Abstract
Objective The aim of this systematic review was to synthesize current knowledge of the factors influencing healthcare professional adoption of mobile health (m-health) applications.
Methods Covering a period from 2000 to 2014, we conducted a systematic literature search on four electronic databases (PubMed, EMBASE, CINAHL, PsychInfo). We also consulted references from included studies. We included studies if they reported the perceptions of healthcare professionals regarding barriers and facilitators to m-health utilization, if they were published in English, Spanish, or French and if they presented an empirical study design (qualitative, quantitative, or mixed methods). Two authors independently assessed study quality and performed content analysis using a validated extraction grid with pre-established categorization of barriers and facilitators.
Results The search strategy led to a total of 4223 potentially relevant papers, of which 33 met the inclusion criteria. Main perceived adoption factors to m-health at the individual, organizational, and contextual levels were the following: perceived usefulness and ease of use, design and technical concerns, cost, time, privacy and security issues, familiarity with the technology, risk-benefit assessment, and interaction with others (colleagues, patients, and management).
Conclusion This systematic review provides a set of key elements making it possible to understand the challenges and opportunities for m-health utilization by healthcare providers.
Keywords: m-health, healthcare provider, adoption, systematic review, mixed methods
INTRODUCTION
The number of people in the world who own a mobile phone or other portable electronic communication device has grown exponentially during the last decade. The recent advances regarding mobile technologies have enabled mobile devices to perform functions previously not possible with handheld devices. 1 These innovative applications to address health issues have evolved into a new field of eHealth, known as mobile health or m-health.
Although several definitions to m-health have been proposed, none seems to reach consensus in the international literature. For instance, Mirza suggests that m-health “involves the use of mobile technology to enhance health services. The mobile technology can be either a short-distance or long-distance technology, or be device driven.” 2 For its part, the Global Observatory for eHealth of the World Health Organization defines m-health as medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices. 3 Mobile technologies include mobile phones, PDAs, and PDA phones; smartphones; enterprise digital assistants; portable media players, handheld video-game consoles, and handheld and ultra-portable computers such as tablet PCs. These devices have a range of functions from mobile cellular communication using text messages (Short Message Service - SMS), photos and videos (Multimedia Messaging Service - MMS), telephone and internet access, to multimedia playback and software application support.
m-Health interventions are designed to improve healthcare service delivery processes by providing support and services to healthcare providers (such as education, support in diagnosis, or patient management) or target communication between healthcare services and consumers (such as appointment reminders and test result notification) 4 and, thus, changing the traditional modes of information sharing and dissemination. 5 In 2012, there were approximately 40 000 mobile device applications (apps) related to health. 6
m-Health is thus central to the concept of pervasive healthcare where information and resources services can reach anyone, anytime, and anywhere, by removing geographical, temporal, and other barriers. 7 While there is limited scientific evidence supporting the effectiveness of m-health, 4,8 governments and organizations in many jurisdictions have embraced it as the backbone of the informed and empowered patient or “patient 2.0.” 9,10 m-Health also constitutes an affordable option to increase health promotion, disease prevention, provision of care, and monitoring in low-income countries, where pilot projects are rampant. 11
As with other information and communication technologies (ICT) that have entered the healthcare sphere in the past, such as telemedicine or electronic health records, the success of m-health as a tool to support the delivery of healthcare is tributary to its adoption by healthcare providers. 12 While the factors influencing healthcare providers for adopting a new technology such as m-health could be similar to those involved with other ICT applications, there are specific features about m-health that should be considered. First, unlike previous ICT applications in healthcare, m-health is mainly consumer-centered and consumer-driven. 13 Second, m-health interventions can be seen as a patchwork of small-scale pilot projects 11 and most of these interventions work as black boxes with little use of theoretical foundations. 14
Although mobile communication is now part of the everyday life of most human beings, the use of m-health applications to provide health information and care is particularly challenging and calls for specific strategies. The aim of this paper is to synthesize the scientific literature on the factors that could facilitate or limit healthcare provider utilization of m-health in their work.
METHODS
Search Strategy
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis checklist. 15 Covering a period from January 1, 2000 to October 31, 2014, we conducted a systematic literature search on 4 electronic databases (PUBMED, EMBASE, CINHAL, PsychInfo). We also searched the references of included publications to identify additional relevant literature. The search strategy included 3 categories of keywords: m-health, healthcare professionals, and adoption. These keywords should appear in conjunction in the title or abstract of the article. To refer to m-health, the articles either had to include the term “m-health” (and its alternative formulations), or include both the term “health” and one of the following search terms or their variants: handheld computer, mobile phone, smartphone, mobile application, mobile app, cellular phone, mobile device, mobile technology, SMS, or text message. To refer to healthcare professionals, we used the following search terms or their variants: professional, physician, practitioner, provider, resident, clinician, nurse, midwife, health worker, specialist, dentist, pharmacist, dietician, physiotherapist, cardiologist, surgeon, gynaecologist, ophthalmologist, psychiatrist, and optician. Finally, we searched the following themes related to adoption: acceptance, acceptability, utilization, or attitude.
Duplicate citations across databases were identified and excluded using Endnote and a manual revision was done for verification. If a study was reported in more than one publication and presented the same data, we only included the most recent publication. However, if new data were presented in multiple publications describing the same study, all were included.
Inclusion and Exclusion Criteria
We included studies with an abstract in English, French, or Spanish. The studies had to be based on an empirical design, including qualitative, quantitative, or mixed-methods. The articles should have clearly stated the data collection process as well as research methods and measurement tools used. We excluded publications presenting editorials, comments, position papers, and unstructured observations from this review. We included conference proceedings as long as they presented all relevant data. Studies had to provide data on barriers and facilitators to m-health adoption by healthcare professionals in their results or discussion sections to be included. These barriers or facilitators could be related to one or several healthcare professional groups who were using m-health. We excluded studies that focused only on m-health adoption by healthcare students and studies in which there was no clear distinction between healthcare professionals and other groups (e.g., patients, technology providers) regarding m-health adoption factors.
