Abstract
Objective
The aim of this study was to determine the effects of age and body mass index (BMI) on the functional outcomes, satisfaction rates, and recovery time after open debridement and reattachment surgery in non-athletic patients with insertional Achilles tendinopathy (IAT).
Methods
In this retrospective study, 33 non-athletic patients (34 ankles) in whom open debridement and reattachment surgery was performed for IAT from 2006 to 2016 were included. Change in pain intensity was assessed using a Visual Analogue Scale (VAS) preoperatively and at the final follow-up. Functional assessment was done by preoperative and postoperative American Orthopaedics Foot and Ankle Score (AOFAS) and final follow-up Victorian Institute of Sport Tendon Study Group-Achilles Tendinopathy score (VISA-A). Patient satisfaction was evaluated by Roles & Maudsley score (RMS). The recovery time was defined as the time interval from the first appearance to postoperative relief of symptoms and recording. In addition, the recurrent Haglund’s deformity was determined by postoperative control radiographs.
Results
The mean age at the time of the operation was 51.19 years. The mean follow-up was 61.75±8.49 months. According to BMI, 5 patients were determined as morbid obese, 19 as obese, 3 as overweight, and 6 as normal. The mean VAS score significantly decreased from 8.5 preoperatively to 1.3 postoperatively (p<0.001). The mean AOFAS score significantly improved from 55.8 preoperatively to 92 postoperatively (p<0.001). Postoperative VISA-A score was 86% (range=32%–100%). According to RMS, 22 patients reported the result as excellent, 8 as good, 2 as fair, and 1 as poor. The mean recovery time was 11.8 (range=2–60) months, but one patient did not reach a symptom free status and thus was not included in the recovery time analysis. Postoperative control radiographs revealed signs of recurrence deformity in four patients. Recovery time showed a negative correlation with the age of the patients (r=−0.65). Postoperative scores and BMI showed no significant correlations with the recovery time on the basis of Spearman’s rho test (p=0.196).
Conclusion
The results of this study have shown that open debridement and reattachment surgery may be an effective surgical method in relieving pain and improving functional status with high satisfaction rate and acceptable recovery time in the management of non-athletic patients with IAT.
Level of Evidence
Level IV, Therapeutic study
Keywords: Reattachment surgery, Insertional achilles tendinopathy, Functional outcome, Midline exposure, Open debridement
Introduction
Insertional Achilles tendinopathy (IAT) is a relatively common disorder characterized by pain and swelling at the posterior heel that results in discomfort and impaired physical performance (1, 2). Pathophysiological studies revealed that the absence of inflammatory cells in IAT specimens and the nature of the disease is interpreted as degenerative origin, hence, the terminology shifted toward tendinopathy rather than tendinitis (3). Alteration in collagen fibers, pathological calcification, cartilage-like changes at the stress shielded side of the tendon, and atrophy owing to decreased tensile loads are among the pathological changes seen in affected tendons (4–6). The calcification is thought to be an adaptation process as Achilles tendon (AT) tries to increase the surface area by calcification to decrease the mechanical loads in a unit area (7).
Several factors are shown to a play role in the development of tendinopathy and can be grouped as intrinsic and extrinsic factors. Structural or anatomical lower extremity conditions are among the intrinsic factors (8). Overuse, poor training methods, advanced age, diabetes, rheumatological disorders, several medications, morbid obesity, and inappropriate footwear are listed as extrinsic factors. Conservative approach is still the mainstay of treatment. Shoe gear modifications, heel lifts, and eccentric exercises have been shown to be beneficial. Steroid injections are mostly debated because of its potential for spontaneous tendon rupture and because this disease’s nature is not inflammatory but degenerative (3, 4).
Failure of at least 6 months of conservative treatment is an indication of surgical intervention. Surgical treatment options for IAT are posterosuperior calcaneus prominence (Haglund) resection (9, 10), Zadek calcaneal osteotomy (11), Gastrocnemius lengthening (12), open debridement and tendon reinsertion (13), and augmentation plasty (14).
In this study, we aimed to evaluate the effect of age and body mass index (BMI) on the functional outcomes, satisfaction rates, and recovery time after open debridement and tendon reconstruction. We hypothesized that patients who are older and have a higher BMI will need a longer period of recovery and have lower functional outcomes towing to the limited healing or increased physical demands related with excess body weight.
