Abstract
Purpose of Review
Early-onset Alzheimer’s disease (EOAD), defined as Alzheimer’s disease (AD) occurring before age 65, is significantly less well studied than the late-onset form (LOAD) despite EOAD often presenting with a more aggressive disease progression. The aim of this review is to summarize the current understanding of the etiology of EOAD, their translation into clinical practice, and to suggest steps to be taken to move our understanding forward.
Recent Findings
EOAD cases make up 5–10% of AD cases but only 10–15% of these cases show known mutations in the APP, PSEN1, and PSEN2, which are linked to EOAD. New data suggests that these unexplained cases following a non-Mendelian pattern of inheritance is potentially caused by a mix of common and newly discovered rare variants. However, only a fraction of this genetic variation has been identified to date leaving the molecular mechanisms underlying this type of AD and their association with clinical, biomarker, and neuropathological changes unclear.
Summary
While great advancements have been made in characterizing EOAD, much work is needed to disentangle the molecular mechanisms underlying this type of AD and to identify putative targets for more precise disease screening, diagnosis, prevention, and treatment.
Keywords: Early-onset Alzheimer’s disease, Epidemiology, Genetics, Biomarkers, Neuropathology
Introduction
Dementia is a term that is used to describe a category of diseases characterized by a decline in cognitive function that impairs daily function. To date, there are 50 million people that are living with dementia worldwide [1]. Alzheimer’s disease (AD), the most common form of dementia, accounts for 50–75% of dementia cases [2]. Age is considered to be a principal risk factor for AD, and it is used as a categorical marker [3, 4]. The two main disease subcategories include early onset (EOAD) and late onset (LOAD) of AD, based on an arbitrary cut-off set at the age when individuals start to present symptoms, typically 65 years old [3, 4]. However, a cut-off of 60 years is sometimes used reflecting the arbitrary nature underlying this categorization [5]. Among reported AD cases, EOAD accounts for 5–10% [6]. LOAD has a prevalence of ~ 3.9% worldwide and an estimated annual incidence of ~ 7.5 per 1000 individuals above the age of 60 [7]. In comparison, data on prevalence and incidence of EOAD are much more limited. The studies that have assessed EOAD show that the annual prevalence and incidence of people between the age of 45 and 64 are approximately 24.2/100,000 and 6.3/100,000, respectively [8, 9].
Clinical Manifestations of EOAD
In general, the clinical manifestation of AD is characterized by a predominant impairment of anterograde episodic memory. This symptom is typically accompanied by a multitude of cognitive impairments in domains, such as visuospatial, language, and executive function [7]. The combination of the aforementioned characteristics contributes to a global cognitive decline, eventually leading to a total dependent state, and death [10]. Although this typical clinical presentation of memory-predominant phenotypes overlaps between LOAD and EOAD cases, a subset of EOAD cases show an atypical presentation of preserved episodic memory function but focal cortical symptoms relating to language, visuospatial, or executive function [11]. In 25% of EOAD cases, there is a distinct phenotype of non-memory symptoms, in particular apraxia, visual dysfunction, fluent or non-fluent aphasia, executive dysfunction, or dyscalculia, that is seen as the disease progresses [11–13]. In addition, individuals with EOAD often present with a more aggressive disease progression and a shorter relative survival time [12], with the rate of progression driven at least in part by the nature of the underlying causative variant (see below). EOAD cases have a greater pathological burden (neuritic plaques and neurofibrillary tangles) compared to LOAD [14].
There have been no systematic large-scale studies assessing to what extent the different thresholds used affect estimates of prevalence, incidence, or clinical, genetic, and neuropathological variability. There is significant variability in age of onset both within and across families, which is partly explained by known genetic, environmental, or stochastic factors [15]. While some autosomal dominant cases develop first symptoms as early as their late 20s, others develop the disease in their early 60s (prevalence increases with age) [8, 9]. Finally, in a recent study of mutation carriers and non-carrier in the Dominantly Inherited Alzheimer Network (DIAN) cohort, an observational study of families with PSEN1, PSEN2 or APP causal AD mutations, the personality traits of neuroticism, and conscientiousness were correlated with years to symptom onset, markers of tau pathology in the cerebrospinal fluid (CSF), and longitudinal rates of cognitive decline [16]. This suggests that there is clinically significant variability that needs to be thoroughly investigated in order to better characterize the disease.
Neuropathological Changes
The neuropathology of AD brains is characterized by extracellular accumulation of amyloid plaques, consisting of Aβ40 and Aβ42 peptides generated by the cleavage of APP, and intra-neuronal deposition of neurofibrillary tangles (NTF) composed of hyperphosphorylated tau protein (p-tau) [17]. These pathological hallmarks are often complemented by additional morphological changes including synaptic loss [18], neuronal loss [19], microglial activation [20], reactive astrocytes [21], neurovascular dysfunction [22], disruption of the blood brain barrier [23], and brain atrophy [24]. Up to 50% of AD patients exhibit concurrent α-synuclein (αSyn) pathology [25].
Both Aβ and NFT neuropathological changes in both EOAD and LOAD progressively involve brain regions and neuronal cell types following a characteristic pattern [26]. Aβ accumulates initially across neocortical regions, then the limbic system, diencephalon, basal forebrain, and lastly the cerebellum. In contrast, tau involves first the entorhinal cortex and hippocampus, resulting in early-stage neurofibrillary degeneration, synaptic and neuronal loss and regional atrophy, and subsequently (early/mid stage) the locus coeruleus, basal forebrain, and associated regions of the neocortex, followed by the primary sensory cortex.
The extent to which the neuropathology underlying EOAD differs from that of LOAD remains unclear. Some distinctions have been reported. Temporoparietal-precuneus atrophy is seen in both EOAD and LOAD cases, but EOAD cases are seen to have a higher burden of neuritic plaques and NFT in these regions as well as the frontal cortex (albeit to a lesser degree) when compared to LOAD patients [26]. The neocortex, particularly parietal and occipitoparietal regions, seems to experience a similar burden, while the hippocampus is more likely to be spared in EOAD [27, 28]. Finally, individuals who develop AD at a younger age more often than not seem to have “purer” AD pathology with less concomitant neuropathological changes than older AD patients who often show a plethora of pathologies besides inclusions typical for AD (i.e., Lewy bodies, TDP-43, vascular pathology) [29–31]. It is important to recognize that many of the neuropathological studies conducted have accounted for age of onset and/or cognitive function but not duration of disease.
There are current research efforts to synchronize and fill the gap of understanding of the neuropathological overlap between LOAD and autosomal dominant EOAD by implementing a uniform neuropathological assessment protocol [32]. While this effort will be highly valuable, systematic harmonization of brain tissue assessment from non-Mendelian EOAD cases accounting for the majority of EOAD cases [33] in a similar manner is lacking.
Genetics of EOAD
While the late-onset form of AD has a heritability of between 70 and 80% [3, 34], the heritability of EOAD is higher amounting to 92–100% [3]. This correlates with the observation that up to 60% of EOAD subjects have at least one affected first-degree relative [33, 35].
Mendelian EOAD
As described above, families affected by EOAD can either follow a Mendelian (M-EOAD) or non-Mendelian inheritance pattern (NM-EOAD). Mendelian EOAD is caused by variants in APP [36], PSEN1 [37], or PSEN2 [37, 38]. Known to date are close to 330 mutations (duplications and missense) in these three genes accounting for 10–15% (APP), 30–70% (PSEN1), and < 5% (PSEN2) of M-EOAD cases, respectively (https://www.alzforum.org/alzgene). While identification of these genetic variations has largely enhanced our understanding of AD pathogenesis, they only explain 10–15% of familial EOAD cases, leaving the vast proportion of cases unexplained [33, 39].
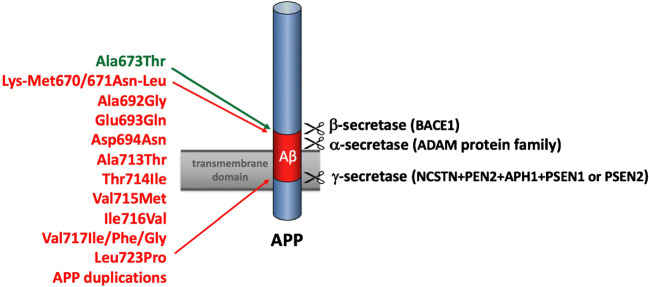
Mutations in all three genes affect the amyloidogenic pathway leading to increased generation and aggregation of Aβ [40, 41]. Aβ peptides result from the cleavage of APP by β- and γ-secretases; PSEN1 and PSEN2 are components of the γ-secretase complex [42]. While most mutations in APP result in increased levels of Aβ aggregation and production [43], a protective APP variant (Icelandic mutation Ala673Thr) decreases Aβ levels by 40% [44] (Fig. 1). Of note, mutations in the same codon (Ala673Val) cause AD when inherited in a recessive fashion [45]. APP carriers tend to have a notable level of amyloid angiopathy in their brain, which can lead to cerebral hemorrhage and stroke (i.e., in carriers of APP duplications) [46, 47].
