Abstract
This study explored narrative responses following abnormal Pap tests among Hispanic migrant farmworkers (N = 18; ages 22–50 years) via in-depth interviews in Florida. Qualitative analyses utilized health literacy domains (obtain/process/understand/communicate) as a conceptual framework. Participants described how they (1) obtained information about getting a Pap test, (2) processed positive and negative reactions following results, (3) understood results and recommended health-promoting behaviors, and (4) communicated and received social support. Women had disparate reactions and understanding following an abnormal Pap result. Health literacy was a meaningful conceptual framework to understand assets and gaps among women receiving an abnormal Pap test result. Future interventions should incorporate health literacy domains and facilitate patient–provider communications and social support to assist women in decision-making and health-promoting behaviors, ultimately decreasing cancer disparities.
Keywords: cancer, community health promotion, culture, health promotion, health psychology, women’s health
Introduction
As of 2016, in the United States, an estimated 13,000 women will be diagnosed with cervical cancer, while nearly 4,100 will die annually from this preventable cancer (National Cancer Institute, n.d.-b). Hispanic women have the highest incidence rate of cervical cancer (10.2 new cases per 100,000 women) and third highest cervical cancer mortality rate (2.8 deaths per 100,000 women) compared to other racial and ethnic groups (National Cancer Institute, n.d.-a). Hispanic migrant farmworkers are particularly at risk due to limited access to prevention and treatment efforts (Mills et al., 2006, 2009).
Dramatic decreases in cervical cancer morbidity and mortality have been documented over the past several decades, largely due to the introduction of the Pap test, which is a cancer screening procedure that detects abnormal changes in cervical cells. Currently, the US Preventive Services Task Force recommends women aged 21–65 years, regardless of sexual history, receive a Pap test every 3 years or women aged 30–65 years complete both a Pap test and human papillomavirus (HPV) test every 5 years (US Preventive Services Task Force, 2012).
An abnormal Pap test is when cell changes are found on the cervix (Centers for Disease Control and Prevention, 2015). Depending on doctors’ recommendations, potential strategies for treating an abnormal Pap test can include increased surveillance, biopsy, or treatment of cervical dysplasia. Hispanic women, however, often face barriers to these doctors’ recommendations that include low knowledge regarding implications of a Pap test result, negative health beliefs, anxiety or fear, pain, and other personal and professional responsibilities (e.g. childcare, work) that interfere with scheduling and attending appointments (Breitkopf et al., 2005; Del Carmen et al., 2007; Eggleston et al., 2007; Percac-Lima et al., 2010). Moreover, navigating the healthcare system following an abnormal Pap test requires women to possess complex knowledge and skills, which can be increasingly difficult given the presence of psychosocial and structural barriers.
Health literacy serves as a potential mechanism to facilitate the required multidimensional skill sets needed to make informed healthcare decisions that are critical in preventing the progression of advanced stage of disease. Specifically, health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (Institute of Medicine, 2004). Previous research has identified health literacy as an integral component to Pap testing in different populations (e.g. African Americans, Hispanics, and Caucasian). However, it has been traditionally applied using objective, quantitative measures. For example, poor health literacy has been associated with low knowledge of Pap testing among women, and served as a stronger predictor of Pap testing knowledge than ethnicity or education (Lindau et al., 2002). Additionally, inadequate health literacy among Hispanic women has been found to decrease the likelihood of ever having a Pap test (Garbers and Chiasson, 2004). Furthermore, health literacy is a key determinant to health (Institute of Medicine, 2009) and has been shown to be a more important predictor than age, race/ethnicity, and income across a range of health outcomes (DeWalt et al., 2004; Weiss et al., 2007).
The application of qualitative methodology to understand health literacy from the patient’s perspective has revealed a deeper dimension of skills that are required, including knowing when and where to find health information, reading/ comprehension, evaluating information, communication, and assertiveness to use and apply these skills (Jordan et al., 2010). Yet, limited research has employed qualitative research methodology to understand the complexities of health literacy as it applies to cervical cancer prevention. Previous research has examined health literacy only as an outcome (Thorburn et al., 2013; Tu and Wang, 2013), rather than an analytic framework that can inform one’s ability to access, understand, and use health information and services. While research supports the association between health literacy and Pap testing, there is a need to understand the lived experiences of women receiving an abnormal Pap test result within the health literacy framework as follow-up care is crucial to prevent progression to advance disease. Thus, a qualitative approach is a fitting methodology to explore these experiences and can further elucidate rich meanings that structure women’s narratives and future decision-making.
