Abstract
OBJECTIVE.
The purpose of the present study is to determine whether abstinence from ejaculation before undergoing multiparametric prostate MRI increases seminal vesicle (SV) volume and therefore improves diagnostic interpretation of the SVs.
MATERIALS AND METHODS.
This retrospective study included 238 patients who underwent 3-T MRI of the prostate over a 4-month period. Patients were requested to complete a questionnaire that asked how long it had been since their last ejaculation (i.e., < 3 days vs ≥ 3 days). Forty-two patients (mean patient age, 62.0 years) indicated that it had been less than 3 days since their last ejaculation and were designated as group 1, whereas the remainder indicated an interval of 3 days or more since their last ejaculation. A group of 42 age-matched subjects (mean patient age, 62.1 years) were randomly selected from the remaining 196 patients and were designated as group 2. SV volumes were measured manually. Two radiologists who were blinded to group assignment and patient characteristics scored the right and left SVs separately to determine diagnostic interpretability, which was scored on a 3-point scale as follows: a score of 1 denoted that the SVs were not dilated and the score was nondiagnostic, a score of 2 indicated that the SVs were not dilated but the score was diagnostic, and a score of 3 denoted that the SVs were dilated and the score was diagnostic. Volume differences and interpretability scores were analyzed using a t test. Interobserver agreement was analyzed using the Cohen kappa statistic. A separate analysis was performed to evaluate differences in diagnostic interpretability for patients 60 years and younger versus patients older than 60 years, by use of the chi-square test and relative risk ratio analysis.
RESULTS.
The right, left, and total SV volumes for group 1 were 3.1 mL, 2.9 mL, and 6.0 mL, respectively, whereas those for group 2 were 4.7 mL, 4.1 mL, and 8.8 mL, respectively (p = 0.011). The mean interpretability scores for group 1 and group 2 were 2.0 and 2.5, respectively. For group 1, reader 1 and reader 2 assigned a nondiagnostic score for 10 and 13 patients, respectively, whereas for group 2, they assigned a nondiagnostic score for two and five patients, respectively (p = 0.01, for reader 1; and p = 0.03, for reader 2). For men in group 1 who were older than 60 years, reader 1 and reader 2 gave a nondiagnostic score for nine and 11 patients, respectively; whereas for men in group 2 who were older than 60 years, the readers gave a nondiagnostic score for two and five patients, respectively (p = 0.01, for reader 1; and p = 0.05, for reader 2).
CONCLUSION.
For men older than 60 years, abstinence from ejaculation for 3 or more days before undergoing MRI examination resulted in larger SV volumes and lower rates of nondiagnostic evaluation and therefore might improve evaluation of SV invasion on multiparametric MRI. The difference is less striking in men 60 years and younger.
Keywords: ejaculation, MRI, prostate, seminal vesicles
Prostate cancer is the most common noncutaneous cancer in men, with 220,800 new cases estimated to develop among men in the United States in 2015 [1]. The management of prostate cancer requires accurate timely diagnosis and staging. Multiparametric MRI is increasingly used for prostate cancer detection, localization, and staging [2]. One commonly assessed sign of extraprostatic extension is involvement of the seminal vesicles (SVs), which increases the cancer stage to T3. However, assessment of the SVs requires that the SVs be sufficiently distended to assess cancer involvement.
It has long been thought that abstinence from ejaculation for 3 days before undergoing multiparametric MRI leads to improved diagnostic accuracy for the SVs; however, scant evidence exists to support this [3, 4]. Prostate Imaging and Reporting and Data System, version 2, which is the most recent version of the recommendations for prostate MRI, confirms that this practice of recommending abstinence from ejaculation has been adopted by many radiologists, although it refrains from completely endorsing the practice [3]. Thus, the aim of the present study is to determine whether abstinence from ejaculation before undergoing multiparametric MRI affects SV volume and, therefore, the diagnostic interpretability of the SVs.
