Abstract
Background: Although 2/3 of US adults and nearly 1/3 of US children have overweight or obesity, weight stigma is common. Many with overweight or obesity ascribe negative ideas to themselves, resulting in internalized weight bias (IWB). In adults, IWB has been associated with psychosocial problems; however, this relationship has been studied little in children. This study aims to describe IWB in children with overweight and obesity and to study the association of children's IWB with experienced weight bias, self-esteem, and their parents' IWB.
Methods: Children ages 9–18 with overweight or obesity completed the Weight Bias Internalization Scale (WBIS), Rosenberg Self-Esteem Scale, and Perception of Teasing Scale; parents completed the Weight Bias Internalization Scale-Modified and the Perceived Weight Discrimination Scale. Descriptive statistics were used to assess IWB, self-esteem, and experienced weight stigma. Chi-square and t-tests were used to examine associations between categorical and continuous variables, respectively. Multivariate linear regression was used to identify correlates of IWB in children.
Results: Of 111 child participants, the median WBIS score was 2.8 out of 7. Higher IWB was associated with more peer teasing (p < 0.001) and lower self-esteem (p < 0.001). IWB in children was not associated with child BMI z-score (p = 0.590) or higher parent IWB (p = 0.287).
Conclusions: Children with overweight and obesity who have experienced more teasing by peers or who have lower self-esteem are more likely to have a higher IWB. However, increasing child BMI z-score and parent IWB are not associated with higher child IWB.
Keywords: childhood obesity, explicit bias, internalized weight bias, parent weight bias, peer teasing, weight-based teasing
Introduction
Nearly one-fifth of US children and adolescents have obesity and a similar proportion have overweight,1–4 both of which are associated with psychological and social problems, including internalization of weight-based stigma or bias. Internalized weight bias (IWB) is defined as attributing negative beliefs about one's weight to oneself, causing a belief in stereotypes and negative thoughts because of weight. This internalized bias is related to poorer health and social outcomes in adults, including worse physical and emotional health and higher rates of body dissatisfaction, low self-esteem, disordered eating, and psychological distress.5–7
In adults, IWB is highly correlated with experienced weight-based stigma or discrimination, and both have independently been associated with poor health outcomes.7 Experience of weight stigma in adults is also correlated with lower self-efficacy, more disordered eating, decreased physical activity, and less weight loss.7 In adolescents with overweight or obesity, weight-based teasing by peers is associated with increased weight gain.8 In a meta-analysis of studies involving both children and adults, IWB was found in several studies to be associated with depression, anxiety, stress, and disordered eating behaviors after controlling for experienced weight stigma.9
The effects and associations of IWB have been studied in adults, but similar effects and associations have not been thoroughly studied in pediatric populations. One study found that bariatric surgery-seeking adolescents responded similarly to questions in the Weight Bias Internalization Scale (WBIS) to adult populations.10,11 This study found that, after controlling for BMI, higher IWB in adolescents is positively correlated with depression and anxiety; behavioral problems; and the eating, shape, and weight concerns subscales of the Eating Disorder Examination Questionnaire; and is negatively correlated with quality of life.10 However, this study of adolescents was not representative of the US population with respect to race/ethnicity and BMI; thus, larger studies of more diverse populations of children and adolescents are needed to understand IWB and outcome differences across demographics.
IWB has been studied thoroughly in adults. Adults who are white, have less education, have lower income, and have higher BMI are more likely to have higher IWB; additionally, those who have a higher BMI are currently trying to lose weight, or who have higher self-perceived weight are likely to have a higher IWB.7 In studies of adults and children, females are more likely to have higher IWB than males,12,13 however, some studies report no significant difference in IWB by gender.14 In addition, food insecurity has been linked to obesity in some populations15 and may be related to IWB. In adults reporting food insecurity, specifically those who report that they are unable to provide food for their children, weight-related self-stigma (similar to IWB) is higher than in those without food insecurity.16
In alignment with studies in adults, a recent study in children reported that IWB was higher in girls, in those with lower household incomes, and in children with overweight and obesity.17 The relationships of these demographic factors with IWB have been studied little in children and warrant further evaluation.
