Summary
Inducible expression of PAX7 in differentiating pluripotent stem cells (PSCs) allows massively scalable generation of human myogenic progenitors, which upon transplantation into dystrophic muscles give rise to donor-derived myofibers and satellite cells. Therefore, PSC-derived PAX7+ myogenic progenitors represent an attractive therapeutic approach to promote muscle regeneration. Work to date has used lentiviral vectors (LVs) that randomly integrate inducible PAX7 transgenes. Here, we investigated whether equivalent induction of the myogenic program could be achieved by targeting the PAX7 transgene into genomic safe harbor (GSH) sites. Across multiple PSC lines, we find that this approach consistently generates expandable myogenic progenitors in vitro, although scalability of expansion is moderately reduced compared with the LV approach. Importantly, transplantation of GSH-targeted myogenic progenitors produces robust engraftment, comparable with LV counterparts. These findings provide proof of concept for the use of GSH targeting as a potential alternative approach to generate therapeutic PSC-derived myogenic progenitors for clinical applications.
Keywords: genomic safe harbor sites, lentivirus, pluripotent stem cells, myogenic progenitors, PAX7, transplantation, muscle regeneration, cell therapy, muscular dystrophies
Highlights
-
•
GSH targeting enables the generation of proliferating PAX7+ myogenic progenitors
-
•
GSH PAX7+ myogenic progenitors proliferate less than LV counterparts
-
•
Efficient myotube formation by GSH PAX7+ myogenic progenitors
-
•
GSH PAX7+ myogenic progenitors display similar engraftment to LV counterparts
In this report, Perlingeiro and colleagues show that the dual genomic safe harbor (GSH) targeting approach allows for the generation of large numbers of PAX7+ myogenic progenitors from human pluripotent stem cells. Upon transplantation, GSH-generated PAX7+ myogenic progenitors give rise to donor-derived myofibers and satellite cells, similarly to LV counterparts.
Introduction
Muscular dystrophies (MDs) encompass more than 40 different genetic disorders characterized by progressive skeletal muscle degeneration and weakness, which in severe disorders result in paralysis and death (Emery, 2002). Despite significant progress in understanding disease pathogenesis and in developing therapeutic strategies, there is still no cure for MDs.
Much current effort is focused on the development of adeno-associated virus (AAV)-mediated gene therapy approaches, which have advanced to the clinical trial stage for the treatment of Duchenne MD (Bowles et al., 2012; Mendell et al., 2010), among a few others (Crudele and Chamberlain, 2019). However, safety and efficacy remain major issues (Goswami et al., 2019). One significant challenge is the immune response against the AAV vector, allowing only a single-dose delivery, which may not be sufficient to provide long-term therapeutic benefit.
Another potential therapeutic strategy consists of replacing diseased muscle by transplanting healthy muscle stem cells. Major caveats here include the accessibility to sufficient number of stem cells from a given donor without damaging the muscle, and the reduction of engraftment potential following their ex vivo expansion (Mendell et al., 1995; Montarras et al., 2005). An alternative approach is to utilize human pluripotent stem cells (hPSCs) to generate transplantable muscle stem cells. PSCs are appealing for therapeutic application as they can repeatedly produce large amounts of differentiated tissue, providing an unlimited source of cells for therapy. However, a critical aspect for translation is their controlled lineage-specific differentiation, since transplantation of contaminating undifferentiated PSCs can lead to tissue abnormalities or even give rise to teratomas. There are several strategies for the derivation of myogenic cells from PSCs, which include the use of PAX7 or MYOD transgene overexpression (Albini et al., 2013; Darabi et al., 2012; Goudenege et al., 2012; Tedesco et al., 2012; Young et al., 2016) and transgene-free methods (Barberi et al., 2007; Chal et al., 2016; Shelton et al., 2014; Xi et al., 2017). Each strategy has unique advantages and disadvantages. Transgene-free methods are attractive, since these do not involve genetic manipulation; however, there are significant limitations in generating large numbers of therapeutically relevant myogenic cells. Moreover, these cultures possess a higher probability of carrying non-myogenic cells, including undifferentiated PSCs (Kim et al., 2017a), an issue that can be minimized by the use of efficient purification protocols (Hicks et al., 2018; Wu et al., 2018). Overexpression of transcription factors associated with the myogenic hierarchy assures the muscle identity of in vitro generated cells. In the case of PAX7, we have documented the generation of large numbers of early myogenic progenitors that upon transplantation into dystrophic mice results in myofiber and satellite cell engraftment (Darabi et al., 2012), suggesting potential for future therapeutic application.
Because lentiviral vectors (LVs) deliver transgenes through random integration, they convey some risk of insertional mutagenesis. To bypass this, we previously investigated the use of the integration-free minicircle vector to generate PSC-derived PAX7+ myogenic progenitors (Kim et al., 2017b). Although the minicircle strategy showed efficient in vitro differentiation of hPSCs into myotubes, due to the transient nature of the minicircle vector, multiple transfections were required to maintain PAX7 expression. Furthermore, this inefficiency in maintaining high levels of PAX7 expression resulted in heterogeneous cultures, which failed to contribute to muscle engraftment (Kim et al., 2017b).
