Abstract
Introduction:
Calcific tendinopathy of the pectoralis major at its humeral insertion is extremely rare. Few cases have been reported in the literature. We reported a unique case of calcification of the pectoralis major insertion site and conducted a review of the existing literature to propose standardized management.
Case Presentation:
We reported a case of a 63-year-old lady, right-handed, non-smoker, homemaker without any history of trauma or symptoms suggestive of para-neoplasia syndrome. For 1 month, the patient presented severe, disabling pain of the left shoulder which occurred spontaneously, usually in the morning and after effort. The patient had painful passive terminal adduction and internal rotation. There was no neurovascular deficiency. Magnetic resonance imaging and computed tomography (CT) scan helped diagnose the calcific tendinopathy at the pectoralis major humeral insertion. Non-surgical management was performed, combining physiotherapy and painkillers. Two months’ control, CT scan reported complete calcification resorption. The biologic assessment revealed hyperparathyroidism.
Conclusion:
This rare and atypical localization can mislead the surgeon. A biological assessment to research a systemic etiology is mandatory and standardized. A biopsy is not required, radiological examinations are sufficient. Surgical treatment may be proposed in specific cases to shorten the necessary rehabilitation time.
Keywords: Calcific tendinopathy, humeral, pectoralis major
Learning Point of the Article:
Even if pectoralis major humeral insertion localization for calcific tendinopathy is rare, non-surgical management without biopsy can be done if biological and radiological assessment are done.
Introduction
Calcific tendinopathy is a common disorder secondary to the periarticular deposition of hydroxyapatite crystals. Mainly localized to the shoulder, this pathology affects about 3% of adults [1]. In the rotator cuff, this pathology is well known and treatment is codified in the literature. Other localizations such as hip, elbow, wrist, knee, and neck have been described, with rare incidences [2, 3, 4, 5, 6].
The natural evolution of calcific tendinopathy has been described by Uhthoff in four stages: Pre-calcific, formative, resorptive, and post-calcific [7].
Usually, symptoms consist of pain and focal tenderness associated with radiological calcification.
Cortical erosions, intraosseous calcifications, and bone marrow edema can be observed using computed tomography (CT) and magnetic resonance imaging (MRI). The pseudo-neoplastic appearance of intraosseous edema, perilesional inflammation, and bone destruction as well as atypical localization may lead to misdiagnosis and unnecessary invasive biopsy [4].
Calcific tendinopathy of the pectoralis major at its humeral insertion is extremely rare. Few cases have been reported in the literature [6, 8, 9, 10, 11, 12, 13]. We reported a new case of calcification of the pectoralis major and conducted a review of the existing literature to propose standardized management.
The patient was informed of the publication of this article and we obtained her consent.
Case Report
The authors report a case of a 63-year-old woman, righthande non-smoker, homemaker leading a sedentary lifestyle The comorbidities present were dyslipidemia, blood hypertension, hypothyroidism, and obesity (body mass index=33). For 1 month, the patient presented severe, disabling pain of the left shoulder which occurred spontaneously, usually in the morning and after effort. The pain was localized regarding the calcification with irradiation in the lateral side of the arm. There was no history of trauma or symptoms suggestive of paraneoplasia syndrome. Active and passive shoulder range of motion was not restricted. However, the patient had painful passive terminal adduction and internal rotation. The palpation of the calcification zone was painful. There was no neurovascular deficiency
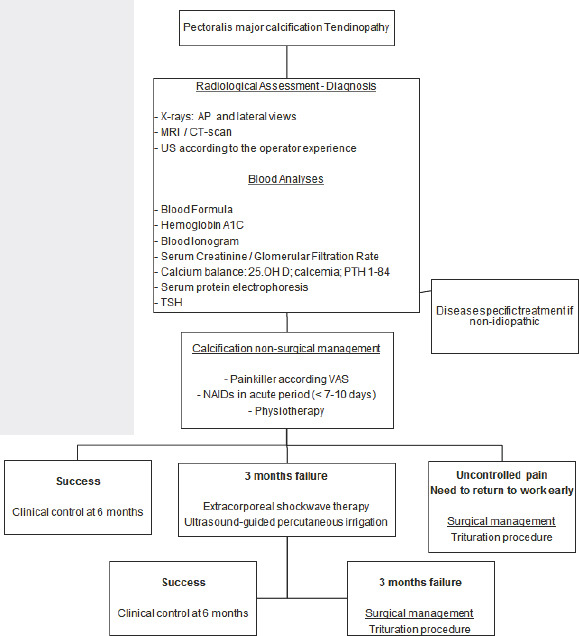
Radiological exploration revealed calcification of the humeral insertion of the pectoralis major. MRI and CT scans helped diagnose the calcific tendinopathy and revealed cortical erosion adjacent to the soft-tissue calcification (Fig. 1a and b).