Children often face added stigma from family members and peers, potentially contributing to IWB. Many adolescents who have overweight or obesity report being teased or bullied by a parent18 or experiencing negative “weight talk” about their weight or weight loss.19 This negative parental input may alter the development of healthy self-image and self-esteem of children with overweight or obesity. Children with overweight or obesity whose parents perceive them to have overweight or obesity are more likely to gain more weight during childhood and adolescence and are more likely to both view their bodies more critically and attempt to lose weight.20
Previous studies have demonstrated that parents have both explicit and implicit bias toward children with obesity, including parents with a childhood history of obesity or those whose children have obesity.21 Parental explicit bias may be the most important contributor to negative self-image and IWB in children,18 but it is not known whether a parent's IWB contributes to this influence.
The aims of this study were as follows: to examine correlates of IWB in children and adolescents; and to determine the association between IWB in children and IWB in their parents, experienced weight stigma of their parents and themselves, and self-esteem of the child. We hypothesized that IWB in children would be higher with increasing child BMI z-score, lower parental BMI, increasing age, female sex, higher household income, increased parental IWB, more experienced weight stigma of parent and child, and lower self-esteem.
Methods
Participants and Study Design
This was a cross-sectional study of 111 parent/child dyads presenting for health care visits at 4 general pediatric clinics in North Carolina. These clinics serve urban, suburban, and rural communities and serve patients across a range of household incomes with proportionately more low-income households than the national average. Data were collected over an 8-week period.
Children were eligible if they were between the ages of 9 and 18, had overweight or obesity (BMI ≥85th percentile for age and gender) based on measured height/weight recorded in the electronic medical record within the past 6 months, were able to read and write in English, and had an eligible parent or legal guardian present at the visit. Those who met study criteria were approached consecutively. Parents or legal guardians (referred to subsequently as “parents”) were eligible if they were ≥18 years old and able to read and write in English. Children were excluded if they had an intellectual disability or significant developmental delay, if they had complex medical conditions that affect weight gain (e.g., congenital heart disease), or if they had not had a well-child visit in the past 12 months.
Although the WBIS is validated in children aged 14 to 18,10 children as young as 9 years old were included in this study for two reasons. First, overweight and obesity are becoming more and more prominent in children of younger ages, and thus, information on IWB in these younger children is valuable. In addition, by age 9, children without significant developmental delay have been shown to be capable of responding to self-reflective survey questions without assistance.22 Similar studies have used and validated a slightly modified version of the WBIS in children as young as age 7.12 As such, the age range of 9 to 18 was deemed appropriate. Initial screening for age, weight category, and intellectual disability or developmental delay was through chart review; other eligibility requirements were confirmed by participants and parents before discussing the study.
After initial eligibility screening, dyads were approached by research assistants in the clinic examination room to confirm they met the eligibility criteria before describing the study. Parents provided informed consent, children provided assent, and surveys were administered in the examination rooms. Children and parents each filled out the survey on paper individually to avoid bias introduced by family observing the participants' responses. Participants each received a $5 gift card for their participation. The study design was approved by the Wake Forest School of Medicine Institutional Review Board.
Measures
Child surveys included the Weight Bias Internalization Scale (WBIS) as modified by Roberto et al.,10 the Rosenberg Self-Esteem Scale (RSE),23 and the Perception of Teasing Scale (POTS).24 The WBIS is an 11-question survey validated for use in adolescents. Each item is scored on a 7-point Likert scale from strongly disagree to strongly agree, with items 1 and 9 reverse-scored. The WBIS as modified by Roberto et al. demonstrated good internal consistency in the study sample (Cronbach's α = 0.92).10 Scores are averaged, with a higher average indicating greater IWB.