The purpose of this exploratory qualitative study was to employ a health literacy analytic framework to explore narrative responses following an abnormal Pap test result among women living in a Hispanic migrant farmworker community. Specifically, the following four health literacy domains were operationalized as major themes related to receiving an abnormal Pap test result: obtain, process, understand, and communicate. It is expected that participants will have limited understanding of the Pap test and their results and that family, culture, and their lived experiences may impact their decision-making processes given this complex and sensitive health issue. A greater understanding of Hispanic migrant women’s experiences across these health literacy domains can help inform patient-centered strategies that assist women in coping with their abnormal Pap test result and engaging in subsequent health promotion behaviors.
Methods
Overview
This study was developed using the Social Cognitive Theory and health literacy–related constructs. Social Cognitive Theory posits that there is a reciprocal relationship between personal factors, environmental factors (social and physical), and a person’s behavior (McAlister et al., 2008). Key constructs utilized included outcome expectancies, outcome expectations, motivation, facilitation, self-regulation, and behavioral capability related to engaging in the necessary follow-up care following an abnormal Pap test result (McAlister et al., 2008). Health literacy domains (obtain, process, understand, communicate) were also used to capture skills and attributes that served as facilitators or barriers to obtaining follow-up care for an abnormal Pap test (Institute of Medicine, 2004).
Setting
Participants were recruited from a local, rural, faith-based primary care clinic where they received Pap testing, which serves low-income migrant families and is located in central west Florida. The clinic is managed by a bilingual physician assistant and staffed by a bilingual registered nurse and volunteer physicians from a nearby university hospital system. A bilingual, bicultural female Hispanic patient navigator who lives in the community also provides patient education and social support services. Participants received the results for the abnormal Pap from this clinic either via a postcard or a follow-up call from the patient navigator telling them that they needed to come into the clinic.
Sampling and recruitment
A trusted patient navigator first contacted potential participants to introduce the study and obtain permission for the research assistant to follow up with more information. If participants were still interested and eligible to participate, the research assistant scheduled an interview at a time and location of the participants’ convenience. Eligibility criteria included (1) female, (2) 21–70 years old, (3) Hispanic, (4) having an abnormal Pap test in the past 36 months, (5) able to speak English or Spanish, (6) able to provide informed consent, and (7) residing in central west Florida. Initially, purposive sampling was used to recruit women who had received an abnormal Pap test, based on time since receiving their test result (<6 months or ⩾6 months) to capture experiences across the continuum of care following receipt of an abnormality. However, few women experienced an abnormal Pap test during the recruitment period. Therefore, the majority of the sampling frame included women who had received an abnormal Pap test result at least 1 year prior to recruitment.
Data collection
A semi-structured interview guide was developed and assessed for content and face validity by the research team. A semi-structured interview guide includes topical areas that elicit data that correspond to main research questions and theoretical underpinnings; these topical areas guide the interview but allow space for participants to expand and discuss information that is relevant to them. Additionally, the patient navigator provided feedback on acceptability and suggestions for additional questions. A brief participant profile survey was also developed to collect data on the following sociodemographic factors: age, race/ethnicity, marital status, country of origin, years of residence in the United States, educational attainment, languages spoken/read, and employment status. Some of the questions that guided the in-depth interviews included the following: “Tell me about the place or person from whom you receive medical care. (obtain); Many women have different reactions to an abnormal Pap. Tell me about the first time that you heard that you had an abnormal Pap.”; “How do you feel about your abnormal Pap now that some time has passed?” (process) (full interview guide available upon request).
Interviews were conducted by a bilingual research assistant who has training and experience conducting interviews in English and Spanish. Written informed consent was obtained prior to each interview, and the research assistant orally administered the participant profile survey. Each interview was audio-recorded, translated, and transcribed verbatim by a professional bilingual translator. Interviews lasted between 20 and 60 minutes, with an average time of 42 minutes (standard deviation (SD) = 10.97). This study was approved by the University of South Florida’s Institutional Review Board.
Data analysis
Research team members developed an initial codebook based on a priori health literacy themes. Using a thematic analysis approach based on a priori codes, three research team members read through the transcripts via open coding to identify the themes related to participants’ reactions to the Pap test abnormality. Specifically, a constant-comparative thematic analysis approach (keeping each of the domains mutually exclusive of the other) was utilized to explore how health literacy domains shape Hispanic migrant women’s Pap test experiences. Constant-comparative thematic analysis compares each theme of all participants so that all instances are compared to each other (Guest et al., 2011). Team members then created analytic notes to document themes emerging from the data (Patton, 2002). Upon further discussion and analysis, commonalities in the themes and how they related to health literacy domains emerged (obtain, process, understand, and communicate). The codebook was constantly refined as new data were collected including subthemes that emerged. During meetings, team members discussed themes and subthemes and came to consensus on any discrepancies in thematic definitions. Discrepancies in coding were discussed and agreed upon. Two additional transcripts, 10 percent of the sample, were coded separately to calculate a kappa statistic of 0.82, indicating “almost perfect agreement” between coders (Bernard and Ryan, 2010). The kappa statistic was calculated on the entire codebook; since codes were developed a priori, it was expected that the overall rate should be consistent across all codes. All coding and analysis was conducted with ATLAS.ti 6.2. Although the interview guide was based on the theoretical frameworks of Social Cognitive Theory and Health Literacy, this article only focuses on these health literacy narratives in which the women richly described. Findings related to the a priori themes guided by Social Cognitive Theory (e.g. behavioral capability, self-regulation) are being reported elsewhere.
