Abstract
Objective:
We aimed to determine the potential association between physician gender and academic advancement among US rheumatologists.
Methods:
We performed a nationwide, cross-sectional study of all practicing rheumatologists in the United States in 2014 using a comprehensive database of all licensed physicians. Among academic rheumatologists, we estimated gender differences in faculty rank, adjusting for differences in physician age, years since residency graduation, publications, NIH grants, registered clinical trials, and appointment at a top 20 medical school using a multivariate logistic regression model. We also estimated gender differences in leadership positions (i.e., division director and fellowship program director).
Results:
Among 6,125 total practicing rheumatologists, 941 (15%) had academic faculty appointments in 2014. Women academic rheumatologists (41.6%) were younger and completed residency more recently than men. Women had fewer total publications, first or last author publications, and NIH grants. In fully-adjusted analyses, women were less likely to be full or associate professors than men (aOR 0.78 [95% CI 0.62–0.99]). Women in rheumatology had similar odds as men of being a fellowship program director or division director (aOR 0.90, 95% CI: 0.69–1.43 and aOR 0.96, 95% CI: 0.66–1.41, respectively).
Conclusion:
Among academic rheumatologists, women are less likely than men to be full or associate professors but have similar odds of being fellowship program directors or division directors, when adjusting for several factors known to influence faculty promotion. These differences suggest barriers to academic promotion despite representation in leadership positions within rheumatology divisions.
Keywords: academic rheumatology, women, workforce, policy
INTRODUCTION
The number of women in medicine continues to rise, with current medical school graduating classes comprised of approximately 50% men and women.1,2 In comparison, fifty years ago, the medical school graduating classes and academic faculty were composed of less than 10 percent women.3 Rheumatology has seen a dramatic increase in the number of women in the specialty with the 2015 American College of Rheumatology (ACR) workforce study reporting that women currently represent 41% of the rheumatology workforce and 66% of rheumatology fellows.4,5 Projections suggest that women will comprise the majority of the rheumatology workforce by 2025.4 As a specialty comprised equally of men and women, it is of interest to determine the equity among faculty and leadership positions as well as the opportunity for men and women to achieve professional growth.
It is well documented that a gender gap exists between men and women when comparing academic rank, leadership roles, and remuneration across United States (US) academic medical centers.6–8 In a study of the US academic physician workforce, women were less likely than men to achieve academic ranks of associate or full professor, even after adjusting for age, experience, specialty, and productivity.1 Similar studies in internal medicine have found variation across subspecialties with regard to the likelihood of women achieving faculty promotion. For instance, women in cardiology are less likely to achieve higher academic ranks than men whereas no differences were observed between men and women with regard to faculty rank in allergy/immunology. 9,10 Differences in academic promotion and leadership positions among women and men in rheumatology have not been previously evaluated. Defining these benchmarks are important to facilitate actions that will improve parity in the rheumatology workforce, help maintain women in academic rheumatology, and ensure that the distribution of men and women in academic rheumatology reflects the demographics of the specialty.
Here, we sought to evaluate differences in academic advancement by gender within rheumatology.
MATERIALS AND METHODS
Data Source and Study Population
We obtained comprehensive, cross-sectional information on physicians in the US which was provided by Doximity, a company that provides a free online networking service for physicians. Physicians do not need to register for an account to be included in this database; it includes all physicians with a registered National Provider Identifier (NPI) number as well as physicians without NPI numbers who have self-registered for an account with Doximity. Data captured on US physicians includes age, sex, year of medical school graduation, year of residency graduation, appointment at a US medical school, faculty rank, and American Board of Internal Medicine specialty certification. The database also includes total numbers of publications as well as numbers of those designated as first author and last author publications (derived from PubMed), the number of National Institutes of Health (NIH) grants with the role as the principal investigator (PI) (derived from NIH RePORT), and the number of clinical trials as the PI or sub-investigator (derived from ClinicalTrials.gov). The designation of the top 20 US medical schools was identified by US News and World Report in 2013. Prior studies have used this database to study faculty promotion in academic medicine,1,9–11 and the data validity for faculty rank, NIH grants, and publications has been previously verified.1 We additionally validated the academic rank of 25 randomly selected rheumatologists.