The RSE is a 10-item survey scored on a 4-point Likert scale from strongly agree to strongly disagree, validated to assess self-esteem in children and adolescents. Scores are totaled and averaged, with higher scores indicating higher self-esteem. The RSE demonstrated good internal consistency in the study sample (Cronbach's α = 0.81).23 The POTS is a 6-item survey scored on a 5-point Likert scale from never to always, indicating experienced peer teasing or stigma regarding weight. Scores are totaled, with higher scores indicating more experienced teasing. The POTS demonstrated good internal consistency in the study sample (Cronbach's α = 0.88).24
Parents were administered the Modified Weight Bias Internalization Scale (WBIS-M)13 and the Perceived Weight Discrimination Scale (PWDS).25 The WBIS-M is an 11-item survey validated in people with a healthy weight and people with overweight or obesity to measure IWB. Each item is scored on a 7-point Likert scale from strongly disagree to strongly agree. Scores are totaled and averaged, with higher average scores indicating greater IWB. The WBIS-M demonstrated good internal consistency in the study sample (Cronbach's α = 0.88).13
The PWDS is a 5-item survey with items measured on a 5-point Likert scale from never to sometimes, used to measure experienced weight-based discrimination in adults. Scores are totaled, with higher scores indicating more experienced weight-based discrimination. The PWDS demonstrated good internal consistency in the study sample (Cronbach's α = 0.94).25
Parents also reported demographics, including parents' report of their child's sex, ethnicity (Hispanic/Latino or not), and race (Asian, black or African American, white or Caucasian, other). For this analysis, child race/ethnicity was categorized as white, black, Hispanic, or other. Parents also self-reported their height, weight, education level (some high school or lower, high school graduate, associate degree, some college, and bachelor's degree or higher), and household income (< $20,000; $20–39,999; $40,000–59,999; $60,000–99,999; or $100,000 or more).
We assessed food insecurity using the US Household Food Security 2-item screener: “Within the past 12 months we worried whether our food would run out before we got money to buy more” and “Within the past 12 months the food we bought just didn't last and we didn't have money to get more.” Response options include often, sometimes, or never. Families screened positive for food insecurity if they answered sometimes or often to either question.26 Child height and weight were extracted from the electronic medical record.
Statistical Analysis
Univariate analyses were used to describe demographic characteristics, IWB, self-esteem, and experienced weight stigma of the sample. Bivariate associations between child IWB and correlates were examined using the two-sample Wilcoxon rank-sum (Mann–Whitney) test (for 2 category independent variables) or the Kruskal–Wallis equality-of-populations rank test (for >2 category independent variables).
Multivariate linear regression was also used to identify correlates of child IWB, including child BMI z-score, age, race/ethnicity, household income and food security, and parent BMI. Separate linear regression models were used to examine the individual associations between child IWB and the following: parent IWB, parental experienced weight stigma, peer teasing, and self-esteem, all models adjusting for the covariates above. Finally, to examine the cumulative association with child IWB, a single linear regression model examined the association between child IWB and parent IWB, parental experienced weight stigma, peer teasing, self-esteem, and covariates.
Results
Of the 130 eligible patients approached for participation, 19 dyads declined to participate for a response rate of 85%. Of the 111 children surveyed, 56.1% were male and the mean age was 13.6 (SD 3.34); 39.4% of participants self-identified as white, 44.2% black, 10.6% Hispanic, and 5.8% another race. The mean BMI z-score was 1.8 (SD 0.45), with 43.3% of child participants having overweight and 56.7% having obesity. Of parents, 80% were mothers, 11% fathers, and 8% grandparents. More than half of parents (59.6%) had obesity. Most households (57.6%) had a household income < $40,000 and 36.8% reported food insecurity (Table 1).
Table 1.
Participant Characteristics
| Child characteristics | Mean (SD) or percentage |
|---|---|
| Male | 56.1 |
| Age, years | 13.6 (3.34) |
| BMI z-score | 1.8 (0.45) |
| Weight status | |
| Overweight | 44.7 |
| Obesity | 55.3 |
| Class I | 34.3 |
| Class II | 13.3 |
| Class III | 7.6 |
| Parent characteristics | Mean (SD) or percentage |
| Legal guardian | |
| Mother | 80 |
| Father | 11 |
| Grandparent | 8 |
| BMI | 33.5 (9.57) |
| Weight status | |
| Underweight | 2.0 |
| Healthy weight | 13.1 |
| Overweight | 25.6 |
| Obesity | 59.6 |
| Household income | |
| < $20K | 29.3 |
| $20K–40K | 28.3 |
| $40K–60K | 15.2 |
| $60K–100K | 12.1 |
| > $100K | 15.2 |
| Race/ethnicity | |
| White | 39.4 |
| Black | 44.2 |
| Hispanic | 10.6 |
| Other | 5.8 |
SD, standard deviation.
