having trouble relaxing | Added: total scores 0–21 (5 = mild, 10 = moderate, 15 = severe depression) | (α = .93) | Spitzer, Kroenke, Williams, and Löwe (2006) |
| Age | — | Raw age | — | — | — | — |
| Income | — | < $15,000 $15,001–25,000 $25,001–50,000 $50,001–75,000 > $75,001 |
— | — | ||
| Gender | — | 0 = female, 1 = male | — | — | — | — |
| Marital status | — | 0 = unmarried, 1 = married | — | — | — | — |
| Intimate partner violence: Partner Victimization Scale | 6 | 0 = no, 1 = yes | Not including horseplay or joking around, my partner pushed, grabbed, shook, or hit me. | Added: total scores 0–24, higher scores indicating more victimization | (α = .87) | Hamby (2016) |
| Adverse childhood experiences | 10 | 0 = no, 1 = yes | See Figure A in online supplemental materials for complete scale. | Added: total scores 0–10 | (α = .79) | Felitti et al. (1998) |
| Family Resilience Index | 20 | 0 = no, 1 = yes | See Figure B in online supplemental materials for complete scale. | Added: total scores 0–20 | (α = .92) | Burnette, Boel-Studt, et al. (2019) |
| Social/community support: Social Support Index | 17 | 1 = strongly disagree, 5 = strongly agree | People in this community are willing to help, and I have friends who let me know they value who I am. | Added: total scores 17–85, with greater scores indicating higher social and community support | (α = .75) | McCubbin, Thompson, and McCubbin (1996) |
Data Analysis
We used a three-stage hierarchical regression to examine outcomes of depression and anxiety, separately. Following the FHORT as our guide, Model 1 included demographics (age, gender, marital status) and the social determinant of health: income. Model 2 included trauma in the form of IPV and ACEs as risk factors. Model 3 focused on family resilience and social support as protective factors. Using the three models, our aims were to (a) examine incremental change in outcome variance that was uniquely associated with different sets of predictors, (b) examine the amount of variance in the outcomes accounted for by each set of predictors, and (c) examine change in the outcomes associated with each individual predictor.
Data were determined to be missing at random. Following Kang’s (2013) guidance on handling missing data, listwise deletion was used. However, the regression also was run using pairwise and mean imputation to examine any significant differences in outcomes with these different strategies. After no significant variation was viewed, listwise deletion was chosen as the most impartial and conservative strategy (Kang, 2013). This left an analytic sample of 117 participants included in the regression analysis. No issue with multicollinearity was observed among all independent variables (Mertler & Vannatta, 2010). Table A in the online supplemental materials displays the correlations between predictor and outcome variables. All analyses were performed using SPSS Version 25 software.
Results
Depression
The Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001) was our measure of depressive symptoms. For PHQ-9 scores, 25.2% of participants reported moderate depressive symptoms or greater, which indicates the percentage of those scoring at the level of clinical significance (Brody, Pratt, & Hughes, 2018). The demographic set (gender, age, income) accounted for 13% of the unique variance in depression, R2Δ = .13, F(4, 112) = 4.26, p = .003. In Model 2, adding IPV victimization and ACEs contributed a 13.2% incremental change in the R2, R2Δ = .13, F(2, 110) = 9.82, p < .000. In Model 3, family resilience and social support accounted for 16% of unique variance in depression, R2Δ = .16, F(2, 108) = 14.84, p < .000. Model 3 was statistically significant with all predictors accounting for 42% of the variance in depression scores, R2 = .42, F(8, 108) = 9.88, p < .000. Results in Table 3 show, in the final model, inclusive of all predictors, only income and family resilience were statistically significant predictors of depression. Specifically, higher scores on the Family Resilience Index (Burnette et al., 2019) and higher income were associated with lower mean depression scores, controlling for all other independent variables. The observed statistical power for this model was equal to 1.
Table 3.