Results
A total of 18 women were recruited and interviewed for this study, 15 with a Pap test abnormality that had been discovered 1 year or longer, and 3 whose abnormal Pap test had been obtained within the past year. Ages ranged from 22 to 50 years (mean (M) = 40 years; SD = 7.9 years). All self-identified as Hispanic and of Mexican origin. All women spoke Spanish as their primary language, except for one participant whose native language was Tzotzil. Among those women working part-or full-time, employment types/settings included agriculture, cleaning, packing plants, supermarket, sewing, or restaurants (see Table 1).
Table 1.
Participant demographics (N = 18).
| Characteristic | Number (%) |
|---|---|
| Marital status | |
| Single | 7 (39) |
| Married | 9 (50) |
| Divorced/separated | 2 (11) |
| Years lived in the United States | |
| 5–9 years | 7 (39) |
| 10–19 years | 6 (33) |
| ⩾20 years | 5 (28) |
| Level of education completed | |
| No education | 3 (17) |
| Elementary school | 8 (44) |
| Some high school | 1 (6) |
| Completed high school | 4 (22) |
| Some university education | 2 (11) |
| Employment status | |
| Part-time | 2 (11) |
| Full-time | 8 (44) |
| Unemployed | 8 (44) |
| Annual income | |
| US$1-US$9999 | 2 (11) |
| US$10,000-US$19,999 | 12 (67) |
| US$20,000-US$29,999 | 3 (17) |
| US$30,000-US$39,999 | 1 (6) |
The salient themes emerging from each participant’s narrative were organized under the four overarching domains of the health literacy framework: obtain, process, understand, and communicate (see Table 2). Specifically, throughout each “Pap story,” participants described (1) how she obtained her Pap test and abnormal result, (2) how she emotionally processed the abnormal test result, (3) how she currently understands what an abnormal result means for her health and recommended future health behaviors, and (4) communication and discourse experiences with healthcare providers, spouses/partners, and female friends, respectively (Figure 1).
Table 2.
Participant quotations by health literacy domains.
| Theme—subtheme | Exemplary quotes (participant number in parentheses) |
|---|---|
| Obtain | “I find out regarding this clinic’s care through a friend that had come here. They found out she had abnormal cells; so after her experience here she mentioned to me […] She was a co-worker many years ago but we are still friends, we know each for very long time.” (P2) “[I found out about the clinic] through a girlfriend that told me because in reality I don’t have the resources to go to the doctor so she told me to go to [clinic name] that everything was free or that I could give a donation and they would accept you. I went and found that it was totally free, that’s how I found out.” (P5) “Someone I know told me that they do the exams very well and they don’t charge you because when you don’t have insurance its more expensive to go see a particular doctor. They gave me the address and I came, and I liked, thanks God. They have done very well with my exams, though sometimes they haven’t come out good.” (P10) |
| Process—Initial Emotional Reaction | “Many questions come to you and a lot of fears thinking that it may be cancer because one doesn’t know about that illness. So when they tell you ‘It’s abnormal’ you think it’s cancer, it’s the first thing that comes to your mind, to think that it’s cancer.” (P7) “I was very distressed by what I had. I was worried because I thought I was going to die.” (P6) “The first time … when they gave me the results I felt sad because the first thing I thought about was my children … my children are young, they need me because I have never been sick … and since I don’t have the income to go to the hospital to take care of it, I was afraid that I wasn’t going to live.” (P5) |