Child and Parent Measures
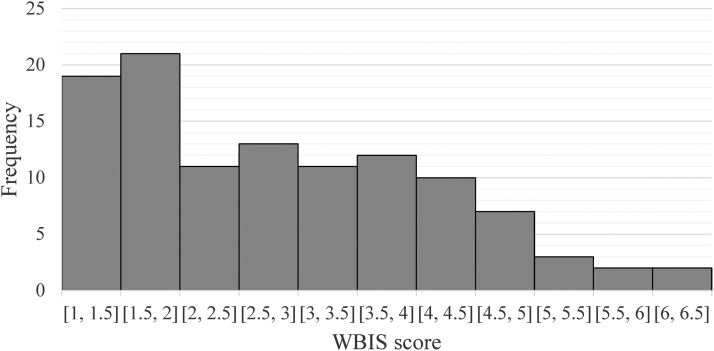
The median child WBIS score was 2.8 out of 7 (IQR 1.75–3.8, range 1–6.5) (Fig. 1). Median RSE score was 2.1 (IQR 1.8–2.65, range 2.2–3) out of 3, with higher scores indicating higher self-esteem. The median POTS score was 1 (IQR 1–1.83, range 1–5) out of 5, with higher scores indicating more perceived teasing about weight. The median WBIS-M score for parents was 2.64 (IQR 1.91–3.82, range 1–6.64) out of 7. The median PWDS score was 2 (IQR 2–2, range 1–4.6) out of 5, with higher scores indicating more perceived discrimination due to weight.
Figure 1.
Distribution of child internalized weight bias.
Correlates of Child IWB
In bivariate analysis, children with food insecurity had higher mean WBIS scores than children without food insecurity (3.11 vs. 2.66, p = 0.049). Child's mean WBIS score was not associated with race or ethnicity, child age, parent education level, household income, child BMI z-score, child weight category, parental perception of child's BMI, parent BMI, parent weight category, parents' perceived weight discrimination, or parental IWB. In multivariate analysis, IWB in children was not associated with child's age, race/ethnicity, or BMI z-score, parent BMI, or household income or food insecurity (Table 2).
Table 2.
Correlates of Child Internalized Weight Bias
| β (95% CI) | |
|---|---|
| Child BMI z-score | 0.18 (−0.48 to 0.84) |
| Age, years | 0.00 (−0.12 to 0.13) |
| Race/ethnicity | −0.12 (−0.56 to 0.33) |
| Household income | −0.05 (−0.32 to 0.22) |
| Parent BMI | −0.01 (−0.05 to 0.02) |
| Food insecurity | 0.43 (−0.30 to 1.16) |
CI, confidence interval.
Association of Child IWB with Peer Teasing, Self-Esteem, and Parent IWB and Perceived Weight Discrimination
In both unadjusted bivariate analysis and adjusted multivariate analysis, child IWB was positively associated with more experienced peer teasing and inversely related to self-esteem (Table 3). Child IWB was not associated with parental IWB or parental experienced weight discrimination in either unadjusted bivariate or adjusted multivariate analysis. In multivariate analysis including peer teasing, child self-esteem, and covariates in a single model, both peer teasing and self-esteem were independently associated with higher IWB (Table 4).
Table 3.
Adjusted Multivariate Regression Models Demonstrating the Associations of Child Internalized Weight Bias with Child and Parent Characteristics
| Child/parent characteristic | Unadjusted | Adjusted | |
|---|---|---|---|
| Model 1 | Child teasing (POTS) | 0.63 (0.35 to 0.90)*** | 0.72 (0.40 to 1.03)*** |
| Model 2 | Child self-esteem (RSE) | −1.74 (−2.14 to −1.32)*** | −1.80 (−2.30 to −1.30)*** |
| Model 3 | Parent IWB | 0.06 (−0.16 to 0.28) | 0.16 (−0.13 to 0.45) |
| Model 4 | Parent weight stigma (PWDS) | 0.05 (−0.35 to 0.46) | 0.24 (−0.30 to 0.79) |
Reported as β-coefficient (95% CI).
The separate adjusted models each included the child/parent characteristic referenced in the model's name in addition to the following covariates: child BMI z-score, child age, child race/ethnicity, parent BMI, household income, and household food insecurity.
p < 0.05, **p < 0.01, ***p < 0.001.
IWB, internalized weight bias; POTS, Perception of Teasing Scale; PWDS, Perceived Weight Discrimination Scale; RSE, Rosenberg Self-Esteem Scale.
Table 4.