We identified all adult rheumatologists in the US physician database with an academic faculty appointment in 2014 and a listed faculty rank of instructor, assistant professor, associate professor, or professor. We extracted the physician information described above.
We also identified the physicians with leadership positions as academic division directors and fellowship program directors by performing a manual review of all academic rheumatology division websites, which were obtained from the Association of American Medical Colleges.12 These data were collected between May and October, 2019. We subsequently linked these positions with the covariates extracted from Doximity. If data was missing from a website, we contacted member(s) of the rheumatology faculty at those institutions to clarify department leadership.
Statistical Analysis
We performed descriptive statistics, comparing physician characteristics among men and women, and performed two-sided t tests for continuous variables and Chi squared tests for categorical variables. We divided physicians by 10-year period of internal medicine residency graduation (1965–1974, 1975–1984, 1985–1994, 1995–2004, and 2005–2014) and determined the proportions of women and men in rheumatology with each academic faculty appointment (e.g., instructor, assistant professor, associate professor, professor) in 2014 per each cohort.
Using the primary outcome of faculty rank as a function of gender, we performed univariate logistic regression to determine the odds ratio (OR) and associated 95% confidence interval (CI) of women achieving the rank of associate professor or professor compared to men. We combined associate and professor ranks because these reflect senior faculty positions. As a secondary outcome, we determined the OR of women achieving the rank of professor compared with men. We performed multivariate logistic regression analyses to determine the adjusted ORs of these primary and secondary outcomes as a function of physician gender when adjusting for age, years since IM residency graduation, total publications, total NIH grants, total clinical trials involvement, and faculty at top 20 medical schools. We excluded rheumatologists with the rank of instructor from these analyses.
Next, we compared the unadjusted and adjusted OR of women being division directors or fellowship program directors compared with men. In the multivariable analyses, we adjusted for the same physician characteristics as in the faculty rank analysis.
All analyses were performed using SAS, version 9.4 (SAS Institute). We considered 2-tailed p values ≤ 0.05 to be statistically significant. This study was exempted from review by the Partners HealthCare Institutional Review Board.
RESULTS
We identified 6,125 practicing rheumatologists, 941 (15%) of whom had academic faculty appointments, in 2014. Among academic rheumatologists, we observed a gradual increase in the proportion of women entering academic rheumatology in each successive decade. Most recently, the number of women entering academic rheumatology exceeded the number of men (Figure 1). We also observed several differences between men and women in academic rheumatology (Table 1). On average, women were younger than men (46.0 ± 9.7 vs. 56.8 ± 11.9 years, P<0.001) and had fewer total publications (12.4 ± 20.8 vs. 26.4 ± 39.4, P<0.001) and NIH grants (0.8 ± 3.0 vs. 1.7 ± 4.4, P<0.001). There was no difference in the number of clinical trials for which women and men were listed as the PI (0.2 ± 0.8 vs. 0.2 ± 0.8, P=0.7).
Figure 1.
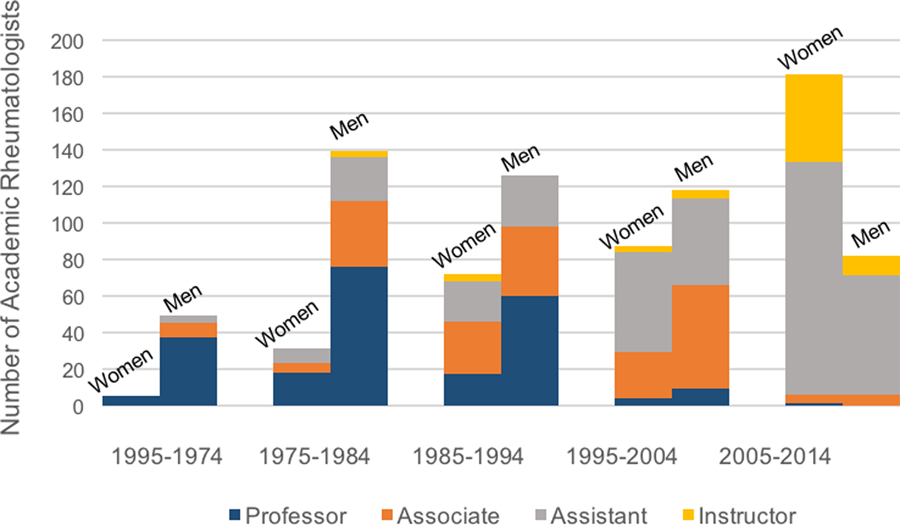
Academic Rank of Faculty Rheumatologists in 2014 by Year of Residency Graduation, According to Gender
Table 1.
