Abstract
Background: The (COVID-19) pandemic resulted in sudden disruption of routine clinical care necessitating rapid transformation to maintain clinical care while safely reducing virus contagion.
Introduction: Memorial Sloan Kettering (MSK) experienced a rapid evolution from delivery of in-person cessation counseling services to virtual telehealth treatments for our tobacco-dependent cancer patients.
Aim: To examine the effect of rapid scaling of tobacco treatment telehealth on patient engagement, as measured by attendance rates for in-person counseling visits versus remote telehealth counseling visits. We also describe the patient, clinician, and health care system challenges encountered in rapid expansion of individual and group tobacco telehealth services.
Methods: Data collected from the electronic medical record during the first 4 months of the COVID-19 pandemic were examined for tobacco treatment counseling.
Results: From January 1, 2020 to March 30, 2020, markedly improved patient engagement was observed in ambulatory tobacco treatment services with greater attendance at scheduled telehealth visits than in-person visits, 75% versus 60.3%, odds ratio 1.84 (confidence interval: 1.26–2.71; p < 0.001). In addition, bedside hospital counseling visits were transformed into inpatient telephone visits with high levels of sustained patient engagement. Lastly, group telehealth services were launched rapidly to increase capacity and provide greater psychosocial support for cancer patients struggling with tobacco dependence.
Discussion: Clinical, Information Technology (IT), and hospital system barriers were successfully addressed for most cancer patients seeking individual telehealth treatment. Group telehealth services were found to be feasible and acceptable.
Conclusions: MSK's rapid leap into virtual care delivery mitigated disruption of tobacco treatment services and demonstrated strong feasibility and acceptance for managing complex tobacco-dependent patients.
Keywords: telemedicine, tobacco, counseling, group, cancer, COVID-19
Background
Global social distancing methods outlined by the Centers for Disease Control and Prevention1 and the World Health Organization2 in March 2020 necessitated a rapid and massive response by health care systems in response to the coronavirus 2019 (COVID-19) pandemic. Hospital systems were required to quickly transform clinical practice models, ensuring that patients and their health care providers reduce the risk of person–person viral spread, while maintaining continuity of care. Rapid implementation of remote telehealth treatment services provided an opportunity to provide both social distancing with efficacious and compassionate clinical care.
Introduction
In addition to being the leading preventable cause of cancer, persistent use of tobacco products after a cancer diagnosis is associated with poorer cancer-related clinical outcomes.3 Continued smoking has been shown to increase risks for higher mortality, and prolong complications during recovery.3 Thus, there is strong clinical rationale to provide access to high-quality tobacco treatment for cancer patients, particularly, in the context of COVID-19 pandemic and emerging concerns about smoking and the severity of COVID-19.4–6 Clinical practice guidelines for promoting smoking cessation among cancer patients exist,7 and these guidelines recommend cessation counseling and pharmacotherapy for all tobacco-dependent cancer patients. Models of tobacco treatment counseling vary greatly and include individual and group counseling delivered in person and through telephone. More recently, there has been growing interest in integrating telehealth tobacco treatment into models of tobacco treatment delivery.8
Our well-established tobacco treatment program (TTP) is embedded in a large metropolitan comprehensive cancer center with regional sites spanning two states. In this article, we sought to explore the impact of COVID-19 on the delivery format of our treatment services. Our primary aim was to evaluate changes in patient engagement, by visit format, as measured by attendance and cancellation rates to see whether telehealth services were not only feasible across our patient population but also more accessible, thereby facilitating lower cancellation rates than in-person visits. Our secondary aim was to describe patient-, clinician-, and system-level barriers encountered during this rapid transformation into a virtual clinic. We also examined patient engagement as the inpatient bedside tobacco treatment counseling program was transformed into a telephone-only counseling format during the COVID-19 pandemic.
A recent call has been made for more research on the feasibility and effectiveness of telehealth tobacco dependence treatment.9 In the 2020 surgeon general's report on smoking cessation,10 group telehealth treatment has been identified as an emerging yet relatively understudied behavioral intervention. Group telehealth treatment may provide additional capacity and psychosocial support attributable to the unique intragroup interactions between patients.11,12 Thus, to maintain continuity of care for existing patients, and expand clinical capacity, we also describe our initial experiences transitioning three weekly regional in-person group meetings into remote group telehealth counseling visits.