Targeted integration of a PAX7 transgene into a genomic safe harbor (GSH) locus, such as the AAVS1, represents an attractive alternative approach. This locus is widely recognized as a potential ideal site for transgene insertion for gene therapy applications (Papapetrou and Schambach, 2016; Smith et al., 2008). Dual GSH targeting, an improved inducible GSH system that utilizes two different GSH loci, has been recently developed (Pawlowski et al., 2017). Advantages of this system include bypassing the promoter interference of two transgenes (Baron and Bujard, 2000) and providing the flexibility of transgene design as a result of targeting two different GSH loci.
Here, we used the dual GSH targeting approach to generate a highly expandable population of PAX7+ myogenic progenitors from hPSCs that upon transplantation contribute to in vivo muscle regeneration. These findings demonstrate the feasibility for the potential future use of transgene targeting into GSH loci as an approach for generating therapeutic hPSC-derived PAX7+ myogenic progenitors.
Results
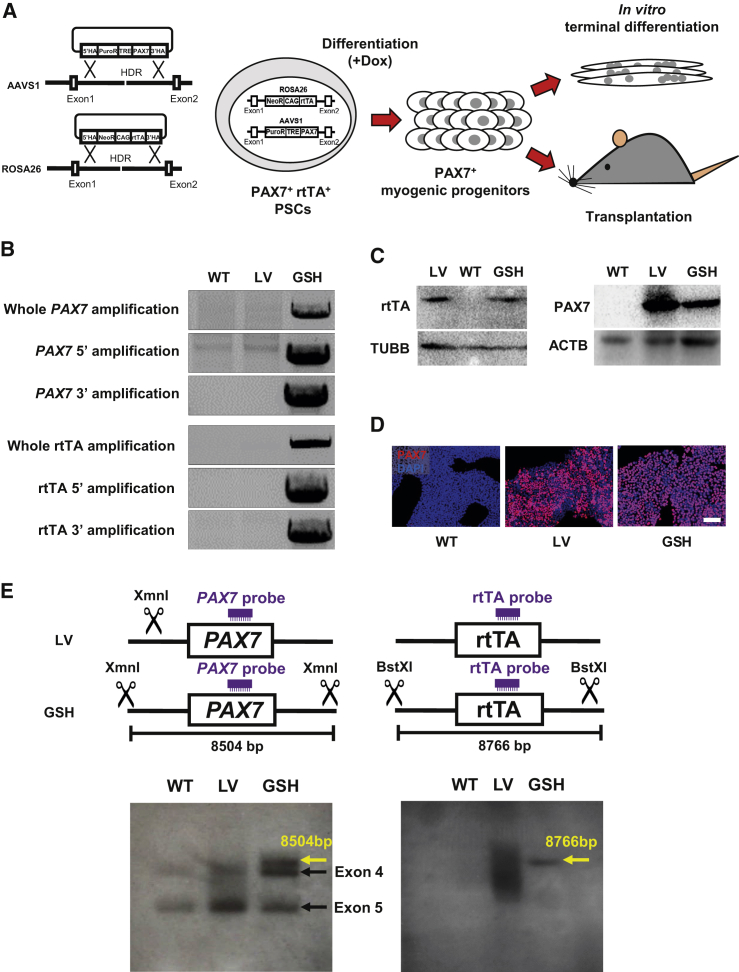
Targeting of PAX7 and rtTA Transgenes into GSH Sites
As outlined in Figure 1A, we inserted the doxycycline (dox)-inducible PAX7 transgene into the AAVS1 locus and the rtTA (tetracycline-responsive transcriptional activator) transgene into the ROSA26 locus using the dual GSH targeting approach (Pawlowski et al., 2017). We confirmed integration of PAX7 and rtTA transgenes into respective GSH loci by knockin-specific PCR (Figures 1B and S1A) and sequencing (Figure S1B). We confirmed protein expression of both PAX7 and rtTA by western blot and immunofluorescence staining following 1 day of dox treatment (Figures 1C, 1D, and S1C). LV hPSC counterparts for each respective line served as positive controls. We confirmed that the integration of PAX7 and rtTA into both GSH sites did not affect the karyotype of genome engineered PSCs (Figure S1D). Next, we performed Southern blots to verify targeted integration. Our results show specific integration of rtTA and PAX7 transgenes at the ROSA26 and AAVS1 loci, respectively (yellow arrow), while this was not the case for the LV approach (Figure 1E). Since the PAX7 probe can hybridize into endogenous exons 4 and 5, two probed bands are detected for PAX7 in all samples (black arrows, Figure 1E).
Figure 1.
Generation of PAX7-Induced PSCs by GSH Loci Targeting
(A) Schematic representation of performed studies.
(B) PCR shows integration analysis of PAX7 and rtTA transgenes into the AAVS1 and ROSA26 loci. Primers were designed outside of the 5′ and 3′ homology arms and within the transgenes. WT, wild-type parental induced pluripotent stem cell (iPSC); LV, lentivirus transduced iPSC; GSH, genomic safe harbor targeted iPSC.