| Process—Negative Reaction | “You think to yourself that if you have that [cancer], they just remove the uterus, I think and I don’t know what else could happen too, that worried me. It worried me because I still have this 8 year old girl, and the other is 15 years old … that’s what worries me.” (P9) “I was scared because one always thinks the worse when they call to say that something came out bad, one thinks is cancer, and what else can one think?” (P3) “Thinking that having an abnormal Pap meant I had terminal cancer, that’s what I thought—that having an abnormal Pap smear, for me was a terminal cancer.” (P15) |
| Process—Positive Reaction | “My positive thought was when I realized that I was in a place where there are many opportunities. I am in a place where it’s not like in my country where if you are sick, they don’t care and here even though you are illegal they help you.” (P5) “I asked God that it wouldn’t be something bad. I said ‘I wish I don’t have anything that it isn’t something …’ an infection is okay, it can be cured with medicine, right? Because we have always, had an infection of anything, vaginal or something, right? I thought on not having anything, that everything was okay.” (P11) “I didn’t get too scared, only for a little while, only at first but after that I know that God is the one who made us and we can get through it.” (P10) |
| Understand—Current Health | “Abnormal is when it comes out with an illness, when they detect something that is not right, that’s what I understand as an abnormal Pap.” (P5) “I guess that it means that one of your body parts, I mean like infection … I guess it’s like a spoiled apple that is getting spoiled from one side but the other is fine. I guess that’s how we are.” (P4) “An abnormal Pap smear is like the beginning of a pre-cancer. Not cancer, but pre-cancer because we are in a stage like what the doctor said, they’re cells that are reproducing and they get to an organ that they invade like roots and that’s when cancer starts to expand everywhere but if you extract the cells, then you’re ripping out the roots. For me it’s like an abnormal Pap smear is a pre-cancer.” (P15) |
| Understand—Future Actions | “With the abnormal pap? Well, you could get depressed from thinking you’re not okay, and waiting for the results, which sometimes take a long time to tell you whether it was cancer or it’s just abnormal; I think that our body starts changing depending what they are telling you from the results.” (P7) “Move forward, go to appointments with the doctors and get their explanations that I can continue moving forward or anything else. Not to let it go, to move forward until getting to the end of it.” (P4) “Well, to follow all doctors’ instructions, for example, like when my results were bad, when the lady called me to tell me my results were abnormal, that I need to come; I mean to obey and do what they tell you to do.” (P3) |
| Communicate | “She is like my confidant and I don’t even know her. When I talk to her, she is my angel … I feel God put her in my way.” (P18) “I told [other girlfriends] about my experience, I felt the need to share that with them, with other girlfriends that had not done the Pap smear for years. I felt that I needed to tell them so they were aware that they may also have something like me.” (P5) “My husband tells me sometimes you have to calm down because I get anxious thinking about it being cancer, or just waiting for the results … it’s nerve wracking just waiting for the results.” (P7) |
Figure 1.
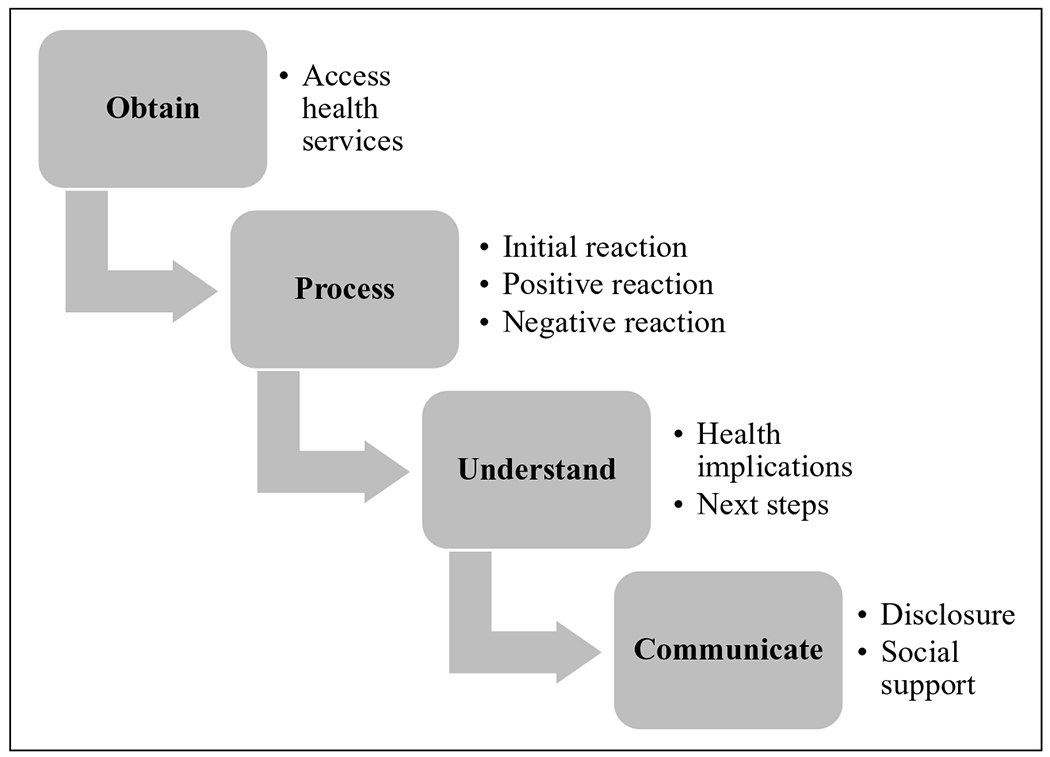
Key findings by health literacy framework.