Characteristics of Academic Rheumatologists in the United States
| Overall (N = 941) |
Men (N = 551) |
Women (N = 390) |
P-value | |
|---|---|---|---|---|
| Faculty Rank (N, %) | < 0.001 | |||
| Professor | 249 (26.7) | 200 (36.8) | 49 (12.6) | |
| Associate | 220 (23.6) | 152 (28.0) | 68 (17.5) | |
| Assistant | 387 (41.5) | 171 (31.5) | 216 (55.5) | |
| Instructor | 76 (8.2) | 20 (3.7) | 56 (14.4) | |
| Faculty at Top 20 Med School (N, %) | 320 (38.1) | 184 (35.9) | 136 (41.6) | 0.096 |
| Age (Mean, SD) | 52.3 (12.3) | 56.8 (11.9) | 46.0 (9.7) | < 0.001 |
| Age groups, y (N, %) | < 0.001 | |||
| Age <40 | 165 (18.4) | 41 (7.8) | 124 (33.5) | |
| Age 40–44 | 132 (14.7) | 64 (12.1) | 68 (18.4) | |
| Age 45–49 | 96 (10.7) | 52 (9.9) | 44 (11.9) | |
| Age 50–54 | 106 (11.8) | 54 (10.2) | 52 (14.1) | |
| Age 55–59 | 121 (13.5) | 79 (15.0) | 42 (11.4) | |
| Age 60–64 | 127 (14.1) | 99 (18.8) | 28 (7.6) | |
| Age 65+ | 151 (16.8) | 139 (26.3) | 12 (3.2) | |
| Year Since Residency (Mean, SD) | 22.0 (12.9) | 26.6 (13.0) | 15.7 (9.8) | < 0.001 |
| FACR (N, %) | 507 (53.9) | 300 (54.5) | 207 (53.1) | 0.678 |
| Publications | ||||
| Total (Mean, SD) | 20.6 (33.7) | 26.4 (39.4) | 12.4 (20.8) | < 0.001 |
| First or Last Author (Mean, SD) | 14.0 (28.9) | 18.4 (33.9) | 7.8 (17.9) | < 0.001 |
| Any Publication (N, %) | 739 (78.5) | 449 (81.5) | 290 (74.4) | 0.009 |
| National Institutes of Health grants | ||||
| NIH Grant Count (Mean, SD) | 1.3 (3.9) | 1.7 (4.4) | 0.8 (3.0) | < 0.001 |
| Any NIH Grant (N, %) | 164 (17.4) | 117 (21.2) | 47 (12.1) | < 0.001 |
| Clinical trials* | ||||
| Total Clinical Trials (Mean, SD) | 0.2 (0.8) | 0.2 (0.8) | 0.2 (0.8) | 0.676 |
| Any Clinical Trial (N, %) | 76 (8.1) | 50 (9.1) | 26 (6.7) | 0.182 |
FACR, Fellow of the American College of Rheumatology
Listed as principal investigator for registered studies on clinicaltrials.gov.
Compared to men, fewer women were professors (12.6% vs 36.8%) or associate professors (17.5% vs. 28.0%); however, a greater proportion of women were assistant professors (55.5% vs 31.5%). These differences were observed in the two most recent decades of residency graduation for which sufficient follow-up time had accrued to permit academic promotion (Figure 1). In unadjusted analyses, women were less likely than men to be full or associate professors (Table 2; OR 0.52, 95% CI: 0.45–0.60). These differences persisted in fully-adjusted analyses (aOR 0.78, 95% CI: 0.62–0.99). When the odds of being a full professor were examined individually (versus assistant professor or associate professor), we found no difference between women and men in fully-adjusted analyses (aOR 1.02, 95% CI: 0.77–1.37). There were only five women represented among all practicing academic rheumatologists who graduated from internal medicine residency between 1965 and 1974 (9.3%), and all of them were eventually promoted to the rank of full professor (Figure 1).
Table 2.