Materials and Methods
Patient Population and Study Design
This retrospective evaluation included 238 patients who underwent 3-T MRI of the prostate between June 2015 and September 2015. The study was approved by the institutional review board at NIH, and informed consent was obtained from each study participant. Patients were asked to complete a questionnaire that asked them to estimate the number of days since their last ejaculation (< 3 days vs ≥ 3 days). Forty-two patients (mean age, 62.0 years; median age, 62.5 years; mean [± SD] prostate specific antigen [PSA] level, 10.1 ± 2.1 ng/mL), 17 of whom were 60 years or younger and 25 of whom were older than 60 years, responded that they had abstained from ejaculation for less than 3 days and were designated as group 1. The remaining patients indicated that 3 or more days had passed since their last ejaculation. Because the SV volume changes with age, it was important to ensure that the two patient groups were evenly matched with regard to age [4]. Thus, a subset of 42 age-matched subjects (mean age, 62 years; median age, 62.5 years; mean PSA level, 7.0 ± 0.6 ng/mL) were randomly selected from the remaining 196 patients and were designated as group 2. Group 2 included 16 patients who were 60 years or younger and 26 patients who were older than 60 years. Patient age ranged from 49 to 78 years (mean ± standard error of the mean [SEM]; 62 ± 0.9 years) (Table S1, supplemental data, can be viewed in the AJR electronic supplement to this article, available at www.ajronline.org).
Three patients in whom gross invasion of almost all SVs by prostate cancer was noted were excluded from the study because it was not possible to measure the volume of healthy SVs in these patients. The volume of healthy SVs also could not be measured in 11 patients who had undergone prior treatment (five of whom had undergone radiotherapy, three of whom had undergone prostatectomy, and three of whom had undergone focal therapy).
MRI Technique
A 3-T MRI unit (Achieva, Philips Healthcare) that used a combination of an anterior 16-channel torso-cardiac coil (SENSE, Invivo) and an endorectal coil (Medrad eCoil, Bayer Healthcare) was used for imaging examinations. The prostate MRI protocol included triplane T2-weighted MRI, axial DWI (with evenly spaced b values of 0–750 s/mm2) and an apparent diffusion coefficient map and a high b value DWI with a b value of 2000 s/mm2) and dynamic contrast-enhanced MRI. However, for the analyses, only triplane T2-weighted images were used. The pulse sequences and parameters of the triplane T2-weighted MRI used in the present study are presented in Table S2 (supplemental data, which can be viewed in the AJR electronic supplement to this article, available at www.ajronline.org).
MRI Analysis
Each SV has a shape that has elements resembling a cylinder and a cone (Fig. 1). On the basis of the assumption that SV volumes were the approximate mean value of the volumes of both a cylinder and a cone that had the same height and radius, we calculated the SV volumes on the basis of T2-weighted MR images with the use of the following formula: V = π × r2 x / x (13 / 20), where V denotes volume, r denotes maximum width of seminal vesicles, and x denotes maximum length of seminal vesicles from ejaculatory ducts to the tip [5] (Fig. 1). Volume validation was done for six patients, and the formula was shown to be consistent with planimetric volume with a deviation of −5.6% to 1.9%. The volumes of the right and left SVs were calculated for each group.
Fig. 1—
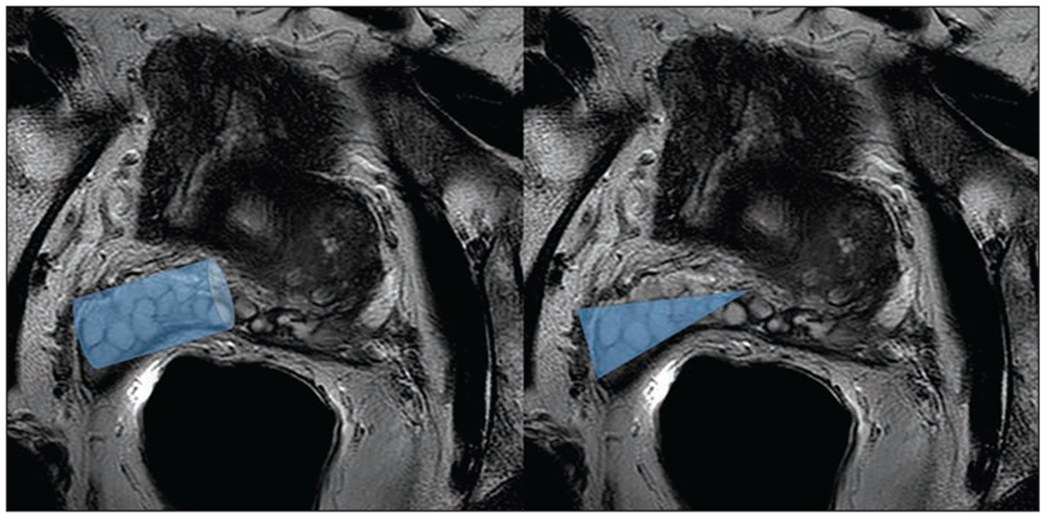
63-year-old man with serum PSA of 6.2 ng/mL who underwent prostate MRI. T2-weighted multiplanar reformatting MR images of seminal vesicles (SVs) show SV volumes of areas resembling cylinder (left) and cone (right) that have same height and radius.