Screening and Data Extraction
One reviewer (P.N.) initially screened all titles and abstracts of references identified through the search strategy and another reviewer (M.P.G.) reviewed the titles and abstracts retained. Then, P.N. and M.P.G. independently reviewed the full text of preselected articles and agreed on their final selection.
Two dyads (P.N. and M.P.G., M.D. and J.P.G.) independently performed data extraction using a validated data extraction grid, developed through previous research related to the classification of barriers and facilitators to information and communication technology adoption by healthcare professionals. 12 This generic data extraction grid has been adapted and validated to classify reported barriers and facilitators to the adoption of electronic health records and electronic prescription. 16,17 The grid was developed using both inductive and deductive methods, and combines several relevant concepts from established theoretical frameworks, notably the Technology Acceptance Model (TAM) and the Diffusion of Innovations Theory. 18,19 Emergent categories were also added during the review process. We populated the data extraction grid in Microsoft Excel software 2010 .
Data Synthesis and Analysis
The reviewers identified sections of the publications that presented a relevant barrier or facilitator to adoption of m-health from the healthcare professionals’ perspective and coded them according to the categories proposed in the grid. Then, we grouped the extracted data into four main categories of adoption factors and each category was decomposed into specific factors. We also extracted data regarding: year of publication, country, and study design (quantitative, qualitative, or mixed-methods), theoretical framework (present or absent), type of participants, care setting, technology used, objectives of the study, data collection methods, and main findings. Quality of studies was not considered in these analyses.
RESULTS
Included Studies
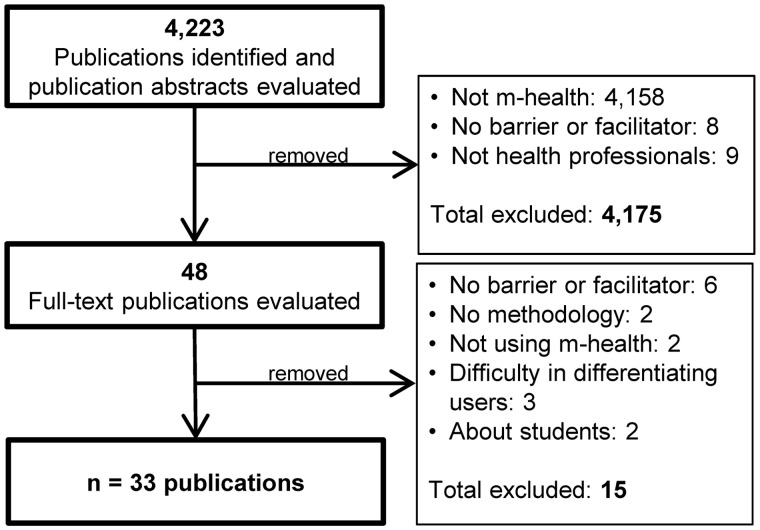
In total, we identified 4223 references from the databases, of which we kept 48 publications for a full-text review. We excluded 15 publications because they did not meet the inclusion criteria: 2 were about m-health use by students 20,21 ; 3 did not clearly differentiate healthcare professionals’ opinions from those of other groups involved in the study 2,22,23 ; 2 presented opinions from professionals who were not using m-health 24,25 ; 6 were not about adoption factors 26–31 ; and 2 did not describe the methodology used. 5,32 Thus, 33 publications were selected in the final review. 1,7,33–63 The study selection flow diagram is presented in Figure 1 .
Figure 1:
– Study selection flow diagram.
Characteristics of Included Studies
The table summarizing the characteristics of included publications can be found in Supplementary File S1 . The included studies were published between 2005 and 2014. Interestingly, more than half of them (57.6%) were published during the last 3 years. 33–36,41,42,44,47,49,51–53,56,58-–63 Few theoretical frameworks were used in the studies. Indeed, only 8 (24.2%) publications mentioned the use of a theoretical framework: the TAM and its updated version (TAM2), 1,7,37,51,62 the Diffusion of Innovations Theory, 1,51,61 the Information System Success Model, 38,47 and the Technology Readiness Index. 62
The studies about m-health adoption were conducted in various countries. More than half of the studies took place in the Americas (n = 18, 54.5%). Among these, 10 were conducted in Canada, 7,43,44,53–59 7 in the United States, 1,40,41,46,48,51,63 and 1 in Guatemala. 42 Six publications (18.2%) were from European countries, including the United Kingdom, 45,49,50 Ireland, 39 Portugal, 46 and Finland. 38 Five studies (15.2%) were from Asia (Taiwan, 37,61,62 Japan, 47 and India 60 ), 4 (12.1%) were conducted in Africa, each representing a different country (Ethiopia, 33 South Africa, 34 Botswana, 35 and Uganda 36 ) and 1 was from Australia. 52
The majority of studies used a quantitative research design (n = 19, 57.6%). 1,7,33,37,39–43,46–49,51,57,60–63 Six studies (18.2%) 34,38,44,53,55,56 employed a qualitative design through the use of focus groups, 34,55 interviews, 38,44,53,56 and written reflections 55 for data collection methods. A mixed methods design was used in 8 publications (24.2%). 35,36,45,50,52,54,58,59
The types of m-health technology studied were the following: a smartphone or mobile phone (n = 15), 1,34–36,38,39,42,44,48–51,56,57,59,60 a PDA (n = 5), 7,33,37,43,55 a remote monitoring system (n = 5), 45,47,52–54 a tablet computer (n = 4), 55,58,59,63 a mobile electronic medical record system (n = 2), 61,62 text messaging (n = 2), 40–42 and mobile technologies in general (n = 1). 46
The healthcare professionals who participated in the included studies were physicians, residents, nurses, health workers, pharmacists, and other types of providers (such as social workers and occupational therapists). Fewer than half of the studies (n = 15, 45.5%) exclusively studied physicians or residents, 33,35,38–40,43,46–49,51,52,58,59,63 7 (21.2%) involved nurses only, 1,7,37,45,55,61,62 and 3 (9.1%) concerned health workers exclusively. 34,42,60 The other publications (n = 8, 24.2%) had various professionals participating in the study. 36,41,44,50,53,54,56,57
Overview of m-health Adoption Factors
In total, 179 elements were identified as barriers to or facilitators for m-health adoption and were classified in the different categories of factors from the extraction grid. Ninety-eight (54.7%) of these elements were classified as facilitators for m-health adoption and 81 (45.3%), as barriers.