Obtain
The first narrative focused on participants’ reports on where they would usually go for primary care services, how and/or from whom they learned about the clinic, and their reflections regarding how/when they found out about their abnormal test results. In general, not all women had a primary source of health care, leading to differences in how they ended up at the clinic. Most of the participants (n = 11) received their primary care at the clinic from which they were recruited, and from these, some (n = 3) also visited other clinics. Other women (n = 4) mentioned receiving their primary care from other nearby clinics. When describing how they knew or heard about the clinic, participants mentioned different sources such as friends (n = 5), neighbors or coworkers (n = 3), familiarity with the location of the clinic (n = 2), a patient navigator (n = 1), and during a health fair that took place in the community (n = 1). Of interest, participants did not explicitly elaborate on the exact point in time when they received the abnormal Pap result, but did reflect on how they processed, understood, and communicated to others regarding their test results, which is further described below in the corresponding sections.
Process
Participants experienced varying positive and negative reactions after receiving the abnormal Pap test result. When asked about their experience of receiving their abnormal Pap test results, almost all women (n = 17) mentioned a negative reaction. Of those, approximately half (n = 8) stated that they initially felt scared or afraid. Specifically, these women were scared as they believed their diagnosis meant that they had cancer (n = 5) or because this was the first time they had an abnormal result and did not know what it meant (n = 5).
When participants first learned of their abnormal Pap test result, they also went through an initial process of explaining and reconciling their diagnosis. Most often women initially thought that their abnormal Pap test result meant that they had cancer (n = 9) and were going to die (n = 7). Other women explicitly stated they were worried (n = 6) or sad (n = 4). Those who were sad said they initially thought about their family and what it would mean for them (n = 3) and/or also because they thought they were going to die (n = 3). Participants also described how they worried about what the next steps of treatment entailed (n = 3).
After participants’ initial reactions to hearing their test results, they continued to experience both negative and positive emotional responses when trying to process what this test result meant. For example, most (n = 12) participants mentioned having some sort of negative emotional reaction to the diagnosis even after some time passed. While some participants initially processed thoughts about their family and loved ones, others (n = 5) mentioned that they continued to be worried and upset for their families even after some time had passed. Other women worried about how they were going to get the care they needed (n = 3) and what type of treatment they would need (n = 4).
When asked “What positive thoughts did you have after the diagnosis?” about half of the women (n = 11) were able to identify positive thoughts or good things that came to their mind. Positive thoughts were with regard to two different phenomena: living in a country where there are trained medical personnel who can treat them (n = 6) and God (n = 4). Participants compared their experiences of previously living in a country where they perceived that medical professionals were not trained to deal with their diagnosis compared to now living in the United States where they could get treatment. Those who mentioned God stated they were putting their health outcomes in the hands of a higher power.
Understand
After participants described how they learned of their abnormal Pap test result and attempted to process this, they then described their current level of understanding of what an abnormal Pap test result meant for their lives. Specifically, the discussion focused on (1) what they interpreted that an abnormal Pap test result meant for their health (n = 16) and (2) their understanding of particular health behaviors and actions that they should be doing following their abnormal test result (n = 15).
When participants described what an abnormal Pap test result meant to them, a spectrum of level of understanding emerged. Few participants reported having no understanding of what an abnormal test result meant for their health (n = 2). Other participants had very limited understanding of what an abnormal Pap test meant, describing that a “positive” or abnormal test result coincided with something bad happening in their bodies (n = 9). However, on the other hand, some women had a deeper understanding of what an abnormal test result indicated (n = 4), such as pre-cancerous activity in the cervix. Overall, most women recognized that the abnormal test result did not mean they had cancer, but rather this was a stage in the disease that could potentially lead to cancer. However, there was confusion regarding what caused an abnormal Pap test result, as some women believed that age, injections, or negligence could be causal factors, whereas others were unsure what causes the abnormality.
Additionally, when describing the future uncertainty that resulted from an abnormal Pap test, women were aware of not only the physical health consequences, but also the mental health effects (n = 4). For example, women discussed the range of psychosocial responses to an abnormal Pap test, such as worry and depression, which could further obfuscate their health and well-being.
The second component of participants’ understanding related to the actions or steps that women should do following an abnormal Pap test result to promote or improve her health. For instance, there was a clear trust in the physicians for directing women in next steps (n = 9). Furthermore, participants described recommended healthcare interactions in the future, such as follow-up tests and additional screenings every 6 months to a year (n = 12).
Women also described other personal behaviors that they could engage in to improve their overall health (n = 4). These behaviors mostly focused on healthy eating and exercising. Finally, there were some participants (n = 3) who reported being unsure of what they should to do following their abnormal Pap test result.
Communicate
Almost all of the participants (n = 17) told at least one other person about their abnormal Pap test result. Half of the women (n= 7) told a partner or husband, while 10 participants told female friends or relatives. Specifically, participants disclosed their test results to their daughters (n = 4), mothers (n = 3), sisters (n = 3), friends in “real life” (n = 2), and friends on “Facebook” (n = 2). Interestingly, three women mentioned telling their sisters and friends their results in order to make them aware that they needed to get a Pap test. Additionally, one woman only told a friend that she randomly met on Facebook even though the two had never met each other.