Fig. 1.
Representative APP mutations causing early-onset Alzheimer’s disease with or without hemorrhage or stroke (in red). All known pathogenic missense substitutions in APP are localized in or around the Aβ-domain encoded by exons 16 and 17. The protective APP variant (Ala673Thr) is indicated in green
Unlike APP mutations that cluster at the Aβ sequence [43], PSEN1 and PSEN2 mutations are found to be widely distributed in these genes (https://www.alzforum.org/alzgene). The majority of them are missense variants and the rest are in-frame deletions/insertions [48–50]. Although PSEN1 and PSEN2 are highly similar in terms of their genomic sequences, structures, and function, PSEN1 mutations appear considerably more pathogenic than PSEN2 [51]. PSEN1-related disease can have an onset as early as the third decade, while symptom onset associated with PSEN2 mutations shows significant variability and can occur beyond age 65 [51]. Notably, the brain expression of PSEN2 is ~ 10-fold lower than that of PSEN1 (https://www.proteinatlas.org/), which could explain more severe disease in PSEN1 carriers.
Non-Mendelian EOAD
Only 10–15% of EOAD cases can be explained by known mutations in PSEN1, PSEN2, and APP [33], and a significant portion of unexplained EOAD cases do not show a Mendelian pattern of inheritance, which inherently means that there are other unidentified genetic variations and mechanisms at play. Nevertheless, large-scale genomic studies conducted to date have mostly ignored this form of EOAD. It is likely a complex genetic disease caused by a mix of both rare and common variants, as suggested by a heritability study that assessed the genetic contribution in NM-EOAD cases from 32 US Alzheimer’s Disease Centers to identify the underlying mode of inheritance [3]. This notion is supported by a recent linkage study among multiplex Caribbean Hispanic families loaded for NM-EOAD [52].
Over the past 10 years, genetic and biological studies identified common and rare genetic variants in the Sortilin-related receptor (SORL1) gene that are linked to both LOAD and EOAD [53–60]. Functional SORL1 is involved in trafficking of APP protein and can decrease levels of Aβ peptides in a multitude of ways, including Aβ peptides being trafficked to a lysosome for degradation, APP being sent to the Golgi apparatus, and the slowing down of the release of APP from the Golgi [61]. SORL1 variants could increase the risk of AD by decreasing the affinity for APP at the cell surface [62], thus modifying the role in which SORL1 plays in intracellular trafficking of APP [59, 63]. Recent meta-analyses and genome-wide association studies observed a ~ 20–90% increase in risk of LOAD [54, 64], and a five-fold increased risk of EOAD associated with rare SORL1 variants [55, 56], which is comparable to the effect size observed in APOE-e4 carriers [55, 56, 65]. A study that used the Exome Aggregation Consortium (ExAC) database (containing genetic variation of 60,706 human samples [66]) classified the pathogenicity of SORL1 variants and found that pathogenic SORL1 variants can increase AD risk by 12-fold as well as cause an earlier age of onset (58.6 ± 5.2 years) for SORL1 carriers [67]. Moreover, it was also found that protein-truncating variants of SORL1 are highly penetrant, which supports earlier findings that the loss of single copy of SORL1 is associated with AD [56]. Supporting the notion that these rare variants might explain part of the missing EOAD heritability, these rare protein-truncating SORL1 variants were observed exclusive in AD cases and absent in the ExAC database [67].
In addition, triggering receptor expressed on myeloid cells 2 (TREM2) has recently been reported to have a significant association with risk of EOAD. Recently, an exome-wide significant association between Arg47His TREM2 variant and EOAD risk was reported by study of the Alzheimer Disease Exome Sequencing-France dataset consisting of 927 LOAD cases, 852 EOAD cases, and 1273 controls [68]. Principal function of TREM2 is an intracellular adaptor for DNAX-activating protein of 12 kDa (DAP12), as well as a modulator of myeloid cell number, proliferation, and survival [68, 69]. Although the data is inconsistent, rare variants of TREM2 have been associated with Aβ deposition, Aβ uptake in microglia [70–72], increased tau in CSF, and the APOE pathway [69, 73]. Together, these data suggest a strong connection to EOAD neuropathology, as well as both amyloid and tau hypotheses of AD [74].
Both genetic and environmental modifiers of AD risk could act through changes at CpG sites, which could affect DNA methylation (DNAm) levels. Similar to genetic mutations, changes in DNAm could lead to increased or decreased gene expression. Notably, CpGs are the most mutable sites in the genome, since methylated-cytosine can spontaneously change to thymine (C > T transition) [66]. Hence, combined genetic and DNAm studies are important for searching of disease modifiers [75].
Intriguingly, DNAm levels at some CpGs are age-related. The joint assessment of selected age-related CpGs is used in 15 reported DNAm clocks [76]. Each DNAm clock could reflect different aspects of biological aging, the pace of which could vary between different people, in contrast to the steady pace of chronological age. It is critical to investigate the expression patterns of genes containing age-related CpGs. Notably, among 1633 genes contributing to different DNAm clocks, 32 genes involved in the amyloid-β pathway, including PSEN1 and BACE1, which encode γ-secretase and β-secretase, respectively [76].
Studies of DNAm clocks are very relevant to age-related disorders, such as AD. A reliable measure of biological age could be a factor in predicting AD onset in pre-symptomatic mutation carriers. The Horvath’s DNAm clock, which assesses ~ 350 CpGs, outperforms other clocks based on its multi-tissue applicability, including blood and brain [77]. DNAm-age acceleration (a discrepancy between DNAm-age and chronological age) was associated with several neurodegenerative disorders [78–81], including AD [82]. Importantly, DNAm-age acceleration was correlated with levels of Aβ-amyloid pathology in AD brains [83]. However, there is only one study of DNAm-age in familial AD. Recently, we investigated a family with identical triplets affected by LOAD in their late 70s, while one of the offspring developed EOAD at age 50. DNAm-age of the triplets was 6–10 years younger than chronological age. In contrast, DNAm-age was 9 years older in the offspring with EOAD, suggesting accelerated aging [84]. However, it is not clear if acceleration of DNAm-age causes aging or reacts to aging, which could be addressed in future longitudinal studies of DNAm clocks.
Biofluid and Brain Imaging Biomarkers of EOAD
To support the clinical diagnosis of EOAD in the clinical setting, identifying biochemical changes in CSF, blood or brain imaging are used as diagnostic tools as they can reflect the pathological changes associated with neurodegenerative diseases [85].
CSF Biomarkers
The most common biomarkers assessed to reflect AD pathology in biofluids are Aβ40, Aβ42, total tau (T-tau), p-tau, and neurofilament light (NFL), an intraneuronal protein and constituent of the axonal cytoskeleton reflecting neuronal degeneration [85]. In CSF, p-tau is measured in order to represent the presence of tau pathology and NFT, whereas T-tau reflects neuronal injury or neurodegeneration [86], although there is evidence that CSF tau might rather represent an increase of neuronal secretion of tau in response to Aβ pathology [87]. The Aβ42 species of Aβ peptides, which is released into CSF [88], is the earliest to accumulate and aggregate into both diffuse and core amyloid plaques [89]. The formation of these hydrophobic plaques consequently lowers Aβ42 that is available to be secreted, causing lower concentration levels of Aβ42 in CSF [85]. Based on the DIAN study, which—as described above—characterizes risk factors, pathophysiology, and biomarker changes across the disease course in carriers of autosomal dominant variants in the APP, PSEN1, or PSEN2 genes, Aβ is the earliest detectable change to be observed in the neurodegenerative cascade 25 years before estimated age of onset [90]. Fibrillar amyloid demonstrated an annual mean percent change of 6.1%, while there was a decreased rate of change of − 8.8% of CSF Aβ42 that slowed near the estimated age of onset [90]. Decline in precuneus metabolism measured by FDG PET took place 17 years before the estimated age of onset, followed by a decline in cognition and accelerated hippocampal atrophy taking place between 2 and 3 years before the estimated age of onset [90]. CSF p-tau is also seen to decline 3 years before the estimated age of onset in these longitudinal analyses, in contrast to previous observations from cross-sectional analyses that found that CSF tau and p-tau levels are significantly higher 14 and 11 years before estimated age of onset, respectively [90]. Various other studies have confirmed that the decrease of CSF Aβ42 and an increase of CSF tau and p-tau are diagnostically significant in AD dementia cases. A meta-analysis completed on 231 studies found a mean fold change of 0.56 (CSF Aβ42), 2.54 (CSF T-tau), and 1.88 (CSF P-tau) in AD patients, respectively, which shows a stronger association of CSF T-tau and CSF P-tau biomarkers to AD than CSF Aβ42 [91]. In contrast to this M-EOAD, there is a significant lack of studies assessing CSF biomarkers in NM-EOAD and potential differing patterns from autosomal dominant EOAD and LOAD. Clarifying longitudinal changes in these biomarkers from early adulthood and across the disease course will be critical to disentangle the molecular distinction of NM-EOAD from M-EOAD and LOAD and improve the use of CSF-based biomarkers for screening and diagnosis in the clinical setting.