Materials and Methods
Study group
After the approval of our study by our institute’s ethical committee (Protocol no: 442683/07.12.2016), we retrospectively reviewed patients with IAT who had undergone open debridement and tendon reinsertion without flexor halluces longus (FHL) transfer. The patients with diabetes, rheumatological diseases, history of local injection, non-insertional AT or AT rupture, and requirement of FHL tendon transfer were excluded. Along with the exclusion criteria, none of our patients were professionally dealing with sports. We identified 34 ankles of 33 patients consisting of 18 female (one bilateral) and 15 male who were suitable to be included in the study group. These patients were operated between the years 2006 and 2016 after a failed conservative treatment of at least 6 months. One patient deceased after the eighth year of operation because of unrelated causes. Patients were invited to outpatient clinic to fill the functional and satisfaction scores and to take control radiographies. In total, 25 patients answered the call, whereas the remaining 8 patients’ functional scores were filled over phone call, but radiographies could not be taken. Mean follow-up was 61.8±8.5 months (range=10–120). Their mean age at the time of operation was 51.19 years (range=38–61). In total, 19 patients were obese, 5 were morbid obese, 3 were overweight, and 6 were normal according to their BMI. No significant comorbidities were present except two patients with hypertension and congestive heart failure.
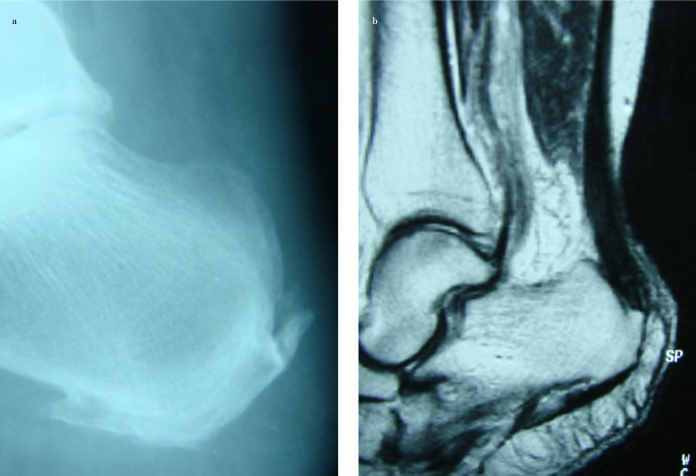
The common complaint of the patients was pain and swelling around the insertion of AT. Radiographs and MRI showed calcifications around the Achilles insertion (Figure 1. a, b)
Figure 1. a, b.
Preoperative plain radiography and MRI of patient with IAT
MRI: magnetic resonance imaging; IAT; insertional Achilles tendinopathy
Surgical technique
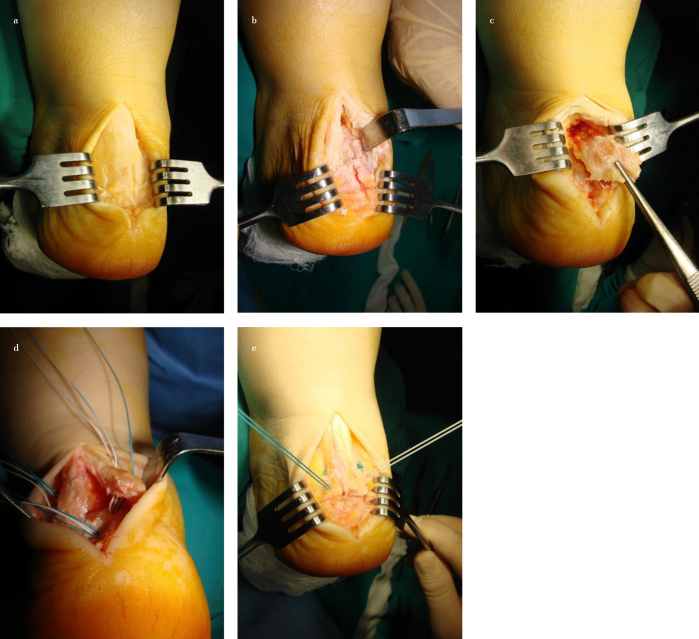
After the administration of anesthesia and prophylactic antibiotics, patient was prepped and draped in the prone position. A thigh tourniquet was inflated, and a central midline incision was used (Figure 2a). After splitting of the AT, tendon was dissected from the spur (Figure 2b). If the tendon looked dark yellow and its texture changed, this part of the tendon was aggressively debrided along with the calcifications within the tendon. Through this incision, retrocalcaneal bursa was also visualised and resected. Next, Haglund deformity was resected with an osteotome, down to the insertion of the AT (Figure 2c). The amount of detachment and debridement was decided intraoperatively by direct visualization (2). When resection was completed, tendon was inspected for stability, and if more than 50% of the tendon was debrided, an augmentation with FHL was performed. Otherwise, tendon was repaired to the insertion site with suture anchors (Figure 2. d, e). Tendon split was repaired with separated non-absorbable, braided suture, and paratenon was repaired with an absorbable 2-0 suture before subcuticular repair and skin closure. All patients were operated by the senior surgeon.
