Abstract
Objective
The delivery of surgical services has undergone a shift in the past decade with increasing numbers of surgeries being performed in the daycare setting. Implementing a minimally invasive surgical approach with a robot with an enhanced recovery protocol permits robot-assisted laparoscopic surgeries (RALS) to be performed as a day-case (DC) procedure. This study aimed to assess the feasibility and safety of DC surgery according to our experience.
Material and methods
In this prospective observational study, 43 patients underwent DC RALS performed by a single surgeon over 18 months [simple nephrectomy (n=7), radical nephrectomy (n=15), radical nephrectomy with para-aortic lymphadenectomy (n=5), and adrenalectomy (n=5)]. In addition, reconstructive urological procedures that included pyeloplasty (n=9), ureteroureterostomy (n=1), and bladder diverticulectomy with ureteric re-implantation (n=1) were performed as DC surgeries during this study period. RALS was performed in the standard way with an enhanced recovery pathway of care for DC. We collected data regarding the demographic information, medical comorbidities, preoperative outcomes, intraoperative outcomes, complications, length of stay, and readmission rates. The data were analyzed and evaluated.
Results
All the patients (100%) were successfully discharged on the same day with no major complications (Clavien–Dindo grade>I). The readmission rates were 0%.
Conclusion
DC RALS are safe and feasible with an enhanced recovery protocol. With adequate protocols in place, these surgeries might prove to be better than the available minimally invasive techniques and can become the standard of care in the future.
Keywords: Day-case, enhanced recovery, robot-assisted laparoscopic surgery
Introduction
Delivery of surgical services has undergone a shift in the past decade with an increasing number of surgeries being performed in the outpatient setting. Robotic surgery, with its innate advantages, such as three-dimensional (3D) visualization, tremor reduction, finer control, and EndoWrist instruments with 7 degrees of freedom, which makes dissection and suturing much easier, has given an extra advantage to the minimally invasive surgery (MIS) technique.[1]
The advent of MIS has led to a better postoperative recovery in many procedures and faster recovery time and return to functions. This has potentially led to the possibility of day-case (DC) procedures in complex urological surgeries.[2]
DC surgery in the United Kingdom (UK) is defined as a patient being admitted to the hospital for a planned procedure and discharged home on the same calendar day. This typically incorporates a stay of 4–6 hours; however, with more complex surgical procedures, longer stays may be required.[3]
In the United States of America (USA), ambulatory surgery is defined as a procedure where the patient goes home at the end of the working day. There is no overnight stay[4], which in the UK is considered as inpatient surgery. The actual DC surgery procedure should be planned and booked as a DC before the patient’s admission to the hospital. Patients who are planned as inpatients but discharged home on the day of surgery count as inpatients with zero length of stay rather than DC.[3] The US model of DC surgery is slightly different from the UK model where patients stay in the hospital for 23 hrs.
DC surgery is a popular pathway of care, and now, even complex procedures are being considered as DC surgery. It benefits the patients by receiving treatment that is best suited for their needs and allows them to recuperate in their own home, with the additional benefits of decreasing the hospital cost and manpower.[5]
With more acquaintance and approach, MIS across various surgical fields are performed in an ambulatory setting. Laparoscopic gynecologic procedures, such as pelvic adhesiolysis, and surgeries, such as laparoscopic cholecystectomy, inguinal hernioplasty, appendectomy, and Nissen fundoplication, have been performed as DC with satisfactory results.[6]
As experience has increased in MIS, urologists have expanded indications for MIS to larger renal tumors (>7 cm, pT2), level I renal vein tumor thrombus, cytoreductive nephrectomy, pyeloplasty, adrenalectomy, and ureteral reconstruction.[7]
The focus of this prospective study was to report our experience of robot-assisted laparoscopic surgeries (RALS) as DC and to assess its feasibility and safety as we believe that the combined advantages of MIS and an enhanced recovery protocol may permit more RALS in a daycare setting.
Material and methods
After sufficient experience in robotic surgery, the surgical team obtained appropriate approval from the hospital management to start DC procedures. All the data were collected and recorded prospectively.
Ethics committee approval was not obtained as the procedures performed were well established. Other than a shorter plan of discharge, no changes were made in the management. This study was approved by the director of medical services of this institution.