(C) Western blots show PAX7 and rtTA expression. WT and LV iPSCs were used as negative and positive controls, respectively. β-Tubulin (TUBB) and β-actin (ACTB) were used as loading controls.
(D) Immunofluorescence staining shows PAX7 expression (in red) upon 1 day of dox induction. DAPI in blue stains nuclei. WT and LV iPSCs were used as negative and positive controls, respectively. Scale bar, 100 μm.
(E) Southern blot shows integration of PAX7 and rtTA transgenes. PAX7 and rtTA probes and digestion sites of XmnI and BstXI enzymes are indicated in the diagram (upper panel). Yellow arrows indicate specific integration of PAX7 and rtTA transgenes in respective GSHs. Black arrows indicate endogenous PAX7 at exons 4 and 5. WT iPSCs served as negative control.
Generation of GSH Myogenic Progenitors
GSH and LV iPAX7 hPSCs were differentiated into embryoid bodies (EBs), and dox treatment began on day 5, as previously described (Selvaraj et al., 2019b). Day-4 EBs showed similar expression of the early mesodermal marker T (Figure 2A), and no differences were observed for the somitic mesodermal genes FOXC2, PAX3, and TCF15 in day-6 EBs (Figure 2A). We detected lower expression levels of PAX7 and MEOX1 in GSH EBs compared with LVs (Figure 2A). This noticeably reduced expression of PAX7 1 day after the start of dox induction may be due to the lower copy number of the PAX7 transgene in the GSH approach (Figure 2A), which then likely directly affects the expression levels of the PAX7 target, MEOX1. On day 15, PAX7+ myogenic progenitors were purified based on the expression of CD54 and Syndecan2 (SDC2), as described by Magli et al. (2017). We observed no differences in the frequency of CD54+SDC2+ myogenic progenitors between GSH and LV approaches (Figure 2B). Next, we assessed PAX7 expression in expanding myogenic progenitors. qRT-PCR results show that LV myogenic progenitors display higher expression levels of total and exogenous (transgene) PAX7 than GSH myogenic progenitors (Figure 2C). No differences were found in the expression levels of endogenous PAX7, which were low in both LV and GSH myogenic progenitors (Figure 2C), indicating that PAX7 expression in these cells is virtually exclusively from the PAX7 transgene. Comparable PAX7 protein expression was observed in GSH and LV myogenic progenitors by western blot (Figure S2A), fluorescence-activated cell sorting (FACS) (Figures 2D and S2B), and immunofluorescence (Figures 2F and S2C) staining. The only difference noted was the intensity of PAX7 expression in the FACS plots, as evidenced by the geometric mean value, which was found to be higher in LV myogenic progenitors (Figure 2E).
Figure 2.
Characterization of GSH PAX7+ Myogenic Progenitors
(A) Bar graphs show expression analysis of paraxial mesoderm (T) at day 4, and somite (FOXC2, MEOX1, PAX3, and TCF15) genes as well as PAX7 at day 6 of EB differentiation for GSH and LV PAX7-induced iPSCs. Data are shown as mean ± SEM of six independent replicates. ∗p < 0.05, ∗∗∗p < 0.001. ns, not significant.
(B) Representative FACS plots show the frequency of CD54+SDC2+ myogenic progenitors in GSH and LV PAX7-induced iPSC-derived EBs at day 15 of differentiation (left), and respective quantification (right). Data are shown as the mean ± SEM of three independent replicates. ns, not significant.
(C) Bar graphs show expression analysis of total, exogenous, and endogenous PAX7 in LV and GSH myogenic progenitors. Data are shown as mean ± S.E.M. of three independent replicates. ∗p < 0.05, ∗∗p < 0.01. ns, not significant.
(D and E) FACS for PAX7. Bar graphs show the quantification of PAX7 expression (D) and the mean fluorescence intensity (MFI), also known as geometric mean (E) in LV and GSH myogenic progenitors. Data are shown as the mean ± SEM of three independent biological replicates performed in triplicate. ∗p < 0.05. ns, not significant.
(F) Representative images show immunofluorescence staining for PAX7 (red) in GSH and LV CD54+SDC2+ myogenic progenitors (left panels). DAPI (blue) stains nuclei. Scale bar, 100 μm. Right panel shows the ratio of percent PAX7-stained area to percent DAPI area in GSH and LV myogenic progenitors. Data are shown as the mean ± SEM of three independent replicates. ns, not significant.
(G) Growth curves of GSH and LV CD54+SDC2+ myogenic progenitors. Cells were counted every 3 days. Data are shown as the mean ± SEM of three independent biological replicates. ∗p < 0.05. ns, not significant.
(H) Bar graphs show the percentage distribution of LV and GSH myogenic progenitors in different stages of the cell cycle. Data are shown as the mean ± SEM of three independent biological replicates. ∗p < 0.05. ns, not significant.