Leadership Positions by Gender in Academic Rheumatology
| Academic Position | Women (N, %) |
Men (N, %) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|---|---|---|---|---|
| N | 390 | 551 | ||
| Faculty Rank | ||||
| Associate professor or professor | 117 (30.1) | 352 (64.8) | 0.52 (0.45–0.60) | 0.78 (0.62–0.99) |
| Professor | 49 (12.6) | 152 (28.0) | 0.54 (0.45–0.64) | 1.02 (0.77–1.37) |
| Leadership Role | ||||
| Division director | 34 (8.7) | 74 (13.4) | 0.94 (0.72–1.21) | 0.96 (0.66–1.41) |
| Program director | 53 (13.6) | 64 (11.6) | 1.13 (0.88–1.46) | 0.99 (0.69–1.43) |
Adjusted for age, years since residency graduation, total publications, total NIH grants, total clinical trials, and faculty at top 20 med schools
Of the 117 academic rheumatology divisions in the US, 108 had an identifiable division director who was a rheumatologist. Of these, 34 programs (31.5%) had women as division directors, and 53 programs (45.3%) had women as fellowship program directors. In contrast to differences in academic rank (Table 2), women and men had similar adjusted odds of being rheumatology fellowship program directors (13.6% vs. 11.6%, aOR 0.99, 95% CI: 0.69–1.43) and rheumatology division directors (8.7% vs. 13.4%, aOR 0.96, 95% CI: 0.66–1.41).
DISCUSSION
We utilized comprehensive cross-sectional information on all licensed US rheumatologists to examine gender differences in academic rank and division-level leadership roles for women in academic rheumatology. We found that women were less likely than men to be associate or full professors, even after accounting for several measures of research and clinical productivity. However, women were as likely as men to hold leadership roles within rheumatology divisions. These findings establish important benchmarks for the rheumatology workforce and identify opportunities to improve equity among men and women in rheumatology.
The reasons remain unclear as to why there is inequity in attaining advanced academic rank in a specialty comprised nearly equally of women and men. However, we found important differences in the characteristics of women and men in academic rheumatology which may contribute to our observations. A traditional pathway to academic promotion entails scholarly productivity, which can be evaluated using publications and grant funding. We found that women had fewer publications and less grant funding than men, but observed no significant gender differences in the likelihood of being the PI of a clinical trial. The explanation for women having fewer publications and NIH grants is likely multifactorial, including time in the workforce, mentorship, work-life balance, and time spent on parental leave. However, gender differences in academic promotion remained after adjusting for each of these typical promotion criteria, indicating that other unidentified factors also contribute to the gap in promotion for women academic rheumatologists.
Gender differences in academic promotion could be partially explained by differences in the amount of effort devoted to medical education and administrative roles, which may reduce time available for research and may not be valued as highly as research productivity in terms of academic promotion. We were unable to determine primary academic roles (e.g., basic science or clinical investigation, medical education, clinical care), and this information is not publicly available or systematically collected to our knowledge for most academic rheumatologists. We were also unable to account for potential differences in tenure versus non-tenure track academic positions and part-time positions. Additional studies are needed to understand the institutional and societal barriers to academic promotion for women. We could not assess the impact of institutional support, mentorship, or overt and unconscious bias on our findings.
While barriers to academic promotion may negatively impact the opportunities for women in rheumatology to achieve senior faculty positions, we found that women and men were similarly likely to occupy key leadership positions within rheumatology divisions. These differences may reflect how decisions regarding who will be advanced through academic and leadership ranks are based on different factors. While academic promotion tracks typically prioritize stringent productivity requirements in the research setting, selection for academic leadership roles may be based on other attributes such as interpersonal, mentorship, and leadership skills. Both achievements reflect important successes in one’s academic career as well as an individual’s impact on his or her profession. Further work is needed to understand how these barriers and opportunities may influence the recruitment and retention of women academic rheumatologists.
