Abstract
Background and Aims:
Paediatric airway, because of its consistent anatomical differences from that of an adult, often encounters difficulty in aligning the line of sight with the laryngeal inlet during intubation. Paediatric videolaryngoscopes (VLs), by obviating the need for aligning the line of sight with the glottis, offer several advantages over direct laryngoscopy. Therefore, this study aimed to compare the recently introduced paediatric King Vision™ VL (KVL) and the direct laryngoscope with Macintosh blade for elective tracheal intubation in infants of age <1 year.
Methods:
Seventy-eight infants of American Society of Anesthesiologists physical status 1 and 2, scheduled for elective surgery, were enrolled for this prospective randomised clinical trial and randomised into either of the two groups – Group K and Group C, where the infants were intubated using size 1 King Vision or direct laryngoscope with Macintosh blade. The primary objective of this study was the time taken for intubation and the first-attempt intubation success rate.
Results:
Time to intubate (25.90 ± 2.34 s vs. 25.03 ± 1.42 s, P = 0.05) and first-attempt intubation success rate (100% vs. 100%, P = 1) were similar between the groups, whereas glottic visualisation (P = 0.01), alternate techniques used to assist intubation (P < 0.001), the ease of intubation (P = 0.02) and intubation difficulty score (P = 0.01) were better in Group K than that in Group C.
Conclusion:
The outcome of KVL and Macintosh laryngoscope was similar in terms of time taken for intubation and first-attempt intubation success rate with KVL having superior glottic visualisation, better ease of intubation and lower intubation difficulty score for elective intubations in children of age <1 year.
Key words: Airway, direct laryngoscope, glottis visualisation, infants, intubation success, King Vision, Macintosh blade, videolaryngoscope
INTRODUCTION
Paediatric anaesthesia and its entire course during the perioperative period often encounters airway and respiratory complications as its most common causes of morbidity and mortality.[1] These adverse events may happen even in healthy children, especially infants. Literature has shown that the highest incidence of difficult laryngoscopy was found among infants, followed by neonates.[2] Preparation for managing an infant's airway requires intricate knowledge regarding the airway anatomy and physiology.[3] Paediatric airway differs markedly from that of adults, particularly during infancy.[3,4] Some of the clinically important differences which can have a direct impact on an infant's airway management are that the larynx is placed at a much higher level (C3–C4) than the adult larynx (C4–C5), larger occiput, a relatively larger tongue[3] with a depressed elongated omega-shaped epiglottis and a concavity along with the slightly inferior and anterior attachment of the vocal cords.[3,4,5] These differences become much less marked, as the child grows older.
As in adults, a prerequisite for successful laryngoscopy and endotracheal intubation in infants requires a clear line of sight between the physician's eyes and the laryngeal inlet.[6] Due to the above-mentioned factors, it is not uncommon that an anaesthesiologist encounters unanticipated difficulty in laryngoscopy and intubation when using conventional direct laryngoscopy using Macintosh blade in an infant. Recent advancements in airway devices resulting from the field of optics and miniature electronics have made possible the advent of paediatric indirect videolaryngoscopes (VLs). Indirect VL, which obviates the need for aligning the line of sight with the laryngeal inlet,[7,8] can afford an added advantage over direct laryngoscopy-guided intubation in the paediatric population.
The efficacy of numerous VLs has been evaluated and compared in the paediatric population in several clinical studies with varying results supporting VL over direct laryngoscope for tracheal intubation.[9,10,11,12,13] King Vision™ VL (KVL) is one such device recently introduced for paediatric age groups, with sizes starting from one.[14] Studies evaluating the efficacy of KVL in children <1 year for routine tracheal intubation are not available. Therefore, this study aimed to find out if the KVL can be compared to the conventional Macintosh laryngoscope in terms of the time taken for intubation and the first-attempt intubation success rate. We hypothesised that the KVL can perform as good as direct laryngoscopy in children <1 year of age for elective tracheal intubation.
