Abstract
Salmonella is primarily known to affect the gastrointestinal tract but can rarely cause infections at uncommon sites, such as the urinary tract. It is known that Salmonella can infect the urinary tract directly by blood, fecal contamination of urethra, urolithiasis, or secondary intraluminal ascending infection.
Our patient is a 59-year-old female with a past medical history of nephrolithiasis and multiple urinary tract infections (UTI) who presented with altered mental status and sepsis complicated by Salmonella bacteremia and UTI. Urine and blood cultures revealed Salmonella species > 100,000 colony-forming units per milliliter (CFU/mL) and non-typhoidal Salmonella, respectively. During the course of her hospital admission, the patient was treated with multiple antibiotics.
On further review, it was noted that the patient had presented to the emergency room (ER) about four months earlier with abdominal pain and watery diarrhea with a stool culture being positive for non-typhoidal Salmonella.
Gastroenteritis, sepsis, and enteric fever are normally known with Salmonella enterica serotype Typhi (S. Typhi). Less common extraintestinal diseases like UTI are due to non-typhoidal Salmonella. The most frequent pathogenesis of Salmonella UTI is probably hematogenous. UTI caused by non-typhoidal Salmonella is usually associated with structural abnormalities of the urinary tract. In our case, the patient had non-typhoidal Salmonella gastroenteritis followed by non-typhoidal Salmonella bacteremia and UTI.
Keywords: salmonella infection, gastroenteritis, urinary tract infection, bacteremia, non-typhoidal salmonella (nts)
Introduction
Salmonella is primarily known to affect the gastrointestinal tract but can rarely cause infections at uncommon sites like the urinary tract [1]. Non-typhoidal Salmonella (NTS) urinary tract infections were found to represent only 0.63% of all Salmonella infections in a large retrospective review [2]. It is known that Salmonella can infect the urinary tract directly by blood, fecal contamination of urethra, urolithiasis, or secondary intraluminal ascending infection.
Structural abnormality of the urinary tract, immunodeficiency, and chronic illness are predisposing factors for NTS urinary tract infections [3-4]. We present a case of altered mental status, nephrolithiasis, and sepsis complicated by Salmonella bacteremia and Salmonella urinary tract infection.
Case presentation
A 59-year-old female with a past medical history of fibromyalgia, chronic obstructive pulmonary disease (COPD), allergic rhinitis, nephrolithiasis, and multiple urinary tract infections presented with altered mental status. On examination, she was febrile, tachycardic, and lethargic but arousable. No other significant examination findings, besides left flank pain and suprapubic tenderness, were noted. Her laboratory studies revealed abnormal liver enzymes, elevated creatinine and lactic acid, hypokalemia, high anion gap, and leukocytosis. Urinalysis was significant for infection.
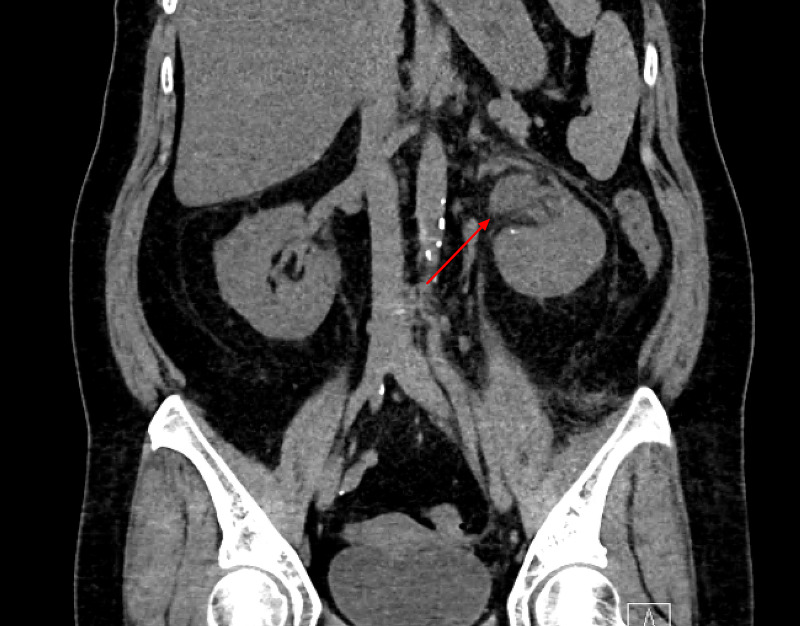
Computed tomography (CT) of the abdomen/pelvis revealed acute obstructing calculi in the distal left ureter, left renal edema, and hydroureteronephrosis (Figures 1-2).
Figure 1. Left renal edema and hydroureteronephrosis.
Figure 2. Acute obstructing calculi in the distal left ureter.