The SVs were evaluated by two experienced radiologists who were blinded to patient age and group information. With the use of a commercial PACS, SVs were graded as follows: a score of 1 denoted that the SVs were not dilated and the score was nondiagnostic, 2 indicted that the SVs were not dilated but the score was diagnostic, and 3 denoted that the SVs were dilated and the score was diagnostic (and was to be used as a reference) (Fig. 2).
Fig. 2—
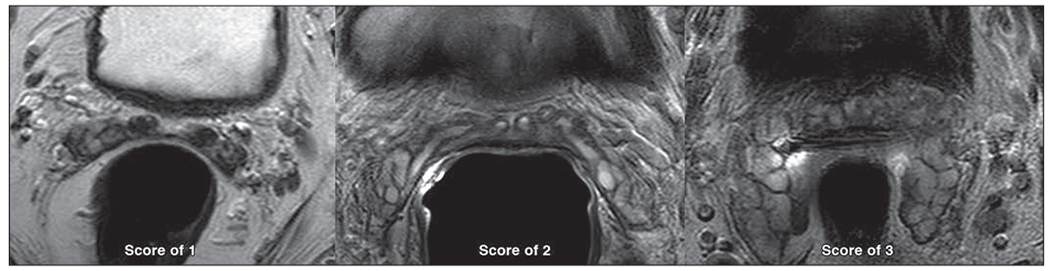
Three patients underwent prostate MRI. Sample T2-weighted multiplanar reformatting MR images of seminal vesicles (SVs) show studies assigned score of 1 (left) for 77-year-old man, which denoted that SVs were not dilated and score was nondiagnostic; score of 2 (middle) for 59-year-old man, which indicated that SVs were not dilated but score was diagnostic; or score of 3 (right) for 71-year-old man, which denoted that SVs were dilated and score was diagnostic.
Statistical Analysis
The volume differences and interpretability scores for the two patient groups were analyzed using a t test, and interobserver agreement for diagnostic interpretability was analyzed using the Cohen kappa statistic. The chi-square test was used to analyze the interpretability score difference when the score was categorized as nondiagnostic or diagnostic. The relative risk ratio was used to assess the risk of obtaining a suboptimal SV evaluation on the basis of the time since the last ejaculation, with the use of statistical software (SPSS, version 23, SPSS-IBM). For the results, p < 0.05 was considered to denote statistical significance.
Results
Seminal Vesicle Volumes
The right, left, and total SV volumes for group 1 were 3.1 mL, 2.9 mL, and 6.0 mL, respectively, and those for group 2 were 4.7 mL, 4.1 mL, and 8.8 mL, respectively (p = 0.011). There was a statistically significant difference between the SV volumes for group 1 versus those for group 2 (6.0 vs 8.8 mL, respectively; p = 0.011) (Table S3, supplemental data, which can be viewed in the AJR electronic supplement to this article, available at www.ajronline.org) (Fig. 3). There was a negative correlation between patient age and SV volumes (Pearson correlation coefficient, −0.226; p = 0.038). There was a statistically significant difference in the volume noted between patients 60 years and younger (8.7 mL) and patients older than 60 years (6.6 mL) (p < 0.05). No correlation was noted between patient age and the serum PSA level or the PSA density. In patients 60 years or younger, the total SV volumes for group 1 and group 2 were 7.9 mL and 9.5 mL, respectively (p = 0.280). In patients older than 60 years, the total SV volumes for group 1 and group 2 were 4.7 mL and 8.4 mL, respectively (p = 0.000114) (Fig. 4).