Methods
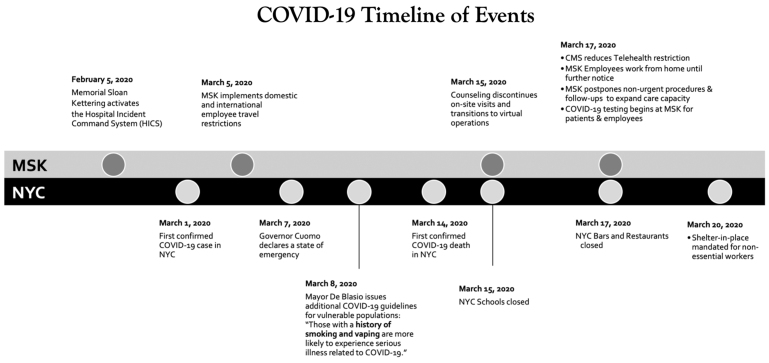
Figure 1 shows a succinct summary of the COVID-19 pandemic timeline in New York City (NYC) and Memorial Sloan Kettering (MSK) Cancer Center's preparedness to address an upsurge in COVID-19 cases within our cancer center.
Fig. 1.
Timelines of coronovirus pandemic events. MSK, Memorial Sloan Kettering; NYC, New York City.
Description of TTP
Universal screening of smoking and use of other tobacco products and an opt-out referral model to in-house tobacco treatment for all current smokers/tobacco users is the standard of care at our cancer center. The backbone of our TTP involves inpatient bedside counseling to all hospitalized patients who report current smoking or use of other tobacco products. Bedside treatment is provided by advanced practice nurses who are certified tobacco treatment specialists. We also offer ambulatory tobacco treatment delivered through individual face-to-face and telephonic counseling sessions combined with evidence-based pharmacotherapy that has been shown to yield high quit rates with cancer patients.13–15
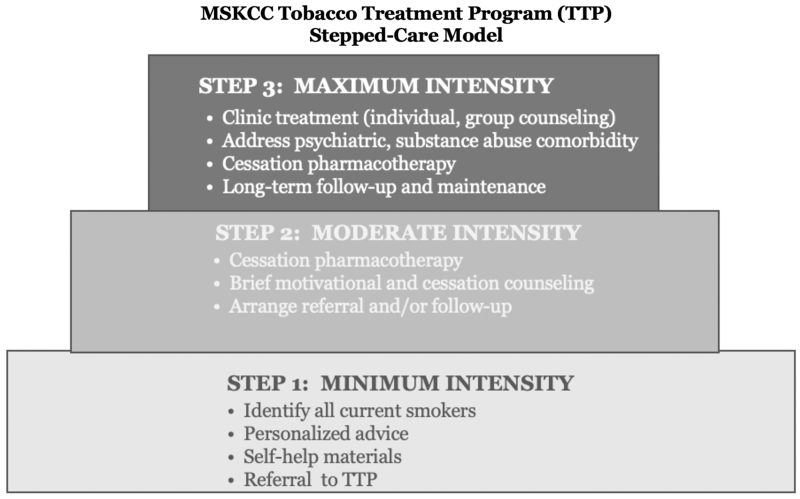
Although inpatient bedside and outpatient telephone counseling have historically comprised ∼85% of our TTPs patient visits, patients with more complex behavioral health comorbidities, such as other addictions and other psychiatric comorbidities, receive more intensive in-person treatment (Fig. 2). Moderate-intensity treatment typically involves a 45–60-min intake and at least 2 to 3, 20–30-min follow-up telephone visits, whereas maximum-intensity treatment typically involves a 45–60-min intake and at least 5 to 10, 30–45-min follow-up visits.
Fig. 2.
Memorial Sloan Kettering Cancer Center tobacco treatment program model. MSKCC, Memorial Sloan Kettering Cancer Center; TTP, tobacco treatment program.
In 2018, as part of our cancer center's burgeoning TeleOncology initiative, our TTP began seeing ∼15% of our maximum-intensity outpatient visits through telehealth modality.16 The volume of telehealth treatment visits delivered remained largely unchanged from January, 2019, until the beginning of the pandemic in early March 2020, whereby we became confronted with a seismic shift as we amplified telehealth TTP services to address the coronavirus pandemic.
Description of Patients
Descriptive data were extracted from the electronic medical records of cancer patients who had tobacco treatment appointments scheduled between January 1, 2020, and April 30, 2020 (289 scheduled for moderate-intensity care, 172 scheduled for maximum-intensity care, and 43 for combination treatment formats, for a total of 418 patients). In addition to appointment disposition data, we used data extracted from MSK's tobacco treatment intake form. This patient-reported clinical form assesses patient tobacco use, smoking patterns and history, level of tobacco dependence, motivation and confidence to quit, and co-occurring conditions.