One of the major characteristics of the LV conditional expression system is the remarkable expansion potential. Therefore, we evaluated whether GSH-generated PAX7+ myogenic progenitors would have comparable expansion capacity compared with LV counterparts. Overall, GSH myogenic progenitors generated from all three PSC lines showed significant expansion potential (Figures 2G and S2D), but the LV-generated myogenic progenitors displayed a clear advantage in scalability, in particular in two of the three PSC lines evaluated (hiPSC-TC1133 and hESC-1). This resulted in greater than an order of magnitude more myogenic progenitor cells at the end of the 3-week expansion period. We then performed cell-cycle analyses by combining bromodeoxyuridine incorporation with propidium iodide staining (Figures 2H and S2E). Our results show that a lower proportion of GSH myogenic progenitors were in S phase compared with LV myogenic progenitors (p < 0.05), whereas the opposite was true for the G1 phase (more of GSH progenitors were in G1 phase), confirming that GSH myogenic progenitors proliferate more slowly than LV myogenic progenitors. This was reflected in the doubling time, as the average ± SEM for LV and GSH myogenic progenitors (all three PSC lines) was 30.8 ± 3.1 and 47.2 ± 1.6 h, respectively. Thus, taken together these results indicate that LV myogenic progenitors were endowed with greater expansion potential than GSH myogenic progenitors due to the attribution of increased proliferation.
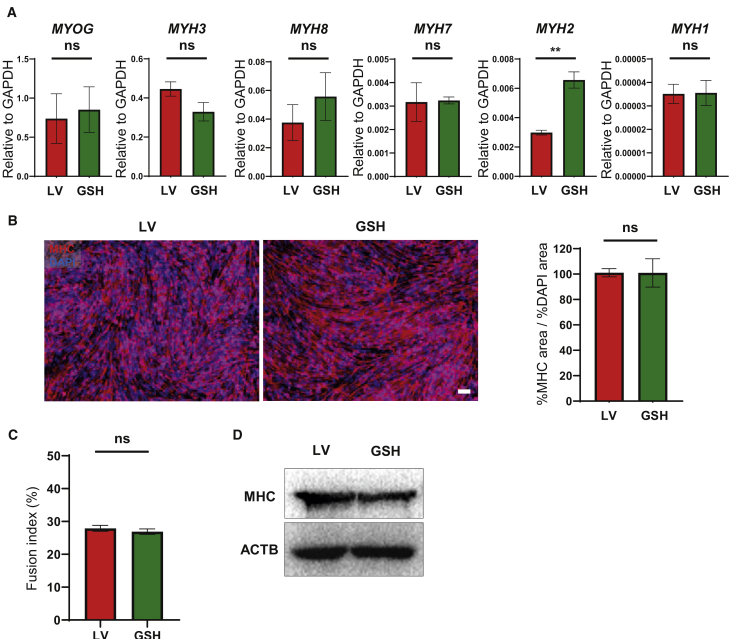
In Vitro Terminal Differentiation of GSH PAX7+ Myogenic Progenitors
Next, we differentiated GSH- and LV-generated myogenic progenitors into myotubes. We observed comparable gene-expression levels for MYOG and several MYH isoforms between the two approaches (Figures 3A and S3A). Quantification of myosin heavy chain (MHC) protein levels revealed no differences between GSH and LV myotubes (Figures 3B, 3D, S3B, and S3D). Moreover, comparable fusion indices were observed (Figures 3C and S3C). These data indicate that GSH-generated myogenic progenitors can efficiently give rise to MHC+ myotubes in vitro.
Figure 3.
Terminal Differentiation of GSH Myogenic Progenitors into Myotubes
(A) Bar graphs show gene expression of MYOGENIN (MYOG) and MYOSIN-HEAVY-CHAIN (MYH) isoforms in GSH and LV iPSC-derived myotubes. Data are shown as the mean ± SEM of six independent replicates. ∗∗p < 0.01. ns, not significant.
(B) Representative images show immunofluorescence staining for MHC (red) in GSH and LV myotubes (left panels). DAPI (blue) stains nuclei. Scale bar, 100 μm. Right panel shows the ratio of percent MHC-stained area to percent DAPI area. Data are shown as the mean ± SEM of three independent replicates. ns, not significant.
(C) Fusion index quantification of LV and GSH myotubes. Data are shown as the mean ± SEM of three independent replicates. ns, not significant.
(D) Western blot for MHC. β-Actin was used as a loading control.
Transplantation of GSH-Generated PAX7+ Myogenic Progenitors
To determine the in vivo regenerative potential of GSH-generated PAX7+ myogenic progenitors, we transplanted these cells into cardiotoxin pre-injured tibialis anterior (TA) muscles of NSG mice. Assessment of injected muscles 2 months later revealed the presence of donor-derived myofibers, as shown by immunofluorescence staining using human DYSTROPHIN and human LAMIN A/C specific antibodies, thus confirming engraftment in recipients transplanted with GSH-generated PAX7+ myogenic progenitors (Figure 4A). No staining was detected in PBS-injected controls (Figure 4A, left). Importantly, quantification of human donor-derived DYSTROPHIN+ fibers showed that GSH- and LV-generated PAX7+ myogenic progenitors have similar engraftment potential (Figure 4B).
Figure 4.