Fig. 3—
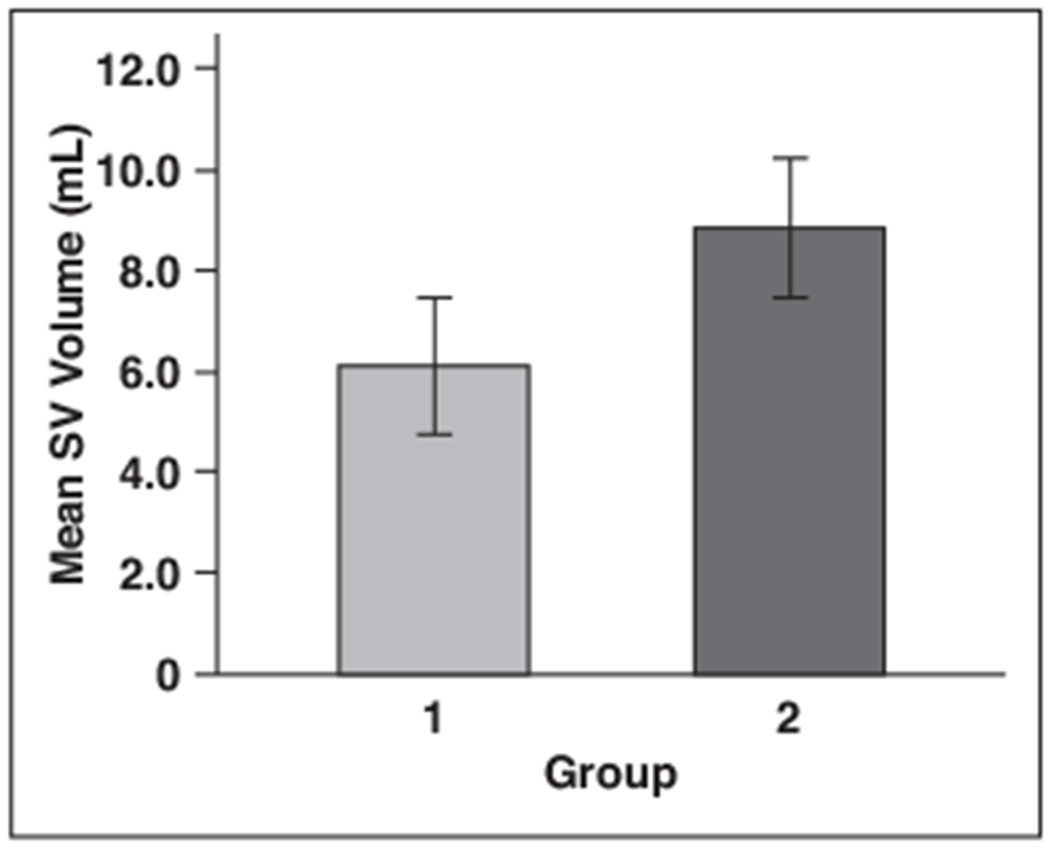
Bar graph of seminal vesicle (SV) volumes in 42 men who abstained from ejaculation for less than 3 days before undergoing prostate MRI (i.e., group 1) and 42 age-matched randomly selected men who abstained from ejaculation for 3 days or more (i.e., group 2). Data are mean volumes (expressed in milliliters) and standard errors.