In addition, information about patient visit disposition was extracted and summarized. Specifically, we examined attendance status (e.g., attended or cancelled/no-show appointment) by mode of delivery (e.g., telehealth or in-person). A summary of demographic characteristics and cancer diagnosis for patients who received maximum-intensity treatment is given in Table 1.
Table 1.
Demographics and Primary Cancer Diagnoses of Patients in Maximum-Intensity Treatment
| Age (mean) | 58.5 (SD = 12.2) |
| Gender, n (%) | |
| Female | 107 (62.2) |
| Male | 65 (37.8) |
| Race, n (%) | |
| Asian | 6 (3.5) |
| Black | 17 (9.9) |
| Unspecified | 14 (8.1) |
| White | 135 (78.5) |
| Hispanic ethnicity, n (%) | 15 (8.8) |
| Cancer type | |
| Bone | 3 (1.74) |
| Brain | 2 (1.16) |
| Breast | 39 (22.67) |
| Colorectal | 8 (4.65) |
| Genitourinary | 25 (14.53) |
| Head and neck | 13 (7.56) |
| Hodgkin's lymphoma | 2 (1.16) |
| Leukemia | 2 (1.16) |
| Liver | 2 (1.16) |
| Lung | 26 (15.12) |
| Non-Hodgkin's lymphoma | 2 (1.16) |
| Skin | 4 (2.33) |
| Other cancers | 41 (23.84) |
| No cancer | 3 (1.74) |
| Total | 172 (100) |
Statistical Methods
Using appointment completion, we created cross-tabulations and conducted chi-squared tests analyzing the likelihood of appointment completion (vs. cancellation) based on whether the appointment was delivered through telehealth or in-person. We also used logistic regression to determine the likelihood of appointment completion while accounting for whether the appointment was scheduled before or after the pandemic declaration. All statistical analyses were done using R Statistical Software.
Results
Moderate-Intensity Treatment (Bedside and Telephone)
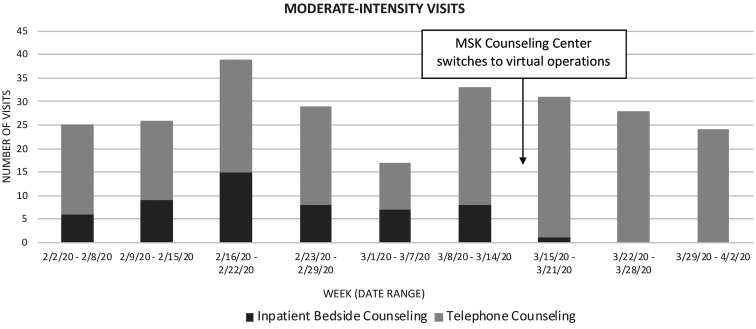
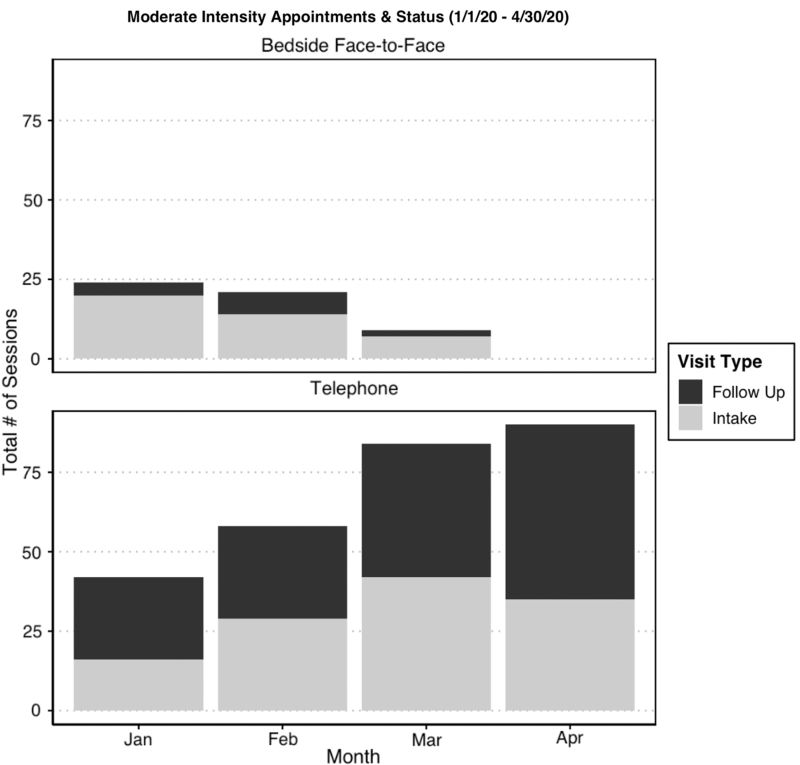
From January 1, 2020, to March 17, 2020, the 289 patients who received moderate-intensity tobacco treatment received bedside inpatient tobacco treatment counseling and phone visits (Fig. 3). By March 18, secondary to COVID-19, all in-person bedside visits were transferred to telephone counseling consistent with new hospital infection control policies. The TTP continued to sustain high volumes of tobacco treatment counseling visits with both inpatients and outpatient follow-up visits. Data highlight patterns of initial intake visits with new patients and follow-up counseling visits (Fig. 4). Since many nonurgent surgeries were postponed due to concerns about patient safety, lower number of referrals were expected.