Patients who were deemed fit for DC surgery, well-motivated with minimal comorbidities, with American Society of Anesthesiology grade 1 or 2, and in whom a straightforward surgery was foreseen by the surgeon were included in the study. All patients were prospectively counseled and consented for the same. Upper tract procedures that included nephrectomy, adrenalectomy, pyeloplasty, and ureteral and lower tract reconstruction, such as ureteroureterostomy and bladder diverticulectomy with ureteric re-implantation, were included in our study protocol. Patients who required complex reconstruction, such as partial nephrectomy and cystectomy, were not considered. The surgeries were performed by a single surgical team, including the surgeon and the anesthetist. All the surgeries were performed through the transperitoneal route with a requisite number of ports to execute a complete surgical operation. Only 1 patient was operated through a retroperitoneal approach for a non-functioning kidney.
A standardized anesthetic technique was used. The patient was induced with midazolam, fentanyl, and propofol and maintained with sevoflurane in air with controlled ventilation via a tracheal tube. Intraoperative opioids were avoided, and patients received 1,000 mg of intravenous paracetamol toward the end of the procedure with a single dose of diclofenac suppository. Multimodal antiemesis was provided with ondansetron (4 mg) with dexamethasone (8 mg). All patients received postoperative care with transverse abdominis plane block at the end of the procedure.
After the surgery, all patients were monitored in the postoperative care unit and evaluated by the surgical team and anesthetist with attention to postoperative vital signs (hourly parameters of pulse rate, blood pressure, temperature, consciousness level, and pain scores were recorded) and blood glucose levels before discharge to determine if inpatient admission was warranted. Patients received disease-specific postoperative instructions and all necessary prescriptions before discharge. Their discharge advice included oral antibiotics, analgesics (tablet paracetamol, 1,000 mg, 3 times a day), antacids (tablet pantoprazole. 40 mg, once a day), and a laxative (syrup, lactulose). None of the patients were administered opiate analgesics. All patients were put on the enhanced recovery pathway of care (ERAS) protocol with early ambulation and early feeding 4 to 6 hours post-surgery. All the patients were discharged home with an abdominal drain and a Foley catheter, if needed.
The discharge criteria were:
Pain score of 1 or less on the visual analog scale (VAS)
The patient demonstrates sufficient food intake
The patient performs personal activities (dresses and walks with a steady gait).
The patient feels safe to be discharged.
All patients were given a single phone number for contact in emergency and readmission, if deemed necessary. All patients were followed up with telephonic interviews on the day after the surgery to confirm the absence of complications and regarding general well-being. The patients were evaluated on the 5th postoperative day to discuss the histopathological examination report and later on the 10th day for the removal of skin sutures/clips. Any patient who was admitted within 30 days of the surgery was considered as a readmission.
Patients who have undergone adrenalectomy require consideration of hormonal changes postoperatively to prevent morbidity and mortality. Postoperative complications, such as electrolyte imbalance, hypotension, and adrenal insufficiency, can be avoided with careful preoperative optimization. Few patients may need glucocorticoid replacement postoperatively.[8]
All patients had a standard follow-up protocol, which was relevant to their condition, and were managed accordingly (Figure 1).
Figure 1.
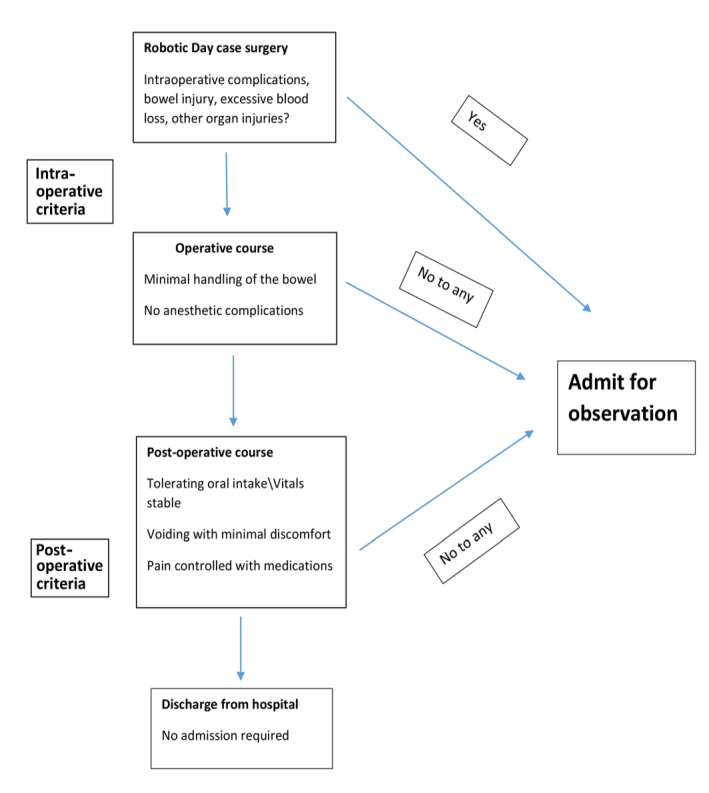
Proposal plan for day case robotic-assisted laparoscopic procedure
Results
RALS was performed in 43 patients over 18 months [simple nephrectomy (n=7), radical nephrectomy (n=15), radical nephrectomy with para-aortic lymphadenectomy (n=5), and adrenalectomy (n=5)]. In addition, reconstructive urological procedures that included pyeloplasty (n=9), ureteroureterostomy (n=1), bladder diverticulectomy with ureteric re-implantation (n=1) were performed as DC surgeries during this study period.