Fig. 4—
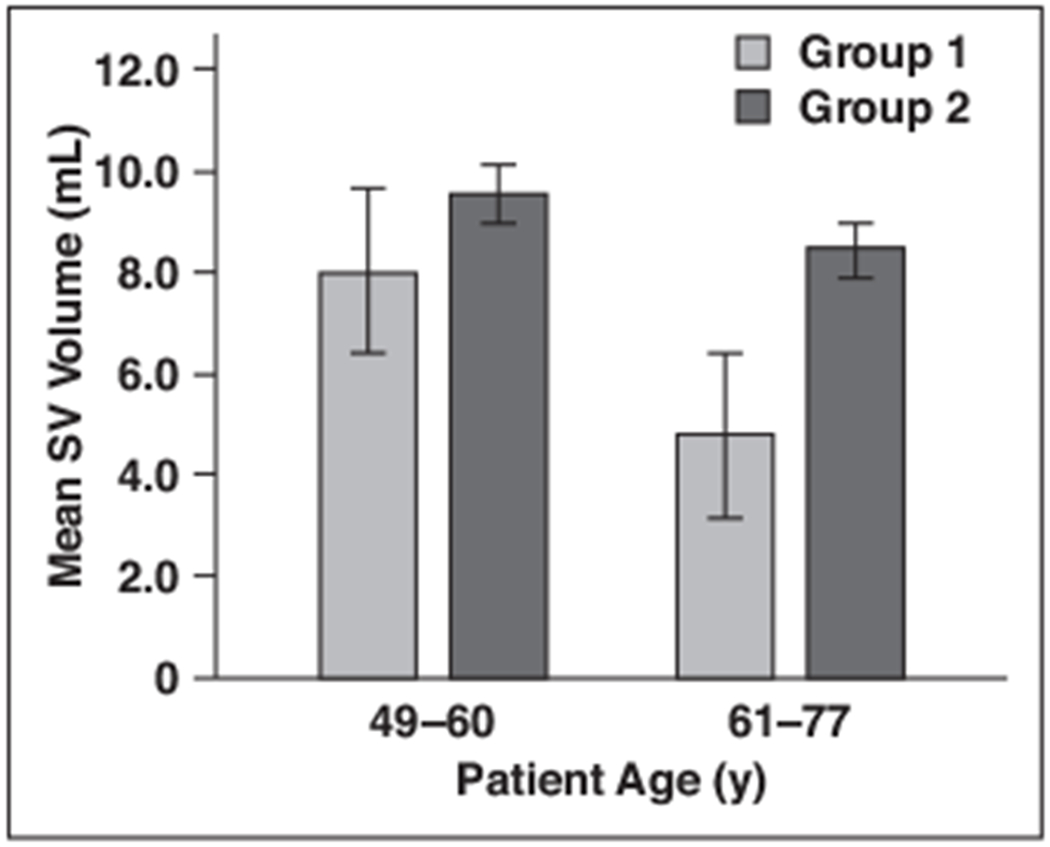
Bar graph of seminal vesicle (SV) volumes in 42 men who abstained from ejaculation for less than 3 days before undergoing prostate MRI (i.e., group 1) and 42 age-matched randomly selected men who abstained from ejaculation for 3 days or more (i.e., group 2), by age. Data are mean volumes (expressed in milliliters) and standard errors.
Interpretability Scores
Cohen kappa statistical analysis revealed a coefficient of 0.7 (denoting good agreement) between the two readers’ interpretability scores. For readers 1 and 2, the mean interpretability score for group 1 and group 2, as based on a 3-point scale, was 2.0 and 2.5, respectively (Table 1). For group 1, reader 1 and reader 2 assigned a nondiagnostic score for 10 and 13 patients, respectively, whereas for group 2, they assigned a nondiagnostic score for two and five patients, respectively (p = 0.01, for reader 1; and p = 0.03, for reader 2). The interpretability scores for each group are shown in Table 2. According to reader 1, a total of 23.8% of the SVs in group 1 and 4.7% of the SVs in group 2 were not diagnostic. According to reader 2, a total of 30.9% of the SVs in group 1 and 11.9% of the SVs in group 2 were not diagnostic. The relative risk ratios were 5 and 2.6 for the two readers, for patients with nondiagnostic studies who abstained from ejaculation for less than 3 days.
TABLE 1:
Interobserver Agreement of Readers 1 and 2 for the Overall Patient Population
| Reader 1 Score | Reader 2 Score | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| 1 | 12 | 0 | 0 |
| 2 | 6 | 23 | 8 |
| 3 | 0 | 2 | 33 |
Note—Data are no. of patients.
TABLE 2:
Overall Interpretability Scores for Groups 1 and 2, According to Reader 1 and Reader 2
| Reader, Group | Nondiagnostic Score | Diagnostic Score | Relative Risk | p |
|---|---|---|---|---|
| Reader 1 | 5 | 0.01 | ||
| Group 1 | 10 (23.8) | 32 (76.2) | ||
| Group 2 | 2 (4.7) | 40 (95.2) | ||
| Reader 2 | 2.6 | 0.03 | ||
| Group 1 | 13 (31.0) | 29 (69.1) | ||
| Group 2 | 5 (11.9) | 37 (88.1) | ||
Note—Except where noted otherwise, data are number (%) of patients. Percentages may not total 100% because of rounding. Group 1 included 42 men who abstained from ejaculation for less than 3 days before undergoing prostate MRI, and group 2 included 42 age-matched randomly selected men who abstained from ejaculation for 3 days or more.