In Vivo Regenerative Potential of GSH Myogenic Progenitors
(A) Representative images show immunofluorescence staining for DYSTROPHIN (DYS, red) and LAMIN A/C (LMNA, green) in TA muscles from NSG mice that had been transplanted with GSH and LV myogenic progenitors. PBS-injected muscles served as negative control (left panel). DAPI stains nuclei (blue). Scale bar, 100 μm.
(B) Graph shows quantification of engraftment (from A) as shown by the number of donor-derived human DYS+ myofibers per section from TA muscles of 26 mice. Error bars represent mean ± SEM. ns, not significant.
(C) Satellite cell engraftment in transplanted muscles. Representative images show immunofluorescence staining for PAX7 (red), LMNA (green), and LAMININ (LM, gray). DAPI in blue stains nuclei. Scale bar, 10 μm.
(D) Percentage of PAX7+/LMNA+ (donor) cells and PAX7+/LMNA− (recipient) cells per muscle section. Data are shown as mean ± SEM (n = 7 mice per group).
(E) Myofiber engraftment in dystrophic mouse models. Representative images show immunofluorescence staining for DYS (red) and LMNA (green) in transplanted TA muscles from NSG-mdx4cv (upper panels) and NSG-C3KO (lower panels) mice. DAPI stains nuclei. Scale bar, 100 μm.
(F) Bar graph shows quantification of engraftment as measured by the maximum number of donor-derived human DYS+ myofibers per section from TA muscles of NSG-mdx4cv (n = 5 mice per group) and NSG-C3KO (n = 8 mice per group). Error bars represent mean ± SEM. ns, not significant.
Since satellite cell engraftment is critical to ensure long-term muscle regeneration, we investigated the ability of transplanted myogenic progenitors to give rise to satellite cells. For this, we stained muscle sections with antibodies to the satellite cell marker PAX7, human LAMIN A/C, and laminin-α2 (LM). Immunofluorescence staining showed that GSH-generated PAX7+ myogenic progenitors were able to seed the satellite cell compartment of transplanted muscles (Figure 4C, lower panel). Quantification revealed approximately 3% human donor contribution to the satellite cell pool, and no differences between the two approaches (Figure 4D). This level of engraftment is in agreement with our previous xenograft studies (Darabi et al., 2012). Of note, much higher numbers of donor-derived satellite cells were detected in our mouse-to-mouse transplantation studies in the presence or absence of pre-conditioning (Azzag et al., 2020; Incitti et al., 2019).
The in vivo engraftment potential of GSH-generated PAX7+ myogenic progenitors was also validated in immunodeficient mouse models of DMD (Arpke et al., 2013) and limb girdle muscular dystrophy type 2A (Selvaraj et al., 2019a). Comparable engraftment for LV and GSH myogenic progenitors (Figures 4E and 4F) was observed in both models, as shown by the presence of donor-derived myofibers expressing human DYSTROPHIN and human LAMIN A/C.
Discussion
Conditional expression of PAX7 allows for the derivation of therapeutically relevant human myogenic progenitors (Darabi et al., 2012; Kim et al., 2017a; Magli et al., 2017; Selvaraj et al., 2019a). However, these studies have used an LV-based approach to deliver the PAX7 transgene, which requires consideration of risks of integrational mutagenesis. On the other hand, GSH sites allow for the insertion of exogenous DNA material with robust expression at specific sites within the host genome, reducing the risk of insertional mutations (Papapetrou and Schambach, 2016).
Several studies have reported the targeting of GSH sites in patient-specific induced PSCs to insert wild-type sequences for the correction of monogenic diseases, including X-linked chronic granulomatous disease and hemophilia B (De Ravin et al., 2016; Lyu et al., 2018; Zou et al., 2011). To date, only Pawlowski et al. (2017) have applied this strategy to induce the in vitro differentiation of hPSCs into specific lineages, but these studies were solely in vitro. Here we report the targeting of GSH sites to generate engraftable hPSC-derived PAX7+ myogenic progenitors, as shown by their ability to contribute to myofibers and satellite cells in vivo, in a manner equivalent to their LV-generated counterparts.
One aspect in which the two approaches differed was the in vitro expansion potential, as GSH myogenic progenitors presented slower proliferation rates than LV-generated myogenic progenitors (doubling time of 47.2 ± 1.6 and 30.8 ± 3.1 h, respectively), which concurred with our cell-cycle assessment. One potential hypothesis for this difference may be the presence of fewer copies of the PAX7 transgene in the GSH compared with the LV approach. Our results show increased PAX7 gene expression (total and exogenous) in LV myogenic progenitors (Figure 2C), but this did not result in significant differences in PAX7 protein expression (Figures 2D, 2F, and S2A–S2C), although we noted higher PAX7 intensity by FACS in LV myogenic progenitors (Figure 2E). Collins et al. (2009) have shown that constitutive expression of PAX7 in satellite cells and C2C12 myoblasts leads to enhanced proliferative rate, and this also applied to fibroblasts upon PAX7 ectopic expression. We have reported similar results in differentiating mouse and human PSCs (Darabi et al., 2011; Kim et al., 2017b). Therefore, these studies suggest a positive correlation between PAX7 expression and proliferation rate. In any case, since GSH-generated myogenic progenitors double approximately every 2 days (47.2 ± 1.6 h), it should be feasible to obtain large numbers of GSH PAX7+ myogenic progenitors for transplantation.