Hierarchical Regression With Symptoms of Depression and Anxiety as Outcomes
| Depressive symptoms |
Anxiety symptoms |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model | B | SE | β | 95% CI | B | SE | β | 95% CI |
| Model 1 | ||||||||
| Age | −.083* | .039 | −.191 | [−.161, −.006] | −.097** | .034 | −.261 | [−.164, −.030] |
| Female | 1.506 | 1.515 | .088 | [−1.496, 4.509] | .798 | 1.305 | .055 | [−1.787, 3.382] |
| Annual income | −1.027** | .331 | −.290 | [−1.683, −.371] | −.680* | .285 | −.225 | [−1.244, −.115] |
| Married/cohabitating | −1.322 | 1.260 | −.098 | [−3.817, 1.174] | −.779 | 1.084 | −.068 | [−2.928, 1.370] |
| Model 2 | ||||||||
| Age | −.050 | .037 | −.113 | [−.123, .024] | −.067* | .032 | −.180 | [−.130, −.004] |
| Female | .060 | 1.460 | .004 | [−2.834, 2.954] | −.383 | 1.243 | −.026 | [−2.846, 2.079] |
| Annual income | −1.132*** | .309 | −.319 | [−1.744, −.520] | −.781** | .263 | −.258 | [−1.302, −.260] |
| Married/cohabitating | −1.179 | 1.176 | −.087 | [−3.510, 1.152] | −.583 | 1.001 | −.051 | [−2.567, 1.401] |
| PVS | .744* | .287 | .247 | [.176, 1.313] | .530* | .244 | .206 | [.047, 1.014] |
| ACES | .537* | .239 | .205 | [.063, 1.012] | .612** | .204 | .275 | [.208, 1.016] |
| Model 3 | ||||||||
| Age | −.060 | .036 | −.136 | [−.130, .011] | −.060 | .032 | −.162 | [−.123, .002] |
| Female | .647 | 1.319 | .038 | [−1.967, 3.262] | .187 | 1.166 | .013 | [−2.124, 2.498] |
| Annual income | −1.004*** | .277 | −.283 | [−1.554, −.454] | −.707** | .245 | −.234 | [−1.193, −.221] |
| Married/cohabitating | −.401 | 1.063 | −.030 | [−2.509, 1.706] | .025 | .940 | .002 | [−1.837, 1.888] |
| PVS | .370 | .265 | .123 | [−.156, .896] | .269 | .235 | .105 | [−.196, .734] |
| ACES | .353 | .217 | .135 | [−.078, .783] | .468* | .192 | .210 | [.087, .848] |
| FRI (current family) | −.751*** | .173 | −.367 | [−1.093, −.408] | −.413** | .153 | −.237 | [−.716, −.110] |
| SSI | −.113 | .072 | −.136 | [−.255, .030] | −.149* | .063 | −.211 | [−.274, −.023] |
Note. N = 117. SE = standard error; CI = confidence interval; PVS = Partner Victimization Scale; ACES = Adverse Childhood Experiences Scale; FRI = Family Resilience Index; SSI = Social Support Index.
p = .05.
p = .01.
p = .001.
Anxiety
The General Anxiety Disorder-7 scale (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006) was used to measure symptoms of anxiety. According to the GAD-7 (M = 12.84, SD = 5.65), 19.7% of participants reported clinically significant levels of anxiety (Spitzer et al., 2006). In the regression analysis, Model 1 (gender, age, income) accounted for 11% of the variance in GAD-7 anxiety scores, R2Δ = .11, F(4, 112) = 3.56, p = .009. Adding IPV victimization and ACEs (Model 2) accounted for a 15.2% incremental change in variance, R2Δ = .15, F(2, 110) = 11.34, p < .000. Model 3 (family resilience and social support) accounted for 11.3% of the unique variance in anxiety scores, R2Δ = .11, F(2, 108) = 9.84, p < .000. Model 3 was statistically significant with all predictors accounting for 61.5% of the variance in anxiety scores, R2 = .62, F(8, 108) = 8.20, p < .000. The final model (see Table 3) shows family resilience and income were most strongly associated with anxiety, followed by ACEs and social support, respectively. Higher family resilience, higher income, and greater social support were associated with lower mean anxiety scores, and a greater number of ACEs was associated with increased anxiety, controlling for other independent variables. The observed statistical power for this model was equal to 1.