Owing to an insufficient renal remnant, 1 patient underwent conversion to radical nephrectomy after a planned partial nephrectomy because of which the planned inpatient surgery could be converted to DC. All the patients were discharged on the same day with the nil readmission rate. A total of 9 patients experienced severe pain, VAS score of 5 (grade 1 Clavien–Dindo complication) requiring more analgesia. They were contacted via telephone, and none required emergency readmission. They were contacted again after 3 hours of additional analgesia for follow-up for resolution of pain, and all of them showed improvement in pain score to VAS 1 (Tables 1 and 2).
Table 1.
Demographic and preoperative parameters
| No | Median age (years, IQR) | Median BMI (kg/m2IQR) | Side | Sex | Median kidney size (cm, IQR) | Median tumor size (cm, IQR) | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| R | L | M | F | ||||||
| Robotic simple nephrectomy | 7 | 45 (22, 56) | 26.2 (25.2, 27.5) | 5 | 2 | 4 | 3 | 11 (6.9, 15.2) | NA |
|
| |||||||||
| Robotic radical nephrectomy | 15 | 55 (31, 75) | 27.4 (24.3, 29.2) | 4 | 11 | 12 | 3 | 12.5 (7, 18.5) | 6.9 (2.5, 13) |
|
| |||||||||
| Robotic radical nephrectomy with lymphadenectomy | 5 | 58 (50, 64) | 25.3 (24.3, 28.2) | 3 | 2 | 4 | 1 | 12 (7, 18.5) | 8 (7, 11.5) |
|
| |||||||||
| Robotic adrenalectomy | 5 | 32 (27, 52) | 27.8 (25.2, 28.5) | 2 | 3 | 3 | 2 | NA | 9.6 (3.8, 15.5) |
|
| |||||||||
| Robotic pyeloplasty | 9 | 35 (17, 54) | 26.2 (24.7, 27.4) | 3 | 6 | 8 | 1 | NA | NA |
|
| |||||||||
| Robotic ureteroureterostomy | 1 | 35 | 26.2 | 1 | F | NA | NA | ||
|
| |||||||||
| Robotic bladder diverticulectomy with ureteric re-implantation | 1 | 16 | 24.2 | 1 | 1 | NA | NA | ||
BMI: body-mass index; IQR: interquartile range; R: right; L: left; M: male; F: female
Table 2.
