Abstract
Background
A relentless flood of information accompanied the novel coronavirus 2019 (COVID-19) pandemic. False news, conspiracy theories, and magical cures were shared with the general public at an alarming rate, which may lead to increased anxiety and stress levels and associated debilitating consequences.
Objectives
To measure the level of COVID-19 information overload (COVIO) and assess the association between COVIO and sociodemographic characteristics among the general public.
Methods
A cross-sectional online survey was conducted between April and May 2020 using a modified Cancer Information Overload scale. The survey was developed and posted on four social media platforms. The data were only collected from those who consented to participate. COVIO score was classified into high vs. low using the asymmetrical distribution as a guide and conducted a binary logistic regression to examine the factors associated with COVIO.
Results
A total number of 584 respondents participated in this study. The mean COVIO score of the respondents was 19.4 (± 4.0). Sources and frequency of receiving COVID-19 information were found to be significant predictors of COVIO. Participants who received information via the broadcast media were more likely to have high COVIO than those who received information via the social media (adjusted odds ratio ([aOR],14.599; 95% confidence interval [CI], 1.608–132.559; p = 0.017). Also, participants who received COVID-19 information every minute (aOR, 3.892; 95% CI, 1.124–13.480; p = 0.032) were more likely to have high COVIO than those who received information every week.
Conclusion
The source of information and the frequency of receiving COVID-19 information were significantly associated with COVIO. The COVID-19 information is often conflicting, leading to confusion and overload of information in the general population. This can have unfavorable effects on the measures taken to control the transmission and management of COVID-19 infection.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-020-00942-0.
Keywords: COVID-19, Information overload, General public
Introduction
Information overload can best be understood as that situation which arises when there is so much relevant and potentially useful information available that it becomes a hindrance rather than a help [1]. Information overload occurs when the level of information is higher than individuals’ information processing capacity, a situation referred to as an “overly information load” [2]. The growing volume of relevant health information over the past decades, especially through internet sources, has amplified the issue of health information overload [3].
The outbreak of 2019 coronavirus disease (COVID-19) in China that spread quickly all over the world was declared pandemic by the World Health Organization (WHO) [4]. The fact that COVID-19 is novel led to generation a of lot of information from different sources. Many of such information are often conflicting, false, or from an ingenuine source. The incessant COVID-19 information received by people on a daily basis may lead to health information overload. However, recent studies have shown that healthy information could safeguard mental health during the COVID-19 pandemic [5].
The United Nations Development Program (UNDP) has stated that “the COVID-19 pandemic is the defining global health crisis of our time and the greatest challenge we have faced since World War Two” [6]. Since the declaration of COVID-19 as a pandemic by the World Health Organization (WHO), information flow has been fast and flowing from various sources ranging from hospitals, co-workers, social media, family, and friends. Not only is the information fast and diverse, but it is also continually changing [7]. It is quite stressful and overwhelming for people to keep up with the constant information influx on COVID-19 which can predispose people to the condition of information overload, making it difficult for them to differentiate which information is reliable and helpful. Information overload can lead people to feel powerless, experience anxiety, fatigue, and paralysis of action, all of which are unhelpful anytime but indeed dangerous in a time of the pandemic. In response, people seek simple but mostly unhelpful information to focus on and, in some cases, avoid information totally [1].
The overwhelming information about the COVID-19 pandemic often makes it difficult to separate fact from fiction and rumor from deliberate efforts to mislead. People may find it challenging to understand and utilize accurate information from many sources at the same time [8]. In this pandemic situation, the general public may be at high risk of experiencing information overload on COVID-19, due to the frequent information in circulation. Therefore, we aimed to evaluate COVID-19 information overload (COVIO) among the general public.
Methods
Study Design/Population
We conducted a cross-sectional study in the form of an online survey (Via Google Surveys ™) over 6 weeks between April and May 2020. Eligible participants included in this study were adults (≥18 years) from the general public, worldwide. The minimum number of participants was determined using single proportion formula [9]. There was no data from a previous study regarding the prevalence of COVID-19 information overload. We, therefore, assumed 50% of participants would have COVID-19 information overload. Assuming a precision of 0.05 at a 95% confidence interval (CI), we calculated the minimum sample size of 384.