Discussion
The purpose of this study was to examine associations between risk and protective factors and symptoms of depression and anxiety among AI/AN adults. Following the FHORT, we explored three hypotheses: (a) higher income will be negatively associated with symptoms of depression and anxiety, (b) IPV and ACEs will be positively associated with symptoms of depression and anxiety, and (c) family resilience and social support will be negatively associated with symptoms of depression and anxiety. Low income, IPV, and ACEs served as measures of proximal oppression, whereas family resilience and social support were measures of protective and promotive factors. Based on the final model for each of the two outcomes, we found support for the first hypothesis as income was negatively associated with both depression and anxiety. We found partial support for the second hypothesis. Neither IPV victimization nor ACEs were significantly associated with depression, and only ACEs were significantly associated with anxiety. We found support for the third hypothesis as family resilience was negatively associated with symptoms of depression and anxiety, whereas social support was negatively associated with symptoms of anxiety.
Several important points can be gleaned from our study results. First, approximately 25% of the people in the sample reported clinically significant levels of depressive symptoms. This rate is much higher than the rate of 8.1% of all Americans age 20 and older (5.5% of men and 10.4% of women) reporting clinically significant levels of depression between the years 2013 and 2016 using the same scale (Brody et al., 2018). Second, 19.7% of participants reported clinically significant levels of anxiety as well, which is much higher than the 8% rate of the general population reporting clinically significant levels of generalized anxiety (Jordan, Shedden-Mora, & Löwe, 2017). This reveals a strong presence of symptoms of depression and anxiety among study participants, consistent with extant literature with respect to increased mental health problems among AI/AN individuals. As expected in the first hypothesis, lower income was associated with higher depressive symptoms, and this association remained across all three models. This finding is significant given AI/ANs tend to be economically disadvantaged due to historical oppression, and this socioeconomic marginalization may have psychological consequences (Gone & Trimble, 2012). Due to historical oppression, poverty may place greater daily stress upon AI/ANs, with fewer financial resources to deal with this stress, leading to greater internalization of oppression, which can manifest as depression. As expected, when IPV and ACE variables were added to the second model, both were positively associated with depressive symptoms. Participants, on average, experienced almost three ACEs, which was consistent with elevated levels of ACEs identified in other tribal research (Brockie et al., 2015; Burnette et al., 2017; Kenney & Singh, 2016; Roh et al., 2015; Warne et al., 2017). Yet in the third model, which added family resilience and social support as predictors, only family resilience and income accounted for unique variance in depressive symptoms. This provides strong preliminary support for the role of family protective and promotive factors in potentially providing a buffer against depressive symptoms. A strong family environment may provide the social support and warmth that enables the risk for depression to be minimized. This is contrary to most models of interventions for depressive symptoms that focus on individual psychotherapy rather than promoting family resilience or involvement.
For anxiety, lower income was associated with higher anxiety symptoms in Model 1, and income remained robust throughout all three models, supporting the first hypothesis. As expected, IPV and ACEs were risk factors for anxiety symptoms. However, in Model 3, when family resilience and social and community support were added, only ACEs accounted for unique variance in depressive symptoms. This may be due to shared variance among the predictor variables. Holistically, the importance of family background, family resilience, and social and community support are highly salient in our study results. Capitalizing on family resilience and social support are promising avenues to buffer against the consequences of psychological trauma in the forms of IPV and ACEs, particularly with respect to symptoms of depression and anxiety.
This work identified factors that may relate to mental health not only at the individual level (income) but also at the family, relational, and community levels (family resilience, social and community support, ACEs, and IPV). Given their relevance, it is important to extend the scope of factors relating to mental health beyond individual phenomena to the social, familial, cultural, and community contexts that play significant roles. Depression, anxiety, and their comorbidity is an increasing challenge for the health care system. As such, it is important to explore which factors might buffer the negative effects of mental health disorders. It is also important to recognize that the focus on racial and/or ethnic group membership in research leads to a more comprehensive understanding of risk and protective factors and provides a clearer picture of how mental health disorders vary across diverse groups (Bracken & Reintjes, 2010; Watkins, Assari, & Johnson-Lawrence, 2015). Researchers should include measures of racial and ethnic group identity in studies of mental health conditions so similar and unique risk and protective factors may be uncovered (Watkins et al., 2015). Understanding similarities and differences in what exacerbates and buffers mental health symptoms among individuals of different racial and ethnic groups may help mental health clinicians and service providers use and develop more effective intervention strategies.