Intraoperative and postoperative parameters
| Median total OT (minutes, IQR) | Median console time (minutes, IQR) | Median EBL (mL, IQR) | Median LOS (hours, IQR) | Clavien–Dindo grade | Discharge | Readmission | |
|---|---|---|---|---|---|---|---|
| Robotic simple nephrectomy | 110 (100, 150) | 80 (60, 120) | 40 (20, 100) | 11 (10, 13) | No | 100% | 0 % |
| Robotic radical nephrectomy | 175 (80, 240) | 120 (45, 180) | 100 (40, 200) | 14 (12, 17) | I–4 | 100% | 0% |
| Robotic radical nephrectomy with lymphadenectomy | 180 (120, 240) | 120 (90, 180) | 150 (100, 150) | 16 (13, 17) | I–2 | 100% | 0 % |
| Robotic adrenalectomy | 120 (75, 130) | 80 (40, 90) | 50 (50, 100) | 10 (8, 12) | No | 100% | No |
| Robotic pyeloplasty | 120 (105, 180) | 90 (70, 120) | 50 (30, 70) | 12 (10, 13) | I–3 | 100% | No |
| Robotic ureteroureterostomy | 120 | 90 | 50 | 11 | No | 100% | No |
| Robotic bladder diverticulectomy with ureteric re-implantation | 150 | 120 | 150 | 10 | No | 100% | No |
OT: operative time; IQR: interquartile range; EBL: estimated blood loss; LOS: length of stay
Discussion
MIS has led to a revolution in the management of patients with urologic pathology. The advantages of MIS include a short hospital stay, reduced postoperative pain, early recovery, and improved cosmesis. Laparoscopic surgery, which is the mainstay of MIS, has innate disadvantages, such as a steep learning curve, 2-dimensional vision, and limited directional capacity of the surgical instruments.[9] The torque on the port during laparoscopic surgery is perceived to cause more pain than in robotic surgery. Robotic surgery, with its advantages, such as 3D visualization, tremor reduction, finer control, and EndoWrist instruments with 7 degrees of freedom, which makes dissection and suturing much easier, offsets the disadvantage of laparoscopic surgery.[1] Achieving expertise in complex laparoscopic surgeries is difficult, leading to longer operation times. However, robotic surgery has the benefit of a shorter learning curve than laparoscopic surgery, which has already been analytically proven.[10] It also allows for very minimal pressure at the site of port insertion; therefore, it is perceived that pain in robotic surgery is far lesser than in laparoscopic surgery. Moreover, the precision of suturing in robotic surgery gives little scope for anastomotic leaks during complex reconstructions in the urinary tract.
Nephrectomy, although a major procedure, has now been the standard for all urological surgeons; hence, it is potentially possible to perform nephrectomy in a DC setting. The author’s team has published a short case series on laparoscopic nephrectomy in the past.[11]
The authors perceived that combining MIS robotics with ERAS protocol would enable far more procedures to be performed as DC procedures, which in turn would lead to early discharge, recovery, and early return to work.
All of these benefits raise the possibility of performing RALS in the DC setting. DC surgeries have many advantages over hospitalization, such as decreased risk of nosocomial infections, a familiar setting for recovery, and early patient ambulation, which reduces the complications related to a prolonged stay, such as atelectasis and deep-vein thrombosis. Furthermore, shorter hospital stays reduce the total cost of treatment and make hospital beds available earlier for patients in greater need of specialized medical and nursing care.[12] DC surgery also has the advantage of cost-effectiveness.[13]
DC robotic surgery for upper tract problems has been attempted previously by Moughnyeh et al.[2] In their study, they demonstrated safety and feasibility of DC robotic adrenalectomy in both functional and non-functional adrenal tumors with more than 8-cm masses.
Larger adrenal tumors have been resected using a laparoscopic approach.[14] In this study, even larger adrenal tumors were resected safely with the robotic approach in the DC setting.
The authors believe that with appropriate case selection and presence of ERAS protocol, DC robotic surgery would be feasible. We believe that this has multiple advantages compared with laparoscopic procedures. The important factors that contribute to completing a DC robotic surgery successfully include appropriate planning, communication, a clear understanding of the surgical procedure and the antecedent complications that might arise, careful case selection with an easy procedure in place for readmission and safety, and open communication channels to reach the patient if there are any issues.
Multiple factors play an important role in performing a DC surgery and the safe postoperative course of events. Proper communication and understanding of the procedure, patient, and healthcare personnel are critical. The patients who underwent surgery were given full liberty for readmission, if the need arose. Cooperation among the departments involved in treating the patients was established before the start of the study. In our opinion, these factors contributed to the success of the study. These factors were the difference between a successful outpatient robotic surgery and other surgeries in urology.
DC robotic-assisted laparoscopic procedures are safe and feasible with enhanced recovery protocol. With adequate protocols in place, these surgeries might prove to be better than the available minimally invasive techniques and can become the standard of care in the future.
Main Points.
To our knowledge, this is the first study of day-case robotic surgery involving upper tracts.
Safe and effective.
No complications.
No readmissions.
Acknowledgements
We are bound to acknowledge the support of our patients for allowing us to conduct the study, our physician assistant, Ms. Shiny Robert, for her contribution in statistical analysis, and the healthcare workers who supported in the entire journey.
Footnotes
Ethics Committee Approval: We had taken approval from competent authority in our institution from the director of medical services before starting this study. As the patient care was not changed in daycare surgery hence ethics committee approval not taken.