Figure 2. a–e.
(a) Midline exposure to Achilles Tendon. (b) Achilles tendon-splitting. (c) Resection of Haglund deformity. (d, e) Reattachment of Achilles tendon by suture anchors
Postoperative care
Patient’s foot was placed in a postoperative splint and remained non-weight bearing for 2 to 3 weeks with the administration of anti-thrombotic drugs. A postoperative boot was given and progressive weight bearing along with a range of motion exercises were begun. Full weight bearing was allowed at 4 weeks after operation.
Outcome parameters
Patients were evaluated for their pain by Visual Analogue Scale (VAS), for their functional scores by American Orthopaedics Foot and Ankle Score (AOFAS) and Victorian Institute of Sport Tendon Study Group-Achilles Tendinopathy score (VISA-A), and for their satisfaction status by Roles & Maudsley score (RMS). Radiographies were taken for the purpose of evaluating for recurrent Haglund deformity by parallel pitch angle and recalcifications in AT by Fowler-Philip angle.
We also questioned the first time the patients felt better than the preoperative status and noted the interval as recovery time.
Statistical analysis
IBM Statistical Package for Social Sciences Statistics version 22 (IBM SPSS Corp., Armonk, NY, USA) was used for the analysis of the data. Paired t-test was used for the analysis of mean preoperative and postoperative functional score and VAS changes. Spearman’s rho test was used for seeking correlation between non-parametric variables.
Results
Mean recovery time was found as 11.8±3.7 months ranging from 2 to 60 months with one patient who did not reach a symptom free status, hence, she was not included in the elapsed time for recovery analysis. Recovery time showed negative correlation with the age of the patients (r=−0.65).
According to RMS, 22 patients described the result as excellent, 8 as good, 2 as fair, and 1 as poor. Postoperative VISA-A score was 86% (range: 32%–100%). Improvements in VAS and AOFAS scores between preoperative and postoperative status were 8.5 (range=6–10) to 1.3 (range=0–7) and 55.8 (range=33–73) to 92 (range=33–100), respectively. The mean difference in VAS was 7.2±1.7 points (p<0.001). Difference in AOFAS was 36.1±18.4 points (p<0.001) (paired t-test). Postoperative scores and BMI did not show any correlation with the recovery time according to Spearman’s rho test (p=0.196).
Mean Fowler-Philip angles in preoperative and postoperative radiographs were 68.75° and 45.38°, respectively. All patients showed Haglund deformity in their preoperative radiographs, which was evaluated with parallel pitch angles. In addition, four patients showed recalcifications, and the mean difference of AOFAS and VAS did not show significant correlation with Fowler-Phillip angle (p=0.470 and p=0.490, respectively) (paired t-test).
There was no wound breakdown, infection, incisional discomfort, or AT rupture.
Discussion
Pain around posterior heel that limits the physical activities is the major complaint of a patient suffering from IAT. The first line of treatment is conservative, which has good clinical results in most of the patients. Eccentric strengthening of AT proves to be efficient with 82% improvement, but after 6 months of failure, surgery should be decided (1, 5, 15).
The results of this study support the effectiveness of open debridement and reattachment surgery in the operative management of IAT, but in contrast to our hypothesis, recovery time was found to be better in older patients.
Recovery time is a crucial aspect of every surgical treatment. In our study, only one patient could not return to her preoperative activity level, but her VAS and AOFAS improved. Maffuli et al. reported that after 48 months of follow-up, 25% of 21 patients were not able to return to their previous activity level after reinsertion surgery, but they did not specifically explain the release amount of AT and supported that athletes showed better improvement than non-athlete group, but all groups’ functional outcomes improved nonetheless (16). Even though none of our patients were professional athletes, return to work delay was 11.8±3.7 months and can be comparable with the study conducted by Saxena (17), where the delay was 15±6.2 weeks for 13 non-elite runners and with Rousseau’s study (18), where the delay was 9.3±4.1 months for 9 runners who underwent reinsertion surgery.
As Maffuli et al. described in non-athletic patients’ AT repair results, this delay can be explained by considering the fact that the average age of the patients and their BMI were higher than these studies (16). Negative correlation of age and return to activity was also supported by McGarvey et al. (13). On the contrary, Johnson et al. compared the patients who are younger and older than the age of 50 years and found no significant difference (19).