Study Strengths and Limitations
Despite relying on a small sample, our results were robust and demonstrated significant associations with depression and anxiety symptoms. Although the selected risk and protective factors were associated with depressive and anxiety symptoms in hypothesized directions, it may be valuable to explore moderation or mediation analyses with larger samples in the future. This would enhance the understanding of how experiences of victimization and factors of family support influence symptoms of depression and anxiety among AI/AN individuals, both directly and indirectly, in addition to focusing on differences by factors such as gender. Likewise, measuring depressive symptoms in tribal communities may vary from nontribal communities; thus, caution should be used in making interpretations due to potential measurement error. Finally, income disparities may operate differently in rural reservation dwelling communities, which may experience increased constraints in economic opportunity and mobility. Researchers also could examine the cumulative effect of these risk and protective factors over time. Moreover, an inquiry on PTSD is warranted as ACEs and IPV also likely would be associated with this outcome. The results of this study may not be generalizable to other AIs. Given the heterogeneity of AI/ANs, researchers are encouraged to continue the exploration of risk and protective factors for mental health symptomology among members of other tribes and with larger samples. Future research to replicate our findings and further test the usefulness of the FHORT for understanding mental health among AI/AN individuals is also recommended.
Implications
Reports of moderate levels of depression and anxiety by participants in this study reflect the larger body of literature on the heightened rates of mental health disorders among AI/AN individuals. Beyond the agreements between the U.S. government and AI/ANs, moral and ethical issues in the failure to close the mental health gap remain. Our study results highlight the association between family trauma, victimization, and mental health symptomology, but they also highlight strengths and protective factors among AI/AN families and communities, which may be steppingstones to greater health and wellness. Our findings appear to be consistent with other researchers studying anxiety and depression among non-AI/ANs and those who specifically integrate trauma in this conceptualization. For example, Watson et al. (2007) developed the Inventory of Depression and Anxiety Symptoms, which was designed to assess specific symptom dimensions of major depression and related anxiety disorders, including suicidality, ill temper, panic, and traumatic intrusions.
Because of their connection with family and tradition, AI/AN families may be an important source of reference for non-AI/AN families as these distinct sources of support and strength may be beneficial for broad populations. Practitioners can work to enhance family resilience as a sustainable source of strength for AI/ANs experiencing symptoms of depression and anxiety. The risk factors identified with AI/AN people may not be as great for non-AI/AN people, but the promotive and protective factors contained in the Family Resilience Inventory (Burnette, Boel-Studt, et al., 2019) may provide guidelines to strengthen and support pathways to resilience for all people. Practitioners and clinicians can situate depression and anxiety within the cultural context of historical oppression, connecting them with historical and sociostructural causes. At the same time, it is important to respect and appreciate AI/AN collective resilience.
Supplementary Material
Clinical Impact Statement.
Although depression and anxiety are disparities among American Indians related to psychological trauma, little research focuses on these populations. This work revealed that primary forms of trauma—adverse childhood experiences and intimate partner violence—play roles in symptoms of depression and anxiety among American Indians. Yet income, family resilience, and social and community support may play an even stronger role in relation to depression and anxiety. Treatments for depression and anxiety may not capitalize on the potentially protective role families and social support could play in offsetting depression and anxiety. Thus, family and social support may be incorporated into treatment.
Acknowledgments
This work was supported by the Fahs-Beck Fund for Research and Experimentation Faculty Grant Program (Grant 552745), The Silberman Fund Faculty Grant Program (Grant 552781), the Newcomb College Institute Faculty Grant at Tulane University, the University Senate Committee on Research Grant Program at Tulane University, the Global South Research Grant through the New Orleans Center for the Gulf South at Tulane University, The Center for Public Service at Tulane University, and the Carol Lavin Bernick Research Grant at Tulane University. This work was supported in part by Award K12HD043451 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (to Catherine E. McKinley, Building Interdisciplinary Research Careers in Women’s Health Scholar). This work also was supported in part by Grant U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Catherine E. McKinley, Tulane University.
Shamra Boel-Studt, Florida State University.