The risk of studies being nondiagnostic was higher in men older than 60 years who did not refrain from ejaculation for 3 days or more. For men 60 years and younger, reader 1 and reader 2 assigned a nondiagnostic score for one in 17 patients in group 1 and for two of 17 patients in group 1; both readers assigned a nondiagnostic score for zero of 16 patients in group 2 (p = 0.325, for reader 1; and p = 0.157, for reader 2). For men older than 60 years, reader 1 and reader 2 assigned a nondiagnostic score for nine and 11 of the 25 patients in group 1, respectively, and for two and five of the 26 patients in group 2, respectively (p = 0.01, for reader 1; and p = 0.057, for reader 2). Thus, for men older than 60 years, the effect of 3 days of abstinence from ejaculation is more prominent than is that for men 60 years or younger (Tables 3 and 4).
TABLE 3:
Interpretability Scores for Patients 60 Years or Younger in Groups 1 and 2, According to Readers 1 and 2
| Reader, Group | Nondiagnostic Score | Diagnostic Score | p |
|---|---|---|---|
| Reader 1 | 0.32 | ||
| Group 1 | 1 (5.8) | 16 (94.1) | |
| Group 2 | 0 (0) | 16 (100.0) | |
| Reader 2 | 0.15 | ||
| Group 1 | 2 (11.7) | 15 (88.3) | |
| Group 2 | 0 (0) | 16 (100.0) | |
Note—Except where noted otherwise, data are number (%) of patients. Percentages may not total 100% because of rounding. Group 1 included 17 men who were 60 years or younger who abstained from ejaculation for less than 3 days before undergoing prostate MRI, and group 2 included 16 age-matched randomly selected men who abstained from ejaculation for 3 days or more.
TABLE 4:
Interpretability Scores for Patients Older Than 60 Years in Groups 1 and 2, According to Readers 1 and 2
| Reader, Group | Nondiagnostic | Diagnostic | Relative Risk | p |
|---|---|---|---|---|
| Reader 1 | 4.68 | 0.01 | ||
| Group 1 | 9 (36.0) | 16 (64.0) | ||
| Group 2 | 2 (7.6) | 24 (92.3) | ||
| Reader 2 | 2.28 | 0.057 | ||
| Group 1 | 11 (44.0) | 14 (56.0) | ||
| Group 2 | 5 (19.2) | 21 (80.8) | ||
Note—Except where noted otherwise, data are number (%) of patients. Percentages may not total 100% because of rounding. Group 1 included 25 men older than 60 years who abstained from ejaculation for less than 3 days before undergoing prostate MRI, and group 2 included 26 age-matched randomly selected men who abstained from ejaculation for 3 days or more.
Discussion
In the present study, we identified statistically significant differences in the SV volumes of men who abstained from ejaculation for at least 3 days before undergoing prostate MRI, compared with those who abstained for less than 3 days. Patients in group 2 (who abstained for at least 3 days) had larger SV volumes than did patients in group 1 (who abstained for less than 3 days). Although the volume differences were statistically significant, it was unclear whether they had a meaningful effect on diagnostic interpretability. Thus, we performed a two-reader study in which readers were asked to judge the interpretability of the SVs. This study revealed that the diagnostic interpretability of SVs was judged to be higher in group 2 than in group 1. For approximately 24–31% of the SVs of patients in group 1, scans were not diagnostic, whereas for 5–12% of patients in group 2, scans were nondiagnostic. Thus, failure to abstain from ejaculation for 3 days or more increased the risk of nondiagnostic scan results for the SVs.
However, there is reason to expect that this could be an age-related phenomenon. In patients older than 60 years, SV volume decreases rapidly, and significant volume differences in this cohort were noted between patients 60 years or younger and patients older than 60 years (p = 0.05). Thus, when interpretability scores were analyzed according to age groups, no statistically significant differences in either volume or interpretability scores were observed between group 1 and group 2. For men older than 60 years, the relative risk of a nondiagnostic scan increased by 2.3-fold to 4.7-fold for men who abstained from ejaculation for less than 3 days before undergoing MRI. Thus, to reduce the rate of nondiagnostic interpretation of SVs, abstinence from ejaculation for 3 days or more is more important for patients older than 60 years. We hypothesize that the rate of replenishment of seminal fluid is higher in younger men and that the effects of abstinence thus are less apparent.