Multivariate Regression Model Demonstrating the Association of Child Internalized Weight Bias with Child Teasing, Child Self-Esteem, and Other Child and Parent Variables
| β-coefficient (95% CI) | |
|---|---|
| Child teasing (POTS) | 0.44 (0.14 to 0.74)** |
| Child self-esteem (Rosenberg) | −0.16 (−0.22 to −0.11)*** |
| Child BMI z-score | 0.02 (−0.56 to 0.59) |
| Child age, years | −0.06 (−0.16 to 0.04) |
| Child race/ethnicity | 0.06 (−0.30 to 0.41) |
| Parent BMI | −0.02 (−0.04 to 0.01) |
| Household income | 0.00 (−0.20 to 0.21) |
| Household food insecurity | −0.10 (−0.69 to 0.50) |
p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
Children with overweight or obesity who have experienced teasing by peers about their weight or who have a lower self-esteem are more likely to have a higher IWB; however, IWB is low overall in this sample of children with overweight and obesity (median 2.8, IQR 1.75–3.8) compared with previously studied samples of adults and children.13,14 IWB in children is not associated with socioeconomic or demographic factors including age, race/ethnicity, household income, or child BMI z-score; this was unexpected in the context of the association of these characteristics with IWB in prior studies of adults7,9,13 and children.17 IWB in children with overweight or obesity is also not associated with parental factors including parental BMI, IWB, or experienced weight-based stigma. There may be an association between household food insecurity and higher IWB.
Although we hypothesized that correlates of IWB in children would parallel those of previous studies in adults, our results do not support these relationships of IWB with personal, social, or demographic factors in children. Previous studies have demonstrated that adults who are white, have less education or lower income, or have a higher BMI are more likely to have high IWB7; however, these relationships are not present in our racially and socioeconomically diverse sample of children. However, other studies in adults have found that those who have experienced weight stigma and teasing had higher IWB,7 which is true in our sample of children.
Previous studies have suggested that a parent's views or attitudes regarding weight can affect a child's health, weight perception, weight gain or loss, and IWB.18–21 However, this study does not demonstrate a significant relationship between parental IWB and child IWB. Explicit or implicit antifat bias in parents was not assessed in this study, which may affect the interaction between parents and children regarding weight. Parent gender may also impact the relationship between parent and child IWB. Most of the parents and guardians surveyed were mothers (80%); due to the low sample size of male parents completing the survey, parent sex was not included in multivariate analysis.
The overall low IWB scores in the children who participated may have limited the evaluation of this relationship. There was also no significant association between parental BMI or parental experienced weight stigma and child IWB.
This sample of children demonstrated a lower IWB (median 2.8) than previous studies of both adults and children. Recent literature studying adults with overweight or obesity has reported mean WBIS scores ranging from 3.30 to 4.11.13,14 In two studies of children and adolescents with overweight or obesity seeking treatment for their weight, mean IWB was 3.78 and 4.29.10,27 A sample of children of all weight categories aged 7 to 11 reported a WBIS-Y mean score of 1.59 (SD 0.56) in girls and 1.50 (SD 0.53) in boys12; however, these were reported on a 4-point scale rather than a comparable 7-point scale.
Similarly, a version of the WBIS modified to be more accessible to younger children, the WBIS-C, was validated in children of all weight categories ages 9 to 13 and reports a WBIS-C score of 1.51 (SD = 0.51) in children of healthy weight and a score of 2.12 (SD 0.67) on a 4-point scale in children with overweight and obesity.28 Although the scale of these studies differs from the 7-point scale used in this study, the score of 2.12 in children with overweight and obesity falls between “somewhat disagree” and “somewhat agree” on the 4-point scale; similar responses would range from 3 to 5 on the 7-point scale used in this and other studies.
A recent study of children across weight statuses found that children with overweight or obesity have higher WBIS-C scores than children with underweight or normal weight.17 Although the scoring is not consistent across studies, these samples all report higher or apparently higher IWB in those with overweight and obesity than what was reported in this sample.
This population is unique in that it included children in younger age groups than many prior studies; although there was not a significant difference in IWB among age groups in the sample, this may have contributed to the lower value overall. In addition, the diverse sample did not mirror populations in other samples. The population in this study included a higher proportion of African American children and a lower proportion of white children. Previous studies have suggested that body dissatisfaction is lower in African Americans of all body types29 and that IWB is generally lower in African Americans than in whites,30 which may predict lower IWB in African American youth and could contribute to the lower IWB overall in this study.