Taken together, our findings demonstrate feasibility for the use of GSH sites as an alternative approach to generate therapeutically relevant PSC-derived PAX7+ myogenic progenitors.
Experimental Procedures
Generation of PAX7+rtTA+ GSH PSC Lines
hROSA26 gRNA/Cas9n and AAVS1 ZFN expression plasmids, as well as pR26_CAG-rtTA and pAAVS1_TRE targeting plasmids, were kindly provided by Dr. Mark Kotter from the University Cambridge, UK (Pawlowski et al., 2017). We used SpeI/EcoRI sites to clone PAX7 (Darabi et al., 2012) into the pAAVS1_TRE targeting plasmid. hROSA26 gRNA/Cas9n expression plasmids and pR26_CAG-rtTA targeting plasmid were delivered to hPSCs by nucleofection (Lonza), as previously described (Pawlowski et al., 2017). The detailed description is provided in Supplemental Experimental Procedures.
hPSC Maintenance and Myogenic Differentiation
PSCs were maintained in mTeSR1 medium (STEMCELL Technologies) on Matrigel-coated plates. Myogenic differentiation was performed as previously described (Selvaraj et al., 2019b). The detailed description is provided in Supplemental Experimental Procedures.
FACS Analysis, Cell Cycle, and Sorting
A detailed description is provided in Supplemental Experimental Procedures.
Transplantation Studies
Animal experiments were carried out according to protocols approved by the University of Minnesota Institutional Animal Care and Use Committee. TA muscles of 6- to 8-week-old NSG (Jackson), and 10- to 12-week-old NSG-mdx4cv and NSG-C3KO mice were pre-injured with cardiotoxin and injected with 1 million myogenic progenitors. The detailed description is provided in Supplemental Experimental Procedures.
qRT-PCR
A detailed description is provided in Supplemental Experimental Procedures.
Immunofluorescence Staining and Western Blot Analysis
A detailed description is provided in Supplemental Experimental Procedures.
Southern Blot Analysis
A detailed description is provided in Supplemental Experimental Procedures.
Statistical Analysis
Differences between the two samples were assessed by using the Student's t test for independent samples. p values lower than 0.05 were considered significant. Statistical analyses were performed using Prism 7 software (GraphPad).
Author Contributions
H.K. designed and performed experiments, analyzed the data, and wrote the manuscript; S.S., J.K., K.A., and B.I.G. performed experiments and analyzed the data; R.C.R.P. contributed to experimental design and interpretation of the data, and wrote the manuscript.
Acknowledgments
We acknowledge the generous support from ADVault and MyDirectives.com (R.C.R.P.). This project was also supported by funds from the NIH, grants R01 AR055299 and AR071439 (R.C.R.P.). We thank Mark Kotter (University of Cambridge, UK) for targeting and expression plasmids. The monoclonal antibody to MHC was obtained from the Developmental Studies Hybridoma Bank developed under the auspices of the NICHD and maintained by the University of Iowa.
Published: December 3, 2020
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.stemcr.2020.11.001.
Supplemental Information
References
- Albini S., Coutinho P., Malecova B., Giordani L., Savchenko A., Forcales S.V., Puri P.L. Epigenetic reprogramming of human embryonic stem cells into skeletal muscle cells and generation of contractile myospheres. Cell Rep. 2013;3:661–670. doi: 10.1016/j.celrep.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpke R.W., Darabi R., Mader T.L., Zhang Y., Toyama A., Lonetree C.L., Nash N., Lowe D.A., Perlingeiro R.C., Kyba M. A new immuno-, dystrophin-deficient model, the NSG-mdx(4Cv) mouse, provides evidence for functional improvement following allogeneic satellite cell transplantation. Stem Cells. 2013;31:1611–1620. doi: 10.1002/stem.1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azzag K., Ortiz-Cordero C., Oliveira N.A.J., Magli A., Selvaraj S., Tungtur S., Upchurch W., Iaizzo P.A., Lu Q.L., Perlingeiro R.C.R. Efficient engraftment of pluripotent stem cell-derived myogenic progenitors in a novel immunodeficient mouse model of limb girdle muscular dystrophy 2I. Skelet. Muscle. 2020;10:10. doi: 10.1186/s13395-020-00228-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barberi T., Bradbury M., Dincer Z., Panagiotakos G., Socci N.D., Studer L. Derivation of engraftable skeletal myoblasts from human embryonic stem cells. Nat. Med. 2007;13:642–648. doi: 10.1038/nm1533. [DOI] [PubMed] [Google Scholar]
- Baron U., Bujard H. Tet repressor-based system for regulated gene expression in eukaryotic cells: principles and advances. Methods Enzymol. 2000;327:401–421. doi: 10.1016/s0076-6879(00)27292-3. [DOI] [PubMed] [Google Scholar]