Plasma Biomarkers
Although measuring changes in CSF is advantageous because of its contact with the extracellular space of the brain, over the past two decades, significant efforts have been made to develop reliable, sensitive, and specific biomarkers of AD measured from blood as they are less invasive and significantly easier to obtain in both clinical and research settings [85]. While the close contact of CSF with the brain results in relatively high levels of molecules associated with brain disease, much lower amounts exist in the bloodstream. Additionally, plasma Aβ can originate from other organs and tissues as well as be broken down by proteases, metabolized in the liver, or cleared by the kidneys [85, 92], all of which can influence the concentration of Aβ in the bloodstream. However, recent technological advancements in ultrasensitive immunoassays (such as the single-molecule array (Simoa technology) and mass spectrometry to assess plasma levels of molecules are providing promising results of the usefulness of these technologies for diagnosis, prognosis, and monitoring of progression of AD [93, 94].
Recent studies demonstrated that in particular the Aβ42/40 ratio measured by ultrasensitive assays provides a sensitive assessment of amyloid burden that correlates both with the Aβ42/40 ratio in CSF and amyloid PET positivity in both M-EOAD and LOAD [95–98]. In addition, several studies have shown that NFL has diagnostic accuracy for AD similar to that of CSF NFL and increases over time as brain atrophy increases and cognition declines [99, 100]. Studies in individuals with M-EOAD including the DIAN study further indicate that, similar to CSF, plasma NFL is elevated more than a decade prior to symptom onset, suggesting that it can serve as a sensitive diagnostic screening tool to identify individuals at risk [101]. While p-tau181 levels are elevated in AD, show associations with both Aβ and tau PET using agents such as C-PiB (Aβ) and 18F-AV-1451(tau) (previously known as T807) [102–104], suggesting greater specificity for AD pathology than other tau species [105], overall the correlation of tau species measured from blood with CSF tau is relatively weak, potentially limiting the usefulness of currently available tau assays for screening, diagnosis, and monitoring of disease progression.
While it is reasonable to postulate that the abovementioned blood-based biomarker changes might behave similarly in NM-EOAD, there is a lack of studies assessing the prognostic and diagnostic validity of these measures in this type of AD.
Neuroimaging
Neuroimaging techniques done in both clinical and AD research settings include structural magnetic resonance imaging (MRI) and fluorodeoxyglucose (FDG)-positron emission tomography (PET), although the latter is often not covered by insurance and thus not performed. Structural MRIs assess the volumetric atrophy seen in AD, while FDG-PET identifies altered glucose metabolism. Current data on M-EOAD continues to parallel the typical presentation of glucose hypometabolism, amyloid deposition, and atrophy that is also seen across many cortical regions (thalamus, putamen, pallidum, hippocampus, caudate, amygdala, and accumbens) in LOAD cases [106]. However, besides the fact that in M-EOAD these changes are seen earlier, they are often more widespread affecting additional areas including the putamen and thalamus [107], and there is often substantial hypometabolism seen first in posterior cingulate/precuneus and lateral parietal regions before it extends to include the frontal and temporal cortices [106]. Data from the DIAN study suggests that carriers of causal mutations exhibit cortical glucose hypometabolism and cortical thinning in the medial and lateral parietal lobes 5–10 years before the estimated age of onset, which suggests that FDG-PET and MRI changes are contemporaneous [106]. Subcortical regions seem to show a differing pattern. While all subcortical gray matter regions exhibited elevated PiB uptake, only the hippocampus showed reduced glucose metabolism [106].
Imaging AD pathology also includes the use of amyloid imaging tracers such as Pittsburgh Compound-B (PiB), as well as three amyloid radiotracers Amyvid™ (florbetapir F18), Neuraceq™ (florbetaben F18) and Vizamyl™ (flutemetamol F18) and one tau ligand (Tauvid™; 18F-flortaucipir) that are now approved by the Food and Drug Administration (FDA) [108].
In line with the morphological and metabolic changes that are seen before the estimated age of onset, elevated PiB levels are observed in almost every cortical region in an evenly dispersed manner almost 15 years before estimated age of onset [106]. However, the pallidum and caudate are exceptions because there is an observed increase of PiB levels but no evidence of metabolic or volumetric changes, which demonstrates that not all regions follow typical biomarker ordering [106]. In company with the elevated levels of PiB, tau-PET imaging demonstrates an increased level of tau tracer binding in the neocortex, and when compared to sporadic LOAD the levels of both agents are higher in M-EOAD [109]. Correlations between the specific component of tauopathy and the observed increase in tau-PET signaling are still unclear.
In line with M-EOAD, NM-EOAD sporadic cases with no family history of AD when compared to LOAD also present with more atrophy [110], robust neocortical glucose hypometabolism [111], and increased tau-PET signaling [112, 113]. Although imaging studies are limited, these findings match the neurodegeneration and tauopathy that are seen in brain autopsies and show a more aggressive disease progression at younger age of onset. These observations are also reflected in analyses of the Alzheimer’s Disease Neuroimaging Initiative (ADNI) dataset (unrelated > 65-year-old subjects) showing more severe changes and disease progression MRI and biofluid-based biomarkers in persons with younger compared to older onset [114].
Conclusion
While there have been important advances in AD research in the past decades in understanding the mechanisms underlying EOAD, a significant part of its etiology remains unclear, hampering more accurate diagnosis and more effective treatment in the clinical setting. While routine screening using whole-exome sequencing is now feasible in the clinical setting, its interpretation (and associated genetic counseling) is largely limited to known mutations in APP, PSEN1, PSEN2, GRN, and MPT, which only account for a small subset of EOAD cases before age 65. Clarifying the genetic, molecular, and clinical distinction of unexplained non-Mendelian EOAD from M-EOAD and LOAD, its pattern of cognitive decline, biomarker, and neuropathological changes over the disease course and the genetic and molecular underpinnings of its observed clinical variability will be critical to improve both diagnostic screening as well as developing more effective preventive and therapeutic targets. To do this, cohorts of NM-EOAD cases with sufficient sample size, deep phenotypic characterization, longitudinal follow-up, comprehensive AD biomarker assessment, and an array of integrative data (i.e., genomic, epigenetic, proteomic, transcriptomic and metabolic data) are needed. Ideally, these datasets would comprise both family-based and case-control cohorts of various ancestral backgrounds to disentangle genetic variation specific to ethnic group, familial aggregation, or sporadic occurrence. Next-generation sequencing data coupled with other multi-omics approaches and extensive bioinformatics in such datasets would further allow to identify allelic effectors of identified loci, molecular underpinnings of disease etiology, progression and variation in age at onset, and the delineation between clinical endophenotypes. Identification of molecular disease signatures and pattern(s) of altered protein expression would allow to discriminate early disease stages, improve disease screening and diagnostics, identify subjects at risk for disease or more severe progression, and facilitate the identification of “druggable” molecular targets and successful repositioning of drugs for clinical application. Application of standardized assessment and analysis protocols comparable to those of the ongoing major studies on M-EOAD and LOAD will be critical to allow for valid comparison of data with these forms of AD.
As described above, the ADNI/DIAN Neuropathology Core has implemented a uniform assessment protocol to evaluate the neuropathological overlap between M-EOAD and LOAD. Similar collections of NM-EOAD brain tissue with standardized neuropathological assessment are needed to comprehensively delineate neuropathological overlap of both these forms with sporadic and familial NM-EOAD. Given that the NM-EOAD is likely heterogeneous, genetic analyses should test a variety of inheritance patters including recessive and polygenic effects.
Finally, there is a critical need for more studies to authenticate the use of ultrasensitive blood-based biomarkers as a screening, diagnostic, and monitoring tool in EOAD subtypes. Current data show that in particular the Aβ42/40 ratio and NFL measured from blood using new technologies show a high degree of specificity and sensitivity to detect AD in individual years before onset of symptoms and correlate with CSF and imaging changes over the disease course. Validation of course and pattern of blood-based biomarkers in EOAD subtypes, ideally informed by genetic background, would be highly valuable for both clinical and research settings.
In-depth characterization of the clinical, genetic, and neuropathological distinction of unexplained EOAD from M-EOAD and LOAD is critical to fully understand the etiology of AD, characterize determinants and modulators of risk and age at onset, refine prevalence and incidence, and develop more effective targets for screening, prevention, and treatment.