Figure 1.
(a and b) Coronal and axial computed tomography scan views of the pectoralis major calcific tendinitis.
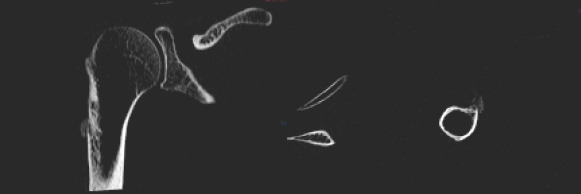
The calcification measured 4.2 cm in its longest axis with two radiological aspects common to calcifications: Comet tail sign and flame appearance (Fig. 2a and b).
Figure 2.
(a and b) Three-dimensional reconstruction of the calcification
A complete blood analyses was performed to research an organic etiology of this calcific tendinopathy. There was no inflammatory syndrome, but it revealed hyperparathyroidism.
Non-surgical management was performed with a combination of physiotherapy and painkillers.
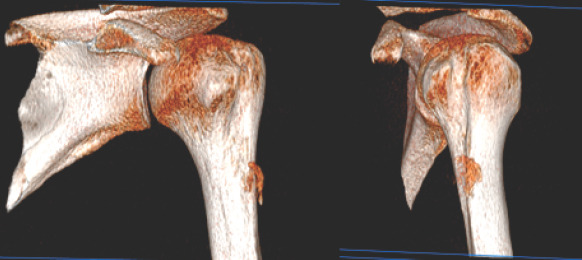
A follow-up CT scan was performed 2 months after the beginning of symptoms. Complete resorption of calcification was observed (Fig. 3a and b). Cortical erosion had disappeared, without sequelae (Fig. 4a and b).
Figure 3.
(a and b) Two months’ follow-up computed tomography scan views: Complete resolution, no calcification, and no bone erosion.
Figure 4.
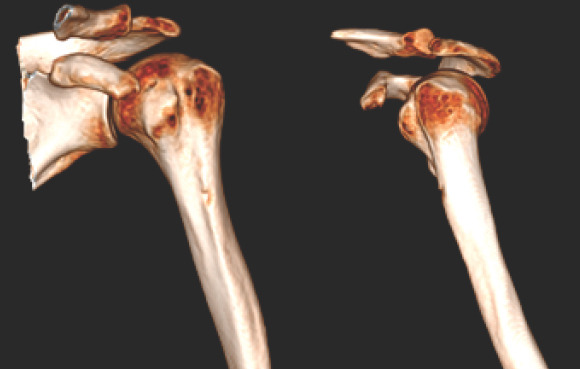
(a and b) Two months’ follow-up three-dimensional reconstruction.
On clinical examination, the patient was completely painless with complete active and passive shoulder range of motion. Forced adduction and internal rotation were painless. Palpation revealed no painful areas.
Hyperparathyroidism management was done in coordination with an endocrinologist.
At 1 year, there was no recurrence, shoulder mobility was complete and painless. Radiological control was without abnormality.
Discussion
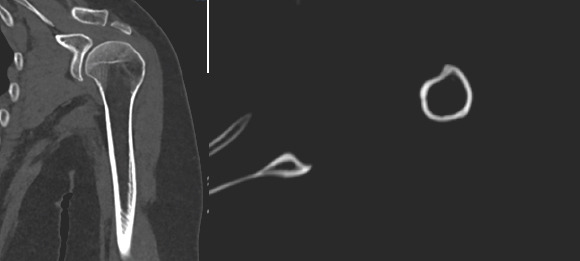
This new rare and atypical case of calcific tendinopathy at the humeral insertion of the pectoralis major completes the small series of cases reported in the literature by proposing a standardized management (flow chart).
Clinical presentation of these calcific tendinopathies is similar and generally acute. Pathology mainly affects women. The pain is localized toward the calcification without any history of trauma. Surgeons can observe a sensitive area due to the inflammatory reaction around the calcification. However, this sign is inconsistent and its absence should not eliminate a calcific pathology. The range of motion is limited in internal rotation and adduction. Although not found in cases of pectoral calcification, Hong et al. [14] described cases associating fever and an increased number of white cells.