- Bowles D.E., McPhee S.W., Li C., Gray S.J., Samulski J.J., Camp A.S., Li J., Wang B., Monahan P.E., Rabinowitz J.E. Phase 1 gene therapy for Duchenne muscular dystrophy using a translational optimized AAV vector. Mol. Ther. 2012;20:443–455. doi: 10.1038/mt.2011.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chal J., Al Tanoury Z., Hestin M., Gobert B., Aivio S., Hick A., Cherrier T., Nesmith A.P., Parker K.K., Pourquie O. Generation of human muscle fibers and satellite-like cells from human pluripotent stem cells in vitro. Nat. Protoc. 2016;11:1833–1850. doi: 10.1038/nprot.2016.110. [DOI] [PubMed] [Google Scholar]
- Collins C.A., Gnocchi V.F., White R.B., Boldrin L., Perez-Ruiz A., Relaix F., Morgan J.E., Zammit P.S. Integrated functions of Pax3 and Pax7 in the regulation of proliferation, cell size and myogenic differentiation. PLoS One. 2009;4:e4475. doi: 10.1371/journal.pone.0004475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crudele J.M., Chamberlain J.S. AAV-based gene therapies for the muscular dystrophies. Hum. Mol. Genet. 2019;28:R102–R107. doi: 10.1093/hmg/ddz128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darabi R., Santos F.N., Filareto A., Pan W., Koene R., Rudnicki M.A., Kyba M., Perlingeiro R.C. Assessment of the myogenic stem cell compartment following transplantation of Pax3/Pax7-induced embryonic stem cell-derived progenitors. Stem Cells. 2011;29:777–790. doi: 10.1002/stem.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darabi R., Arpke R.W., Irion S., Dimos J.T., Grskovic M., Kyba M., Perlingeiro R.C. Human ES- and iPS-derived myogenic progenitors restore DYSTROPHIN and improve contractility upon transplantation in dystrophic mice. Cell Stem Cell. 2012;10:610–619. doi: 10.1016/j.stem.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Ravin S.S., Reik A., Liu P.Q., Li L., Wu X., Su L., Raley C., Theobald N., Choi U., Song A.H. Targeted gene addition in human CD34(+) hematopoietic cells for correction of X-linked chronic granulomatous disease. Nat. Biotechnol. 2016;34:424–429. doi: 10.1038/nbt.3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery A.E.H. The muscular dystrophies. Lancet. 2002;359:687–695. doi: 10.1016/S0140-6736(02)07815-7. [DOI] [PubMed] [Google Scholar]
- Goswami R., Subramanian G., Silayeva L., Newkirk I., Doctor D., Chawla K., Chattopadhyay S., Chandra D., Chilukuri N., Betapudi V. Gene therapy leaves a vicious cycle. Front. Oncol. 2019;9:297. doi: 10.3389/fonc.2019.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudenege S., Lebel C., Huot N.B., Dufour C., Fujii I., Gekas J., Rousseau J., Tremblay J.P. Myoblasts derived from normal hESCs and dystrophic hiPSCs efficiently fuse with existing muscle fibers following transplantation. Mol. Ther. 2012;20:2153–2167. doi: 10.1038/mt.2012.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks M.R., Hiserodt J., Paras K., Fujiwara W., Eskin A., Jan M., Xi H., Young C.S., Evseenko D., Nelson S.F. ERBB3 and NGFR mark a distinct skeletal muscle progenitor cell in human development and hPSCs. Nat. Cell Biol. 2018;20:46–57. doi: 10.1038/s41556-017-0010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incitti T., Magli A., Darabi R., Yuan C., Lin K., Arpke R.W., Azzag K., Yamamoto A., Stewart R., Thomson J.A. Pluripotent stem cell-derived myogenic progenitors remodel their molecular signature upon in vivo engraftment. Proc. Natl. Acad. Sci. U S A. 2019;116:4346–4351. doi: 10.1073/pnas.1808303116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Magli A., Chan S.S.K., Oliveira V.K.P., Wu J., Darabi R., Kyba M., Perlingeiro R.C.R. Expansion and purification are critical for the therapeutic application of pluripotent stem cell-derived myogenic progenitors. Stem Cell Reports. 2017;9:12–22. doi: 10.1016/j.stemcr.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Oliveira V.K.P., Yamamoto A., Perlingeiro R.C.R. Generation of skeletal myogenic progenitors from human pluripotent stem cells using non-viral delivery of minicircle DNA. Stem Cell Res. 2017;23:87–94. doi: 10.1016/j.scr.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu C., Shen J., Wang R., Gu H., Zhang J., Xue F., Liu X., Liu W., Fu R., Zhang L. Targeted genome engineering in human induced pluripotent stem cells from patients with hemophilia B using the CRISPR-Cas9 system. Stem Cell Res. Ther. 2018;9:92. doi: 10.1186/s13287-018-0839-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magli A., Incitti T., Kiley J., Swanson S.A., Darabi R., Rinaldi F., Selvaraj S., Yamamoto A., Tolar J., Yuan C. PAX7 targets, CD54, integrin alpha9beta1, and SDC2, allow isolation of human ESC/iPSC-derived myogenic progenitors. Cell Rep. 2017;19:2867–2877. doi: 10.1016/j.celrep.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendell J.R., Kissel J.T., Amato A.A., King W., Signore L., Prior T.W., Sahenk Z., Benson S., McAndrew P.E., Rice R. Myoblast transfer in the treatment of Duchenne's muscular dystrophy. N. Engl. J. Med. 1995;333:832–838. doi: 10.1056/NEJM199509283331303. [DOI] [PubMed] [Google Scholar]