Code Availability
N/A.
Funding
This work was in part supported by the National Institutes of Health (NIH) grants RF1AG054080 (CR, GB, ER, TA), R01AG064614 (CR, GB), U01AG052410 (CR), P50AG008702 (CR), U01AG052410 (GB), and RF1AG054074 (GB). Dr. Rogaeva was further supported by the Canadian Consortium on Neurodegeneration in Aging.
Data Availability
N/A.
Compliance with Ethical Standards
Conflict of Interest
Temitope Ayodele, Ekaterina Rogaeva, Jiji T. Kurup, Gary Beecham, and Christiane Reitz declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Dementia
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.World Health Organization 2019 10 facts on dementia 2019 [.
- 2.Alzheimer’s Association 2019 Alzheimer’s disease facts and figures. Alzheimers Dement. 2019;15(3):321–387. [Google Scholar]
- 3.Wingo TS, Lah JJ, Levey AI, Cutler DJ. Autosomal recessive causes likely in early-onset Alzheimer disease. Arch Neurol. 2012;69(1):59–64. doi: 10.1001/archneurol.2011.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barber IS, Braae A, Clement N, Patel T, Guetta-Baranes T, Brookes K, et al. Mutation analysis of sporadic early-onset Alzheimer’s disease using the NeuroX array. Neurobiol Aging. 2017;49(215):e1–e8. doi: 10.1016/j.neurobiolaging.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szigeti K, Doody RS. Should EOAD patients be included in clinical trials? Alzheimers Res Ther. 2011;3(1):4. doi: 10.1186/alzrt63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alzheimer's A. Early-onset dementia: a national challenge, a future crisis. Washington, DC: Alzheimer's Association; 2006. [Google Scholar]
- 7.Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer disease. Nat Rev Neurol. 2011;7(3):137–152. doi: 10.1038/nrneurol.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lambert MA, Bickel H, Prince M, Fratiglioni L, Von Strauss E, Frydecka D, et al. Estimating the burden of early onset dementia; systematic review of disease prevalence. Eur J Neurol. 2014;21(4):563–569. doi: 10.1111/ene.12325. [DOI] [PubMed] [Google Scholar]
- 9.Renvoize E, Hanson M, Dale M. Prevalence and causes of young onset dementia in an English health district. Int J Geriatr Psychiatry. 2011;26(1):106–107. doi: 10.1002/gps.2456. [DOI] [PubMed] [Google Scholar]
- 10.Lane CA, Hardy J, Schott JM. Alzheimer’s disease. Eur J Neurol. 2018;25(1):59–70. doi: 10.1111/ene.13439. [DOI] [PubMed] [Google Scholar]
- 11.van der Flier WM, Pijnenburg YA, Fox NC, Scheltens P. Early-onset versus late-onset Alzheimer’s disease: the case of the missing APOE ɛ4 allele. Lancet Neurol. 2011;10(3):280–288. doi: 10.1016/S1474-4422(10)70306-9. [DOI] [PubMed] [Google Scholar]
- 12.Bateman RJ, Aisen PS, De Strooper B, Fox NC, Lemere CA, Ringman JM, et al. Autosomal-dominant Alzheimer’s disease: a review and proposal for the prevention of Alzheimer’s disease. Alzheimers Res Ther. 2011;3(1):1. doi: 10.1186/alzrt59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryan NS, Rossor MN. Correlating familial Alzheimer’s disease gene mutations with clinical phenotype. Biomark Med. 2010;4(1):99–112. doi: 10.2217/bmm.09.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marshall GA, Fairbanks LA, Tekin S, Vinters HV, Cummings JL. Early-onset Alzheimer’s disease is associated with greater pathologic burden. J Geriatr Psychiatry Neurol. 2007;20(1):29–33. doi: 10.1177/0891988706297086. [DOI] [PubMed] [Google Scholar]
- 15.Ryman DC, Acosta-Baena N, Aisen PS, Bird T, Danek A, Fox NC, Goate A, Frommelt P, Ghetti B, Langbaum JBS, Lopera F, Martins R, Masters CL, Mayeux RP, McDade E, Moreno S, Reiman EM, Ringman JM, Salloway S, Schofield PR, Sperling R, Tariot PN, Xiong C, Morris JC, Bateman RJ, And the Dominantly Inherited Alzheimer Network Symptom onset in autosomal dominant Alzheimer disease: a systematic review and meta-analysis. Neurology. 2014;83(3):253–260. doi: 10.1212/WNL.0000000000000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aschenbrenner AJ, Petros J, McDade E, Wang G, Balota DA, Benzinger TL, Cruchaga C, Goate A, Xiong C, Perrin R, Fagan AM, Graff-Radford N, Ghetti B, Levin J, Weidinger E, Schofield P, Gräber S, Lee JH, Chhatwal JP, Morris JC, Bateman R, Hassenstab J, Dominantly Inherited Alzheimer Network Relationships between big-five personality factors and Alzheimer's disease pathology in autosomal dominant Alzheimer's disease. Alzheimers Dement (Amst) 2020;12(1):e12038. doi: 10.1002/dad2.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med. 2011;1(1):a006189. doi: 10.1101/cshperspect.a006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen MK, Mecca AP, Naganawa M, Finnema SJ, Toyonaga T, Lin SF, Najafzadeh S, Ropchan J, Lu Y, McDonald JW, Michalak HR, Nabulsi NB, Arnsten AFT, Huang Y, Carson RE, van Dyck CH. Assessing synaptic density in Alzheimer disease with synaptic vesicle glycoprotein 2A positron emission tomographic imaging. JAMA Neurol. 2018;75(10):1215–1224. doi: 10.1001/jamaneurol.2018.1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.West MJ, Coleman PD, Flood DG, Troncoso JC. Differences in the pattern of hippocampal neuronal loss in normal ageing and Alzheimer’s disease. Lancet. 1994;344(8925):769–772. doi: 10.1016/s0140-6736(94)92338-8. [DOI] [PubMed] [Google Scholar]
- 20.Keren-Shaul H, Spinrad A, Weiner A, Matcovitch-Natan O, Dvir-Szternfeld R, Ulland TK, et al. A unique microglia type associated with restricting development of Alzheimer’s disease. Cell. 2017;169(7):1276–90e17. doi: 10.1016/j.cell.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 21.Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Münch AE, Chung WS, Peterson TC, Wilton DK, Frouin A, Napier BA, Panicker N, Kumar M, Buckwalter MS, Rowitch DH, Dawson VL, Dawson TM, Stevens B, Barres BA. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481–487. doi: 10.1038/nature21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kisler K, Nelson AR, Montagne A, Zlokovic BV. Cerebral blood flow regulation and neurovascular dysfunction in Alzheimer disease. Nat Rev Neurosci. 2017;18(7):419–434. doi: 10.1038/nrn.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nation DA, Sweeney MD, Montagne A, Sagare AP, D'Orazio LM, Pachicano M, et al. Blood-brain barrier breakdown is an early biomarker of human cognitive dysfunction. Nat Med. 2019;25(2):270–276. doi: 10.1038/s41591-018-0297-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pini L, Pievani M, Bocchetta M, Altomare D, Bosco P, Cavedo E, Galluzzi S, Marizzoni M, Frisoni GB. Brain atrophy in Alzheimer’s disease and aging. Ageing Res Rev. 2016;30:25–48. doi: 10.1016/j.arr.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Arai Y, Yamazaki M, Mori O, Muramatsu H, Asano G, Katayama Y. Alpha-synuclein-positive structures in cases with sporadic Alzheimer’s disease: morphology and its relationship to tau aggregation. Brain Res. 2001;888(2):287–296. doi: 10.1016/s0006-8993(00)03082-1. [DOI] [PubMed] [Google Scholar]
- 26.Palasí A, Gutiérrez-Iglesias B, Alegret M, Pujadas F, Olabarrieta M, Liébana D, Quintana M, Álvarez-Sabín J, Boada M. Differentiated clinical presentation of early and late-onset Alzheimer’s disease: is 65 years of age providing a reliable threshold? J Neurol. 2015;262(5):1238–1246. doi: 10.1007/s00415-015-7698-3. [DOI] [PubMed] [Google Scholar]