Fig. 3.
Moderate-intensity visits by week. MSK, Memorial Sloan Kettering.
Fig. 4.
Moderate-intensity visits, stratified by status, month, and appointment type.
Maximum-Intensity Treatment (In-Person and Telehealth)
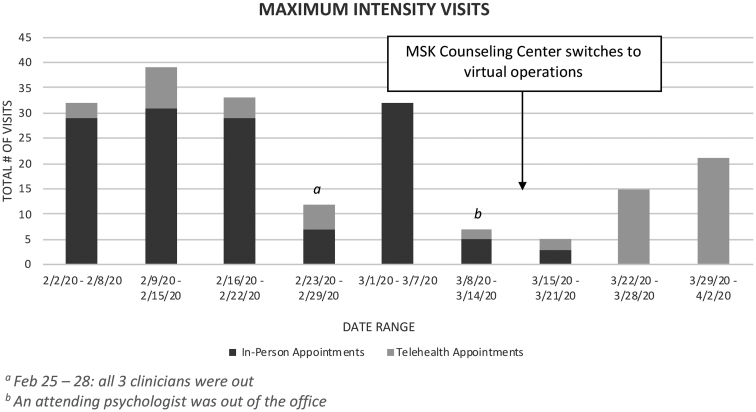
Of the 172 maximum-intensity counseling patients scheduled, 135 patients received in-person appointments, 73 received telehealth appointments, and 36 received both treatment delivery formats. Until March 1, most ambulatory TTP appointments were conducted in-person at one of our clinical sites. However, the COVID-19 shelter in-place order rapidly reversed this practice pattern (Fig. 5). In-person counseling visits (i.e., individual and group) are shown from February to March. During January and February 2020, ∼15% of all visits were through telehealth, but this quickly transformed by late March to 100% telehealth visits.
Fig. 5.
Maximum-intensity visits by week. MSK, Memorial Sloan Kettering.
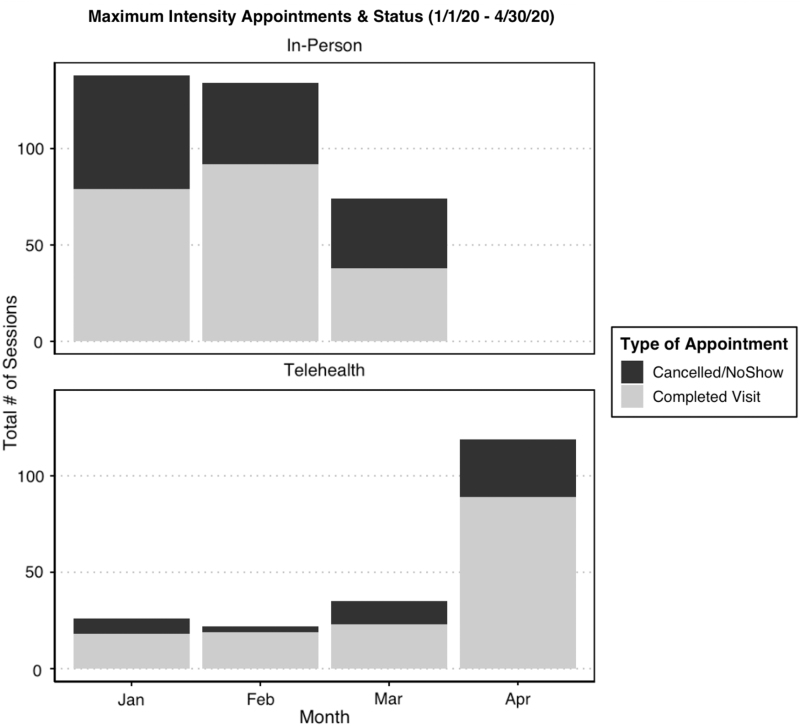
Figure 6 shows our maximum-intensity treatment, across time, comparing telehealth visits with in-person visits. When initially comparing appointment mode of delivery (Table 2), the odds of completion for telehealth versus in-person appointments, we found significantly higher rates of visit completion (75% vs. 60.3%) with the unadjusted odds ratio = 1.84 (confidence interval: 1.26–2.71; p < 0.001). As given in Table 3, when controlling for whether the appointment occurred before or after the pandemic outbreak, a telehealth visit had 2.30 times (1.47–3.66; p < 0.001) the odds of completion compared with those of an in-person visit.