Women who disclosed their diagnosis often received at least one of the four forms of social support: emotional, instrumental, informational, and appraisal (House, 1981). In addition to being recipients of social support, participants (n = 5) also provided informational support to some of those to whom they disclosed (mostly regarding the importance of a Pap test and where to receive testing), resulting in a relationship of reciprocity. Specifically, after participants received their abnormal Pap test result, they wanted to make sure other women knew about the importance of getting the Pap test, so they took on a health educator role for their family and friends.
In general, most women (n = 11) received emotional support from those to whom they disclosed their abnormal Pap test result. This often came in the form of reassurances that everything would be alright, asking them how they felt, and decreasing their anxieties about subsequent test results.
Some women (n = 4) also received instrumental support from their family and friends. This support came in the form of giving the woman a ride to the doctor’s office and accompanying them to their appointments. Two women received appraisal support from the people to whom they disclosed their test results. This appraisal support came in the form of comparing the healthcare systems with regard to training and access in the United States to that of Mexico.
Discussion
Similar to other research that explored the “patient journey” to describe health literacy from the patient’s perspective (Jordan et al., 2010: 38), this study utilized a health literacy framework to explore the narratives of Hispanic migrant farmworker women following an abnormal Pap test result. Four major health literacy domains were identified among the women’s stories of receiving an abnormal Pap test result: obtain, process, understand, and communicate. Women described how they obtained the information to get a Pap test from family, friends, neighbors, or coworkers. Additionally, some women were aware of the health clinic or patient navigator prior to going to get her Pap test. As other research found (Daley et al., 2010, 2015; Newton and McCabe, 2008), participants then experienced two initial processes after receiving the abnormal Pap test result: emotional reactions (e.g. worry, sadness, faith in God) and cognitive reactions (e.g. thinking about origin of HPV infection). Finally, participants’ current level of understanding of what an abnormal test result meant for them occurred over a continuum, with some women demonstrating advanced knowledge, while others had very limited knowledge. Discussions also focused on interpreting what an abnormal Pap test result meant for their health (e.g. needing to undergo follow-up examinations), as well as ideas regarding what they could do after getting an abnormal Pap test result (e.g. follow physician instructions, eat healthy, exercise).
Participants discussed processing the abnormal test result with negative emotional reactions including being scared or afraid. However, believing in God and living in a country (United States) where they could get treatment were mentioned as positive factors that helped them process their result. In addition, having a partner, friends, or other female family member with whom they could disclose their experience of having an abnormal Pap test, and the resulting social support, greatly aided women during their experiences. Other research has also found that having supportive relationships assists women in dealing with an abnormal Pap test (Monsonego et al., 2011).
During the understanding phase, participants in this study discussed the importance of following physicians’ directions and complying with the recommended follow-up care. However, women were less clear about what the abnormal Pap test really meant, and reported a gradient of understanding of the abnormality. Previous research has shown that Hispanic women have limited knowledge about cervical cancer screening (Scarinci et al., 2003). Additionally, discrepancies between the literacy level of the cancer screening information and with what providers want to share with their patients, with what low-income African American and Hispanics patients are actually able to understand have been reported in the literature (Simon et al., 2010). However, there is limited research regarding women’s understanding of an abnormal Pap test. Thus, given the potential severity of an abnormal cervical cancer screening test, women need to be better informed regarding potential future sequelae. Since these women placed trust in their healthcare providers, future research should examine the patient-provider interaction to determine effective patient-centered communication techniques and how best to facilitate shared decision-making regarding follow-up care when delivering this type of information. Enhancing such patient-provider communications may increase patients’ health literacy levels, ultimately contributing to women’s knowledge and skills that are critical in preventing advanced stages of disease.
Notwithstanding, the above findings must be considered in light of study limitations. As characteristic of all qualitative research, findings are not generalizable. Participants were recruited from one local community clinic in central west Florida, and all women were originally from Mexico. Although efforts were made to recruit women with varying time since receiving their test results, most women received their test result at least 1 year prior to the interview. Thus, significant time may have elapsed since the abnormal Pap test, making it difficult for women to recall the experience. Additionally, women had variation in the severity of the cervical abnormality, with some requiring surveillance, and others requiring more invasive follow-up testing and treatment. These factors may impact their understanding regarding the cervical abnormality that was discovered. Furthermore, the sample size was small, and although data redundancy was reached, whether data saturation was achieved remains unknown. However, meaningful and credible findings were able to be produced even given the smaller sample size (Sandelowski, 1995). The Pap story narratives emerged from the data although participants were not explicitly asked to tell their “story.” Although these emerging data are powerful, the fact that we did not ask each participant to provide the story regarding their experience with an abnormal Pap test limited our analysis as not all participants discussed all themes during the interviews. Consequently, in order to fully understand how health literacy frames women’s experiences from receiving an abnormal Pap test result, future research should focus additional in-depth explorations of women’s experiences in obtaining, processing, understanding, and communicating with regard to cervical cancer prevention information and services. It is expected that results would be similar to the findings of this study, as all women were able to include at least one piece to the health literacy puzzle in their Pap story narrative.