- 27.Squire LR, Genzel L, Wixted JT, Morris RG. Memory consolidation. Cold Spring Harb Perspect Biol. 2015;7(8):a021766. doi: 10.1101/cshperspect.a021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray ME, Graff-Radford NR, Ross OA, Petersen RC, Duara R, Dickson DW. Neuropathologically defined subtypes of Alzheimer's disease with distinct clinical characteristics: a retrospective study. Lancet Neurol. 2011;10(9):785–796. doi: 10.1016/S1474-4422(11)70156-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Savva GM, Wharton SB, Ince PG, Forster G, Matthews FE, Brayne C. Age, neuropathology, and dementia. N Engl J Med. 2009;360(22):2302–2309. doi: 10.1056/NEJMoa0806142. [DOI] [PubMed] [Google Scholar]
- 30.Middleton LE, Grinberg LT, Miller B, Kawas C, Yaffe K. Neuropathologic features associated with Alzheimer disease diagnosis: age matters. Neurology. 2011;77(19):1737–1744. doi: 10.1212/WNL.0b013e318236f0cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haroutunian V, Schnaider-Beeri M, Schmeidler J, Wysocki M, Purohit DP, Perl DP, et al. Role of the neuropathology of Alzheimer disease in dementia in the oldest-old. Arch Neurol. 2008;65(9):1211–1217. doi: 10.1001/archneur.65.9.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cairns NJ, Perrin RJ, Franklin EE, Carter D, Vincent B, Xie M, Bateman RJ, Benzinger T, Friedrichsen K, Brooks WS, Halliday GM, McLean C, Ghetti B, Morris JC, the Alzheimer Disease Neuroimaging Initiative. the Dominantly Inherited Alzheimer Network Neuropathologic assessment of participants in two multi-center longitudinal observational studies: the Alzheimer Disease Neuroimaging Initiative (ADNI) and the Dominantly Inherited Alzheimer Network (DIAN) Neuropathology. 2015;35(4):390–400. doi: 10.1111/neup.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campion D, Dumanchin C, Hannequin D, Dubois B, Belliard S, Puel M, Thomas-Anterion C, Michon A, Martin C, Charbonnier F, Raux G, Camuzat A, Penet C, Mesnage V, Martinez M, Clerget-Darpoux F, Brice A, Frebourg T. Early-onset autosomal dominant Alzheimer disease: prevalence, genetic heterogeneity, and mutation spectrum. Am J Hum Genet. 1999;65(3):664–670. doi: 10.1086/302553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gatz M, Reynolds CA, Fratiglioni L, Johansson B, Mortimer JA, Berg S, Fiske A, Pedersen NL. Role of genes and environments for explaining Alzheimer disease. Arch Gen Psychiatry. 2006;63(2):168–174. doi: 10.1001/archpsyc.63.2.168. [DOI] [PubMed] [Google Scholar]
- 35.Jarmolowicz AI, Chen HY, Panegyres PK. The patterns of inheritance in early-onset dementia: Alzheimer’s disease and frontotemporal dementia. Am J Alzheimers Dis Other Dement. 2015;30(3):299–306. doi: 10.1177/1533317514545825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goate A, Chartier-Harlin MC, Mullan M, Brown J, Crawford F, Fidani L, Giuffra L, Haynes A, Irving N, James L, Mant R, Newton P, Rooke K, Roques P, Talbot C, Pericak-Vance M, Roses A, Williamson R, Rossor M, Owen M, Hardy J. Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature. 1991;349(6311):704–706. doi: 10.1038/349704a0. [DOI] [PubMed] [Google Scholar]
- 37.Sherrington R, Rogaev EI, Liang Y, Rogaeva EA, Levesque G, Ikeda M, Chi H, Lin C, Li G, Holman K, Tsuda T, Mar L, Foncin JF, Bruni AC, Montesi MP, Sorbi S, Rainero I, Pinessi L, Nee L, Chumakov I, Pollen D, Brookes A, Sanseau P, Polinsky RJ, Wasco W, da Silva HAR, Haines JL, Pericak-Vance MA, Tanzi RE, Roses AD, Fraser PE, Rommens JM, St George-Hyslop PH. Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature. 1995;375(6534):754–760. doi: 10.1038/375754a0. [DOI] [PubMed] [Google Scholar]
- 38.Levy-Lahad E, Wasco W, Poorkaj P, Romano DM, Oshima J, Pettingell WH, et al. Candidate gene for the chromosome 1 familial Alzheimer’s disease locus. Science. 1995;269(5226):973–7. [DOI] [PubMed]
- 39.Bates KA, Verdile G, Li QX, Ames D, Hudson P, Masters CL, Martins RN. Clearance mechanisms of Alzheimer’s amyloid-beta peptide: implications for therapeutic design and diagnostic tests. Mol Psychiatry. 2009;14(5):469–486. doi: 10.1038/mp.2008.96. [DOI] [PubMed] [Google Scholar]
- 40.Wolfe MS. The gamma-secretase complex: membrane-embedded proteolytic ensemble. Biochemistry. 2006;45(26):7931–7939. doi: 10.1021/bi060799c. [DOI] [PubMed] [Google Scholar]
- 41.Selkoe DJ, Wolfe MS. Presenilin: running with scissors in the membrane. Cell. 2007;131(2):215–221. doi: 10.1016/j.cell.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 42.Haass C, De Strooper B. The presenilins in Alzheimer's disease--proteolysis holds the key. Science. 1999;286(5441):916–919. doi: 10.1126/science.286.5441.916. [DOI] [PubMed] [Google Scholar]
- 43.Sisodia SS, St George-Hyslop PH. Gamma-Secretase, Notch, Abeta and Alzheimer’s disease: where do the presenilins fit in? Nat Rev Neurosci. 2002;3(4):281–290. doi: 10.1038/nrn785. [DOI] [PubMed] [Google Scholar]
- 44.Jonsson T, Atwal JK, Steinberg S, Snaedal J, Jonsson PV, Bjornsson S, Stefansson H, Sulem P, Gudbjartsson D, Maloney J, Hoyte K, Gustafson A, Liu Y, Lu Y, Bhangale T, Graham RR, Huttenlocher J, Bjornsdottir G, Andreassen OA, Jönsson EG, Palotie A, Behrens TW, Magnusson OT, Kong A, Thorsteinsdottir U, Watts RJ, Stefansson K. A mutation in APP protects against Alzheimer’s disease and age-related cognitive decline. Nature. 2012;488(7409):96–99. doi: 10.1038/nature11283. [DOI] [PubMed] [Google Scholar]
- 45.Di Fede G, Catania M, Morbin M, Rossi G, Suardi S, Mazzoleni G, et al. A recessive mutation in the APP gene with dominant-negative effect on amyloidogenesis. Science. 2009;323(5920):1473–1477. doi: 10.1126/science.1168979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rovelet-Lecrux A, Hannequin D, Raux G, Le Meur N, Laquerrière A, Vital A, et al. APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet. 2006;38(1):24–26. doi: 10.1038/ng1718. [DOI] [PubMed] [Google Scholar]
- 47.Guyant-Marechal I, Berger E, Laquerrière A, Rovelet-Lecrux A, Viennet G, Frebourg T, et al. Intrafamilial diversity of phenotype associated with app duplication. Neurology. 2008;71(23):1925–1926. doi: 10.1212/01.wnl.0000339400.64213.56. [DOI] [PubMed] [Google Scholar]
- 48.Crook R, Verkkoniemi A, Perez-Tur J, Mehta N, Baker M, Houlden H, Farrer M, Hutton M, Lincoln S, Hardy J, Gwinn K, Somer M, Paetau A, Kalimo H, Ylikoski R, Pöyhönen M, Kucera S, Haltia M. A variant of Alzheimer’s disease with spastic paraparesis and unusual plaques due to deletion of exon 9 of presenilin 1. Nat Med. 1998;4(4):452–455. doi: 10.1038/nm0498-452. [DOI] [PubMed] [Google Scholar]
- 49.Rogaeva EA, Fafel KC, Song YQ, Medeiros H, Sato C, Liang Y, Richard E, Rogaev EI, Frommelt P, Sadovnick AD, Meschino W, Rockwood K, Boss MA, Mayeux R, St. George-Hyslop P. Screening for PS1 mutations in a referral-based series of AD cases: 21 novel mutations. Neurology. 2001;57(4):621–625. doi: 10.1212/wnl.57.4.621. [DOI] [PubMed] [Google Scholar]
- 50.De Jonghe C, Cruts M, Rogaeva EA, Tysoe C, Singleton A, Vanderstichele H, et al. Aberrant splicing in the presenilin-1 intron 4 mutation causes presenile Alzheimer’s disease by increased Abeta42 secretion. Hum Mol Genet. 1999;8(8):1529–1540. doi: 10.1093/hmg/8.8.1529. [DOI] [PubMed] [Google Scholar]
- 51.Snider BJ, Norton J, Coats MA, Chakraverty S, Hou CE, Jervis R, Lendon CL, Goate AM, McKeel DW, Morris JC. Novel presenilin 1 mutation (S170F) causing Alzheimer disease with Lewy bodies in the third decade of life. Arch Neurol. 2005;62(12):1821–1830. doi: 10.1001/archneur.62.12.1821. [DOI] [PubMed] [Google Scholar]