Recruitment
Participants were recruited for an online survey (via Google survey) using social media platforms, including Facebook, WhatsApp, LinkedIn, and Twitter. To administer the survey to the target population, an advertisement page was created. The page was designed using Google forms, where the eligibility criteria, survey link (COVID-19 Information overload scale–COVIO scale), and invitation to participate in the study were presented. The survey was designed to ensure that participants were able to make comments, tag friends, and share the advertisement on their profile page, or other social media platforms groups.
Participants were able to access the survey page by clicking on the advertisement, after which they would be directed to the survey page. The page contained information about the study, consent, and the adapted survey scale. Prior to participation in the survey, participants were required to provide informed consent and all responses were collected anonymously. Also, the approval to share the survey advertisement on the social media groups was sought from the group’s administrator.
Procedure
The online survey was designed and reported based on the Checklist for Reporting Results of Internet E-Surveys (CHERRIES), and guidelines for good practice in the conduct and reporting of survey research [10, 11]. The Google survey contained three pages; study/consent information page, sociodemographic information page, and COVIO scale. Participants were required to respond to all the items in the survey. They were also able to review and change their responses, suspend and resume later, or quit the survey at any time. Participants that decline to consent are taken to the end page and were excluded in the final analysis.
The following information was collected from the respondents: demographic characteristics such as age, gender, marital status, highest educational level, employment status, type of employment, nationality, current country of residence, and residence type. Other information collected included source of information overload, frequency of receiving information, and whether the information about COVID-19 was solicited or not.
Outcome Measures
Being a novel disease condition, there was no scale for measuring COVID-19 information overload in the literature. Consequently, we adopted a previously validated cancer information overload (CIO) tool [10] which was also used elsewhere [12]. The original eight-item CIO scale contains a four-point Likert scale, i.e., strongly disagree with a score of 1, disagree 2 points, agree 3 points, and strongly agree with a value of 4 [13]. The original CIO scale was scored by taking the total points obtained by respondents for each item. The scores ranged from a minimum of 8 to a maximum of 32 points. Higher scores indicate a greater degree of health information overload based on the recommendation of Jensen and colleagues [13]. In the modified CIO scale used in this study, we assessed COVIO of participants by retaining the four-point Likert scale per item as well as the method of scoring. The term ‘cancer’ from all items within the original CIO scale was replaced with ‘COVID-19’ to suit the context of our study (Appendix 1).
Data Presentation and Analysis
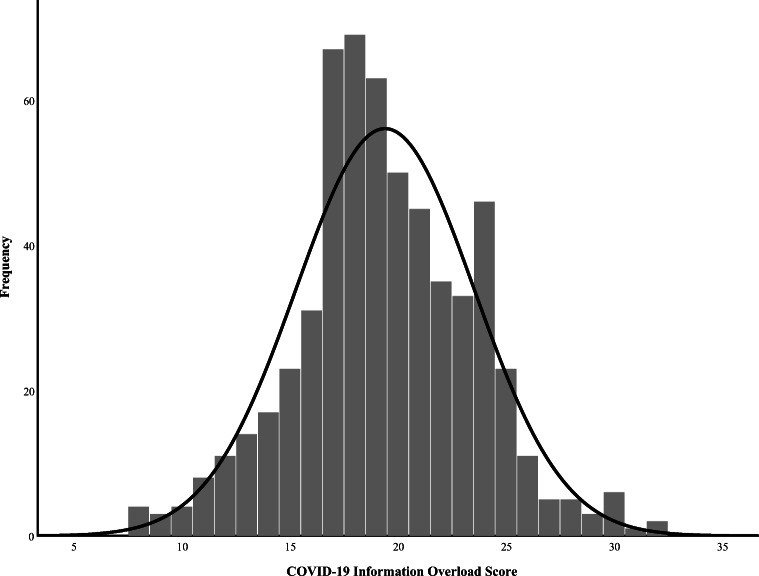
The data collected were exported into Microsoft Excel from the Google Forms, and then into IBM SPSS Statistics Version 24.0 (IBM Corporation: Chicago, IL) for statistical analysis. Categorical variables were presented as frequency and percentages, and numerical data were presented as mean (standard deviation) or median (interquartile range) depending on the normality distribution of the data. The normality distribution of the COVIO scores was checked using the histogram method and Kolmogorov-Smirnov (KS) test. Both methods showed that the COVIO scores were not normally distributed as histogram was skewed to the right and KS p < 0.001. The predictors of COVIO were determined using regression analyses. Binary logistic regression was applied given the non-normal distribution of the COVIO score, and its suitability in identifying independent predictors of a binary outcome variable with controlling confounders [14]. In the regression analysis, a univariable analysis was initially conducted to screen all independent variables for inclusion in the multiple logistic regression (MLR) analysis. From the results of the univariable analysis, variables with p < 0.25 and those considered relevant were included in the MLR [15]. The relevant variables were those with evidence of predicting information overload in the previous literature. Overall, p < 0.05 was considered statistically significant. The results of the MLR were presented as a crude odds ratio (OR) with 95% confidence intervals (CIs), and corresponding p values. The MLR was initially performed using the backward elimination (backward LR) process [16]. In order to allow variables to be maintained in the model for as long as possible, the removal criteria was set at p = 0.10. The process was then repeated using forward selection (forward LR) option and compared before final confirmation of factors associated with COVIO. Multicollinearity between the variables was checked using correlation matrix with higher values indicating multicollinearity. Assumptions of model fit were checked using Hosmer-Lemeshow and Omnibus tests. The final model was presented as adjusted odds ratio [aOR] with 95% confidence intervals (CIs) and corresponding p values in Table 4.