METHODS
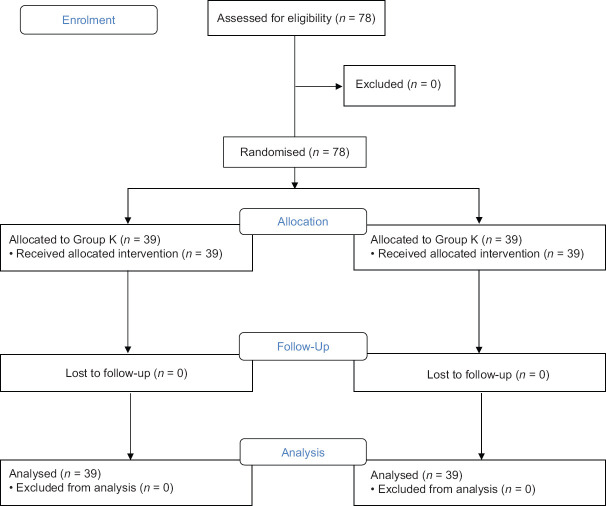
After obtaining approval from the institute's ethics committee (project no: JIP/IEC/2017/0273), Clinical Trials registration (NCT03378154) was done. Patients aged 0–1 year, belonging to American Society of Anesthesiologists physical status 1 and 2 and scheduled for elective surgery under general anaesthesia were enrolled for the study. Informed consent was obtained from either the patients' parents or legally acceptable representatives. Patients with an anticipated difficult airway, tracheal or laryngeal pathologies, cervical spine injuries, active respiratory infection or lung diseases and those with aspiration risk or requiring rapid sequence induction were excluded from the study. A total of 78 patients were randomised to two groups (39 each) using a computer-generated randomisation chart: Group K (non-channelled blade of KVL) and Group C (conventional direct laryngoscope with Macintosh blade) [Figure 1]. Group allocation was concealed using a serially numbered opaque sealed envelope. The objective of the study was to compare the non-channelled blade of size 1 KVL and direct laryngoscope with the Macintosh blade in infants <1 year of age in terms of the time taken for intubation and first-attempt intubation success rate. The secondary objectives were to compare glottis visualisation, the ease of intubation and intubation difficulty score, the alternative technique used in assisting intubation and complication rate.
Figure 1.
Consort flow diagram
After shifting the patient to the operation room, standard monitors in the form of non-invasive blood pressure, electrocardiogram and pulse oximeter (SpO2) were connected and baseline parameters were noted. All infants were provided with a shoulder roll to assist in intubation. A standard induction protocol using either inhalational or intravenous induction technique was used for the induction of general anaesthesia. If intravenous induction was chosen, intravenous fentanyl of 2 μg/kg and thiopentone of 5 mg/kg were used and for inhalational induction, sevoflurane up to 2 minimum alveolar concentration was used. Intravenous vecuronium 0.1 mg/kg was used for muscle relaxation. All the intubation procedures were performed (as per manufacturer's recommendation) by an experienced anaesthesiologist, who had done at least thirty intubations, with each device. Standard PVC-made endotracheal tube (ET) (uncuffed) was used for all the intubations. The ET tube was preformed to the shape of the non-channelled blade of KVL using a rigid stylet for patients in Group K.
The laryngeal view was assessed using Cormack–Lehane grade (CL-grade)[15] and the percentage of glottis opening score (POGO score).[16] An attempt is defined as the insertion of the ET tube into the trachea via the glottis under visualisation using a laryngoscope within 60 s. Inability to pass the ET tube into the glottis within 60 s was considered a failure of the first attempt. More than two attempts of inability to intubate were considered a failure of intubation and the anaesthesiologist was allowed to choose any method of choice for further airway management. First-attempt success rate, time taken until the ET passes the glottis – the time from the introduction of the blade across the teeth to the passage of ET tube beyond the glottis – and the time taken for intubation (until the appearance of end-tidal CO2[EtCO2] trace) – the time from the introduction of the blade across the teeth to the appearance of the EtCO2 graph were recorded by an anaesthesiologist who was not a part of the study. The ease of intubation was graded using a 5-point Likert scale [Table 1]. The difficulty of intubation [Tables 2a and 2b] was assessed using the modified Intubation Difficulty Scale (IDS) using seven parameters.[17] Alternative techniques such as the use of bougie, need for external laryngeal manipulation (BURP manoeuvre) or the need for another specialist were employed. Complications such as airway injury, oesophageal intubation, bronchospasm and desaturation were also recorded.
Table 1.
Ease of intubation using a 5-point Likert scale
| Grade | Ease of intubation |
|---|---|
| 1 | Very easy |
| 2 | Easy |
| 3 | Don’t know |
| 4 | Difficult |
| 5 | Very difficult |
Table 2a.