- 52.Cheng R, Tang M, Martinez I, Ayodele T, Baez P, Reyes-Dumeyer D, et al. Linkage analysis of multiplex Caribbean Hispanic families loaded for unexplained early-onset cases identifies novel Alzheimer’s disease loci. Alzheimers Dement (Amst) 2018;10:554–562. doi: 10.1016/j.dadm.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pottier C, Hannequin D, Coutant S, Rovelet-Lecrux A, Wallon D, Rousseau S, et al. High frequency of potentially pathogenic SORL1 mutations in autosomal dominant early-onset Alzheimer disease. Mol Psychiatry. 2012;17(9):875–879. doi: 10.1038/mp.2012.15. [DOI] [PubMed] [Google Scholar]
- 54.Vardarajan BN, Zhang Y, Lee JH, Cheng R, Bohm C, Ghani M, Reitz C, Reyes-Dumeyer D, Shen Y, Rogaeva E, St George-Hyslop P, Mayeux R. Coding mutations in SORL1 and Alzheimer disease. Ann Neurol. 2015;77(2):215–227. doi: 10.1002/ana.24305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nicolas G, Charbonnier C, Wallon D, Quenez O, Bellenguez C, Grenier-Boley B, et al. SORL1 rare variants: a major risk factor for familial early-onset Alzheimer's disease. Mol Psychiatry. 2016;21(6):831–836. doi: 10.1038/mp.2015.121. [DOI] [PubMed] [Google Scholar]
- 56.Verheijen J, Van den Bossche T, van der Zee J, Engelborghs S, Sanchez-Valle R, Lladó A, et al. A comprehensive study of the genetic impact of rare variants in SORL1 in European early-onset Alzheimer’s disease. Acta Neuropathol. 2016;132(2):213–224. doi: 10.1007/s00401-016-1566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Andersen OM, Rudolph IM, Willnow TE. Risk factor SORL1: from genetic association to functional validation in Alzheimer's disease. Acta Neuropathol. 2016;132(5):653–665. doi: 10.1007/s00401-016-1615-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet. 2013;45(12):1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rogaeva E, Meng Y, Lee JH, Gu Y, Kawarai T, Zou F, Katayama T, Baldwin CT, Cheng R, Hasegawa H, Chen F, Shibata N, Lunetta KL, Pardossi-Piquard R, Bohm C, Wakutani Y, Cupples LA, Cuenco KT, Green RC, Pinessi L, Rainero I, Sorbi S, Bruni A, Duara R, Friedland RP, Inzelberg R, Hampe W, Bujo H, Song YQ, Andersen OM, Willnow TE, Graff-Radford N, Petersen RC, Dickson D, der SD, Fraser PE, Schmitt-Ulms G, Younkin S, Mayeux R, Farrer LA, St George-Hyslop P. The neuronal sortilin-related receptor SORL1 is genetically associated with Alzheimer disease. Nat Genet. 2007;39(2):168–177. doi: 10.1038/ng1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reitz C, Cheng R, Rogaeva E, Lee JH, Tokuhiro S, Zou F, Bettens K, Sleegers K, Tan EK, Kimura R, Shibata N, Arai H, Kamboh MI, Prince JA, Maier W, Riemenschneider M, Owen M, Harold D, Hollingworth P, Cellini E, Sorbi S, Nacmias B, Takeda M, Pericak-Vance MA, Haines JL, Younkin S, Williams J, van Broeckhoven C, Farrer LA, St George-Hyslop PH, Mayeux R, Genetic and Environmental Risk in Alzheimer Disease 1 Consortium Meta-analysis of the association between variants in SORL1 and Alzheimer disease. Arch Neurol. 2011;68(1):99–106. doi: 10.1001/archneurol.2010.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Campion D, Charbonnier C, Nicolas G. SORL1 genetic variants and Alzheimer disease risk: a literature review and meta-analysis of sequencing data. Acta Neuropathol. 2019;138(2):173–186. doi: 10.1007/s00401-019-01991-4. [DOI] [PubMed] [Google Scholar]
- 62.Cuccaro ML, Carney RM, Zhang Y, Bohm C, Kunkle BW, Vardarajan BN, Whitehead PL, Cukier HN, Mayeux R, St. George-Hyslop P, Pericak-Vance MA. SORL1 mutations in early- and late-onset Alzheimer disease. Neurol Genet. 2016;2(6):e116. doi: 10.1212/NXG.0000000000000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Barthelson K, Newman M, Lardelli M. Sorting out the role of the sortilin-related receptor 1 in Alzheimer’s disease. J Alzheimers Dis Rep. 2020;4(1):123–140. doi: 10.3233/ADR-200177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet. 2019;51(3):414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses A, Haines J, Pericak-Vance M. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261(5123):921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 66.Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536(7616):285–291. doi: 10.1038/nature19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Holstege H, van der Lee SJ, Hulsman M, Wong TH, van Rooij JG, Weiss M, et al. Characterization of pathogenic SORL1 genetic variants for association with Alzheimer’s disease: a clinical interpretation strategy. Eur J Hum Genet. 2017;25(8):973–981. doi: 10.1038/ejhg.2017.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bellenguez C, Charbonnier C, Grenier-Boley B, Quenez O, Le Guennec K, Nicolas G, et al. Contribution to Alzheimer's disease risk of rare variants in TREM2, SORL1, and ABCA7 in 1779 cases and 1273 controls. Neurobiol Aging. 2017;59(220):e1–e9. doi: 10.1016/j.neurobiolaging.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 69.Gratuze M, Leyns CEG, Holtzman DM. New insights into the role of TREM2 in Alzheimer’s disease. Mol Neurodegener. 2018;13(1):66. doi: 10.1186/s13024-018-0298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jiang T, Tan L, Zhu XC, Zhang QQ, Cao L, Tan MS, Gu LZ, Wang HF, Ding ZZ, Zhang YD, Yu JT. Upregulation of TREM2 ameliorates neuropathology and rescues spatial cognitive impairment in a transgenic mouse model of Alzheimer’s disease. Neuropsychopharmacology. 2014;39(13):2949–2962. doi: 10.1038/npp.2014.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ulrich JD, Finn MB, Wang Y, Shen A, Mahan TE, Jiang H, Stewart FR, Piccio L, Colonna M, Holtzman DM. Altered microglial response to Abeta plaques in APPPS1-21 mice heterozygous for TREM2. Mol Neurodegener. 2014;9:20. doi: 10.1186/1750-1326-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kleinberger G, Yamanishi Y, Suarez-Calvet M, Czirr E, Lohmann E, Cuyvers E, et al. TREM2 mutations implicated in neurodegeneration impair cell surface transport and phagocytosis. Sci Transl Med. 2014;6(243):243ra86. doi: 10.1126/scitranslmed.3009093. [DOI] [PubMed] [Google Scholar]
- 73.Lill CM, Rengmark A, Pihlstrøm L, Fogh I, Shatunov A, Sleiman PM, Wang LS, Liu T, Lassen CF, Meissner E, Alexopoulos P, Calvo A, Chio A, Dizdar N, Faltraco F, Forsgren L, Kirchheiner J, Kurz A, Larsen JP, Liebsch M, Linder J, Morrison KE, Nissbrandt H, Otto M, Pahnke J, Partch A, Restagno G, Rujescu D, Schnack C, Shaw CE, Shaw PJ, Tumani H, Tysnes OB, Valladares O, Silani V, van den Berg LH, van Rheenen W, Veldink JH, Lindenberger U, Steinhagen-Thiessen E, SLAGEN Consortium. Teipel S, Perneczky R, Hakonarson H, Hampel H, von Arnim CAF, Olsen JH, van Deerlin VM, al-Chalabi A, Toft M, Ritz B, Bertram L. The role of TREM2 R47H as a risk factor for Alzheimer's disease, frontotemporal lobar degeneration, amyotrophic lateral sclerosis, and Parkinson's disease. Alzheimers Dement. 2015;11(12):1407–1416. doi: 10.1016/j.jalz.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kametani F, Hasegawa M. Reconsideration of amyloid hypothesis and tau hypothesis in Alzheimer’s disease. Front Neurosci. 2018;12:25. doi: 10.3389/fnins.2018.