Table 4.
Multiple logistic regression—final model
| Variable | Adjusted OR (95% CI) | p value |
|---|---|---|
| Sources of COVID-19 information | ||
| Social media (SM) | 1 | |
| Broadcast media (BM) | 14.599 (1.608–132.559) | 0.017* |
| SM + BM | 8.132 (0.634–104.296) | 0.107 |
| SM + PM | 6.921 (0.774–61.908) | 0.084 |
| SM + BM + PM (print media) | 0.000 (0.00) | 0.999 |
| Frequency of receiving COVID-19 information | ||
| Every week | 1 | |
| Every day | 1.241 (0.448–3.441) | 0.677 |
| Every hour | 1.834 (0.640–5.255) | 0.259 |
| Every minute | 3.892 (1.124–13.480) | 0.032* |
* = p < 0.05
Results
Recruitment Process of the Study Participants
A total of 584 participants responded to the online survey. Of these participants, 5 (0.9%) declined to proceed with the survey and were excluded, 579 (99.1%) participants with complete responses were included in the final analysis. Figure 1 summarizes the recruitment process of the study participants.
Fig. 1.
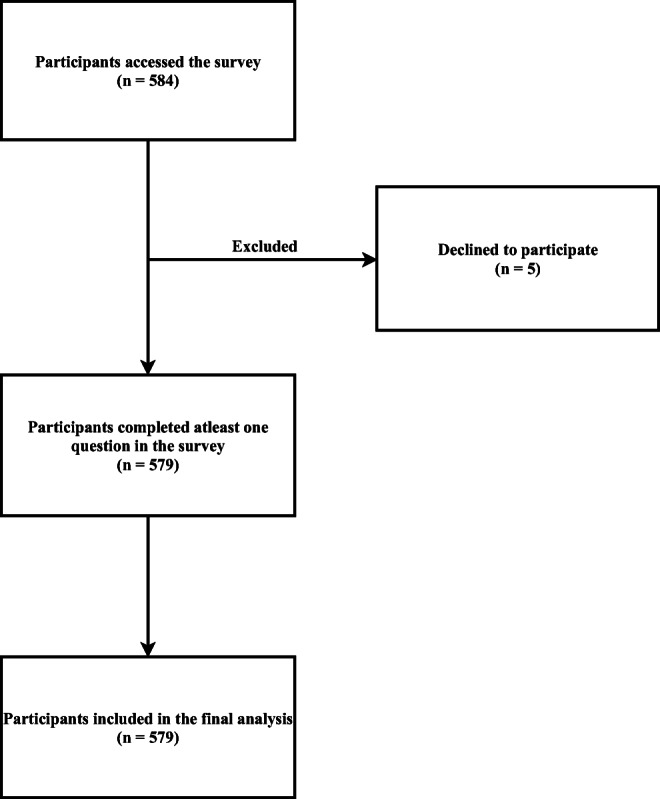
The flowchart of the recruitment process of the study participants
Demographic Characteristics of Respondents
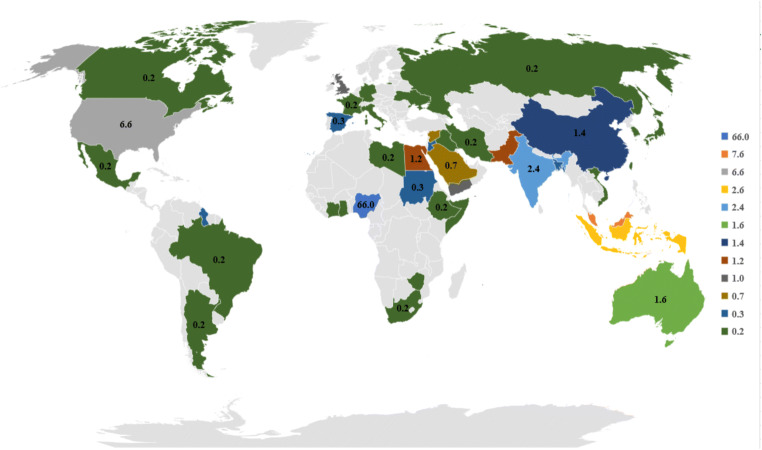
The majority of the respondents were females 335 (57.9%) and the mean age was 33.0 (± 8.7), more than half were married 302 (52.2%), having postgraduate level of education 316 (54.6%) and majority are living in urban settlement 519 (89.6%). In addition, more than half of the respondents are not health-related professionals 302 (52.2%) (Table 1). The percentage distribution of responses to the survey by countries is presented in Fig. 2.
Table 1.
Sociodemographic characteristics of respondents (n = 579)
| Characteristics | Frequency | Percentage (%) |
|---|---|---|
| Age (years) | ||
| Mean (±SD) = 33.0(8.7) | ||
| Gender | ||
| Male | 244 | 42.1 |
| Female | 335 | 57.9 |
| Marital status | ||