Finally, while the health literacy framework was able to explain some of the phenomena among women’s experiences of receiving an abnormal Pap test result, there are some limitations in its application. First, the researchers applied this framework as distinct stages to the accounts women provided. It is possible that women did not experience their diagnoses in such a linear fashion used in this study. Second, the field of health literacy is still evolving (Paasche-Orlow et al., 2010; Pleasant et al., 2011). Existing frameworks for health literacy lack a comprehensive and multidimensional approach, which limit current research on this topic (Pleasant et al., 2011). Extending this issue, other factors of health literacy beyond obtain, process, understand, and communicate could add utility to understanding how women experience an abnormal Pap test result. These could be proximal or distal forces that impact a person’s health literacy level, including but not limited to educational attainment, income, language, family and social environment, physical environment, media, culture, and political forces (Sørensen et al., 2012). These factors were not explicitly taken into account during this study and should be included in future research to identify antecedents and other contextual factors that influence the health literacy process following an abnormal Pap test result.
This exploratory qualitative study builds on previous research related to health literacy framework and women’s experiences with receiving an abnormal Pap diagnosis. Study findings also build on previous research regarding Hispanic migrant workers’ experiences regarding access to healthcare information and services and engaging in primary and secondary prevention of cervical cancer. The narrative accounts in this study were applicable to all of the four domains of the health literacy framework. Overall, this study found that women tend to have disparate reactions and understanding following an abnormal Pap result, which may impact the effectiveness of follow-up care. Multiple health education/information sharing opportunities may be needed to have patients understand patient-specific follow-up care in a clear format. Additionally, materials need to be culturally and linguistically appropriate and sensitive. Future research should explore what are the best methods (pamphlets, patient navigator, peer-to-peer) to provide this information that will facilitate understanding and evaluation of treatment options and how to communicate this to providers and family members. Such health education/information materials should be patient-centered and developed and tested in collaboration with the target population. In conclusion, through providing a rich account of these health literacy processes among this Hispanic migrant population, researchers and healthcare providers can be better informed of potential gaps and leverage points that could guide future interventions, with the ultimate goal of impacting the way women understand an abnormal Pap and decreasing cervical cancer health disparities among this population.
Acknowledgements
The research team acknowledges Catholic Mobile Medical Services at the San Jose Mission for all of the collaboration and support. In addition, the research team is thankful to Ms Gloria Arroyo, Patient Navigator at San Diego State University, for her assistance providing study information to participants and for the valuable feedback on instrument guide drafts. Finally, the research team is externally grateful to the women who shared their personal experiences and stories.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by the Tampa Bay Community Cancer Network (TBCCN) training core, a National Cancer Institute’s Center to Reduce Cancer Health Disparities Community Network Program Center (5U54CA153509). Funding for the patient navigator effort was provided by a grant from the National Cancer Institute and the Office of Research in Women’s Health (R21CA167418).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Bernard HR and Ryan GW (2010) Analyzing Qualitative Data: Systematic Approaches. Thousand Oaks, CA: SAGE. [Google Scholar]
- Breitkopf CR, Pearson HC and Breitkopf DM (2005) Poor knowledge regarding the Pap test among low-income women undergoing routine screening. Perspectives on Sexual and Reproductive Health 37(2): 78–84. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2015) Making sense of your Pap & HPV test results. Available at: http://www.cdc.gov/std/hpv/pap/default.htm#sec4 (accessed 20 May 2016).