Lynette M. Renner, University of Minnesota
Charles R. Figley, Tulane University
References
- American Association of Suicidology. (2010). Some facts about suicide and depression. Retrieved from http://www.suicidology.org/
- American Psychological Association. (2010). APA fact sheet, mental health disparities: American Indian and Alaska Natives Retrieved from http://www.psych.org/share/omna/mental-health-disparities-fact-sheet--american-indians.aspx
- Beals J, Belcourt-Dittloff A, Garroutte EM, Croy C, Jervis LL, Whitesell NR, … the AI-SUPERPFP Team. (2013). Trauma and conditional risk of posttraumatic stress disorder in two American Indian reservation communities. Social Psychiatry and Psychiatric Epidemiology, 48, 895–905. 10.1007/s00127-012-0615-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, Manson SM, Croy C, Klein SA, Whitesell NR, & Mitchell CM, & the AI-SUPERPFP Team. (2013). Lifetime prevalence of posttraumatic stress disorder in two American Indian reservation populations. Journal of Traumatic Stress, 26, 512–520. 10.1002/jts.21835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bracken BA, & Reintjes C (2010). Age, race, and gender differences in depressive symptoms: A lifespan developmental investigation. Journal of Psychoeducational Assessment, 28, 40–53. 10.1177/0734282909336081 [DOI] [Google Scholar]
- Breiding MJ, Chen J, & Black MC (2014). Intimate partner violence in the United States—2010. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, & Campbell JC (2015). The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based Native American adolescents and young adults. American Journal of Community Psychology, 55, 411–421. 10.1007/s10464-015-9721-3 [DOI] [PubMed] [Google Scholar]
- Brody DJ, Pratt LA, & Hughes J (2018). Prevalence of depression among adults aged 20 and over: United States, 2013–2016 (NCHS Data Brief No. 303). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Burnette CE (2015). Historical oppression and intimate partner violence experienced by Indigenous women in the U.S.: Understanding connections. Social Service Review, 89, 531–563. 10.1086/683336 [DOI] [Google Scholar]
- Burnette CE (2017). Family and cultural protective factors as the bedrock of resilience and growth for Indigenous women who have experienced violence. Journal of Family Social Work, 21, 45–62. 10.1080/10522158.2017.1402532 [DOI] [Google Scholar]
- Burnette CE, Boel-Studt S, Renner LM, Figley CR, Theall KP, Miller Scarnato J, & Billiot S (2019). The Family Resilience Inventory: A culturally grounded measure of current and family-of-origin protective processes in Native American families. Family Process, 59, 695–708. 10.1111/famp.12423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CE, & Figley CR (2017). Historical oppression, resilience, and transcendence: Can a holistic framework help explain violence experienced by Indigenous people? Social Work, 62, 37–44. 10.1093/sw/sww065 [DOI] [PubMed] [Google Scholar]
- Burnette CE, Roh S, Lee KH, Lee YS, Newland LA, & Jun JS (2017). A comparison of risk and protective factors related to depressive symptoms among American Indian and Caucasian older adults. Health & Social Work, 42(1), e15–e23. 10.1093/hsw/hlw055 [DOI] [PubMed] [Google Scholar]
- Çayır E, Burke MP, Spencer M, Schure MB, & Goins RT (2017). Lifetime trauma and depressive symptomatology among older American Indians: The native elder care study. Community Mental Health Journal, 54, 740–747. 10.1007/s10597-017-0179-7 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). American Indian and Alaska Native death rates nearly 50 percent greater than those of non-Hispanic Whites. Retrieved from http://www.cdc.gov/media/releases/2014/p0422-natamerican-deathrate.html
- Creswell JW, & Plano Clark VL (2017). Designing and conducting mixed methods research. Thousand Oaks, CA: Sage. [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, & Anda RF (2003). The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventive Medicine, 37, 268–277. 10.1016/S0091-7435(03)00123-3 [DOI] [PubMed] [Google Scholar]
- Duran B, Malcoe LH, Sanders M, Waitzkin H, Skipper B, & Yager J (2004). Child maltreatment prevalence and mental disorders outcomes among American Indian women in primary care. Child Abuse & Neglect, 28, 131–145. 10.1016/j.chiabu.2003.06.005 [DOI] [PubMed] [Google Scholar]