Only a very limited number of studies focus on the effect of ejaculation on MRI findings for the prostate and SVs. Using sonographic evaluation, Fuse et al. [6] showed that SV volume diminished after ejaculation. The mean length of the right and left SVs was 34 and 35 mm, respectively, before ejaculation and was 30 and 29 mm, respectively, after ejaculation (p < 0.05), whereas the mean widths of the SVs were not different before and after ejaculation [6]. Another study reported differences in SV volume before and after ejaculation in eight young men (mean age, 23 years). It was shown that the SV volume decreased by an average of 41% (median, 44.5%; p = 0.004) after ejaculation [7]. However, the effect of the duration of abstinence on the diagnostic interpretability of the SVs was not evaluated, and the age of the subjects was not relevant to the interpretation of MR images of prostate cancer [4, 8]. Nonetheless, Prostate Imaging and Reporting and Data System, version 2, mentions that patients should refrain from ejaculation for 3 days before undergoing the MRI examination, to maintain the maximum distention of the SVs, although the basis for this recommendation was not firmly established [3, 4].
The present study has several limitations. First, our cohort was relatively small. Larger-scale studies are needed to further confirm these findings, although the magnitude of the differences suggests that a larger study will simply confirm the value of at least 3 days of abstinence in distending the SVs. Second, we did not investigate the effect of other potentially confounding factors (e.g., race or ethnicity) or medications (e.g., α-blockers) that may confound SV volumes by inhibiting contraction. Finally, we studied only the subjective impressions of the two readers, not the actual staging outcomes. Although we consider this a worth-while goal, it would require an extremely large group of patients to accrue sufficient numbers of patients in both groups (60 years and younger vs older than 60 years) who have SV invasion. We think that a reasonable interpretation of these data is that at least 3 days of abstinence could improve assessment of the SVs, at least for men older than 60 years. It should be noted that men are asked to abstain from ejaculating for 3 days before a serum PSA test is performed.
In conclusion, abstinence from ejaculation for 3 days or more before undergoing prostate multiparametric MRI resulted in larger SV volumes and improved diagnostic scores. The effect was more pronounced among patients older than 60 years, but it was observed to a lesser extent among men 60 years and younger. Therefore, in view of the absence of cost, and because men receive similar instructions before samples are acquired for PSA tests, this is an easily implemented patient preparation procedure that may improve the diagnostic value of multiparametric MRI, especially in men older than 60 years.
Supplementary Material
Footnotes
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as representing the views of the National Institutes of Health.
Supplemental Data
Available online at www.ajronline.org.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015; 65:5–29 [DOI] [PubMed] [Google Scholar]
- 2.Johnson LM, Turkbey B, Figg WD, Choyke PL. Multiparametric MRI in prostate cancer management. Nat Rev Clin Oncol 2014: 11:346–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging-Reporting and Data System, 2015, version 2. Eur Urol 2016; 69(1): 16–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akiyama K The volume of the seminal vesicles in general senior population [in Japanese], Nihon Hinyokika Gakkai Zasshi 1994; 85:932–937 [DOI] [PubMed] [Google Scholar]
- 5.Kim B, Kawashima A, Ryu JA, Takahashi N, Hartman RP, King BF Jr. Imaging of the seminal vesicle and vas deferens. RadioGraphics 2009; 29:1105–1121 [DOI] [PubMed] [Google Scholar]
- 6.Fuse H, Okumura A, Satomi S, Kazama T, Katayama T. Evaluation of seminal vesicle characteristics by ultrasonography before and after ejaculation. Urol Int 1992; 49:110–113 [DOI] [PubMed] [Google Scholar]
- 7.Medved M, Sammet S, Yousuf A, Oto A. MR imaging of the prostate and adjacent anatomic structures before, during and after ejaculation: qualitative and quantitative evaluation Radiology 2014; 271:452–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liou CL, Wei JW, Wang AC, et al. Volume of the seminal vesicles and cross-sectional area of the ampulla of vas deferens: measurement on trans abdominal sonography. Chin J Radiol 2005; 30:335–340 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