Urology was consulted, and the patient underwent left ureteroscopy with a J-stent placement. Urine and blood cultures revealed Salmonella species > 100,000 colony-forming units per milliliter (CFU/mL) and NTS, respectively. The patient was treated with multiple antibiotics during her hospitalization, initially started on ceftriaxone, 1 g IV daily, transitioned to ampicillin, 2 g IV q four hrs, and then eventually to levofloxacin, 750 mg PO daily, due to persistent fever and leukocytosis. Her symptoms significantly improved on levofloxacin which was also continued on discharge for a further two weeks. On further review, it was known that patient had presented to the emergency room (ER) about four months earlier with abdominal pain and watery diarrhea with a stool culture being positive for NTS. Repeat laboratory studies, urinalysis, and urine culture at the clinic one month after hospital discharge were unremarkable with the patient being completely stable with no new symptoms.
Discussion
Gastroenteritis, sepsis, and enteric fever are normally known with S. Typhi. Less common extraintestinal diseases, such as urinary tract infections, are due to NTS [5]. Predisposing factors for NTS UTI include chronic diseases like diabetes, immune deficiency, or genitourinary tract abnormalities, including nephrolithiasis, chronic pyelonephritis, urethrorectal, or retrovesical fistula. It should not be ignored that NTS UTI can also occur in the healthy immunocompetent population [6].
The most frequent pathogenesis of a Salmonella upper urinary tract infection is probably hematogenous. Salmonella enters the body through ingestion and colonizes the ileum and colon. When Salmonella invades the bloodstream, it can seed distant target organs, such as the kidneys, and cause pyelonephritis. In our case, the patient had NTS gastroenteritis, followed by NTS bacteremia and UTI. Abuhasna et al. reported a similar case in which the patient had NTS UTI and was found to have blood cultures positive for NTS, making hematogenous cause a significant reason for NTS UTI [7]. Salmonella UTI has symptoms similar to other gram-negative UTIs, ranging from asymptomatic bacteriuria to renal abscess [8]. The reported duration of antibiotic therapy in a Salmonella urinary tract infection ranges from two (for mild infections) to over six weeks [9].
Conclusions
NTS infections often present with self-limiting gastroenteritis. Urinary tract infections caused by NTS are usually associated with structural abnormalities of the urinary tract and should prompt the physician to evaluate further. Nephrocalcinosis and nephrolithiasis are the major risk factors.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Extra-intestinal manifestations of salmonella infections. Cohen JI, Bartlett JA, Corey GR. Medicine (Baltimore) 1987;66:349–388. doi: 10.1097/00005792-198709000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Salmonella infections in the U.S.A.; a second series of 2,000 human infections recorded by the N.Y. Salmonella Center. Seligman E, Saphra I, Wassermann M. https://www.jimmunol.org/content/54/1/69.short. J Immunol. 1946;54:69–87. [PubMed] [Google Scholar]
- 3.Clinical spectrum of urinary tract infections due on nontyphoidal Salmonella species. Ramos JM, Aguado JM, García-Corbeira P, Alés JM, Soriano F. Clin Infect Dis. 1996;23:388–390. doi: 10.1093/clinids/23.2.388. [DOI] [PubMed] [Google Scholar]
- 4.Pyonephrosis caused by Salmonella typhi: a case report. Batista da Costa J, Cornu JN, Levgraverend D, et al. Urol Int. 2014;96:241–243. doi: 10.1159/000360741. [DOI] [PubMed] [Google Scholar]
- 5.Urinary tract infections associated with nontyphoidal Salmonella serogroups. Abbott SL, Portoni BA, Janda JM. J Clin Microbiol. 1999;37:4177–4178. doi: 10.1128/jcm.37.12.4177-4178.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Group D salmonella urinary tract infection in an immunocompetent male. Jehangir A, Poudel D, Fareedy SB, Salman A, Qureshi A, Jehangir Q, Alweis R. Case Rep Infect Dis. 2015;2015:608632. doi: 10.1155/2015/608632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Non-typhoidal Salmonella group D bacteremia and urosepsis in a patient diagnosed with HIV infection. Abuhasna S, Al Jundi A, Rahman MU, Said W. J Glob Infect Dis. 2012;4:218–219. doi: 10.4103/0974-777X.103902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clinical spectrum of urinary tract infections due to nontyphoidal Salmonella species. Paterson DL, Harrison MW, Robson JM. Clin Infect Dis. 1997;25:754. doi: 10.1086/513751. [DOI] [PubMed] [Google Scholar]
- 9.Chronic Salmonella bacteriuria with intermittent bacteremia treated with low doses of amoxicillin or ampicillin. Bassily SB, Kilpatrick ME, Farid Z, Mikhail IA, El-Masry NA. Antimicrob Agents Chemother. 1981;20:630–633. doi: 10.1128/aac.20.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]