| Single | 258 | 44.6 |
| Married | 302 | 52.2 |
| Divorced | 10 | 1.7 |
| Separated | 3 | 0.5 |
| Widowed | 3 | 0.5 |
| Partnered | 3 | 0.5 |
| Highest educational level | ||
| Associate degree | 24 | 4.1 |
| Bachelors | 179 | 30.9 |
| Diploma | 24 | 4.1 |
| Higher National Diploma (HND) | 2 | 0.3 |
| National certificate of education (NCE) | 7 | 1.2 |
| Postgraduate | 316 | 54.6 |
| Primary school certificate | 1 | 0.2 |
| Secondary school certificate | 24 | 4.1 |
| Vocational training | 2 | 0.3 |
| Current employment status | ||
| Full-time work | 280 | 48.4 |
| Not working | 44 | 7.6 |
| Part-time work | 30 | 5.2 |
| Retiree | 3 | 0.5 |
| Self-employed | 48 | 8.3 |
| Student | 174 | 30.1 |
| Professional background | ||
| Health related | 277 | 47.8 |
| Non-health related | 302 | 52.2 |
| Location of residence | ||
| Rural | 60 | 10.4 |
| Urban | 519 | 89.6 |
Fig. 2.
Percentage distribution of responses by countriesa. a = A table showing the complete response has been included as supplementary material (Appendix 2)
Distribution of COVIO
Participants were divided into low COVIO and high COVIO groups based on their level of COVIO. Since there was no cut-off COVIO score for high COVIO in the literature and the distribution of the scores was asymmetrical, a score of 18 and below was considered as low COVIO based on the histogram. (Fig. 3). The determination of the cut-off score based on asymmetrical distribution was supported by a previous study [17].
Fig. 3.
Distribution of COVIO scores among the respondents
Attributes of COVID-19 Information
Table 2 shows that majority of the information on COVID-19 were obtained through a combination of social media and broadcast media 372 (64.2%) and social media alone 189 (32.6%). Most of the information were solicited 212 (36.6%) and received daily 369 (63.7%).
Table 2.