Modified Intubation Difficulty Scale
| Parameter | Scoring |
|---|---|
| Number of intubation attempts | Each supplementary attempt adds 1 point |
| Number of operators | Each additional operator adds 1 point |
| Alternative technique used | Adds 1 point |
| Glottis exposure (CL grade) | Grade minus one (CL 1=0, CL 2=1, CL 3=2, CL 4=3) |
| Lifting force applied | Normal=0, increased=1 |
| External pressure applied | No=0, yes=1 |
| Vocal cord position at intubation | Abducted=0, adducted=1 |
CL – Cormack-Lehane
Table 2b.
Final Intubation Difficulty Scale
| IDS score | Degree of ease |
|---|---|
| 0 | Easy |
| 1-5 | Slight difficulty |
| More than 5 | Moderate or major difficulty |
IDS – Intubation Difficulty Scale
Data were analysed using International Business Machine (IBM) Statistical Package for the Social Sciences software of version 21 (SPSS, Inc., Chicago, IL, USA). Age, weight and the time taken for intubation were represented as mean and standard deviation and analysed using Student's t-test. First-attempt success rate, POGO score and CL-grade for glottic visualisation, ease of intubation, intubation difficulty score, the alternative technique used and complications were expressed as percentages and proportions and analysed using Mann–Whitney test. The sample size was estimated using the statistical formula for comparing two individual means. It was calculated based on the study by Vlatten et al.[18] who compared STORZ DCI VL versus Miller or Macintosh direct laryngoscope in children of age ranging from 6 months to 4 years, with the minimum expected difference in the intubation time of 4.5 s. The sample size was estimated at 5% level of significance with 80% power and was calculated to be 39 in each group.
RESULTS
After obtaining informed consent from the parent/legally acceptable representative, a total of 78 infants were randomly allocated to two groups (39 each) [Figure 1]. Size 1 non-channelled blade of KVL was used in Group K and direct laryngoscope with Macintosh blade (Size 1) was used in Group C for the tracheal intubation. The mean age (8.6 ± 3.6 vs. 6.8 ± 3.9 months, P = 0.03) and weight (7.8 ± 2.2 vs. 6.7 ± 2.0 kg, P = 0.03) in patients of Group C were found to be higher and statistically significant than those of Group K.
The time taken for the passage of the laryngoscope blade through the incisors and the visualisation of the passage of ET tube through the glottis (21.8 ± 2.62 vs. 20.21 ± 1.88 s) and the time taken for intubation i.e., the time taken from the introduction of the KVL through the incisors until the appearance of the EtCO2 tracing (25.90 ± 2.34 vs. 25.03 ± 1.42 s) were comparable in Group K and Group C, P = 0.063 and P = 0.05, respectively [Table 3]. First-attempt intubation was successful in all patients (100%) using both the devices.
Table 3.
Time taken for tracheal intubation between the study groups
| Group K (n=39) | Group C (n=39) | P | |
|---|---|---|---|
| Time till ET passes the glottis in seconds (mean±SD) | 21.18±2.62 | 20.21±1.88 | 0.063 |
| Time taken for intubation in seconds (until the appearance of EtCO2 trace) (mean±SD) | 25.90±2.34 | 25.03±1.42 | 0.051 |
SD – Standard deviation; ET – Endotracheal tube
CL grading and POGO scores were used for visualisation of the glottis. CL Grade 1 and 2 were obtained in all the 39 patients in both the groups. KVL was found to provide CL Grade 1 view in 94.9% of patients as compared to 48.7% of patients in Group C (P = 0.01). The glottic view was also assessed using the POGO score. The mean POGO scores were statistically significantly higher in Group K as compared to Group C (P = 0.01).
Ease of intubation using the King Vision and conventional laryngoscope was noted based on a 5-point Likert scale. Intubation was easy (Grade 1 and 2 in Likert scale) in 36 (92.3%) patients in Group K as compared to 30 (76.9%) patients in Group C (P = 0.026). The IDS denotes the degree of difficulty of intubation. Difficulty in intubation was noted in 22 (56.4%) patients in Group C as compared to 5 (12.8%) patients in Group K (P = 0.01). The median score was 1 in Group C as compared to 0 in Group K.
External laryngeal manoeuvre (BURP manoeuvre) for aiding the passage of ET tube through the glottic opening was needed in 16 (41%) patients in Group C as compared to 2 (5.1%) patients in Group K, which was statistically significant (P < 0.001). None of the other alternative techniques was used in the study. There were no complications such as airway injury, oesophageal intubation, bronchospasm and desaturation in both the groups.
DISCUSSION
Our randomised clinical trial has shown that the time taken for intubation and the first-attempt intubation success rate were similar between the study groups.