In our study, we excluded patients who required more than 50% of AT release because of the need of FHL tendon augmentation (20). On the contrary, Gillis et al. had shown 90% of AT release and repair with double row suture anchors results and found 100% satisfaction without any tendon rupture (2). Hunt et al. prospectively analyzed 39 patients who underwent 25%–60% debridement with or without FHL augmentation (21). They advocated that with FHL augmentation, plantar flexion strength would be greater, but functional outcomes and satisfaction rates did not show any significance. Although satisfaction rates of these FHL augmented groups were similar to ours, VAS and AOFAS improvements were higher in our study, which supports the idea that FHL augmentation should be performed if the debridement involves more than 50% of total AT (21).
Fowler-Phillip angle’s prognostic and diagnostic value is widely discussed in the literature. Many authors evaluated that parallel pitch and Fowler-Phillip angle was not trustworthy (1, 22). According to our preoperative and postoperative values, only 3 patients’ Fowler-Phillip angle was exceeding 70° but no correlation was found with preoperative VAS and AOFAS scores (p=0.470 and p=0.490, respectively).
McAlister et al. had reported the largest study population in literature about Achilles detachment and reattachment, but their follow-up period was 6.2±5.5 months (23). In their population (n=98), they encountered 4 (4%) cases of failure in tendon-bone interface, 2 (2%) cases of recurrent pain and tendinitis, 7 (7.1%) cases of wound drainage requiring surgery, 2 cases of wound drainage (23). The reported complication rates in literature were between 4.7% and 41% (24). In our study, we did not encounter any complications, but one of our patients (6.25%) was not symptom free in our last examination, that is, her radiographs showed recalcifications but refused to be revised.
Limitations of our study were its retrospective nature and small study group, but to purify our patient population, strict exclusion criteria were formed, thus, small but relatively homogeneous group was achieved. Nonetheless, more concrete arguments may be revealed by the comparative research.
In conclusion, in the light of our patients’ satisfaction level we suggest debridement below the level of 50% and reattachment by suture anchors, which has favorable outcomes. Statistically significant improvement in our patients’ VAS and AOFAS scores may support our suggestion. According to the literature, non-athlete patient groups’ recovery time may be longer than that of the athletes, but in our study, we found that older and non-athletic patients’ recovery time was achieved earlier, which we atoned to lower expectancy of our patients than the athletic patients who desire greater improvements for returning back to sport. Owing to its improved functionality, open debridement and reattachment surgery can be considered for IAT, but younger patients with high expectations should be counseled about the prolonged healing time before surgery.
HIGHLIGHTS
Debridement below the level of 50% and reattachment by suture anchors has favourable outcomes in insertional Achilles tendinopathy.
After a mean follow-up of 61,8 months, 90% of the patients were satisfied with the results.
Recovery time is lower in older patients, which can be atoned to higher expectancy of younger population.
Extended healing period should be counselled especially with young population.
Figure 3.

Postoperative plain radiography
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethical Committee of İstanbul University, Cerrahpaşa School of Medicine (Protocol no: 442683/07.12.2016).
Informed Consent: Informed consent was obtained from the patients contributed in our study.
Author Contributions: Concept - N.S.Y., L.A.; Design - N.S.Y., L.A., A.C.; Supervision - N.S.Y., T.O.; Materials - L.A., A.C.; Data Collection and/or Processing - N.S.Y., A.C.; Analysis and/or Interpretation - N.S.Y., L.A.; Literature Search - L.A.; Writing Manuscript - L.A., N.S.Y.; Critical Review - A.C., T.O.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Miao XD, Jiang H, Wu YP, Tao HM, Yang DS, Hu H. Treatment of calcified insertional Achilles tendinopathy by the posterior midline approach. J Foot Ankle Surg. 2016;55:529–34. doi: 10.1053/j.jfas.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Gillis CT, Lin JS. Use of a central splitting approach and near complete detachment for insertional calcific Achilles tendinopathy repaired with an Achilles bridging suture. J Foot Ankle Surg. 2016;55:235–9. doi: 10.1053/j.jfas.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Li HY, Hua YH. Achilles tendinopathy: Current concepts about the basic science and clinical treatments. Biomed Res Int. 2016;2016 doi: 10.1155/2016/6492597. 6492597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clain MR, Baxter DE. Achilles tendinitis. Foot Ankle. 1992;13:482–7. doi: 10.1177/107110079201300810. [DOI] [PubMed] [Google Scholar]