The complete list of factors with selected quotes for factors with 4 elements or more can be found in Table 1 . We also present an analysis of the factors from studies conducted in developing countries at the end of the section.
Table 1:
List of factors extracted from the literature and selected quotes for the main factors (classified by barriers and facilitators)
| Factor | No. of Barriers | No. of Facilitators | Total | |
|---|---|---|---|---|
| 1. Factors related to mHealth characteristics | 33 | 40 | 73 | |
| 1.1 | Design and technical concerns | 7 | 2 | 9 |
| “Participants also commented on the screen size of most smartphones and technical limitations of most mobile devices (e.g., touchscreen keyboards, no printing, unable to view certain websites or file formats).” (B) 59 | ||||
| 1.2.1 | Perceived usefulness | 3 | 18 | 21 |
| “I would use an app with clinical guidelines that are hospital specific, including management advice for common conditions. This would be very useful on a busy ward because with only a few computers it is difficult to get a monitor when they are needed for urgent clinical work” (F) 49 | ||||
| 1.2.2 | Compatibility (with work process) | 2 | 2 | |
| 1.2.3 | Perceived ease of use | 3 | 7 | 10 |
| “The ease of use and portability of the system were also found to be benefits of the mobile phone-based telemonitoring system” (F) 53 | ||||
| 1.2.5 | Observability (observance, control, verification) | 3 | 3 | |
| 1.3 | System reliability or dependability | 1 | 1 | |
| 1.4 | Interoperability | 1 | 4 | 5 |
| “The importance of staying connected and up to date with a central EPR [electronic patient record] through the PDA [personal digital assistant] was emphasized by 11 users.” (F) 43 | ||||
| 1.5.1 | Privacy and security concerns | 5 | 5 | |
| “Qualitative analysis revealed that use of smartphones while providing patient care created risks to patient privacy” (B) 48 | ||||
| 1.5.2 | Medicolegal issues | 2 | 2 | |
| 1.7.2 | Satisfaction about content available (completeness) | 1 | 1 | |
| 1.7.3 | Content appropriate for the users (relevance) | 1 | 2 | 3 |
| 1.7.4 | Accuracy (improved OR errors, omissions, update) | 2 | 1 | 3 |
| 1.7.5 | Quality standard | 1 | 1 | 2 |
| 1.9 | Cost issues | 5 | 5 | |
| “The clinicians and patients indicated cost was one of the main barriers to implementing the telemonitoring system on a long-term basis, although the cost to deliver this mobile phone service is projected to be much lower than conventional telemonitoring.” (B) 53 | ||||
| 1.13 | Cell phone accuracy | 1 | 1 | |
| 2. Individual factors: knowledge, attitude, and socio-demographic characteristics | 16 | 33 | 49 | |
| 2.1.1 | Awareness of the objectives and/or existence of mHealth | 1 | 1 | |
| 2.1.2 | Familiarity, ability with mHealth | 3 | 3 | 6 |
| “Providers and staff in this study were also supportive of text message reminder/recall, which is important given their familiarity with this system, particularly downstream effects following deployment.” (F) 41 | ||||
| 2.1.3 | Familiarity with technologies in general | 1 | 4 | 5 |
| “Doctors owning handhelds alone or in combination with laptops used them more frequently than those using laptops alone.” (F) 46 | ||||
| 2.2.1 | Risk-benefit assessment (perception) | 1 | 6 | 7 |
| “Physicians from a wide range of clinical expertise most valued perceived value as a mediator of the effects exercised by both overall quality and net benefits over intention to use mobile diabetes monitoring.” (F) 47 | ||||
| 2.2.3 | Autonomy | 2 | 2 | |
| 2.2.4 | Impact on clinical uncertainty | 1 | 1 | |
| 2.2.5 | Time issues | 3 | 7 | 10 |
| “The main reason for this improved efficiency was the perceived decrease in wait times with the BlackBerry phone calling and emailing capabilities when compared to the traditional paging system.” (F) 56 | ||||
| 2.2.6 | Outcome expectancy (leads or not to desired outcome) | 1 | 1 | 2 |
| 2.2.7 | Agreement with mHealth (Welcoming/resistant) | 4 | 5 | 9 |
| “32 (76,2%) of users do it on their own initiative rather than as part of the program/services/clinic requirement. Most PDA use is self-motivated in nature, with little to no guidance, training, or report available at the organizational level.” (F) 43 | ||||
| 2.2.8 | Self-efficacy (belief in one’s competence to use mHealth) | 1 | 2 | 3 |
| 2.2.9 | Impact on professional security | 1 | 1 | |
| 2.2.10 | Voluntary ownership | 1 | 1 | |
| 2.3.3 | Experience | 1 | 1 | |
| 3. External Factors: Human environment | 12 | 7 | 19 | |
| 3.1.1 | Patients’ attitudes and preferences towards mHealth | 2 | 1 | 3 |
| 3.1.2 | Patient and health professional interaction | 5 | 4 | 9 |
| “Three of the respondents who like to use full-size computer saw using the mobile as the most disturbing way of information retrieval during patient contacts.” (B) 38 | ||||
| 3.1.3 | Applicability to the characteristics of patients | 1 | 1 | |
| 3.1.4 | Other factors associated with patients | 1 | 1 | 2 |
| 3.2.1 | Attitude of colleagues about mHealth | 1 | 1 | |
| 3.2.2 | Support and promotion of mHealth by colleagues | 1 | 1 | |
| 3.2.3 | Other factors associated with peers | 2 | 2 | |
| 4. External Factors: Organizational Environment | 20 | 18 | 38 | |
| 4.1 | Internal environment | 2 | 2 | |
| 4.1.1.4 | Physician salary status and reimbursement | 1 | 1 | |
| 4.1.2.1 | Lack of time and workload | 3 | 3 | |