Origin of these calcifications is still today a matter of research.
Different theories have been exposed to explain the supraspinatus calcification phenomena, most frequent localization. One of them is that the calcific tendonitis is a degenerative process with necrosis of tendon fibers with accompanying inflammation within the tendon [15]. However, this theory is compromised when we consider the average age of calcification cases, which is 55 years old. [8, 9, 10, 11, 12, 13]. Another theory presented by Uhthoff et al. [7] would be related to a hypovascularized critical area 1 cm from the tendon insertion. The poor oxygenation of this part of the tendon can trigger the transformation of the tendon into fibrocartilage leading to the deposition of calcium. According to the same author, there is a significant correlation between the paroxysm of pain and the phase of calcium resorption. The tendon recovers normal architecture after the calcification disappearance.
High-performance radiological examinations such as CT scan and MRI allow an accurate analysis of the lesions. Erroneous diagnosis of neoplasm or infectious osteitis can be making due to extensive associated edema. Cortical erosion is not considered benign in the literature and not associated with wellknown calcification localizations [1, 16]. However, in our case, cortical erosion is the natural evolution of humeral calcification. Thus, it should not lead to an invasive biopsy and rather suggests a benign pathology. Besides, signs such as comet tail or flame appearance of the calcification are indicative of the pathology. For Hayes et al. [6], the woven bone, that can be observed on the CT scan, represents a repair phenomenon that results from bone involvement and that it should not suggest any alternative diagnosis. A differential radiological diagnosis must be evoked, the traumatic avulsion of the bony insertion of the pectoralis major tendon. Findings that suggest calcific tendinitis over neoplasm include characteristic location and the lack of a softtissue mass. Parsonage-Turner syndrome MRI reports denervation changes in muscles, in contrast to our case where the muscle is healthy. Clinical context is different and concerns rather high-level sportsmen and women [17].
Recently, Cholet [9] introduced the use of ultrasound in the characterization of these calcifications. The ultrasound aspect was similar in all four cases: Linear, sat preferentially in the interstitial and deep tendinous fibers, and was parallel to the tendon major axis. Bone erosions were small (<2 cm), oval shaped, located in the subcortical region, contained calcific fragments, and were associated with reactional peripheral hyperostosis. This simple and low-cost tool remains operator dependent, but according to the author, it allows, based on these criteria, to make a diagnosis without CT scan, or MRI or biopsy.
Three cases in the literature have been biopsied [6, 13]. The result was similar and revealed fibrocartilaginous metaplasia. This supports the idea that the radioclinical diagnosis can be done without a biopsy. However, as soon as the clinical context is evocative of malign or infectious disease (alteration of the general state and concomitant malign systemic pathology), we believe that biopsy is necessary. Care should be taken that chondral metaplasia in the setting of tendon calcification will be not misinterpreted as a chondral neoplasm.
The evolution of the case presented in this article is in agreement with the literature showing a spontaneous resolution between 6 and 10 weeks. Only Cholet [9] presented a case of chronic calcification that required a year to achieve complete resorption. Severe acute pain can be controlled by analgesics associated with appropriate physiotherapy. In this case, we use Non-steroidal anti-inflammatory drugs in the acute period (< 7–10 days). Pain reduction is the primary objective. There are no guidelines about medications in case of this specific localization. Cimetidine was used by Yokoyama et al. [18] to reduce symptoms. The mechanism is unclear, but the authors used the rationale of serum calcium reduction in patients with hyperparathyroidism treated with a histamine blocker. In our practice, we prefer to begin with non-operative management. Bechay et al. [19] analyzed recent literature evaluating the clinical outcomes of non-operative and operative treatment for calcific tendinopathy of the shoulder. Conser vative management (analgesics associated with physiotherapy) is very effective for most patients and should be the first line of treatment. Sansone et al. [20], in his literature review about calcific tendinopathy of the shoulder, detailed the current concepts. We apply the physiotherapy protocol described by Abate et al. [21], in 5 weeks. In the 1st week, stretching, pendulum and isometric exercises, and self-assisted exercises in the pain-free range of motion were started. In the 2nd week, physiotherapist started active exercises to increase the range of motion (especially in internal rotation and adduction in our case). The kinematics of the scapulothoracic joint was also addressed. In the 3rd week, strengthening and endurance exercises, using both elastic bands and weights, were started. Strength, resistance, and power were gradually increased in the past 2 weeks. These exercises are adapted to each patient according to the physical capacities and pain. Corticosteroid injection can also be used in the acute phase, if the patient has inflammatory symptoms, but this treatment is debated because it could have no effect or even a negative effect interrupting calcium deposits’ reabsorption [22]. Plasma-rich platelet (PRP) therapy is still debated in the literature. Different PRP compositions and preparations exist in the market. Its use is more frequent in gluteus muscle tendinopathies. Concerning the shoulder, Seijas et al. [23] reported its use in a case with good results at medium term. In patients who fail to respond to conservative management, extracorporeal shockwave therapy and ultrasound-guided percutaneous irrigation are often effective and should be the next step in treatment. Definition of failure of non-operative therapy is persistent symptoms for at least 6 months, including 3 months of standardized nonoperative treatments. Although surgical treatment by trituration is a consensual option in the treatment of supraspinatus calcifications, we believe that it is important to mention it in this type of calcification. Surgery should be reserved for patients who have failed these other modalities of treatment. Thus, when necessary, that is, uncontrolled pain or the need to return to work early, surgical options by trituration can be proposed to the patient.