Fig. 6.
Maximum-intensity visits, stratified by status, month, and appointment type.
Table 2.
Description of Tobacco Treatment Program Appointment Characteristics
| APPOINTMENT CHARACTERISTICS (MAXIMUM INTENSITY) | ||
|---|---|---|
| IN-PERSON | TELEHEALTH | |
| Scheduled visits | N = 345 | N = 200 |
| Completed visits/Total visits | N = 208 (60.3%) | N = 150 (75.0%) |
| January 2020 | 78/137 (56.9%) | 18/26 (69.2%) |
| February 2020 | 92/134 (68.7%) | 19/22 (86.3%) |
| March 2020 | 38/74 (51.4%) | 23/35 (65.7%) |
| April 2020 | 0 (—) | 90/117 (76.9%) |
| Appointment outcome | ||
| Completed visit | 208 (60.3%) | 150 (75.0%) |
| Cancelled/no show | 137 (39.7%) | 50 (25.0%) |
| Unique Patients* | 135 | 73 |
Thirty-six patients attended both visit formats.
Table 3.
Adjusted Model of Tobacco Treatment Program Visit Completion
| ADJUSTED MODEL (OUTCOME = COMPLETION) | ||
|---|---|---|
| OR | 95% CI | |
| (Intercept) | 1.6648463 | (1.3163702–2.11532) |
| Telehealth vs. in-person | 2.3027221 | (1.4702514–3.656305) |
| After pandemic declaration vs. before* | 0.6718356 | (0.4345675–1.032593) |
Pandemic period defined as March and April 2020.
CI, confidence interval; OR, odds ratio.
Discussion
Overall, transformation of both the in-person outpatient TTP services and inpatient bedside tobacco treatment counseling was successful. Hospital bedside in-person counseling was quickly transformed into telephone counseling visits, which allowed us to keep both patients and clinicians safe in the context of COVID-19. In addition, after a brief workflow remake and setup phase for ∼10 days, we observed a rapid rise in delivery of individual and group telehealth tobacco treatment services. The coronavirus pandemic served as a catalyst to accelerate expansion and scaling up of tobacco telehealth treatment delivery.
The observed pattern of robust engagement with follow-up telehealth visits, demonstrated by high rates of patient attendance at weekly virtual counseling visits, is encouraging. Research17 indicates that 75% of patients in the general population resume smoking in the first 4 weeks after their quit date. In addition, initial smoking relapse is a common experience with cancer patients.18,19 Moreover, patient acceptance of a high dose of counseling and medications at the same time leads to the highest of long-term quit rates.10,13,20
Challenges and Lessons Learned
Examination of patient engagement during the rapid transition from in-person to telehealth mode of delivery for tobacco treatment also provided the opportunity to explore patient-, clinician-, and system-level barriers for virtual tobacco treatment delivery. A discussion of challenges and lessons learned follows along with potential solutions that may be useful to other health systems transitioning to a telehealth platform to provide tobacco treatment services.
Patient Barriers
Despite overall high patient acceptance with tobacco telehealth treatment, some patients experienced discomfort navigating audiovisual components of their digital devices—smartphones, iPad/computers, with a subgroup of our patients (typically older, ages 65–80 years), at times resulting in challenges with telehealth setup. Often initial resistance was overcome by follow-up telephone support and technical assistance provided by our clinical support and Information Technology (IT) staff, and/or more digitally savvy family members (e.g., grandchildren) who assisted patients with telehealth setup. Nevertheless, we found that there is a “digital divide,”21,22—some patients will not be as comfortable using telehealth technology and other societal barriers (i.e., costs) prevent some people with lower income and some minorities have older digital equipment and less access to functioning bandwidth. As New York City has been described as the epicenter of the coronavirus pandemic in the United States, many of our patients were experiencing noteworthy surges in anxiety related to the stress of the epidemic, and in some cases, this anxiety may have been compounding these IT issues exacerbating the “digital divide.” In contrast, we have been able to conduct visits by using telehealth with virtual translators providing greater access to tobacco treatment services for many non-English speaking patients.