| 4.1.2.2 | Work flexibility | 1 | 2 | 3 |
| 4.1.2.3 | Relations among colleagues | 3 | 3 | 6 |
| “Similarly, nurses, social workers, pharmacists and therapist noted the less intrusive nature of the emails and appreciated the direct relay of information to physicians instead of waiting for a callback to explain the purpose of the page.” (F) 44 | ||||
| 4.1.2.5 | Additional tasks | 1 | 1 | |
| 4.1.4.1 | Resources available | 2 | 2 | |
| 4.1.4.2 | Materials resources (access to mHealth) | 1 | 1 | |
| 4.1.4.3 | Human resources (IT support, other) | 3 | 3 | |
| 4.1.5.1 | Training | 2 | 2 | 4 |
| “24 non-users cited the need for initial training and 6 other non-users who stopped using PDAs gave as reasons a lack of training/support.” (B) 43 | ||||
| 4.1.5.3 | Management (strategic plan to implement mHealth) | 2 | 2 | 4 |
| “As all the messages sent via the online paging system were delivered to the Team Smartphone, many social workers, pharmacists and therapists expressed uncertainties as to whether the most responsible physician with whom they wished to communicate actually received their intended messages.” (B) 44 | ||||
| 4.1.5.4 | Communication and collaboration effort | 2 | 2 | |
| 4.1.5.9 | Readiness | 1 | 1 | 2 |
| 4.1.5.10 | Choice of the mHealth system | 1 | 1 | |
| 4.2 | External environment | 2 | 2 | |
| 4.2.3 | Health care policies and socio-political context | 1 | 1 | |
| Grand total: | 81 | 98 | 179 | |
Factors Related to m-health Characteristics
A total of 73 elements (40.8%) pertain to the category “Factors related to the m-health characteristics,” with 33 of them identified as barriers and 40 as facilitators. The most recurrent adoption factor was perceived usefulness, with 21 extracted elements. 1,7,33,34,36–39,42–46,49,51–54,57,58,60 It was seen more often as a facilitator for m-health adoption (in 18 studies 1,7,33,34,36–39,42,44,45,49,51–54,58,60 ) than as a barrier (in 3 studies 43,46,57 ). Perceived usefulness is defined as an individual’s perception that the utilization of a particular mobile device will be advantageous in an organizational setting over a current practice. 19
Perceived ease of use was another frequently mentioned factor (n = 10). 7,37,43,53,54,56,58,60,61 Perceived ease of use is the perception by an individual that the utilization of a mobile technology will be relatively painless and effortless. 19 Therefore, it was important for the professionals to perceive the usefulness and ease of use of the technology in their working environment; otherwise there would be less incentive to use them. Design and technical concern were also mentioned on 9 occasions, 43,53,55,58,59 and were perceived mainly as barrier (7 as a barrier 43,55,58,59 and 2 as a facilitator 53,58 ). Main issues raised were limited features, 43,58,59 size, 55,58,59 and complexity of using some features. 58,59
Other factors related to m-health characteristics were interoperability (integration with other systems), 1,34,40,43,51 cost issues, 43,48–50,53 and privacy and security concerns 36,42,48,55 (all of them extracted 5 times). Both cost issues and privacy and security concerns were seen exclusively as barriers to the adoption of m-health. Indeed, professionals were worried about the security and confidentiality of the data contained in and transferred through these technologies, as well as potential device theft. Additionally, cost of the mobile technology and smartphone applications were perceived as barriers to m-health adoption. Other factors identified in this category were compatibility with the work process, 38,61 observability (observance, control, verification), 1,51,61 system reliability (ability to perform its functions), 55 medico-legal issues, 50,54 availability of the content, 38 appropriate content, 45,58,60 accuracy of the data, 52–54 quality standards, 36,48 and cell phone accuracy. 41
Individual Factors: Knowledge, Attitude, and Socio-demographic Characteristics
Individual factors represented 49 (27.4%) of the extracted elements. There were twice as many facilitators as barriers in this category (32 and 16, respectively). The most common factor identified was time issues (n = 10). 39,44,45,48,49,52,56,57,59 Generally, professionals thought that m-health saved time by allowing quicker contact and communication than other technologies. 39,48,49,52,56,57 However, some pointed out that m-health may be time consuming by being disruptive to their workflow. 44,45,59 Agreement with the technology (n = 9) 37,40,42,43,46,60,62 was perceived either as a facilitator or a barrier; the agreement being dependent on other factors, such as interest, motivation, and comfort with the technology.
Risk-benefit assessment was also mentioned seven times. 39,44,47,48,52,53 Even if one comment underlined that m-health may make it difficult to communicate complex issues to their patients, 44 professionals believed that m-health could improve patient care. 39,44,47,48,52,53 Familiarity and ability with m-health (n = 6) 40-43,51,59 and with technologies in general (n = 5) 33,46,50,62 were other important factors of this category. Finally, professional autonomy, 38,55 clinical uncertainty, 53 outcome expectancy, 50,56 self-efficacy, 35,55 professional security, 36 awareness of existence of m-health, 59 professional experience, 61 and voluntary ownership of m-health 46 were other factors identified in this category.