This calcific tendinitis of the pectoralis major may be similar to the calcific tendinitis of the gluteus maximus, which is well described in the literature [2]. The anatomical formations of muscles and tendons are similar, as are their functions. Concerning the gluteus maximus, the calcification location is anterior on linea aspera corresponding to its femoral insertion. Concerning the pectoralis major, the location reported in rare cases is at the level of its diaphyseal-metaphyseal humeral insertion. There is a clinical parallelism, the calcific tendinitis of the gluteus maximus corresponds to a misleading, radiating pain in the gluteal region. Thus, although localization in the pectoralis major is rare, we believe that its parallelism to the gluteus maximus can help us in understanding, etiological diagnosis and treatment.
Finally, it is important to note that in this reported case, calcification was the first symptom of a systemic pathology. We have not found other cases in the literature of systemic pathology and specifically of hyperparathyroidism diagnosed by this type of calcification. The authors of the different cases reported in the literature, concerning calcification of the pectoralis major, do not perform a biological assessment except for the investigation of an inflammatory syndrome.
However, there are multiple systemic pathologies causing calcifications such as collagen vascular disease, renal osteodystrophy, hypervitaminosis D, milk-alkali syndrome, and sarcoidosis, but we did not find any case of calcification of the pectoralis major.
Thus, we believe that the management of this type of pathology must systematically be done in collaboration with a specialist physician.
Conclusion
This case completes the series of case reports already present for his atypical location. Analysis of all these cases allows us to provide guidelines in the management of this pathology. A biological assessment to research a systemic etiology is mandatory and standardized. Surgeons can dispense with invasive examinations such as a biopsy to make the diagnosis and confirm the benign nature of the radiological lesion. Surgical treatment may be proposed in specific cases to shorten the necessary rehabilitation time.
Clinical Message.
Calcific tendinopathy of the pectoralis major at its humeral insertion can mislead the surgeon. A biological assessment to research a systemic etiology is mandatory and standardized. A biopsy is not required, radiological examinations are sufficient. Surgical treatment may be proposed in specific cases to shorten the necessary rehabilitation time.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ. Osseous involvement in calcific tendinitis: A retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181:965–72. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]
- 2.Hottat N, Fumière E, Delcour C. Calcific tendinitis of the gluteus maximus tendon: CT findings. Eur Radiol. 1999;9:1104–6. doi: 10.1007/s003300050799. [DOI] [PubMed] [Google Scholar]
- 3.Berney JW. Calcifying peritendinitis of the gluteus maximus tendon. Radiology. 1972;102:517–8. doi: 10.1148/102.3.517. [DOI] [PubMed] [Google Scholar]
- 4.Hodge JC, Schneider R, Freiberger RH, Magid SK. Calcific tendinitis in the proximal thigh. Arthritis Rheum. 1993;36:1476–82. doi: 10.1002/art.1780361021. [DOI] [PubMed] [Google Scholar]
- 5.Newmark H, Forrester DM, Brown JC, Robinson A, Olken SM, Bledsoe R. Calcific Tendinitis of the Neck. Radiology. 1978;128:355–8. doi: 10.1148/128.2.355. [DOI] [PubMed] [Google Scholar]
- 6.Hayes CW, Rosenthal DI, Plata MJ, Hudson TM. Calcific tendinitis in unusual sites associated with cortical bone erosion. AJR Am J Roentgenol. 1987;149:967–70. doi: 10.2214/ajr.149.5.967. [DOI] [PubMed] [Google Scholar]