- Duran B, Oetzel J, Parker T, Malcoe LH, Lucero J, & Jiang Y (2009). Intimate partner violence and alcohol, drug, and mental disorders among American Indian women in primary care. American Indian and Alaska Native Mental Health Research, 16, 11–27. 10.5820/aian.1602.2009.11 [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Gilder DA, & Yehuda R (2013). Lifetime history of traumatic events in an American Indian community sample: Heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. Journal of Psychiatric Research, 47, 155–161. 10.1016/j.jpsychires.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T, Walters KL, Pearson CR, & Campbell CD (2012). Indian boarding school experience, substance use, and mental health among urban two-spirit American Indian/Alaska Natives. The American Journal of Drug and Alcohol Abuse, 38, 421–427. 10.3109/00952990.2012.701358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ (2002). Belastungen in der Kindheit und Gesundheit im Erwachsenenalter: die Verwandlung von Gold in Blei [The relationship of adverse childhood experiences to adult health: Turning gold into lead]. Zeitschrift für Psychosomatische Medizin und Psychotherapie, 48, 359–369. 10.13109/zptm.2002.48.4359 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fleming J, & Ledogar RJ (2008). Resilience, an evolving concept: A review of literature relevant to Aboriginal research. Pimatisiwin, 6, 7–23. Retrieved from https://journalindigenouswellbeing.com/media/2019/02/3_Fleming.pdf [PMC free article] [PubMed] [Google Scholar]
- Gone JP, & Trimble JE (2012). American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology, 8, 131–160. 10.1146/annurev-clinpsy-032511-143127 [DOI] [PubMed] [Google Scholar]
- Hamby S (2016). Self-report measures that do not produce gender parity in intimate partner violence: A multi-study investigation. Psychology of Violence, 6, 323–335. 10.1037/a0038207 [DOI] [Google Scholar]
- Ho AK, Thorpe CT, Pandhi N, Palta M, Smith MA, & Johnson HM (2015). Association of anxiety and depression with hypertension control: A U.S. multidisciplinary group practice observational study. Journal of Hypertension, 33, 2215–2222. 10.1097/HJH.0000000000000693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indian Health Services. (2018). Disparities. Retrieved from https://www.ihs.gov/newsroom/includes/themes/responsive2017/display_objects/documents/factsheets/Disparities.pdf
- Indian Health Services. (2019). Basis for health services. Retrieved from https://www.ihs.gov/newsroom/factsheets/basisforhealthservices/
- Jacobson NC, & Newman MG (2017). Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychological Bulletin, 143, 1155–1200. 10.1037/bul0000111 [DOI] [PubMed] [Google Scholar]
- Jordan P, Shedden-Mora MC, & Löwe B (2017). Psychometric analysis of the Generalized Anxiety Disorder scale (GAD-7) in primary care using modern item response theory. PLoS ONE, 12(8), e0182162 10.1371/journal.pone.0182162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang H (2013). The prevention and handling of the missing data. Korean Journal of Anesthesiology, 64, 402–406. 10.4097/kjae.2013.64.5.402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney MK, & Singh GK (2016). Adverse childhood experiences among American Indian/Alaska Native children: The 2011–2012 National Survey of Children’s Health. Scientifica, 2016, 7424239 10.1155/2016/7424239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Smith A, & Gracey M (2009). Indigenous health part 2: The underlying causes of the health gap. The Lancet, 374, 76–85. 10.1016/S0140-6736(09)60827-8 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Novins DK, Beals J, & Manson SM, & the AI-SUPERPFP Team. (2005). Childhood physical and sexual abuse and subsequent depressive and anxiety disorders for two American Indian tribes. Psychological Medicine, 35, 329–340. 10.1017/S0033291704003599 [DOI] [PubMed] [Google Scholar]
- Masten AS (2018). Resilience theory and research on children and families: Past, present, and promise. Journal of Family Theory & Review, 10, 12–31. 10.1111/jftr.12255 [DOI] [Google Scholar]
- Masten AS, & Monn AR (2015). Child and family resilience: A call for integrated science, practice, and professional training. Family Relations, 64, 5–21. [Google Scholar]
- McCubbin HI, Thompson AI, & McCubbin MA (1996). Family assessment: Resiliency, coping and adaptation: Inventories for research and practice. Madison, WI: University of Wisconsin-Madison, Center for Excellence in Family Studies. [Google Scholar]