External Factors: Human Environment
External factors related to the human environment represented 19 of the elements identified in the review (10.6%). Twelve of the factors extracted were barriers and 7 were facilitators. Factors related to patients were underlined more often than factors related to colleagues. Indeed, the 2 most recurrent factors of this category concern the patient–professional interaction (n = 9) 38,48–50,52,63 and patients’ attitude and preferences towards m-health (n = 3). 34,42,49 Professionals believed that the use of m-health, especially in the case of smartphones, could be disruptive during visits 38,48–50,63 and could be misinterpreted as checking email or SMS. 38,49 Others believed that it could facilitate the relationship with their patients by having a new means of communication with them. 38,42,50,52,63 Other factors related to patients were applicability to the patients’ characteristics, 54 patients’ perception of the professional, 55 and the professionals’ belief that patients gained better knowledge of themselves. 52 There were few mentions of factors related to peers, such as the attitude of colleagues about m-health, 49 their support and promotion of m-health, 35 and miscommunication while using m-health. 56
External Factors: Organizational Environment
The last category includes external factors found in the organizational environment and accounts for 21.2% (n = 38) of the elements extracted in this review. Barriers and facilitators were spread equally, totaling 20 and 18 factors, respectively. In this category, the most common factor was relations among colleagues. 44,55,57 One of the perceived barriers was that m-health technologies, by allowing a more direct relay of the information among colleagues, also increased the potential to be disturbed in their workflow. Management support was also seen as an important facilitator in this category (n = 4). 1,44,46,51 In fact, good support from management may facilitate healthcare professional adoption of m-health. 1,51 However, professionals raised concerns about poor management of information and the imposition of the devices upon professionals who may not want to use them. 44,46
Availability 59,63 and access to material 42 and human resources, 41,43,54 as well as training 35,43,45,63 were also seen as adoption factors related to the organization. In addition, some factors related to healthcare professionals’ work environment could be seen as barriers or facilitators to m-health adoption. In fact, issues related to time and workload, 40,53,54 work flexibility (by the increased mobility and management issue between work and home), 55,57 additional tasks, 36 reimbursement of tasks related to m-health, 54 and communication in the workplace 34,36 were factors raised as potential barriers to m-health adoption. Other factors mentioned were workplace readiness to implement m-health, 41,54 choice of the device used, 46 and healthcare system support. 54 Finally, some studies described factors only in terms of internal environment 1,51 and external environment, 1,51 without providing more details.
Factors Related to Developing Countries
We also analyzed extracted data related to the 6 studies that took place in developing countries (Botswana, 35 Ethiopia, 33 Guatemala, 42 India, 60 South Africa, 34 and Uganda 36 ). In total, 25 factors were identified in these studies (20 facilitators and 5 barriers). The most recurrent factor identified for the 6 studies was perceived usefulness with 5 elements (all facilitators), 33,34,36,42,60 which is comparable to the results from studies in developed countries. However, these studies identified 5 factors that were not mentioned in other studies: professional security, 36 support and promotion of m-health by colleagues, 35 additional tasks, 36 and material resources 42 as well as communication and collaboration effort. 34,36
Other factors identified from these studies related to functionalities of m-health (ease of use, 60 interoperability, 34 relevance, 60 and quality 36 ), privacy and security issues, 36,42 familiarity, 42 and self-perceived competency 35 with m-health, familiarity with technologies, 33 agreement with m-health, 42,60 training, 35 patients attitude toward m-health, 34,42 and their interaction with professionals. 35
DISCUSSION
This review aimed to summarize the literature on factors that could facilitate or restrain health professional use of m-health in their work. These professionals, like many other people, possess mobile phones or other portable electronic communication devices. However, this does not mean that they use mobile devices for their work. Given the considerable attention that m-health receives globally, it seemed important to identify the factors that could facilitate or limit its adoption by healthcare professionals.
The main findings of this review highlight that several factors are associated with m-health adoption at the individual, organizational, and contextual levels. Usefulness and ease of use of the technology were seen as two of the most important factors with respect to the adoption of m-health in the included publications. Although those two TAM factors 19 were included in the extraction grid and are common in studies explicitly based on the TAM, 1,7,37,51,62 they were also frequently mentioned as being critical for healthcare professional adoption of m-health in publications not explicitly using the TAM.
In contrast to a recent review suggesting that m-health could constitute an affordable option for health promotion, 49 our findings show that healthcare professionals think cost issues could limit their adoption of m-health. 43,48–50,53 In fact, all elements identified that were related to costs were exclusively seen as barriers. More particularly, long-term costs of the technology as well as costs of the device and applications were mentioned in the studies.
The role of m-health to support patient empowerment has been mentioned in the literature. 38,48 This benefit was also perceived in the reviewed studies. In fact, healthcare professionals believed that patients gained better knowledge of themselves, 52 and that their relationship with them was improved with the use of m-health. 38,42,50,52,63 Additionally, the results show that healthcare providers agree that m-health could improve patient care, 39,44,47,48,52,53 supporting the idea of a consumer-centered approach promoted by the use of ICT applications. 49
As such, m-health is perceived as a technology that can reach anyone, anytime, and anywhere. While the findings of our review support this general idea, it was not necessarily seen as a benefit. Professionals in fact expressed the belief that m-health brought quicker contact and communication 39,48,49,52,56,57 and improved their access to colleagues, 44,55,57 which could constitute benefits. Conversely, the increased workload 36,50,53–55 and the disturbed workflow by colleagues 55,57 were seen as barriers to their adoption of m-health.
Other important adoption factors that were highlighted in this review include interoperability 1,34,40,43,51 and familiarity with the technology. 33,40–43,46,50,51,59 These two factors were also identified in other reviews on ICT adoption among healthcare professionals. 1,44,46 Additionally, support of the technology, through management, 1,44,46,51 training, 35,43,45,63 and as well as material and human resources, 41–43,54,59,63 were also identified in this review.