Attributes of COVID-19 Information
| Sources of COVID-19 information | ||
| Social media (SM) | 189 | 32.6 |
| Broadcast media (BM) | 9 | 1.6 |
| SM + BM | 372 | 64.2 |
| SM + PM (print media) | 3 | 0.5 |
| SM + BM + PM | 6 | 1.0 |
| Frequency of receiving COVID-19 information | ||
| Every minute | 40 | 6.9 |
| Every hour | 154 | 26.6 |
| Every day | 369 | 63.7 |
| Every week | 16 | 2.8 |
| Solicitation for COVID-19 information | ||
| Mostly solicited | 104 | 18.0 |
| Solicited | 212 | 36.6 |
| Unsolicited | 161 | 27.8 |
| Mostly unsolicited | 102 | 17.6 |
COVIO scores among the Participants
Item-by-item analysis of COVIO scores is shown in Table 3. The overall mean (±SD) COVIO score was 19.40 (4.12). The lowest and highest scores were 2.0 (0.7) on item 6, and 2.8 (0.7) on item 5, respectively. Among the eight items of the adopted tool, responses from three items (1, 5, and 8) showed higher COVIO score. The items include: “there are so many different recommendations about preventing COVID-19, it is hard to know which ones to follow” 307 (53.0%),” “information about COVID-19 all starts to sound the same after a while 426 (73.6%)” and “I feel overloaded by the amount of COVID-19 information I am supposed to know” 335 (57.9%).
Table 3.
Item-by-item analysis of COVIO scores
| SN | Item | Response option frequencies (%) | Mean (SD) | |||
|---|---|---|---|---|---|---|
| Strongly disagree | Disagree | Agree | Strongly agree | |||
| 1. | There are so many different recommendations about preventing COVID-19, it is hard to know which ones to follow | 56 (9.7) | 216 (37.3) | 212 (36.6) | 95 (16.4) | 2.6 (0.9) |
| 2. | There is not enough time to do all the things recommended to prevent COVID-19 | 72 (12.4) | 274 (47.3) | 188 (32.5) | 45 (7.8) | 2.4 (0.8) |
| 3. | It has gotten to the point where I do not even care to hear new information about COVID-19 | 103 (17.8) | 220 (38.0) | 173 (29.9) | 83 (14.3) | 2.4 (0.9) |
| 4. | No one could do all the COVID-19 recommendations that are given | 81 (14.0) | 256 (44.2) | 189 (32.6) | 53 (9.2) | 2.3 (0.8) |
| 5. | Information about COVID-19 all starts to sound the same after a while | 24 (4.1) | 129 (22.3) | 348 (60.1) | 78 (13.5) | 2.8 (0.7) |
| 6. | I forget most COVID-19 information right after I hear or read it | 126 (21.8) | 349 (60.3) | 88 (15.2) | 16 (2.8) | 2.0 (0.7) |
| 7. | Most things I hear or read about COVID-19 seem unbelievable | 80 (13.8) | 348 (60.1) | 129 (22.3) | 22 (3.8) | 2.2 (0.7) |
| 8. | I feel overloaded by the amount of COVID-19 information I am supposed to know | 36 (6.2) | 208 (35.9) | 233 (40.2) | 102 (17.6) | 2.7 (0.8) |
|
COVID-19 information overload score Mean (SD) = 19.40 (4.12) | ||||||
Factors Associated with COVIO
In the univariable analysis, 10 variables were analyzed (Appendix 3). The variables that had a p < 0.25 and those that are theoretically considered relevant were included in the MLR. The MLR shows that the predictors of COVIO were sources of COVID-19 information through broadcast media (BM) (aOR; 14.599; 95% CI, 1.608–132.559), and frequency of receiving COVID-19 information every minute (aOR 3.892; 95% CI 1.124–13.480). No multicollinearity in the included variables was observed. Interactions between variables were also assessed, and none were identified. The Hosmer-Lemeshow test showed a good fit with level of significance greater than 0.05 (p = 0.834). The classification table shows that the model has a sensitivity, specificity, and an overall accuracy of 65.5%, 55.7%, and 61.3%, respectively (Appendix 4). The final model was presented as aORs with 95% CIs and corresponding p values in Table 4. The details of the initial backward elimination process is also available as Appendix 5.
Discussion
Too much information, especially contradictory information, can have untoward effects on the general public [18, 19]. Reliable and timely information from credible sources is essential to mitigate the negative consequences of misinformation on health, notably the current COVID-19 pandemic. Being a novel ailment, we adopted the available health-information overload assessment tool, CIO [13] to identify factors that are predictors of COVIO. Sources and frequency of COVID-19 information receipt have been found to be significant predictors of COVIO. Participants receiving information through the broadcast media were more likely to have a high COVIO than those receiving information through the social media. We discuss our key findings in detail in the succeeding paragraphs.