- McKinley CE, Boel-Studt S, Renner LM, Figley CR, Billiot S, & Theall KP (2020). The Historical Oppression Scale: Preliminary conceptualization and measurement of historical oppression among Indigenous peoples of the United States. Transcultural Psychiatry, 57, 288–303. 10.1177/1363461520909605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Figley CR, Woodward SM, Liddell JL, Billiot S, Comby N, & Sanders S (2019). Community-engaged and culturally relevant research to develop behavioral health interventions with American Indians and Alaska Natives. American Indian and Alaska Native Mental Health Research, 26, 79–103. 10.5820/aian.2603.2019.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, & Janczewski CE (2018). Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of U.S. women. Child Abuse & Neglect, 76, 480–487. 10.1016/j.chiabu.2017.12.012 [DOI] [PubMed] [Google Scholar]
- Mertler CA, & Vannatta RA (2010). Advanced and multivariate statistical methods (4th ed.). Los Angeles, CA: Pyrecek. [Google Scholar]
- Moghaddam JF, Dickerson DL, Yoon G, & Westermeyer J (2014). Nicotine dependence and psychiatric and substance use disorder comorbidities among American Indians/Alaska Natives: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 144, 127–133. 10.1016/j.drugalcdep.2014.08.017 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2015). Major depression among adults. Retrieved from https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml
- Penninx BW, Geerlings SW, Deeg DJ, van Eijk JT, van Tilburg W, & Beekman AT (1999). Minor and major depression and the risk of death in older persons. Archives of General Psychiatry, 56, 889–895. 10.1001/archpsyc.56.10.889 [DOI] [PubMed] [Google Scholar]
- Qualtrics. (2014). Qualtrics [Computer software]. Provo, UT: Qualtrics. [Google Scholar]
- Rieckmann T, McCarty D, Kovas A, Spicer P, Bray J, Gilbert S, & Mercer J (2012). American Indians with substance use disorders: Treatment needs and comorbid conditions. The American Journal of Drug and Alcohol Abuse, 38, 498–504. 10.3109/00952990.2012.694530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roh S, Burnette CE, Lee KH, Lee YS, Easton SD, & Lawler MJ (2015). Risk and protective factors for depressive symptoms among American Indian older adults: Adverse childhood experiences and social support. Aging & Mental Health, 19, 371–380. 10.1080/13607863.2014.938603 [DOI] [PubMed] [Google Scholar]
- Salcedo B (2018, January 19). The comorbidity of anxiety and depression [Web log post]. Retrieved from https://www.nami.org/blogs/nami-blog/january-2018/the-comorbidity-of-anxiety-and-depression
- Sarche M, & Spicer P (2008). Poverty and health disparities for American Indian and Alaska Native children: Current knowledge and future prospects. Annals of the New York Academy of Sciences, 1136, 126–136. 10.1196/annals.1425.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schure M, & Goins RT (2017). Psychometric examination of the center for epidemiologic studies depression scale with older American Indians: The Native Elder Care Study. American Indian and Alaska Native Mental Health Research, 24, 1–13. 10.5820/AIAN.2403.2017.1 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, & Calhoun LG (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15, 1–18. 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- U.S. Census Bureau. (2016). Urban and Rural Areas. Retrieved from https://www.census.gov/history/www/programs/geography/urban_and_rural_areas.html#:~:text==The%20Census%20Bureau%20has%20continued,%2C%204%2C000%2C%20and%202%2C500%20inhabitants
- U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2019). Child Maltreatment 2017. Retrieved from https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment
- Warne D, Dulacki K, Spurlock M, Meath T, Davis MM, Wright B, & McConnell KJ (2017). Adverse childhood experiences (ACE) among American Indians in South Dakota and associations with mental health conditions, alcohol use, and smoking. Journal of Health Care for the Poor and Underserved, 28, 1559–1577. 10.1353/hpu.2017.0133 [DOI] [PubMed] [Google Scholar]
- Watkins DC, Assari S, & Johnson-Lawrence V (2015). Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. Journal of Racial and Ethnic Health Disparities, 2, 385–394. 10.1007/s40615-015-0085-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, … Stuart S (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological assessment, 19, 253–268. [DOI] [PubMed] [Google Scholar]
- Whitfield CL, Anda RF, Dube SR, & Felitti VJ (2003). Violent childhood experiences and the risk of intimate partner violence in adults’ assessment in a large health maintenance organization. Journal of Interpersonal Violence, 18, 166–185. 10.1177/0886260502238733 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