We also assessed the results regarding studies conducted in developing countries. 33–36,42,60 While usefulness was also identified as the main factor that may facilitate use of m-health by healthcare providers, these studies were the only ones highlighting factors related to the interrelation between colleagues (promotion of m-health and collaboration effort), 34–36 job security, 36 additional tasks that may arise while using m-health, 36 and the need of accessibility to phones and electricity in order to use m-health. 42
Limitations
While providing an exhaustive synthesis of the current knowledge on healthcare professional m-health adoption factors, this review has some limitations. First, we used a generic grid of adoption factors as the conceptual framework for classifying elements identified as barriers and facilitators to m-health adoption from the studies included in this review. As such, we relabeled some of the original factors in order for them to fit within our conceptual framework. We acknowledge that the use of other theoretical frameworks or models could have uncovered other dimensions of the adoption of m-health. However, we think that the framework used is comprehensive and well suited to present adoption factors of m-health perceived by health professionals as it is based on extensive theoretical and empirical research.
Second, this review only considered data that were presented in published studies, and no additional contacts were made with the authors to receive additional information or to validate our classification. Thus, it is likely that other m-health adoption factors could have been missed.
Third, we conducted a mixed-method systematic review, and we combined data from qualitative and quantitative studies indistinctively in our synthesis. The use of other synthesis approaches, such as meta-narrative synthesis or realist review, could have brought a deeper analysis of m-health adoption in healthcare. Future reviews using these approaches could be guided by the RAMESES reporting standards. 64
Finally, we only conducted literature searches in four bibliographic databases, but we carefully checked references of included studies as well as articles citing those studies in order to identify other potentially relevant publications. Gray literature searches could have enabled the identification of other relevant studies.
CONCLUSION
The entire issue of m-health is attracting a great deal of attention worldwide because it presents a unique way to provide information and resources to healthcare professionals and patients alike, and may be a promising tool to support healthcare. The findings from this systematic review provide a common ground, making it possible to better understand the challenges and opportunities related to m-health utilization by healthcare providers. While some of the barriers and facilitators to m-health adoption are similar to those identified in systematic reviews about other ICT applications, this review has enabled us to identify factors that are specific to m-health.
Supplementary Material
Acknowledgments
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
M.P.G. designed the systematic review. P.N. screened titles and abstracts of references identified in the databases and M.P.G. reviewed the selection. M.P.G. and P.N. reviewed the full text articles. All authors contributed to data extraction and J.P.G. synthetized the data. All authors participated in the drafting of the manuscript and review of the content. All authors approved the final version of the review.
SUPPLEMENTARY MATERIAL
Supplementary material is available online at http://jamia.oxfordjournals.org/ .
REFERENCES
- 1. Putzer GJ, Park Y . The effects of innovation factors on smartphone adoption among nurses in community hospitals . Perspect Health Inf Manag. 2010. ; 7 : 1b . [PMC free article] [PubMed] [Google Scholar]
- 2. Mirza F, Norris T . Opportunities and barriers for mobile health in New Zealand . Stud Health Technol Inform. 2007. ; 129 ( Pt1 ): 102 – 106 . [PubMed] [Google Scholar]
- 3. World Health Organization . mHealth: new horizons for health through mobile technologies - Based on the findings of the second global survey on eHealth (Global Observatory for eHealth series) . Geneva, Switzerland: ; 2011. . [Google Scholar]
- 4. Free C, Phillips G, Watson L, et al. . The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis . PLoS Med. 2013. ; 10 ( 1 ): e1001363 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elwood D, Diamond MC, Heckman J, et al. . Mobile health: exploring attitudes among physical medicine and rehabilitation physicians toward this emerging element of health delivery . PM&R. 2011. ; 3 ( 7 ): 678 – 680 . [DOI] [PubMed] [Google Scholar]
- 6. Boulos MN, Brewer AC, Karimkhani C, et al. . Mobile medical and health apps: state of the art, concerns, regulatory control and certification . Online J Public Health Inform . 2014. ; 5 ( 3 ): e229 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang H, Cocosila M, Archer N . Factors of adoption of mobile information technology by homecare nurses: a technology acceptance model 2 approach . Comput Inform Nurs. 2010. ; 28 ( 1 ): 49 – 56 . [DOI] [PubMed] [Google Scholar]
- 8. Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S . Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa . BMC Public Health. 2014. ; 14 ( 1 ): 188 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ricciardi L, Mostashari F, Murphy J, et al. . A national action plan to support consumer engagement via e-health . Health Aff . 2013. ; 32 ( 2 ): 376 – 384 . [DOI] [PubMed] [Google Scholar]
- 10. Bos L, Marsh A, Carroll D, et al. . Patient 2.0 Empowerment . In: Arabnia HR, Marsh A , eds. International Conference on Semantic Web & Web Services . Las Vegas, NV: : Springer; ; 2008. : 164 – 167 . [Google Scholar]