It is logical to presume online health information-seeking to be significantly associated with overload. Our analysis, however, showed no significant association between online health information-seeking and COVIO. On the other hand, broadcast media (which is an offline information-seeking medium) was found to be a significant predictor of COVIO. A probable explanation is that, while the offline seeker has little or no control over what is aired at a point in time, an online seeker can fine-tune the search terms to suit the desired search need at any point in time thereby getting a tailored information. Moreso, an online user can easily search other websites for clarification or authentication whenever there is a mistrust of information received from a single online source [20]. One may think that the mistrust should serve as a deterrent to continue a search. However, the optimism of understanding an ambiguity usually serves as a motivator for the online seekers to continue searching even if he feels a little bit anxious or overwhelmed [20]. Thus, this optimism of clarifying an earlier information may prevent the online seeker from being overloaded with the information received.
Contrary to our finding, Kim and co-researchers [21] did not find any statistically significant difference between offline and online health information seekers. Also while Kim et al. [21] hypothesize that overload was more likely related to numbers rather than the type of health information source, we found the type (i.e., BM) to be a significant predictor to COVIO.
Conflicting evidence seems to exist regarding the association between the frequency of receiving information and health information overload. While Kim et al [21] did not find any association between the frequency of seeking cancer information and information overload, the result of this study suggests that messages received per minute are significant predictors of COVIO. Further, Schmitt and colleagues [22] have shown that individuals who received information by push notifications often experience more information overload. Per minute messages share a similar trait to push notifications in terms of frequency. A push notification is an unsolicited message sent to a device relating to one of its applications, even when it is not running [23]. Usually, as much as 16 push notifications can be sent to a smartphone through a single application (app). It is essential, however, to note the distinction that respondents in this study mostly solicit the information obtained, unlike unsolicited push notifications. Despite this difference, it is evident that both push notifications and receiving information every minute are significant predictors of IO.
Soliciting information was not found to be a significant predictor of COVIO. This finding may be due to the self-efficacy of most of the participants. Self-efficacy refers to a person’s confidence for successfully performing a specific task with the belief of achieving positive consequences. Previous research has shown that perceived self-efficacy may influence an individual’s information-seeking behavior [22]. People with a higher perceived self-efficacy seek information more and are less likely to experience overload [22]. In our study, the health background and high level of education attained by most of the respondents may explain their self-efficacy. Similar to what we found, Kim and colleagues [21] also found no link between behavioral aspects of online cancer information-seeking and cancer information overload.
Educational level has shown disproportionate evidence in terms of its relationship with health information overload. We did not find any relationship between educational level and COVIO. The non-significant association in our study may be linked to the fact that most of our respondents have a postgraduate education, which means they are well educated and therefore may not be vulnerable to COVIO. Another reason might be the fact that nearly half of the respondents come from a health background. Several studies identified a negative association between higher education level and information overload [3]. This is not surprising, because improved education results in improved access to knowledge, health information-seeking behavior and, in general, the opportunity to make sense of the information received. Contrary to the findings, however, Ramondt et al. [19] found higher education level to be a significant predictor of diet information overload, and therefore argued that attainment of higher educational level does not automatically translate into the skills needed to manage too much information.
Limitations in the demographics of the sample are acknowledged. The sample comprises a relatively higher number of respondents from Nigeria; therefore, caution should be exercised in generalizing the results. However, the inter-cultural diversity reflected by the three major nationality groups (Nigeria, Malaysia, and USA) with several other nationalities captured in the “others” group would make the results applicable to the general public. Plausible cross-cultural biases between African, western, and eastern cultures are also reduced by such diversity.
Although the study has a diverse multicultural sample, obtaining more data from other countries, especially from the west, would boost the generalizability of the study findings. The social network of the authors may have influenced the number of those with higher academic qualifications responding to the survey. However, recruiting through social media platforms may have led to the sampling of respondents that are representative of the target population that are susceptible to COVIO.