Previous studies of IWB, its psychometric properties, and its clinical correlates include populations that are mostly white; as such, the diversity of this study population complements existing literature and adds to the understanding of IWB in African American and Hispanic children. In addition, most tools used to measure IWB are validated in mostly white populations and thus may not accurately assess IWB in children of all races. Given the dearth of data representing children of various racial backgrounds, further study is warranted to evaluate clinical correlates of IWB in African American and Hispanic children.
The study location in the Southeastern United States could also contribute to a lower IWB than prior studies, where studies are heavily focused in the Northeastern United States and in Europe. Several previous studies of IWB in those with overweight and obesity include only participants who are seeking treatment for weight, whereas this population was not treatment-seeking; this also may contribute to the lower IWB in this sample than in prior studies.5,27,30
In our population of children, weight-based teasing by peers and low self-esteem are associated with a higher IWB. Weight-based peer teasing in children has been associated with poorer academic outcomes, restrictive eating habits, psychosocial and developmental challenges, and lower self-esteem,10,11,31–33 all of which are also related to higher IWB.12,27 Our results support that this teasing may be associated with increased IWB in children; however, both experienced teasing by peers (as measured by the POTS) and IWB are low overall in this sample of children.
In addition, our results demonstrate a relationship between low self-esteem and higher IWB in children. These results are consistent with prior studies in children and adults.27,34 Low self-esteem in children is associated with worse physical and psychological health, higher rates of disordered eating, increased risk-taking behaviors, and increased incidence of suicidal ideation,35,36 making self-esteem and IWB important areas of study.
It is likely that the development of IWB in children and its association with peer teasing and low self-esteem is complex and multifactorial. IWB does not vary by age in this study group, which may suggest that IWB develops and changes at an earlier age. Prior studies suggest that implicit stigma about weight may develop in children as young as preschool age,18 and weight-based teasing may start at a similar time. It is possible that teasing based on weight that occurs at such a young age may change a child's developing concept of self, lower a child's self-esteem, and increase IWB; our results concur that factors that lower a child's self-esteem may also be associated with a higher IWB. The contribution of parental teasing and outside influences such as media and other stigma may also contribute to early development of IWB.
In older children and adolescents, pubertal changes and increasing attention to appearance likely increase the focus on a child's weight, which may also be associated with increased IWB. A 2009 study of early-adolescent girls found that girls in later stages of puberty were more likely to report peer victimization on the basis of weight and more likely to report concerns about their weight.37 In addition, a 2002 study of Australian adolescents found that puberty was a key predictor for efforts to change one's body.38 These results support changes in focus on weight and appearance during older adolescence, specifically during puberty.
However, the low IWB in our population of children and adolescents may suggest that these changes are not necessarily associated with a higher IWB. It is also possible that IWB does not vary at all by age, but is more inherent to the individual than to an age or age range. It is likely that these factors and others lead children and adolescents to attribute to themselves negative ideas and opinions about people with overweight and obesity.
This study has important limitations. The study group includes 111 parent/child dyads at 4 pediatric clinics in 1 geographic area in North Carolina, which may limit generalizability. The smaller size of the study may limit our power to detect possible relationships between IWB and child and parent demographics as hypothesized, as data collection was limited to an 8-week period due to funding constraints. This study included mainly mothers and very few fathers or other guardians, which may have altered the relationships between parent and child IWB. In addition, although the participants at these clinics are diverse in terms of race and ethnicity and household income, the study group overrepresents participants who identify as black and those with household incomes < $60,000 per year.
The majority of children surveyed have low IWB, so it is possible that surveying more children with higher IWB would demonstrate different relationships and results. Furthermore, a relationship between IWB and food insecurity is inconclusive: bivariate analysis demonstrates a significant relationship between IWB and food insecurity (p = 0.049), but this relationship is not significant in multivariate analysis. This inconsistency may be related to a lack of power or a different variable in our analysis. A larger more representative study population may find further relationships between IWB in children and other factors.