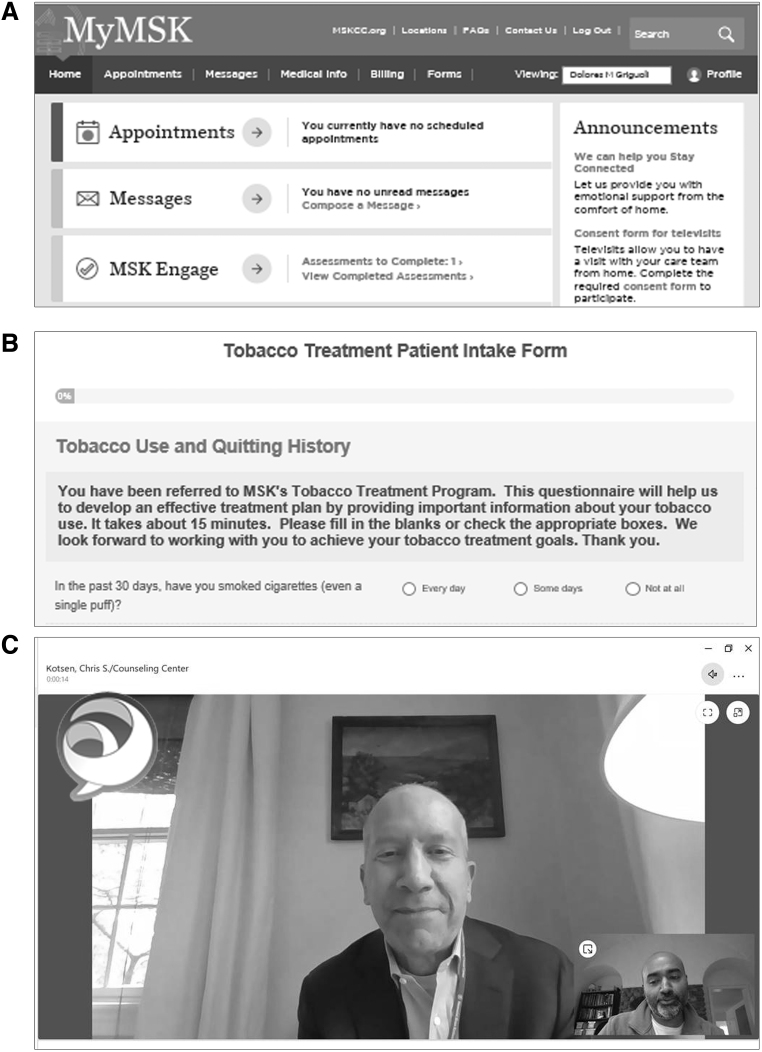
Micro (Hospital) Systems and Clinician Barriers
MSK has been using a Cisco Jabber® videoconference application (Cisco, San Francisco, CA) that is HIPAA compliant and encrypted for TeleOncology services. Current workflows illustrate the need for patients to preregister on the MSK patient portal before the first visit (i.e., username and passwords) as detailed in Fig. 7A and completing our TTP intake form (Fig. 7B). Step two involves setup with the Cisco Jabber Guest app for the actual telehealth visit (Fig. 7C), with functionality that depends on the type of digital device used—smart phone, iPad, apple computer, or PC computer. While uploading the app, there are multiple steps (allowing downloads to computer camera and audio, etc.), which, for some patients, can lead to difficulties causing frustration, getting stuck, or giving up on the device.
Fig. 7.
(A) Screenshots of patient portal, (B) intake forms, and (C) Cisco Jabber® telehealth visit. Used with permission.
In addition, with three practicing TTP clinicians working remotely, ∼8–10 different administrative support staff quickly became experts linking patients to the IT department, transferring multiple phone lines, communicating with each other, transferring “calls,” troubleshooting IT difficulties, and providing unified messaging to anxious patients. Our support staff and clinicians transitioned from in-person clinic operations to working from home within a 2-week period. Getting support staff and faculty fully set up with remote home computers was expedited by using mobile hospital telephones to transform an in-person clinic counseling center into a virtual treatment clinic. Finally, this rapid re-engineering of clinical workflow occurred within a context of pandemic anxiety and a large cancer care setting ramping up the use of telehealth by dozens of other clinical departments (medical oncology, surgery, radiation, etc.), leading to a surge for telehealth setup support and patient demand. Clinicians needed to accelerate their comfort levels with navigating IT platforms, cameras, audio, and troubleshooting with patients about home privacy, and limited wireless access. In a few instances, a switch to FaceTime platform was needed. Also, ∼15% of patients reported digital obstacles that could not be overcome, so the clinician switched to traditional telephone visit format.