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang M, Ferrari R, Tartaglia MC, Keith J, Surace EI, Wolf U, Sato C, Grinberg M, Liang Y, Xi Z, Dupont K, McGoldrick P, Weichert A, McKeever PM, Schneider R, McCorkindale MD, Manzoni C, Rademakers R, Graff-Radford NR, Dickson DW, Parisi JE, Boeve BF, Petersen RC, Miller BL, Seeley WW, van Swieten JC, van Rooij J, Pijnenburg Y, van der Zee J, van Broeckhoven C, le Ber I, van Deerlin V, Suh ER, Rohrer JD, Mead S, Graff C, Öijerstedt L, Pickering-Brown S, Rollinson S, Rossi G, Tagliavini F, Brooks WS, Dobson-Stone C, Halliday GM, Hodges JR, Piguet O, Binetti G, Benussi L, Ghidoni R, Nacmias B, Sorbi S, Bruni AC, Galimberti D, Scarpini E, Rainero I, Rubino E, Clarimon J, Lleó A, Ruiz A, Hernández I, Pastor P, Diez-Fairen M, Borroni B, Pasquier F, Deramecourt V, Lebouvier T, Perneczky R, Diehl-Schmid J, Grafman J, Huey ED, Mayeux R, Nalls MA, Hernandez D, Singleton A, Momeni P, Zeng Z, Hardy J, Robertson J, Zinman L, Rogaeva E, International FTD-Genomics Consortium (IFGC) Ferrari R, Hernandez DG, Nalls MA, Rohrer JD, Ramasamy A, Kwok JBJ, Dobson-Stone C, Brooks WS, Schofield PR, Halliday GM, Hodges JR, Piguet O, Bartley L, Thompson E, Hernández I, Ruiz A, Boada M, Borroni B, Padovani A, Cruchaga C, Cairns NJ, Benussi L, Binetti G, Ghidoni R, Forloni G, Albani D, Galimberti D, Fenoglio C, Serpente M, Scarpini E, Clarimón J, Lleó A, Blesa R, Waldö ML, Nilsson K, Nilsson C, Mackenzie IRA, Hsiung GYR, Mann DMA, Grafman J, Morris CM, Attems J, Griffiths TD, McKeith IG, Thomas AJ, Pietrini P, Huey ED, Wassermann EM, Baborie A, Jaros E, Tierney MC, Pastor P, Razquin C, Ortega-Cubero S, Alonso E, Perneczky R, Diehl-Schmid J, Alexopoulos P, Kurz A, Rainero I, Rubino E, Pinessi L, Rogaeva E, St George-Hyslop P, Rossi G, Tagliavini F, Giaccone G, Rowe JB, Schlachetzki JCM, Uphill J, Collinge J, Mead S, Danek A, van Deerlin VM, Grossman M, Trojanowski JQ, van der Zee J, van Broeckhoven C, Cappa SF, Leber I, Hannequin D, Golfier V, Vercelletto M, Brice A, Nacmias B, Sorbi S, Bagnoli S, Piaceri I, Nielsen JE, Hjermind LE, Riemenschneider M, Mayhaus M, Ibach B, Gasparoni G, Pichler S, Gu W, Rossor MN, Fox NC, Warren JD, Grazia Spillantini M, Morris HR, Rizzu P, Heutink P, Snowden JS, Rollinson S, Richardson A, Gerhard A, Bruni AC, Maletta R, Frangipane F, Cupidi C, Bernardi L, Anfossi M, Gallo M, Elena Conidi M, Smirne N, Rademakers R, Baker M, Dickson DW, Graff-Radford NR, Petersen RC, Knopman D, Josephs KA, Boeve BF, Parisi JE, Seeley WW, Miller BL, Karydas AM, Rosen H, van Swieten JC, Dopper EGP, Seelaar H, Pijnenburg YAL, Scheltens P, Logroscino G, Capozzo R, Novelli V, Puca AA, Franceschi M, Postiglione A, Milan G, Sorrentino P, Kristiansen M, Chiang HH, Graff C, Pasquier F, Rollin A, Deramecourt V, Lebouvier T, Kapogiannis D, Ferrucci L, Pickering-Brown S, Singleton AB, Hardy J, Momeni P. A C6orf10/LOC101929163 locus is associated with age of onset in C9orf72 carriers. Brain. 2018;141(10):2895–2907. doi: 10.1093/brain/awy238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bergsma T and Rogaeva E. DNA methylation clocks and their predictive capacity for ageing phenotypes and healthspan. Neuroscience Insights, 2020 (Submitted). [DOI] [PMC free article] [PubMed]
- 77.Horvath S. DNA methylation age of human tissues and cell types. Genome Biol. 2013;14(10):R115. doi: 10.1186/gb-2013-14-10-r115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Horvath S, Ritz BR. Increased epigenetic age and granulocyte counts in the blood of Parkinson’s disease patients. Aging. 2015;7(12):1130–1142. doi: 10.18632/aging.100859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Horvath S, Langfelder P, Kwak S, Aaronson J, Rosinski J, Vogt TF, Eszes M, Faull RLM, Curtis MA, Waldvogel HJ, Choi OW, Tung S, Vinters HV, Coppola G, Yang XW. Huntington’s disease accelerates epigenetic aging of human brain and disrupts DNA methylation levels. Aging (Albany NY) 2016;8(7):1485–1512. doi: 10.18632/aging.101005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang M, Tartaglia MC, Moreno D, Sato C, McKeever P, Weichert A, Keith J, Robertson J, Zinman L, Rogaeva E. DNA methylation age-acceleration is associated with disease duration and age at onset in C9orf72 patients. Acta Neuropathol. 2017;134:271–279. doi: 10.1007/s00401-017-1713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang M, McKeever PM, Xi Z, Moreno D, Sato C, Bergsma T, et al. DNA methylation age acceleration is associated with ALS age of onset and survival. Acta Neuropathol. 2020;139(5):943–6 [DOI] [PMC free article] [PubMed]
- 82.Levine ME, Lu AT, Bennett DA, Horvath S. Epigenetic age of the pre-frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer's disease related cognitive functioning. Aging. 2015;7(12):1198–1211. doi: 10.18632/aging.100864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Degerman S, Josefsson M, Nordin Adolfsson A, Wennstedt S, Landfors M, Haider Z, Pudas S, Hultdin M, Nyberg L, Adolfsson R. Maintained memory in aging is associated with young epigenetic age. Neurobiol Aging. 2017;55:167–171. doi: 10.1016/j.neurobiolaging.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 84.Zhang M, Dilliott AA, Khallaf R, Robinson JF, Hegele RA, Comishen M, Sato C, Tosto G, Reitz C, Mayeux R, George-Hyslop PS, Freedman M, Rogaeva E. Genetic and epigenetic study of an Alzheimer's disease family with monozygotic triplets. Brain. 2019;142(11):3375–3381. doi: 10.1093/brain/awz289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Blennow K, Zetterberg H. Biomarkers for Alzheimer’s disease: current status and prospects for the future. J Intern Med. 2018;284(6):643–663. doi: 10.1111/joim.12816. [DOI] [PubMed] [Google Scholar]
- 86.Jack CR, Jr, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, Hampel H, Jagust WJ, Johnson KA, Knopman DS, Petersen RC, Scheltens P, Sperling RA, Dubois B. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539–547. doi: 10.1212/WNL.0000000000002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Allen M, Kachadoorian M, Quicksall Z, Zou F, Chai HS, Younkin C, Crook JE, Pankratz V, Carrasquillo MM, Krishnan S, Nguyen T, Ma L, Malphrus K, Lincoln S, Bisceglio G, Kolbert CP, Jen J, Mukherjee S, Kauwe JK, Crane PK, Haines JL, Mayeux R, Pericak-Vance MA, Farrer LA, Schellenberg GD, Alzheimer’s Disease Genetics Consortium (ADGC) Parisi JE, Petersen RC, Graff-Radford NR, Dickson DW, Younkin SG, Ertekin-Taner N. Association of MAPT haplotypes with Alzheimer’s disease risk and MAPT brain gene expression levels. Alzheimers Res Ther. 2014;6(4):39. doi: 10.1186/alzrt268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Niemantsverdriet E, Valckx S, Bjerke M, Engelborghs S. Alzheimer’s disease CSF biomarkers: clinical indications and rational use. Acta Neurol Belg. 2017;117(3):591–602. doi: 10.1007/s13760-017-0816-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iwatsubo T, Odaka A, Suzuki N, Mizusawa H, Nukina N, Ihara Y. Visualization of a beta 42(43) and a beta 40 in senile plaques with end-specific a beta monoclonals: evidence that an initially deposited species is a beta 42(43) Neuron. 1994;13(1):45–53. doi: 10.1016/0896-6273(94)90458-8. [DOI] [PubMed] [Google Scholar]
- 90.McDade E, Wang G, Gordon BA, Hassenstab J, Benzinger TLS, Buckles V, Fagan AM, Holtzman DM, Cairns NJ, Goate AM, Marcus DS, Morris JC, Paumier K, Xiong C, Allegri R, Berman SB, Klunk W, Noble J, Ringman J, Ghetti B, Farlow M, Sperling RA, Chhatwal J, Salloway S, Graff-Radford NR, Schofield PR, Masters C, Rossor MN, Fox NC, Levin J, Jucker M, Bateman RJ, for the Dominantly Inherited Alzheimer Network Longitudinal cognitive and biomarker changes in dominantly inherited Alzheimer disease. Neurology. 2018;91(14):e1295–ee306. doi: 10.1212/WNL.0000000000006277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Olsson B, Lautner R, Andreasson U, Öhrfelt A, Portelius E, Bjerke M, Hölttä M, Rosén C, Olsson C, Strobel G, Wu E, Dakin K, Petzold M, Blennow K, Zetterberg H. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15(7):673–684. doi: 10.1016/S1474-4422(16)00070-3. [DOI] [PubMed] [Google Scholar]