IWB in children has not been thoroughly studied, and further research is necessary to better describe and characterize children's IWB. Future studies should seek to describe further IWB in a group that better represents the US population and evaluates how IWB may change longitudinally throughout childhood and adolescence. Evaluation of IWB in children without overweight and obesity is also warranted, as some adults without overweight or obesity have been shown to have higher IWBs.13
This study demonstrates a significant relationship between self-esteem and peer teasing and higher IWB in children, and providers caring for these children should consider assessing and discussing these issues with children and their patients. While further evaluation of IWB in children is warranted, these results provide a novel description of IWB in a diverse population of children and adolescents with overweight and obesity and provoke new questions about IWB in the larger population of children and teenagers.
Conclusions
Children with overweight or obesity who have lower self-esteem or have experienced more teasing by peers about their weight are more likely to have higher IWB. IWB is not, however, associated with a child's BMI z-score, age, gender, race/ethnicity, parent BMI or IWB, or parental experienced weight-based stigma. IWB is low overall in this diverse sample of children. Additional research is needed to assess IWB in broader samples of children, investigate the relationship between food insecurity and IWB, and further evaluate the relationships among peer teasing, self-esteem, and IWB.
Acknowledgments
The authors acknowledge the Pediatrics Department of the Wake Forest School of Medicine, the Brenner FIT program, and the Wake Forest Associated Pediatric Clinics for their support of this research. This study was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding Information
Ignition Grant of the Wake Forest CTSI, which is supported by the National Center for Advancing Translational Sciences, NIH, through grant award number UL1TR001420; National Institutes of Health T35 Training Grant.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Fryar CD, Carroll MD, Ogden CL. Prevalence of Overweight and Obesity Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2013–2014. Hyattsville, MD: National Center for Health, 2016 [Google Scholar]
- 2. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004;291:2847–2850 [DOI] [PubMed] [Google Scholar]
- 4. Lifshitz F. Obesity in children. J Clin Res Pediatr Endocrinol 2008;1:53–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Latner JD, Durso LE, Mond JM. Health and health-related quality of life among treatment-seeking overweight and obese adults: Associations with internalized weight bias. J Eat Disord 2013;1:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pearl RL, Hopkins CH, Berkowitz RI, et al. Group cognitive-behavioral treatment for internalized weight stigma: A pilot study. Eat Weight Disord 2018;23:357–362 [DOI] [PubMed] [Google Scholar]
- 7. Puhl RM, Himmelstein MS, Quinn DM. Internalizing weight stigma: Prevalence and sociodemographic considerations in US adults. Obesity (Silver Spring) 2017;26:167–175 [DOI] [PubMed] [Google Scholar]
- 8. Schvey NA, Marwitz SE, Mi SJ, et al. Weight-based teasing is associated with gain in BMI and fat mass among children and adolescents at-risk for obesity: A longitudinal study. Pediatr Obes 2019;14:e12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pearl RL, Puhl RM. Weight bias internalization and health: A systematic review. Obes Rev 2018; 19:1141–1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roberto CA, Sysko R, Bush J, et al. Clinical correlates of the weight bias internalization scale in a sample of obese adolescents seeking bariatric surgery. Obesity (Silver Spring) 2012;20:533–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity (Silver Spring) 2009;17:941–964 [DOI] [PubMed] [Google Scholar]
- 12. Zuba A, Warschburger P. The role of weight teasing and weight bias internalization in psychological functioning: A prospective study among school-aged children. Eur Child Adolesc Psychiatry 2017;26:1245–1255 [DOI] [PubMed] [Google Scholar]
- 13. Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: Validation of the Modified Weight Bias Internalization Scale. Body Image 2014;11:89–92 [DOI] [PubMed] [Google Scholar]
- 14. Durso LE, Latner JD. Understanding self-directed stigma: Development of the Weight Bias Internalization Scale. Obesity (Silver Spring) 2008;16(Suppl 2):S80–S86 [DOI] [PubMed] [Google Scholar]