Critical to our rapid telehealth transformation was leveraging systems-level problem-solving during bimonthly TelePsych check-in meetings. This committee includes our service chief, director of TeleOncology, IT staff, multiple administrators, our counseling center director, and other clinicians in the psychiatry department who render telehealth services. Ongoing meetings focus on identifying and troubleshooting workflow processes, IT and device barriers, and overcoming clinician and patient barriers to improve the patient experience.
Macro Systems Barriers
Before the COVID-19 pandemic, the U.S. health care system has not consistently provided insurance coverage for telehealth services. These fragmented telehealth policies have created ambiguity for health care administrators considering expanding hospital-based telehealth services. However, in late March, Medicare began loosening some restrictions enabling greater access to telehealth services for beneficiaries.23 During this public health emergency, patients have been able to receive treatment safely and comfortably at home, group psychotherapy is now a covered benefit, telehealth services are billable across state lines, and other changes are rapidly evolving to better align with the way clinical care is being practiced. For billing purposes, next to the CPT code rendered, clinicians add a telehealth modifier (GT), although some private insurance plans are requesting a 95 CPT modifier. In the case of tobacco dependence treatment, insurance billing barriers lead to lower utilization on a population-wide basis,10,16,24 and now that clinicians are more incentivized to provide virtual care, a rapid paradigm shift is occurring, which could likely lead to the sustainability for TTPs within health care systems.
Limitations
Many patients are not currently working or working from home, so it is unclear whether the trends observed for greater patient engagement in tobacco telehealth treatment will be sustained. At the present time, it is unknown as to whether Medicare regulations that have been loosened will be permanent or will return to prepandemic policies that disincentivize hospital systems for telehealth care delivery. These regulations impact reimbursement for a large portion of our patient population. However, most state laws have already mandated that private insurance plans and Medicaid must reimburse telehealth services at in-person rates.
Emergence of Group Tobacco Treatment Within Teleoncology Platforms
Although MSK introduced TeleOncology treatment services since 2018, our TTP is the first MSK clinical service to offer treatment in a group telehealth format. Despite two successful group telehealth IT demonstrations with staff only, our first “live” group treatment in February was unsuccessful, as we encountered technical roadblocks between our IT Cisco Jabber link and the EMR scheduling system, through the patient portal, leading to patients' devices being unable to see and hear the clinician. As a result, patient visits were transferred into individual telehealth visits for that week. However, by March 18, 2020, after IT changes in the Cisco Jabber build of a “bridge,” this began working more effectively with group members who became able to interact with each other and the treating psychologist in the virtual setting. By April 8, 2020, we successfully coordinated simultaneous treatment with 8 patients at once (across hundreds of miles involving three states) into a wonderful gallery view, and by April 15, 2020, we have already scaled up services, conducting two separate group meetings per week, already scheduling 12 patient visits per week.
The 2020 SGR on smoking cessation10 reported that traditional in-person group treatment format has lower reach than other efficacious treatments, in part due to travel barriers, transportation costs, lost work time, and childcare issues. In contrast, in-person group treatment modality is very efficient and has one of the largest effect sizes of all treatment formats, based on randomized controlled trials (RCTs) and treatment in real-world settings.13,25,26 Our promising initial experience rolling out group telehealth tobacco treatment with cancer patients demonstrates strong feasibility and engagement for this novel group treatment format.
Conclusions
We have successfully transformed bedside inpatient counseling to telephone counseling, and our in-person ambulatory clinic has been rapidly transformed to a virtual tobacco treatment clinic. Hospital systems considering engaging in TTP telehealth services can benefit from developing a telehealth oversight committee and holding regular meetings involving clinicians, support staff, administrators, and telehealth IT staff to establish and maintain smooth clinical workflow. The selection of a user-friendly telehealth platform is critical for patient setup and clinical workflows. In addition, telehealth group tobacco treatment was found to be feasible and able to address many travel barriers typically associated with lower attendance. The coronavirus pandemic's impact on patient motivation for tobacco dependence treatment may be conceptualized as a catalyzing “teachable moment.” Further research involving RCTs of individual and group telehealth, particularly in cancer centers, which examines long-term quit rates and cost-effectiveness, will be critical to further expand telehealth tobacco treatments.
Acknowledgments
We gratefully acknowledge the assistance of the TeleOncology Department at MSK: Christian Otto, Joseph McCabe, Regi Phillips, Jennie Huang, Anna Boyko, Cara Stern, and Sofia Fatalevich. In addition, we thank the Tele Psych Administrative Support Team in the Department of Psychiatry and Behavioral Sciences: Christian Nelson, Kylie Cotter, Kristin O'Donoghue, Jashonna Harris, Vikki Mills, Dionne Birkbeck, Shoshana Paul, and Reeja Thomas, as well as other office and care coordinators.