- Daley EM, Perrin KM, McDermott RJ, et al. (2010) The psychosocial burden of HPV: A mixed-method study of knowledge, attitudes and behaviors among HPV+ women. Journal of Health Psychology 15(2): 279–290. [DOI] [PubMed] [Google Scholar]
- Daley EM, Vamos CA, Wheldon CW, et al. (2015) Negative emotions and stigma associated with a human papillomavirus test result: A comparison between human papillomavirus–positive men and women. Journal of Health Psychology 20(8): 1073–1082. [DOI] [PubMed] [Google Scholar]
- Del Carmen MG, Findley M, Muzikansky A, et al. (2007) Demographic, risk factor, and knowledge differences between Latinas and non-Latinas referred to colposcopy. Gynecologic Oncology 104(1): 70–76. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Berkman ND, Sheridan S, et al. (2004) Literacy and health outcomes. Journal of General Internal Medicine 19(12): 1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggleston KS, Coker AL, Das IP, et al. (2007) Understanding barriers for adherence to follow-up care for abnormal pap tests. Journal of Women’s Health 16(3): 311–330. [DOI] [PubMed] [Google Scholar]
- Garbers S and Chiasson MA (2004) Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Preventing Chronic Disease 1(4): A07. [PMC free article] [PubMed] [Google Scholar]
- Guest G, MacQueen KM and Namey EE (2011) Applied Thematic Analysis. Thousand Oaks, CA: SAGE. [Google Scholar]
- House JS (1981) Work Stress and Social Support. Reading, MA: Addison-Wesley. [Google Scholar]
- Institute of Medicine (2004) Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Institute of Medicine (2009) Measures of Health Literacy: Workshop Summary. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Jordan JE, Buchbinder R and Osborne RH (2010) Conceptualising health literacy from the patient perspective. Patient Education and Counseling 79(1): 36–42. [DOI] [PubMed] [Google Scholar]
- Lindau ST, Tomori C, Lyons T, et al. (2002) The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. American Journal of Obstetrics and Gynecology 186(5): 938–943. [DOI] [PubMed] [Google Scholar]
- McAlister AL, Perry CL and Parcel GS (2008) How individuals, environments, and health behaviors interact: Social cognitive theory In: Glanz K, Rimer BK and Viswanath K (eds) Health Behavior and Health Education: Theory, Research, and Practice (4th edn). San Francisco, CA: John Wiley & Sons, pp. 169–188. [Google Scholar]
- Mills PK, Beaumont JJ and Nasseri K (2006) Proportionate mortality among current and former members of the United Farm Workers of America, AFL-CIO, in California 1973–2000. Journal of Agromedicine 11(1): 39–48. [DOI] [PubMed] [Google Scholar]
- Mills PK, Dodge J and Yang R (2009) Cancer in migrant and seasonal hired farm workers. Journal of Agromedicine 14(2): 185–191. [DOI] [PubMed] [Google Scholar]
- Monsonego J, Cortes J, da Silva DP, et al. (2011) Psychological impact, support and information needs for women with an abnormal Pap smear: Comparative results of a questionnaire in three European countries. BMC Women’s Health 11: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute (n.d.-a) SEER stat fact sheets: Cervix uteri. Available at: http://seer.cancer.gov/statfacts/html/cervix.html (accessed 5 February 2013).
- National Cancer Institute (n.d.-b) SEER stat fact sheets: Cervix uteri Cancer. Available at: http://seer.cancer.gov/statfacts/html/cervix.html (accessed 1 February 2016).
- Newton DC and McCabe MP (2008) Sexually transmitted infections: Impact on individuals and their relationships. Journal of Health Psychology 13(7): 864–869. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, Wilson EA and McCormack L (2010) The evolving field of health literacy research. Journal of Health Communication 15(Suppl. 2): 5–8. [DOI] [PubMed] [Google Scholar]
- Patton MQ (2002) Qualitative Evaluation and Research Methods (6th edn). Thousand Oaks, CA: SAGE. [Google Scholar]
- Percac-Lima S, Aldrich LS, Gamba GB, et al. (2010) Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. Journal of General Internal Medicine 25(11): 1198–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleasant A, McKinney J and Rikard RV (2011) Health literacy measurement: A proposed research agenda. Journal of Health Communication 16(Suppl. 3): 11–21. [DOI] [PubMed] [Google Scholar]
- Sandelowski M (1995) Sample size in qualitative research. Research in Nursing & Health 18(2): 179–183. [DOI] [PubMed] [Google Scholar]
- Scarinci IC, Beech BM, Kovach KW, et al. (2003) An examination of sociocultural factors associated with cervical cancer screening among low-income Latina immigrants of reproductive age. Journal of Immigrant Health 5(3): 119–128. [DOI] [PubMed] [Google Scholar]
- Simon MA, Cofta-Woerpel L, Randhawa V, et al. (2010) Using the word “cancer” in communication about an abnormal Pap test: Finding common ground with patient-provider communication. Patient Education and Counseling 81(1): 106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen K, Van den Broucke S, Fullam J, et al. (2012) Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 12(1): 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorburn S, Keon KL and Kue J (2013) Sources of breast and cervical cancer information for Hmong women and men. Women & Health 53(5): 468–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu Y-C and Wang H-H (2013) An exploration of human papillomavirus-related cervical cancer prevention experiences among college women: A descriptive qualitative approach. Journal of Clinical Nursing 22(23–24): 3300–3309. [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force (2012) Final recommendation statement: Cervical cancer: Screening, October 2014. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/cervical-cancer-screening (accessed 29 December 2014).
- Weiss BD, American Medical Association Foundation and American Medical Association (2007) Health Literacy and Patient Safety: Help Patients Understand (2nd edn). Available at: http://med.fsu.edu/userFiles/file/ahec_health_clinicians_manual.pdf (accessed 23 July 2015).