The COVID-19 information is often conflicting, leading to confusion and overload of information in the general population. This can have unfavorable effects on the measures taken to control the transmission and management of the infection. For example, there has been overwhelming and conflicting information as regards the use of face masks to prevent the transmission of COVID-19 [24–26]. This often leads to confusion and mistrust instead of helping the general public [27]. Another example of conflicting information is with regard to social distancing [28, 29]. Social distancing was reported to slow the transmission rate of the virus in some instances [30]. However, information from some studies were stating asymptomatic cases do not transmit the virus while others are stating otherwise [29]. The conflicting information may lead to a nonchalant attitude by the general public about the enforcement of social distancing by some governments [31].
Several recommendations have been proposed previously by some researchers [32] on how to curb COVID-19 information overload. Example of such measures include minimizing exposure to news, verifying the news from reliable sources, avoiding daily updates on infection and death tolls, and visiting only official websites for any COVID-19-related information.
In March 2020, the WHO launched an easily accessible Health Alert system on WhatsApp. The new free-to-use service was developed to respond to public questions about coronavirus and to provide timely, accurate, and official information 24 h a day, globally. The service will also offer the latest numbers and situation updates to government decision-makers. The details on how to use the service are available on the website [33]. An advancement in this service is the IFCN Fact Checking Organizations on WhatsApp. The WHO also recommends the double-checking of evidence for any information received that sounds suspicious or inconsistent through the International Fact-Checking Network (IFCN) allied Fact Checking Organizations on WhatsApp [34].
Conclusion
Our study demonstrated that COVID-19 information overload is common among the public. The source of information and the frequency of receiving COVID-19 information were significantly associated with COVIO. Therefore, there is a need for health institutions and other stakeholders to set up or improve on programs and strategies that will raise awareness and ensure public enlightenment on the best ways to manage COVIO and its health consequences.
Supplementary Information
(DOCX 65 kb)
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mustapha Mohammed, Email: macreener88@gmail.com.
Abubakar Sha’aban, Email: abuushaaban2@gmail.com.
Abubakar Ibrahim Jatau, Email: pharmjt@gmail.com.
Ismaeel Yunusa, Email: ismaeelrx@gmail.com.
Abubakar Musa Isa, Email: abuquatalo05@gmail.com.
Abubakar Sadiq Wada, Email: pharmwada17@gmail.com.
Kehinde Obamiro, Email: kehinde.obamiro@utas.edu.au.
Hadzliana Zainal, Email: hadz@usm.my.
Baharudin Ibrahim, Email: baharudin.ibrahim@usm.my.
References
- 1.Bawden D. Robinson L. Information overload: an overview. Oxford Encyclopedia of Political Decision Making. Oxford University Press; 2020. [Google Scholar]
- 2.Eppler MJ, Mengis J. A framework for information overload research in organizations. Università della Svizzera italiana. 2003.
- 3.Khaleel I, Wimmer BC, Peterson GM, Zaidi STR, Roehrer E, Cummings E, Lee K. Health information overload among health consumers: a scoping review. Patient Educ Couns. 2020;103(1):15–32. doi: 10.1016/j.pec.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNDP. COVID-19 pandemic: Humanity needs leadership and solidarity to defeat the coronavirus. 2020.
- 7.Poonia SK, Rajasekaran K. Information overload: a method to share updates among frontline staff during the COVID-19 pandemic. Otolaryngol Head Neck Surg 2020;0(0):0194599820922988. 10.1177/0194599820922988, 163, 60, 62. [DOI] [PubMed]
- 8.Klepper BOaD. Virus outbreak means (mis)information overload: how to cope. The Seattle Times 2020.