- 15. Moradi S, Mirzababaei A, Dadfarma A, et al. Food insecurity and adult weight abnormality risk: A systematic review and meta-analysis. Eur J Nutr 2019;58:45–61 [DOI] [PubMed] [Google Scholar]
- 16. Becker CB, Middlemass K, Taylor B, et al. Food insecurity and eating disorder pathology. Int J Eat Disord 2017;50:1031–1040 [DOI] [PubMed] [Google Scholar]
- 17. Gmeiner MS, Warschburger P. Intrapersonal predictors of weight bias internalization among elementary school children: A prospective analysis. BMC Pediatr 2020;20:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pont SJ, Puhl R, Cook SR, et al. Stigma experienced by children and adolescents with obesity. Pediatrics 2017;140:e20173034. [DOI] [PubMed] [Google Scholar]
- 19. Pudney EV, Himmelstein MS, Puhl RM. The role of weight stigma in parental weight talk. Pediatr Obes 2019;14:e12534. [DOI] [PubMed] [Google Scholar]
- 20. Robinson E, Sutin AR. Parents' perceptions of their children as overweight and children's weight concerns and weight gain. Psychol Sci 2017;28:320–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lydecker JA, O'Brien E, Grilo CM. Parents have both implicit and explicit biases against children with obesity. J Behav Med 2018;41:784–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Borgers NB, de Leeuw E, Hox J. Children as respondents in survey research: Cognitive development and response quality. Bull Méthodol Sociol 2000;66:60–75 [Google Scholar]
- 23. Rosenberg M. Society and the Adolescent Self-Image. Princeton University Press: Princeton, NJ, 1989 [Google Scholar]
- 24. Thompson JK, Cattarin J, Fowler B, et al. The Perception of Teasing Scale (POTS): A Revision and Extension of the Physical Appearance Related Teasing Scale (PARTS). J Pers Assess 1995;65:146–157 [DOI] [PubMed] [Google Scholar]
- 25. Grant BF, Dawson DA. Introduction to the national epidemiologic survey on alcohol and related conditions. Alcohol Res Health 2006;29:74–78 [PMC free article] [PubMed] [Google Scholar]
- 26. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126:e26–e32 [DOI] [PubMed] [Google Scholar]
- 27. Ciupitu-Plath C, Wiegand S, Babitsch B. The Weight Bias Internalization Scale for youth: Validation of a specific tool for assessing internalized weight bias among treatment-seeking German adolescents with overweight. J Pediatr Psychol 2018;43:40–51 [DOI] [PubMed] [Google Scholar]
- 28. Zuba A, Warschburger P. Weight bias internalization across weight categories among school-aged children. Validation of the Weight Bias Internalization Scale for children. Body Image 2018;25:56–65 [DOI] [PubMed] [Google Scholar]
- 29. Yates A, Edman J, Aruguete M. Ethnic differences in BMI and body/self-dissatisfaction among Whites, Asian subgroups, Pacific Islanders, and African-Americans. J Adolesc Health 2018;34:300–307 [DOI] [PubMed] [Google Scholar]
- 30. Pearl RL, Wadden TA, Hopkins CM, et al. Association between weight bias internalization and metabolic syndrome among treatment-seeking individuals with obesity. Obesity (Silver Spring) 2017;25:317–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Krukowski RA, Smith West D, Philyaw Perez A, et al. Overweight children, weight-based teasing and academic performance. Int J Pediatr Obes 2009;4:274–280 [DOI] [PubMed] [Google Scholar]
- 32. Goldfield G, Moore C, Henderson K, et al. The relation between weight-based teasing and psychological adjustment in adolescents. Paediatr Child Health 2010;15:283–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Arch Pediatr Adolesc Med 2003;157:733–738 [DOI] [PubMed] [Google Scholar]
- 34. Pearl RL, Puhl RM. The distinct effects of internalizing weight bias: An experimental study. Body Image 2016;17:38–42 [DOI] [PubMed] [Google Scholar]
- 35. McGee ROB, Williams S. Does low self-esteem predict health compromising behaviours among adolescents? J Adolesc 2000;23:569–582 [DOI] [PubMed] [Google Scholar]
- 36. Overholser JC, Adams DM, Lehnert KL, et al. Self-esteem deficits and suicidal tendencies among adolescents. J Am Acad Child Adolesc Psychiatry 1995;34:919–928 [DOI] [PubMed] [Google Scholar]
- 37. Compian LJ, Gowen LK, Hayward C. The interactive effects of puberty and peer victimization on weight concerns and depression symptoms among early adolescent girls. J Early Adolesc 2009;29:357–375 [Google Scholar]
- 38. McCabe MP, Ricciardelli LA, Finemore J. The role of puberty, media and popularity with peers on strategies to increase weight, decrease weight and increase muscle tone among adolescent boys and girls. J Psychosom Res 2002;52:145–153 [DOI] [PubMed] [Google Scholar]