- 92.Toledo JB, Shaw LM, Trojanowski JQ. Plasma amyloid beta measurements - a desired but elusive Alzheimer’s disease biomarker. Alzheimers Res Ther. 2013;5(2):8. doi: 10.1186/alzrt162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shi L, Baird AL, Westwood S, Hye A, Dobson R, Thambisetty M, Lovestone S. A decade of blood biomarkers for Alzheimer’s disease research: an evolving field, improving study designs, and the challenge of replication. J Alzheimers Dis. 2018;62(3):1181–1198. doi: 10.3233/JAD-170531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hampel H, Vergallo A, Afshar M, Akman-Anderson L, Arenas J, Benda N, Batrla R, Broich K, Caraci F, Cuello AC, Emanuele E, Haberkamp M, Kiddle SJ, Lucía A, Mapstone M, Verdooner SR, Woodcock J, Lista S. Blood-based systems biology biomarkers for next-generation clinical trials in Alzheimer’s disease. Dialogues Clin Neurosci. 2019;21(2):177–191. doi: 10.31887/DCNS.2019.21.2/hhampel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ovod V, Ramsey KN, Mawuenyega KG, Bollinger JG, Hicks T, Schneider T, Sullivan M, Paumier K, Holtzman DM, Morris JC, Benzinger T, Fagan AM, Patterson BW, Bateman RJ. Amyloid beta concentrations and stable isotope labeling kinetics of human plasma specific to central nervous system amyloidosis. Alzheimers Dement. 2017;13(8):841–849. doi: 10.1016/j.jalz.2017.06.2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nabers A, Perna L, Lange J, Mons U, Schartner J, Guldenhaupt J, et al. Amyloid blood biomarker detects Alzheimer’s disease. EMBO Mol Med. 2018;10(5). [DOI] [PMC free article] [PubMed]
- 97.Palmqvist S, Janelidze S, Stomrud E, Zetterberg H, Karl J, Zink K, et al. Performance of fully automated plasma assays as screening tests for Alzheimer disease-related beta-amyloid status. JAMA Neurol. 2019. [DOI] [PMC free article] [PubMed]
- 98.Kaneko N, Nakamura A, Washimi Y, Kato T, Sakurai T, Arahata Y, et al. Novel plasma biomarker surrogating cerebral amyloid deposition. Proc Jpn Acad Ser B Phys Biol Sci. 2014;90(9):353–364. doi: 10.2183/pjab.90.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gisslén M, Price RW, Andreasson U, Norgren N, Nilsson S, Hagberg L, Fuchs D, Spudich S, Blennow K, Zetterberg H. Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine. 2016;3:135–140. doi: 10.1016/j.ebiom.2015.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mattsson N, Andreasson U, Zetterberg H, Blennow K. Alzheimer’s disease neuroimaging I. Association of Plasma Neurofilament Light With Neurodegeneration in Patients With Alzheimer Disease. JAMA Neurol. 2017;74(5):557–566. doi: 10.1001/jamaneurol.2016.6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Preische O, Schultz SA, Apel A, Kuhle J, Kaeser SA, Barro C, et al. Serum neurofilament dynamics predicts neurodegeneration and clinical progression in presymptomatic Alzheimer’s disease. Nat Med. 2019;25(2):277–283. doi: 10.1038/s41591-018-0304-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Brier MR, Gordon B, Friedrichsen K, McCarthy J, Stern A, Christensen J, et al. Tau and Aβ imaging, CSF measures, and cognition in Alzheimer's disease. Sci Transl Med. 338;2016(8):338ra66. [DOI] [PMC free article] [PubMed]
- 103.Chhatwal JP, Schultz AP, Marshall GA, Boot B, Gomez-Isla T, Dumurgier J, LaPoint M, Scherzer C, Roe AD, Hyman BT, Sperling RA, Johnson KA. Temporal T807 binding correlates with CSF tau and phospho-tau in normal elderly. Neurology. 2016;87(9):920–926. doi: 10.1212/WNL.0000000000003050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gordon BA, Friedrichsen K, Brier M, Blazey T, Su Y, Christensen J, Aldea P, McConathy J, Holtzman DM, Cairns NJ, Morris JC, Fagan AM, Ances BM, Benzinger TLS. The relationship between cerebrospinal fluid markers of Alzheimer pathology and positron emission tomography tau imaging. Brain. 2016;139(Pt 8):2249–2260. doi: 10.1093/brain/aww139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jack CR, Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, Holtzman DM, Jagust W, Jessen F, Karlawish J, Liu E, Molinuevo JL, Montine T, Phelps C, Rankin KP, Rowe CC, Scheltens P, Siemers E, Snyder HM, Sperling R, Elliott C, Masliah E, Ryan L, Silverberg N. NIA-AA research framework: toward a biological definition of Alzheimer's disease. Alzheimers Dement. 2018;14(4):535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Benzinger TL, Blazey T, Jack CR, Jr, Koeppe RA, Su Y, Xiong C, et al. Regional variability of imaging biomarkers in autosomal dominant Alzheimer’s disease. Proc Natl Acad Sci U S A. 2013;110(47):E4502–E4509. doi: 10.1073/pnas.1317918110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Knight WD, Okello AA, Ryan NS, Turkheimer FE, Rodriguez Martinez de Llano S, Edison P, et al. Carbon-11-Pittsburgh compound B positron emission tomography imaging of amyloid deposition in presenilin 1 mutation carriers. Brain. 2011;134(Pt 1):293–300. doi: 10.1093/brain/awq310. [DOI] [PubMed] [Google Scholar]
- 108.Rowley PA, Samsonov AA, Betthauser TJ, Pirasteh A, Johnson SC, Eisenmenger LB. Amyloid and Tau PET imaging of Alzheimer disease and other neurodegenerative conditions. Seminars in Ultrasound, CT and MRI. 2020. [DOI] [PubMed]
- 109.Gordon BA, Blazey TM, Christensen J, Dincer A, Flores S, Keefe S, Chen C, Su Y, McDade EM, Wang G, Li Y, Hassenstab J, Aschenbrenner A, Hornbeck R, Jack CR, Jr, Ances BM, Berman SB, Brosch JR, Galasko D, Gauthier S, Lah JJ, Masellis M, van Dyck CH, Mintun MA, Klein G, Ristic S, Cairns NJ, Marcus DS, Xiong C, Holtzman DM, Raichle ME, Morris JC, Bateman RJ, Benzinger TLS. Tau PET in autosomal dominant Alzheimer’s disease: relationship with cognition, dementia and other biomarkers. Brain. 2019;142(4):1063–1076. doi: 10.1093/brain/awz019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Moller C, Vrenken H, Jiskoot L, Versteeg A, Barkhof F, Scheltens P, et al. Different patterns of gray matter atrophy in early- and late-onset Alzheimer’s disease. Neurobiol Aging. 2013;34(8):2014–2022. doi: 10.1016/j.neurobiolaging.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 111.Rabinovici GD, Furst AJ, Alkalay A, Racine CA, O'Neil JP, Janabi M, et al. Increased metabolic vulnerability in early-onset Alzheimer's disease is not related to amyloid burden. Brain. 2010;133(Pt 2):512–528. doi: 10.1093/brain/awp326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cho H, Choi JY, Lee SH, Lee JH, Choi YC, Ryu YH, Lee MS, Lyoo CH. Excessive tau accumulation in the parieto-occipital cortex characterizes early-onset Alzheimer’s disease. Neurobiol Aging. 2017;53:103–111. doi: 10.1016/j.neurobiolaging.2017.01.024. [DOI] [PubMed] [Google Scholar]
- 113.Scholl M, Ossenkoppele R, Strandberg O, Palmqvist S, Fs SB, Jogi J, et al. Distinct 18F-AV-1451 tau PET retention patterns in early- and late-onset Alzheimer's disease. Brain. 2017;140(9):2286–2294. doi: 10.1093/brain/awx171. [DOI] [PubMed] [Google Scholar]
- 114.Holland D, Desikan RS, Dale AM, LK ME. Alzheimer’s Disease Neuroimaging I. Rates of decline in Alzheimer disease decrease with age. PLoS One. 2012;7(8):e42325. doi: 10.1371/journal.pone.0042325. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A.