These findings were similar to that of the study by Jagannathan et al.[14] who compared direct laryngoscopy using a Miller blade (DL) with the paediatric KVL in 200 children aged <2 years for elective tracheal intubation as a randomised equivalence trial.[14] Although our study was conducted exclusively on infants, similar to our study results, they found that the total time for successful intubation was not statistically different between the groups, with the POGO score being better with Group KVL. In addition, there was no statistical difference in terms of tracheal intubation attempts, time to best glottic view and complications. They concluded that in children <2 years of age for routine intubation, KVL was equivalent to DC with Miller blade in terms of total time for intubation. They had included children with age up to 2 years, whereas we restricted the upper limit of the age to be 1 year (between 2 months and 9 months). This had focused the results more to the infantile age groups.
Recent literature[19,20] has studied the superiority of VL over direct laryngoscopy in neonates and infants by novices and found that novices had higher first-attempt success rate and fewer oesophageal intubations with VL as compared to those with direct laryngoscope-guided intubation. Therefore, the performance of KVL, in terms of first-attempt intubation success rate and complications in paediatric tracheal intubation, when used by trainees and novices, is another important premise which warrants future dedicated research.
Sun et al.[10] conducted a meta-analysis of 14 randomised controlled trials on children aged <18 years including neonates and infants comparing VLs with direct laryngoscope and concluded that VLs such as Airtraq™, GlideScope®, Storz, TruView, Pentax-AWS®, Bullard and McGrath®, despite better glottic visualisation, were associated with increased time to intubate and faced higher failures than direct laryngoscope. In contrast to the conclusion drawn from this meta-analysis, our study has shown that the time taken for intubation in infants when using paediatric KVL did not differ from that of direct laryngoscopy. This may be due to the fact that this meta-analysis had not included the new paediatric KVL in their analysis and had included children aged up to 18 years.
KVL has also been used successfully in few difficult airway clinical scenarios where direct laryngoscopy either has failed or not possible.[21] Based on our clinical experience with its use in difficult airway cases, it is likely that KVL can be better than the conventional direct laryngoscope in difficult airway scenarios. Because KVL has offered better glottic visualisation scores, ease of intubation and intubation difficulty scores, future researches on anticipated difficult airway in infants using KVL can be undertaken.
KVL, being similar to Macintosh laryngoscopy in terms of intubation time, first-attempt success and complication rates with superior glottic visualisation, better ease of intubation and lower intubation difficulty score, can, therefore act as a potential alternative to direct laryngoscope with Macintosh blade for intubation in infants where the direct laryngoscopy-guided glottic view is poor with higher CL grades and poor POGO scores, although future similar studies are warranted in the infantile age group to prove this finding.
There are a few limitations in our study. First, the study did not intend to find which laryngoscopy performs well when encountering an anticipated difficult airway. Second, all tracheal intubations, in this study, were performed by experienced anaesthesiologists in all patients in both the groups and hence the results cannot be generalised to trainees and novices.
Third, all the tracheal intubations were performed in a controlled environment inside the operation room and therefore, until we have further evidences on the performance of KVL in emergency scenarios, we recommend the use of direct laryngoscopy for all emergency purposes.
CONCLUSION
The outcome of KVL and Macintosh laryngoscope was similar in terms of time taken for intubation and first-attempt intubation success rate with KVL having superior glottic visualisation, better ease of intubation and lower intubation difficulty score for elective intubations in children of age <1 year.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jimenez N, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. An update on pediatric anesthesia liability: A closed claims analysis. Anesth Analg. 2007;104:147–53. doi: 10.1213/01.ane.0000246813.04771.03. [DOI] [PubMed] [Google Scholar]