- 9.Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci. 2006;1:9–14. [Google Scholar]
- 10.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. International journal for quality in health care : journal of the International Society for Quality in Health Care. 2003;15(3):261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- 12.Obamiro K, Lee K. Information overload in patients with atrial fibrillation: can the cancer information overload (CIO) scale be used? Patient Educ Couns. 2019;102(3):550–554. doi: 10.1016/j.pec.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Jensen JD, Carcioppolo N, King AJ, Scherr CL, Jones CL, Niederdeppe J. The cancer information overload (CIO) scale: establishing predictive and discriminant validity. Patient Educ Couns. 2014;94(1):90–96. doi: 10.1016/j.pec.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Stoltzfus JC. Logistic regression: a brief primer. Acad Emerg Med. 2011;18(10):1099–1104. doi: 10.1111/j.1553-2712.2011.01185.x. [DOI] [PubMed] [Google Scholar]
- 15.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiegand RE. Performance of using multiple stepwise algorithms for variable selection. Stat Med. 2010;29(15):1647–1659. doi: 10.1002/sim.3943. [DOI] [PubMed] [Google Scholar]
- 17.Jankowska-Polańska B, Uchmanowicz I, Dudek K, Mazur G. Relationship between patients' knowledge and medication adherence among patients with hypertension. Patient preference and adherence. 2016;10:2437–2447. doi: 10.2147/PPA.S117269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagler RH. Adverse outcomes associated with media exposure to contradictory nutrition messages. J Health Commun. 2014;19(1):24–40. doi: 10.1080/10810730.2013.798384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramondt S, Ramírez AS. Assessing the impact of the public nutrition information environment: adapting the cancer information overload scale to measure diet information overload. Patient Educ Couns. 2019;102(1):37–42. doi: 10.1016/j.pec.2018.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swar B, Hameed T, Reychav I. Information overload, psychological ill-being, and behavioral intention to continue online healthcare information search. Comput Hum Behav. 2017;70:416–425. doi: 10.1016/j.chb.2016.12.068. [DOI] [Google Scholar]
- 21.Kim K, Lustria MLA, Burke D, Kwon N. Predictors of cancer information overload: findings from a national survey. Inf Res. 2007;12(4):12–14. [Google Scholar]
- 22.Schmitt JB, Debbelt CA, Schneider FM. Too much information? Predictors of information overload in the context of online news exposure. Inf Commun Soc. 2018;21(8):1151–1167. doi: 10.1080/1369118X.2017.1305427. [DOI] [Google Scholar]
- 23.Cambridge Advanced Learner's Dictionary & Thesaurus: Cambridge University Press; n.d. Push notification.
- 24.Liang M, Gao L, Cheng C, Zhou Q, Uy JP, Heiner K et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;36:101751-. 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed]
- 25.Worby CJ, Chang H-H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nature Communications. 2020;11(1). 10.1038/s41467-020-17922-x. [DOI] [PMC free article] [PubMed]
- 26.Asadi S, Cappa CD, Barreda S, Wexler AS, Bouvier NM, Ristenpart WD. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Scientific Reports. 2020;10(1). 10.1038/s41598-020-72798-7. [DOI] [PMC free article] [PubMed]
- 27.Jaiswal J, Loschiavo C, Perlman DC. Disinformation, misinformation and inequality-driven mistrust in the time of COVID-19: lessons unlearned from AIDS Denialism. AIDS Behav. 2020;24(10):2776–2780. doi: 10.1007/s10461-020-02925-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones NR, Qureshi ZU, Temple RJ, Larwood JPJ, Greenhalgh T, Bourouiba L. Two metres or one: what is the evidence for physical distancing in covid-19? BMJ. 2020:m3223. 10.1136/bmj.m3223. [DOI] [PubMed]
- 29.Tsirtsakis A. Questions raised over WHO’s seemingly conflicting COVID-19 advice. newsGP. 2020 09 Jun 2020.
- 30.Aquino EML, Silveira IH, Pescarini JM, Aquino R, Souza-Filho JAD, Rocha ADS, et al. Medidas de distanciamento social no controle da pandemia de COVID-19: potenciais impactos e desafios no Brasil. Ciência & Saúde Coletiva. 2020;25(suppl 1):2423–2446. doi: 10.1590/1413-81232020256.1.10502020. [DOI] [PubMed] [Google Scholar]
- 31.Pedersen MJ, Favero N. Social distancing during the COVID −19 pandemic: who are the present and future noncompliers? Public Adm Rev. 2020;80(5):805–814. doi: 10.1111/puar.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rathore FA, Farooq F. Information Overload and Infodemic in the COVID-19 Pandemic. J Pak Med Assoc. 2020;70(Suppl 3)(5):S162-S5. 10.5455/jpma.38. [DOI] [PubMed]
- 33.World Health Organisation. World Health Organisation WhatsApp contact. 2020. https://api.whatsapp.com/send/?phone=41798931892&text=hi&app_absent=0. Accessed 24/11/2020 2020.
- 34.International Fact-Checking Network. IFCN Fact Checking Organizations on WhatsApp. WhatsAppp. 2020. https://faq.whatsapp.com/general/ifcn-fact-checking-organizations-on-whatsapp. Accessed 24/11/2020 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 65 kb)