- 7.Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: A new concept of its pathogenesis. Clin Orthop Relat Res. 1976;118:164–8. [PubMed] [Google Scholar]
- 8.Morán Blanco LM, González Leyte M. Calcifying tendinosis of the pectoralis major muscle with intraosseous migration. Radiologia. 2011;53:364–7. doi: 10.1016/j.rx.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Cholet C, Guerini H, Pessis E, Drapé JL, Campagna R. Ultrasound features of painful intraosseous migration of pectoralis major tendinous calcifications with follow-up. J Ultrasound. 2019;23:411–7. doi: 10.1007/s40477-019-00395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cahir J, Saifuddin A. Calcific tendonitis of pectoralis major: CT and MRI findings. Skeletal Radiol. 2005;34:234–8. doi: 10.1007/s00256-004-0842-2. [DOI] [PubMed] [Google Scholar]
- 11.Ikegawa S. Calcific tendinitis of the pectoralis major insertion. A report of two cases. Arch Orthop Trauma Surg. 1996;115:118–9. doi: 10.1007/BF00573455. [DOI] [PubMed] [Google Scholar]
- 12.Kraemer EJ, El-Khoury GY. Atypical calcific tendinitis with cortical erosions. Skeletal Radiol. 2000;29:690–6. doi: 10.1007/s002560000278. [DOI] [PubMed] [Google Scholar]
- 13.Dürr HR, Lienemann A, Silbernagl H, Nerlich A, Refior HJ. Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion. Eur Radiol. 1997;7:1215–7. doi: 10.1007/s003300050277. [DOI] [PubMed] [Google Scholar]
- 14.Hong MJ, Kim YD, Park JK, Kang TU. Successful treatment of rectus femoris calcification with ultrasound-guided injection:A case report. Korean J Pain. 2015;28:52–6. doi: 10.3344/kjp.2015.28.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peterson RR. Prevention!A new approach to tendinitis. Occup Health Nurs. 1979;27:19–23. doi: 10.1177/216507997902700503. [DOI] [PubMed] [Google Scholar]
- 16.Hendrix RW, Rogers LF, Davis TM. Cortical bone metastases. Radiology. 1991;181:409–13. doi: 10.1148/radiology.181.2.1924781. [DOI] [PubMed] [Google Scholar]
- 17.Connell DA, Potter HG, Sherman MF, Wickiewicz TL. Injuries of the pectoralis major muscle: Evaluation with MR imaging. Radiology. 1999;210:785–91. doi: 10.1148/radiology.210.3.r99fe43785. [DOI] [PubMed] [Google Scholar]
- 18.Yokoyama M, Aono H, Takeda A, Morita K. Cimetidine for chronic calcifying tendinitis of the shoulder. Reg Anesth Pain Med. 2003;28:248–52. doi: 10.1053/rapm.2003.50048. [DOI] [PubMed] [Google Scholar]
- 19.Bechay J, Lawrence C, Namdari S. Calcific tendinopathy of the rotator cuff: A review of operative versus nonoperative management. Phys Sportsmed. 2020;Volume 1:1–6. doi: 10.1080/00913847.2019.1710617. [DOI] [PubMed] [Google Scholar]
- 20.Sansone V, Maiorano E, Galluzzo A, Pascale V. Calcific tendinopathy of the shoulder: Clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev. 2018;10:63–72. doi: 10.2147/ORR.S138225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abate M, Schiavone C, Salini V. Usefulness of rehabilitation in patients with rotator cuff calcific tendinopathy after ultrasound-guided percutaneous treatment. Med Princ Pract. 2015;24:23–9. doi: 10.1159/000366422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malahias MA, Chronopoulos E, Raoulis V, Vergados N, Kaseta MK, Nikolaou VS. Questioning the therapeutic value of corticosteroid bursal injection after ultrasoundguided irrigation and lavage for the treatment of shoulder calcific tendinosis. J Orthop. 2020;18:16–22. doi: 10.1016/j.jor.2019.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seijas R, Ares O, Alvarez P, Cusco X, Garcia-Balletbo M, Cugat R. Platelet-rich plasma for calcific tendinitis of the shoulder:A case report. J Orthop Surg (Hong Kong) 2012;20:126–30. doi: 10.1177/230949901202000128. [DOI] [PubMed] [Google Scholar]