- 5.Johnson KW, Zalavaras C, Thordarson DB. Surgical management of insertional calcific Achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006;27:245–50. doi: 10.1177/107110070602700404. [DOI] [PubMed] [Google Scholar]
- 6.Maffulli N, Reaper J, Ewen SW, Waterston SW, Barrass V. Chondral metaplasia in calcific insertional tendinopathy of the achilles tendon. Clin J Sport Med. 2006;16:329–34. doi: 10.1097/00042752-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin M, Ruffian A, Ralphs J. The mechanism of formation of bony spurs (enthesophytes) in the achilles tendon. Arthritis Rheum. 2000;43:576–83. doi: 10.1002/1529-0131(200003)43:3<576::AID-ANR14>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 8.Caudell GM. Insertional Achilles tendinopathy. Clin Podiatr Med Surg. 2017;34:195–205. doi: 10.1016/j.cpm.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Sella EJ, Caminear DS, McLarney EA. Haglund’s syndrome. J Foot Ankle Surg. 1998;37:110–4. doi: 10.1016/S1067-2516(98)80089-6. [DOI] [PubMed] [Google Scholar]
- 10.Nesse E, Finsen V. Poor results after resection for Haglund’s heel. Analysis of 35 heels in 23 patients after 3 years. Acta Orthop Scand. 1994;65:107–9. doi: 10.3109/17453679408993732. [DOI] [PubMed] [Google Scholar]
- 11.Zadek I. An operation for the cure of achillobursitis. Am J Surg. 1939;43:542–6. doi: 10.1016/S0002-9610(39)90877-9. [DOI] [Google Scholar]
- 12.Strayer LM. Recession of the gastrocnemius; an operation to relieve spastic contracture of the calf muscles. J Bone Joint Surg Am. 1950;32:671–6. doi: 10.2106/00004623-195032030-00022. [DOI] [PubMed] [Google Scholar]
- 13.McGarvey WC, Palumbo RC, Baxter DE, Leibman BD. Insertional achilles tendinosis: Surgical treatment through a central tendon splitting approach. Foot Ankle Int. 2002;23:19–25. doi: 10.1177/107110070202300104. [DOI] [PubMed] [Google Scholar]
- 14.Saxena A. Surgery for chronic achilles tendon problems. J Foot Ankle Surg. 1995;34:294–300. doi: 10.1016/S1067-2516(09)80063-X. [DOI] [PubMed] [Google Scholar]
- 15.Andres BM, Murrell GAC. Treatment of tendinopathy: What works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008;466:1539–54. doi: 10.1007/s11999-008-0260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maffulli N, Testa V, Capasso G, et al. Surgery for chronic achilles tendinopathy yields worse results in nonathletic patients. Clin J Sport Med. 2006;16:123–8. doi: 10.1097/00042752-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Saxena A. Results of chronic achilles tendinopathy surgery on elite and non-elite track athletes. Foot Ankle Int. 2003;24:712–20. doi: 10.1177/107110070302400911. [DOI] [PubMed] [Google Scholar]
- 18.Rousseau R, Gerometta A, Fogerty S, Rolland E, Catonné Y, Khiami F. Results of surgical treatment of calcaneus insertional tendinopathy in middle- and long-distance runners. Knee Surg Sports Traumatol Arthrosc. 2015;23:2494–501. doi: 10.1007/s00167-014-2986-5. [DOI] [PubMed] [Google Scholar]
- 19.Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific Achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006;27:245–50. doi: 10.1177/107110070602700404. [DOI] [PubMed] [Google Scholar]
- 20.Kolodziej P, Glisson RR, Nunley JA. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund’s deformity: A biomechanical study. Foot Ankle Int. 1999;20:433–7. doi: 10.1177/107110079902000707. [DOI] [PubMed] [Google Scholar]
- 21.Hunt KJ, Cohen BE, Davis WH, Anderson RB, Jones CP. Surgical treatment of insertional achilles tendinopathy with or without flexor hallucis longus tendon transfer: A prospective, randomized study. Foot Ankle Int. 2015;36:998–1005. doi: 10.1177/1071100715586182. [DOI] [PubMed] [Google Scholar]
- 22.Schneider W, Niehus W, Knahr K. Haglund’s syndrome: Disappointing results following surgery-A clinical and radiographic analysis. Foot Ankle Int. 2000;21:26–30. doi: 10.1177/107110070002100105. [DOI] [PubMed] [Google Scholar]
- 23.McAlister JE, Hyer CF. Safety of Achilles detachment and reattachment using a standard midline approach to insertional enthesophytes. J Foot Ankle Surg. 2015;54:214–9. doi: 10.1053/j.jfas.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Irwin TA. Current concepts review: Insertional Achilles tendinopathy. Foot Ankle Int. 2010;31:933–9. doi: 10.3113/FAI.2010.0933. [DOI] [PubMed] [Google Scholar]