Informed Consent: Written informed consents were obtained from patients for their anonymous information to be published in this article.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – N.R., S.B., M.T., S.P.; Design – N.R., S.B., M.T., S.P., R.P.; Supervision – N.R., S.B.; Resources – N.R., S.B., M.T., S.P., P.C., S.R.; Materials – S.B.; Data Collection and/or Processing – N.R., S.B., M.T., S.P., R.P.; Analysis and/or Interpretation – N.R., S.B.; Literature Search – S.B.; Writing Manuscript – S.B., N.R.; Critical Review – N.R., S.B., M.T., S.P.; Other – S.B., N.R.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Lin CY, Yang CR, Cheng CL, Ho HC, Chiu KY, Su CK, et al. Application in robotic urologic surgery. J Chin Med Assoc. 2014;77:242–5. doi: 10.1016/j.jcma.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 2.Moughnyeh M, Lindeman B, Porterfield JR, Dream S. Outpatient robot-assisted adrenalectomy: Is it safe? Am J Surg. 2020;220:296–7. doi: 10.1016/j.amjsurg.2020.04.037. [DOI] [PubMed] [Google Scholar]
- 3.Quemby DJ, Stocker ME. Day surgery development and practice: Key factors for a successful pathway. Continuing Education in Anaesthesia, Critical Care and Pain. 2014;14:256–61. doi: 10.1093/bjaceaccp/mkt066. [DOI] [Google Scholar]
- 4.Philip BK. Day care surgery: The United States model of health care. Ambulatory Surgery. 2012;174:81–2. [Google Scholar]
- 5.Cassinotti E, Colombo EM, Di Giuseppe M, Rovera F, Dionigi G, Boni L. Current indications for laparoscopy in day-case surgery. Int J Surg. 2008;6(Suppl 1):S93–6. doi: 10.1016/j.ijsu.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Rubinstein M, Finelli A, Moinzadeh A, Singh D, Ukimura O, Desai MM, et al. Outpatient laparoscopic pyeloplasty. Urology. 2005;66:41–3. doi: 10.1016/j.urology.2005.02.035. [DOI] [PubMed] [Google Scholar]
- 7.Ilie CP, Luscombe CJ, Smith I, Boddy J, Mischianu D, Golash A. Day case laparoscopic nephrectomy. J Endourol. 2011;25:631–4. doi: 10.1089/end.2010.0503. [DOI] [PubMed] [Google Scholar]
- 8.Ortiz DI, Findling JW, Carroll TB, Javorsky BR, Carr AA, Evans DB, et al. Cosyntropin stimulation testing on postoperative day 1 allows for selective glucocorticoid replacement therapy after adrenalectomy for hypercortisolism: Results of a novel, multidisciplinary institutional protocol. Surgery. 2016;159:259–65. doi: 10.1016/j.surg.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Chaussy Y, Becmeur F, Lardy H, Aubert D. Robot-assisted surgery: Current status evaluation in abdominal and urological pediatric surgery. J Laparoendosc Adv Surg Tech A. 2013;23:530–8. doi: 10.1089/lap.2012.0192. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed K, Ibrahim A, Wang TT, Khan N, Challacombe B, Khan MS, et al. Assessing the cost effectiveness of robotics in urological surgery - a systematic review. BJU Int. 2012;110:1544–56. doi: 10.1111/j.1464-410X.2012.11015.x. [DOI] [PubMed] [Google Scholar]
- 11.Ragavan N, Dholakia K, Baskaran J, Ramesh M. Day-case laparoscopic nephrectomy: Feasibility and safety. J Clin Urol. 2019;12:466–9. doi: 10.1177/2051415819852278. [DOI] [Google Scholar]
- 12.Palmer JS. Extravesical ureteral reimplantation: An outpatient procedure. J Urol. 2008;180(Suppl 4):1828–31. doi: 10.1016/j.juro.2008.04.080. [DOI] [PubMed] [Google Scholar]
- 13.Manzia TM, Quaranta C, Filingeri V, Toti L, Anselmo A, Tariciotti L, et al. Feasibility and cost effectiveness of ambulatory laparoscopic cholecystectomy. A retrospective cohort study. Ann Med Surg. 2020;55:56–61. doi: 10.1016/j.amsu.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zografos GN, Farfaras A, Vasiliadis G, Pappa T, Aggeli C, Vasilatou E, et al. Laparoscopic resection of large adrenal tumors. JSLS. 2010;14:364–8. doi: 10.4293/108680810X12924466007160. [DOI] [PMC free article] [PubMed] [Google Scholar]