- Mendell J.R., Campbell K., Rodino-Klapac L., Sahenk Z., Shilling C., Lewis S., Bowles D., Gray S., Li C., Galloway G. Dystrophin immunity in Duchenne's muscular dystrophy. N. Engl. J. Med. 2010;363:1429–1437. doi: 10.1056/NEJMoa1000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montarras D., Morgan J., Collins C., Relaix F., Zaffran S., Cumano A., Partridge T., Buckingham M. Direct isolation of satellite cells for skeletal muscle regeneration. Science. 2005;309:2064–2067. doi: 10.1126/science.1114758. [DOI] [PubMed] [Google Scholar]
- Papapetrou E.P., Schambach A. Gene insertion into genomic safe harbors for human gene therapy. Mol. Ther. 2016;24:678–684. doi: 10.1038/mt.2016.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlowski M., Ortmann D., Bertero A., Tavares J.M., Pedersen R.A., Vallier L., Kotter M.R.N. Inducible and deterministic forward programming of human pluripotent stem cells into neurons, skeletal myocytes, and oligodendrocytes. Stem Cell Reports. 2017;8:803–812. doi: 10.1016/j.stemcr.2017.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvaraj S., Dhoke N.R., Kiley J., Mateos-Aierdi A.J., Tungtur S., Mondragon-Gonzalez R., Killeen G., Oliveira V.K.P., Lopez de Munain A., Perlingeiro R.C.R. Gene correction of LGMD2A patient-specific iPSCs for the development of targeted autologous cell therapy. Mol. Ther. 2019;27:2147–2157. doi: 10.1016/j.ymthe.2019.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvaraj S., Mondragon-Gonzalez R., Xu B., Magli A., Kim H., Laine J., Kiley J., McKee H., Rinaldi F., Aho J. Screening identifies small molecules that enhance the maturation of human pluripotent stem cell-derived myotubes. eLife. 2019;8:e47970. doi: 10.7554/eLife.47970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton M., Metz J., Liu J., Carpenedo R.L., Demers S.P., Stanford W.L., Skerjanc I.S. Derivation and expansion of PAX7-positive muscle progenitors from human and mouse embryonic stem cells. Stem Cell Reports. 2014;3:516–529. doi: 10.1016/j.stemcr.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.R., Maguire S., Davis L.A., Alexander M., Yang F., Chandran S., ffrench-Constant C., Pedersen R.A. Robust, persistent transgene expression in human embryonic stem cells is achieved with AAVS1-targeted integration. Stem Cells. 2008;26:496–504. doi: 10.1634/stemcells.2007-0039. [DOI] [PubMed] [Google Scholar]
- Tedesco F.S., Gerli M.F.M., Perani L., Benedetti S., Ungaro F., Cassano M., Antonini S., Tagliafico E., Artusi V., Longa E. Transplantation of genetically corrected human iPSC-derived progenitors in mice with limb-girdle muscular dystrophy. Sci. Transl. Med. 2012;4:140ra189. doi: 10.1126/scitranslmed.3003541. [DOI] [PubMed] [Google Scholar]
- Wu J., Matthias N., Lo J., Ortiz-Vitali J.L., Shieh A.W., Wang S.H., Darabi R. A myogenic double-reporter human pluripotent stem cell line allows prospective isolation of skeletal muscle progenitors. Cell Rep. 2018;25:1966–1981.e4. doi: 10.1016/j.celrep.2018.10.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi H., Fujiwara W., Gonzalez K., Jan M., Liebscher S., Van Handel B., Schenke-Layland K., Pyle A.D. In vivo human somitogenesis guides somite development from hPSCs. Cell Rep. 2017;18:1573–1585. doi: 10.1016/j.celrep.2017.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young C.S., Hicks M.R., Ermolova N.V., Nakano H., Jan M., Younesi S., Karumbayaram S., Kumagai-Cresse C., Wang D., Zack J.A. A single CRISPR-Cas9 deletion strategy that targets the majority of DMD patients restores dystrophin function in hiPSC-derived muscle cells. Cell Stem Cell. 2016;18:533–540. doi: 10.1016/j.stem.2016.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou J., Sweeney C.L., Chou B.K., Choi U., Pan J., Wang H., Dowey S.N., Cheng L., Malech H.L. Oxidase-deficient neutrophils from X-linked chronic granulomatous disease iPS cells: functional correction by zinc finger nuclease-mediated safe harbor targeting. Blood. 2011;117:5561–5572. doi: 10.1182/blood-2010-12-328161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.