- 2.Heinrich S, Birkholz T, Ihmsen H, Irouschek A, Ackermann A, Schmidt J. Incidence and predictors of difficult laryngoscopy in 11,219 pediatric anesthesia procedures. Paediatr Anaesth. 2012;22:729–36. doi: 10.1111/j.1460-9592.2012.03813.x. [DOI] [PubMed] [Google Scholar]
- 3.Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci. 2014;4:65–70. doi: 10.4103/2229-5151.128015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adewale L. Anatomy and assessment of the pediatric airway. Paediatr Anaesth. 2009;19(Suppl 1):1–8. doi: 10.1111/j.1460-9592.2009.03012.x. [DOI] [PubMed] [Google Scholar]
- 5.Eckenhoff JE. Some anatomic considerations of the infant larynx influencing endotracheal anesthesia. Anesthesiology. 1951;12:401–10. doi: 10.1097/00000542-195107000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Collins SR. Direct and indirect laryngoscopy: Equipment and techniques. Respir Care. 2014;59:850–62. doi: 10.4187/respcare.03033. [DOI] [PubMed] [Google Scholar]
- 7.Chemsian R, Bhananker S, Ramaiah R. Videolaryngoscopy. Int J Crit Illn Inj Sci. 2014;4:35–41. doi: 10.4103/2229-5151.128011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lingappan K, Arnold JL, Fernandes CJ, Pammi M. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. Cochrane Database Syst Rev. 2018;6:CD009975. doi: 10.1002/14651858.CD009975.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White MC, Marsh CJ, Beringer RM, Nolan JA, Choi AY, Medlock KE, et al. A randomised, controlled trial comparing the Airtraq™ optical laryngoscope with conventional laryngoscopy in infants and children. Anaesthesia. 2012;67:226–31. doi: 10.1111/j.1365-2044.2011.06978.x. [DOI] [PubMed] [Google Scholar]
- 10.Sun Y, Lu Y, Huang Y, Jiang H. Pediatric video laryngoscope versus direct laryngoscope: A meta-analysis of randomized controlled trials. Paediatr Anaesth. 2014;24:1056–65. doi: 10.1111/pan.12458. [DOI] [PubMed] [Google Scholar]
- 11.Fiadjoe JE, Gurnaney H, Dalesio N, Sussman E, Zhao H, Zhang X, et al. A prospective randomized equivalence trial of the GlideScope Cobalt® video laryngoscope to traditional direct laryngoscopy in neonates and infants. Anesthesiology. 2012;116:622–8. doi: 10.1097/ALN.0b013e318246ea4d. [DOI] [PubMed] [Google Scholar]
- 12.Mutlak H, Rolle U, Rosskopf W, Schalk R, Zacharowski K, Meininger D, et al. Comparison of the TruView infant EVO2 PCD™ and C-MAC video laryngoscopes with direct Macintosh laryngoscopy for routine tracheal intubation in infants with normal airways. Clinics (Sao Paulo) 2014;69:23–7. doi: 10.6061/clinics/2014(01)04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JT, Na HS, Bae JY, Kim DW, Kim HS, Kim CS, et al. GlideScope video laryngoscope: A randomized clinical trial in 203 paediatric patients. Br J Anaesth. 2008;101:531–4. doi: 10.1093/bja/aen234. [DOI] [PubMed] [Google Scholar]
- 14.Jagannathan N, Hajduk J, Sohn L, Huang A, Sawardekar A, Albers B, et al. Randomized equivalence trial of the King Vision aBlade videolaryngoscope with the Miller direct laryngoscope for routine tracheal intubation in children<2 years of age. Br J Anaesth. 2017;118:932–7. doi: 10.1093/bja/aex073. [DOI] [PubMed] [Google Scholar]
- 15.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 16.Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: Validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med. 1998;5:919–23. doi: 10.1111/j.1553-2712.1998.tb02823.x. [DOI] [PubMed] [Google Scholar]
- 17.Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The intubation difficulty scale (IDS): Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–7. doi: 10.1097/00000542-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Vlatten A, Aucoin S, Litz S, Macmanus B, Soder C. A comparison of the STORZ video laryngoscope and standard direct laryngoscopy for intubation in the Pediatric airway-A randomized clinical trial. Paediatr Anaesth. 2009;19:1102–7. doi: 10.1111/j.1460-9592.2009.03127.x. [DOI] [PubMed] [Google Scholar]
- 19.Saran A, Dave NM, Karnik PP. Efficacy and safety of videolaryngoscopy-guided verbal feedback to teach neonatal and infant intubation. A prospective randomised cross over study. Indian J Anaesth. 2019;63:791–6. doi: 10.4103/ija.IJA_823_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myatra SN, Doctor JR. Use of videolaryngoscopy as a teaching tool for novices performing tracheal intubation results in greater first pass success in neonates and infants. Indian J Anaesth. 2019;63:781–3. doi: 10.4103/ija.IJA_738_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srinivasan G, Sivakumar RK, Bidkar P, Sharma D. Paediatric King Vision® videolaryngoscope in a case of infantile oral mass: A useful alternative to fiberoptic bronchoscope as a first choice in paediatric difficult airway. Indian J Anaesth. 2019;63:325–7. doi: 10.4103/ija.IJA_792_18. [DOI] [PMC free article] [PubMed] [Google Scholar]