- 11. Heerden AV, Tomlinson M, Swartz L . Point of care in your pocket: a research agenda for the field of m-health . Bull World Health Organ. 2012. ; 90 ( 5 ): 393 – 394 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gagnon MP, Desmartis M, Labrecque M, et al. . Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals . J Med Sys . 2012. ; 36 ( 1 ): 241 – 277 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Akter S, Ray P . mHealth - an Ultimate Platform to Serve the Unserved . Yearb Med Inform . 2010. ; 5 : 94 – 100 . [PubMed] [Google Scholar]
- 14. Tomlinson M, Rotheram-Borus MJ, Swartz L, et al. . Scaling Up mHealth: where is the evidence? PLoS Med . 2013. ; 10 ( 2 ): e1001382 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement . PLoS Med . 2009. ; 6 ( 7 ): e1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McGinn CA, Grenier S, Duplantie J, et al. . Comparison of user groups' perspectives of barriers and facilitators to implementing electronic health records: a systematic review . BMC Med . 2011. ; 9 : 46 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gagnon MP, Nsangou ER, Payne-Gagnon J, Grenier S, Sicotte C . Barriers and facilitators to implementing electronic prescription: a systematic review of user groups' perceptions . J Am Med Inform Assoc . 2014. ; 21 ( 3 ): 535 – 541 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rogers EM . The Diffusion of Innovations . New York: : The Free Press; ; 1995. . [Google Scholar]
- 19. Davis FD . Perceived usefulness, perceived ease of use, and user acceptance of information technology . MIS Q. 1989. ; 13 ( 3 ): 319 – 340 . [Google Scholar]
- 20. Wallace S, Clark M, White J . ‘It's on my iPhone': attitudes to the use of mobile computing devices in medical education, a mixed-methods study . BMJ Open. 2012. ; 2 ( 4 ): e001099 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wittmann-Price RA, Kennedy LD, Godwin C . Use of personal phones by senior nursing students to access health care information during clinical education: staff nurses' and students' perceptions . J Nurs Educ. 2012. ; 51 ( 11 ): 642 – 646 . [DOI] [PubMed] [Google Scholar]
- 22. Cleland J, Caldow J, Ryan D . A qualitative study of the attitudes of patients and staff to the use of mobile phone technology for recording and gathering asthma data . J Telemed Telecare. 2007. ; 13 ( 2 ): 85 – 89 . [DOI] [PubMed] [Google Scholar]
- 23. Pinnock H, Slack R, Pagliari C, et al. . Understanding the potential role of mobile phone-based monitoring on asthma self-management: qualitative study . Clin Exp Allergy. 2007. ; 37 ( 5 ): 794 – 802 . [DOI] [PubMed] [Google Scholar]
- 24. Baranoski AS, Meuser E, Hardy H, et al. . Patient and provider perspectives on cellular phone-based technology to improve HIV treatment adherence . AIDS Care. 2014. ; 26 ( 1 ): 26 – 32 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bostock Y, Hanley J, McGown D, et al. . The acceptability to patients and professionals of remote blood pressure monitoring using mobile phones . Prim Health Care Res Dev. 2009. ; 10 ( 4 ): 299 – 308 . [Google Scholar]
- 26. Franko OI, Tirrell TF . Smartphone app use among medical providers in ACGME training programs . J Med Syst. 2012. ; 36 ( 5 ): 3135 – 3139 . [DOI] [PubMed] [Google Scholar]
- 27. Soni RK, Palevsky PM . The smartphone in nephrology: preliminary survey on current trends and perceived needs . Am J Kidney Dis. 2013. ; 61 ( 4 ): A91 . [Google Scholar]
- 28. Tanaka PP, Hawrylyshyn K, Macario A . Use of tablet (iPad ® ) as a tool for teaching anesthesiology in an orthopedic rotation . Rev Bras Anestesiol. 2012. ; 62 ( 2 ): 214 – 222 . [DOI] [PubMed] [Google Scholar]
- 29. Handler SM, Boyce RD, Ligons FM, et al. . Use and perceived benefits of mobile devices by physicians in preventing adverse drug events in the nursing home . J Am Med Dir Assoc. 2013. ; 14 ( 12 ): 906 – 910 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Velez O, Okyere PB, Kanter AS, Bakken S . A usability study of a mobile health application for rural Ghanaian midwives . J Midwifery Womens Health. 2014. ; 59 ( 2 ): 184 – 191 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Palazuelos D, Diallo AB, Palazuelos L, et al. . User perceptions of an mHealth medicine dosing tool for community health workers . JMIR Mhealth Uhealth. 2013. ; 1 ( 1 ): e2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hensel BK, Fontelo P . Physician attitudes toward SMS/Text messaging in medicine . AMIA Annu Symp Proc. 2008. : 965 . [PubMed] [Google Scholar]
- 33. Ben-Yakov M, Hunchak C, Landes M . Personal digital assistant use by emergency medicine residents in ethiopia: An educational pilot on behalf of the TAAAC(EM) collaboration . Can J Emerg Med. 2013. ; 15 : S77 . [Google Scholar]
- 34. Chaiyachati KH, Loveday M, Lorenz S, et al. . A pilot study of an mHealth application for healthcare workers: poor uptake despite high reported acceptability at a rural South African community-based MDR-TB treatment program . PLoS One. 2013. ; 8 ( 5 ): e64662 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chang AY, Ghose S, Littman-Quinn R, et al. . Use of mobile learning by resident physicians in Botswana . Telemed J E Health. 2012. ; 18 ( 1 ): 11 – 13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chang LW, Njie-Carr V, Kalenge S, et al. . Perceptions and acceptability of mHealth interventions for improving patient care at a community-based HIV/AIDS clinic in Uganda: a mixed methods study . AIDS Care. 2013. ; 25 ( 7 ): 874 – 880 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chang P, Hsu CL, Lan CF . Is PDA good for complex documentation in healthcare? Stud Health Technol Inform . 2009. ; 146 : 115 – 120 . [PubMed] [Google Scholar]
- 38. Harkke V . Impacts of physicians' usage of a mobile information system . Int J Electron Healthc. 2006. ; 2 ( 4 ): 345 – 361 . [DOI] [PubMed] [Google Scholar]