Disclosure Statement
C.K. and L.C.-H. have received honorariums from the Lung Cancer National Training Network Advisory Board, University of Louisville. No other competing financial interests exist.
Funding Information
This study was supported by grants from the National Cancer Institute, Moonshot Cancer Center Cessation Initiative (C3I) 3P30CA008748.
References
- 1. Center for Disease Control. Social distancing, quarantine, and isolation. 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html (last accessed April28, 2020).
- 2. World Health Organization. Advice for public. 2020; Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (last accessed April28, 2020)
- 3. United States Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health. Atlanta, GA. 2014 [Google Scholar]
- 4. Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med 2020;M20-1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med 2020. [Epub ahead of print]; DOI: 10.1056/NEJMoa2007621 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Smoking cessation. NCCN, 2020 [Google Scholar]
- 8. Tzelepis F, Paul CL, Williams CM, et al. Real-time video counselling for smoking cessation. Cochrane Database Syst Rev 2019 [Epub (November 7, 2019] DOI: 10.1002/14651858.CD012659.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fiore MC, D'Angelo H, Baker T. Effective cessation treatment for patients with cancer who smoke-the fourth pillar of cancer care. JAMA Netw Open 2019;2:e1912264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. United States Department of Health and Human Services. Smoking Cessation. A Report of the Surgeon General. Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health. Atlanta, GA. 2020 [Google Scholar]
- 11. Hajek P. Withdrawal-oriented therapy for smokers. 1989;84:591–598 [DOI] [PubMed] [Google Scholar]
- 12. Yalom I, Leszcz M. The theory and practice of group psychotherapy, 5th ed. New York, NY, US: Basic Books, 2005 [Google Scholar]
- 13. Fiore MC, Jaén CR, Baker T, et al. Clinical practice guideline: Treating tobacco use and dependence: 2008 Update. United States Department of Health and Human Service; Public Health Service. Rockville, MD, 2008 [Google Scholar]
- 14. Cinciripini PM, Karam-Hage M, Kypriotakis G, et al. Association of a comprehensive smoking cessation program with smoking abstinence among patients with cancer. JAMA Netw Open 2019;2:e1912251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ostroff JS, Park ER. Results from a Randomized Controlled Comparative Effectiveness Trial of Tobacco Treatment in Cancer Care. Annual Society for Nicotine and Tobacco Research Annual Meeting, San Francisco, CA, 2019 [Google Scholar]
- 16. Bloom EL, Burke MV, Kotsen C, et al. Billing practices among US tobacco use treatment providers. J Addict Med 2018;12:381–386 [DOI] [PubMed] [Google Scholar]
- 17. Zhu SH, Pierce JP. A new scheduling method for time-limited counseling. Prof Psychol Res Pr 1995;6:624–625 [Google Scholar]
- 18. Gritz ER, Schacherer C, Koehly L, Nielsen IR, Abemayor E. Smoking withdrawal and relapse in head and neck cancer patients. Head Neck 1999;21:420–427 [DOI] [PubMed] [Google Scholar]
- 19. Simmons VN, Litvin EB, Jacobsen PB, et al. Predictors of smoking relapse in patients with thoracic cancer or head and neck cancer. Cancer 2013;119:1420–1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Siu AL. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2015;163:622–634 [DOI] [PubMed] [Google Scholar]
- 21. Perrin A, Turner E Smartphones help blacks, Hispanics bridge some—but not all—digital gaps with whites. Pew Research Center, 2019. Available at https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites (last accessed July2, 2020).
- 22. Webb Hooper M, Carpenter K, Payne M, Resnicow K. Effects of a culturally specific tobacco cessation intervention among African American Quitline enrollees: A randomized controlled trial. BMC Public Health 2018;18:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Medicare & Medicaid Services. Physicians and Other Clinicians: CMS Flexibilities to Fight COVID-19. CMS.gov Available from: https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf (last accessed July2, 2020)
- 24. Nolan MB, Warner DO. Perioperative tobacco use treatments: Putting them into practice. BMJ 2017;358:j3340. [DOI] [PubMed] [Google Scholar]
- 25. Kotsen C, Santorelli ML, Bloom EL, et al. A narrative review of intensive group tobacco treatment: Clinical, research, and US policy recommendations. Nicotine Tob Res 2019;21:1580–1589 [DOI] [PubMed] [Google Scholar]
- 26. Public Health England. Models of delivery for stop smoking services: Options and evidence. London, England: PHE Publications, 2017, gateway number 2017342 [Google Scholar]