As internal medicine residents have grown more interested in pursuing careers in rheumatology, competition for a limited number of spots in rheumatology fellowship training programs has increased; in fact, rheumatology has become nearly as competitive as the historically most competitive medicine subspecialty, cardiology, in terms of the proportion of fellowship applicants who fail to match in a training program.13 However, rheumatology faces major challenges with the projected upcoming workforce gap.5 While the academic workforce comprises only a small proportion (15%) of the entire rheumatology workforce, academic institutions provide the vast majority of rheumatology specialty training.4 It is important to maintain adequate representation of women among leadership positions in these academic rheumatology divisions, and to ensure that there is equity between genders for advancement in an academic rheumatology career. Furthermore, given growth in supply-demand mismatches for rheumatologists, it behooves the specialty of rheumatology to not only increase its numbers of new trainees but also undertake efforts to reduce avoidable attrition from this specialty. Addressing physician job satisfaction, physician wellness and successful professional growth are important features in sustaining a healthy rheumatology workforce.
Our study has several strengths and limitations. Our data source contained comprehensive cross-sectional information on all US physicians with an NPI number. Therefore, our findings are highly generalizable. However, we are not able to account for physicians who left academic practice. If greater numbers of women than men left the academic rheumatology workforce—for one of many reasons, including that they were not promoted—our findings could underestimate sex differences in academic rank. We also cannot account for how parental leave, which has historically been longer for women than for men, may have impacted our results. In addition, we cannot account for differences in work effort, and we know that women rheumatologists are more likely to work part-time than are their male counterparts.4 We were also unable to assess gender disparities in pay.
In conclusion, we found that women in rheumatology are less likely than men to achieve senior faculty positions in US medical schools but have similar opportunities for attaining leadership opportunities within rheumatology divisions. These discrepancies might indicate differences in the value placed on different roles women and men may have in the academic setting and highlight barriers to the promotion of women faculty. Further work is needed to characterize and address these barriers. As the workforce gender balance continues to shift, equity in the academic advancement of women in rheumatology must be ensured.
Acknowledgements:
Preliminary data from this study was presented as an abstract at the American College of Rheumatology Annual Meeting in November, 2019.
Financial Support:
Dr. Jorge receives funding from the Rheumatology Research Foundation (Scientist Development Award).
Dr. Wallace receives funding from NIH/NIAMS (K23AR073334 and L30AR070520).
REFERENCES
- 1.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex Differences in Academic Rank in US Medical Schools in 2014. Jama 2015;314:1149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Applicants, Matriculants, Enrollment, Graduates, MD-PhD, and Residency Applicants Data2019.
- 3.Magrane D, Jolly P. The changing representation of men and women in academic medicine 2005
- 4.Battafarano DF, Ditmyer M, Bolster MB, et al. 2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030. Arthritis care & research 2018;70:617–26. [DOI] [PubMed] [Google Scholar]
- 5.Bolster MB, Bass AR, Hausmann JS, et al. 2015 American College of Rheumatology Workforce Study: The Role of Graduate Medical Education in Adult Rheumatology. Arthritis & rheumatology (Hoboken, NJ) 2018;70:817–25. [DOI] [PubMed] [Google Scholar]
- 6.Nonnemaker L Women physicians in academic medicine: new insights from cohort studies. The New England journal of medicine 2000;342:399–405. [DOI] [PubMed] [Google Scholar]
- 7.Ruzycki SM, Freeman G, Bharwani A, Brown A. Association of Physician Characteristics With Perceptions and Experiences of Gender Equity in an Academic Internal Medicine Department. JAMA network open 2019;2:e1915165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jena AB, Olenski AR, Blumenthal DM. Sex Differences in Physician Salary in US Public Medical Schools. JAMA internal medicine 2016;176:1294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenthal DM, Olenski AR, Yeh RW, et al. Sex Differences in Faculty Rank Among Academic Cardiologists in the United States. Circulation 2017;135:506–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blumenthal KG, Huebner EM, Banerji A, et al. Sex differences in academic rank in allergy/immunology. The Journal of allergy and clinical immunology 2019. [DOI] [PMC free article] [PubMed]
- 11.Manne-Goehler J, Kapoor N, Blumenthal DM, Stead W. Sex differences in achievement and faculty rank in academic infectious diseases. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2019. [DOI] [PubMed]
- 12.Rheumatology (Internal Medicine). Electronic Residency Application Service. AAMC; 2019, at https://services.aamc.org/.) [Google Scholar]
- 13.Charting Outcomes in the match, Specialties Matching Service, Appointment year 2018: National Resident Matching Program; October 2018.