- 39. Haroon M, Yasin F, Eckel R, et al. . Perceptions and attitudes of hospital staff toward paging system and the use of mobile phones . Int J Technol Assess Health Care. 2010. ; 26 ( 4 ): 377 – 381 . [DOI] [PubMed] [Google Scholar]
- 40. Hart T, Ahlers-Schmidt CR, Chesser A, et al. . Physician impressions of using text message technology to increase vaccination compliance . Telemed J E Health. 2011. ; 17 ( 6 ): 427 – 430 . [DOI] [PubMed] [Google Scholar]
- 41. Hofstetter AM, Vargas CY, Kennedy A, et al. . Parental and provider preferences and concerns regarding text message reminder/recall for early childhood vaccinations . Prev Med. 2013. ; 57 ( 2 ): 75 – 80 . [DOI] [PubMed] [Google Scholar]
- 42. Irwin TE, Nordstrom SK, Pyra M . Acceptability of mobile phone technology for tracking cervical cancer in rural Guatemala . Int J Gynaecol Obstet. 2012. ; 119 : S375 – S376 . [Google Scholar]
- 43. Lau F, Yang J, Pereira J, et al. . A survey of PDA use by palliative medicine practitioners . J Palliat Care. 2006. ; 22 ( 4 ): 267 – 274 . [PubMed] [Google Scholar]
- 44. Lo V, Wu RC, Morra D, et al. . The use of smartphones in general and internal medicine units: a boon or a bane to the promotion of interprofessional collaboration? J Interprof Care . 2012 ; 26 ( 4 ): 276 – 282 . [DOI] [PubMed] [Google Scholar]
- 45. Maguire R, McCann L, Miller M, et al. . Nurse's perceptions and experiences of using of a mobile-phone-based Advanced Symptom Management System (ASyMS) to monitor and manage chemotherapy-related toxicity . Eur J Oncol Nurs. 2008. ; 12 ( 4 ): 380 – 386 . [DOI] [PubMed] [Google Scholar]
- 46. Martins HM, Jones MR . What explains doctors' usage of Mobile Information and Communication Technologies? A comparison of US and Portuguese hospitals . AMIA Annu Symp Proc. 2005. : 495 – 499 . [PMC free article] [PubMed] [Google Scholar]
- 47. Okazaki S, Castaneda JA, Sanz S, et al. . Factors affecting mobile diabetes monitoring adoption among physicians: questionnaire study and path model . J Med Internet Res. 2012. ; 14 ( 6 ): e183 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Patel M, Dine J, Asch D . Resident use of smartphones while providing patient care . J Gen Intern Med. 2011. ; 26 : S103 – S104 . [Google Scholar]
- 49. Payne KB, Wharrad H, Watts K . Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey . BMC Med Inform Decis Mak. 2012. ; 12 : 121 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pinnock H, Slack R, Pagliari C, et al. . Professional and patient attitudes to using mobile phone technology to monitor asthma: questionnaire survey . Prim Care Respir J. 2006. ; 15 ( 4 ): 237 – 245 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Putzer GJ, Park Y . Are physicians likely to adopt emerging mobile technologies? Attitudes and innovation factors affecting smartphone use in the southeastern United States . Perspect Health Inf Manag. 2012. ; 9 : 1b . [PMC free article] [PubMed] [Google Scholar]
- 52. Reid SC, Kauer SD, Khor AS, et al. . Using a mobile phone application in youth mental health: An evaluation study . Aust Fam Physician. 2012. ; 41 ( 9 ): 711 – 714 . [PubMed] [Google Scholar]
- 53. Seto E, Leonard KJ, Cafazzo JA, et al. . Perceptions and experiences of heart failure patients and clinicians on the use of mobile phone-based telemonitoring . J Med Internet Res. 2012. ; 14 ( 1 ): 180 – 189 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Seto E, Leonard KJ, Masino C, et al. . Attitudes of heart failure patients and health care providers towards mobile phone-based remote monitoring . J Med Internet Res. 2010. ; 12 ( 4 ): e55 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Valaitis RK, O'Mara LM . Public health nurses' perceptions of mobile computing in a school program . Comput Inform Nurs. 2005. ; 23 ( 3 ): 153 – 160 . [DOI] [PubMed] [Google Scholar]
- 56. Wilson C, Wu R, Lo V, et al. . Effects of smartphones on pharmacist-physician clinical communication . J Pharm Technol. 2012. ; 28 ( 6 ): 234 – 242 . [Google Scholar]
- 57. Wu RC, Morra D, Quan S, et al. . The use of smartphones for clinical communication on internal medicine wards . J Hosp Med. 2010. ; 5 ( 9 ): 553 – 559 . [DOI] [PubMed] [Google Scholar]
- 58. Archibald D, Macdonald CJ, Plante J, et al. . Residents' and preceptors' perceptions of the use of the iPad for clinical teaching in a family medicine residency program . BMC Med Educ. 2014. ; 14 : 174 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Boruff JT, Storie D . Mobile devices in medicine: a survey of how medical students, residents, and faculty use smartphones and other mobile devices to find information . J Med Libr Assoc. 2014. ; 102 ( 1 ): 22 – 30 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gautham M, Iyengar MS, Johnson CW . Mobile phone-based clinical guidance for rural health providers in India . Health Informatics J . 2014. ; March (online first) . [DOI] [PubMed] [Google Scholar]
- 61. Hsu SC, Liu CF, Weng RH, et al. . Factors influencing nurses' intentions toward the use of mobile electronic medical records . Comput Inform Nurs. 2013. ; 31 ( 3 ): 124 – 132 . [DOI] [PubMed] [Google Scholar]
- 62. Kuo KM, Liu CF, Ma CC . An investigation of the effect of nurses' technology readiness on the acceptance of mobile electronic medical record systems . BMC Med Inform Decis Mak. 2013. ; 13 : 88 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sclafani J, Tirrell TF, Franko OI . Mobile tablet use among academic physicians and trainees . J Med Syst. 2013. ; 37 ( 1 ): 9903 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wong G, Greenhalgh T, Westhorp G, et al. . RAMESES publication standards: meta-narrative reviews . BMC Med . 2013. ; 11 : 20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.