Abstract
While most countries in the Western Pacific Region (WPR) had similar trajectories of COVID-19 from January to May, their implementations of non-pharmaceutical interventions (NPIs) differed by transmission stages. To offer a better understanding for an implementation of multidisciplinary policies in COVID-19 control, we compared the impact of NPIs by assessing the transmissibility and severity of COVID-19 in different phases of the epidemic during the first five months in WPR. In this study, we estimated the piecewise instantaneous reproduction number (Rt) and the reporting delay-adjusted case-fatality ratio (dCFR) of COVID-19 in seven WPR jurisdictions: Hong Kong Special Administrative Region, Japan, Malaysia, Shanghai, Singapore, South Korea, and Taiwan. According to the results, implementing NPIs was associated with an apparent reduction of the piecewise Rt in two epidemic waves in general. However, large cluster outbreaks raised the piecewise Rt to a high level. We also observed relaxing the NPIs could result in an increase of Rt. The estimated dCFR ranged from 0.09% to 1.59% among the jurisdictions, except in Japan where an estimate of 5.31% might be due to low testing efforts. To conclude, in conjunction with border control measures to reduce influx of imported cases which might cause local outbreaks, other NPIs including social distancing measures along with case finding by rapid tests are also necessary to prevent potential large cluster outbreaks and transmissions from undetected cases. A comparatively lower CFR may reflect the health system capacity of these jurisdictions. In order to keep track of sustained disease transmission due to resumption of economic activities, a close monitoring of disease transmissibility is recommended in the relaxation phase. The report of transmission of SARS CoV-2 to pets in Hong Kong and to mink in farm outbreaks highlight for the control of COVID-19 and emerging infectious disease, the One Health approach is critical in understanding and accounting for how human, animals and environment health are intricately connected.
Keywords: COVID-19, Case-fatality, Reproduction number, Western pacific, Non-pharmaceutical
Highlights
-
•
Multidisciplinary One Health policies to combat COVID-19 are required in WPR.
-
•
NPIs were associated with an apparent reduction in transmissibility of COVID-19.
-
•
However, some large cluster outbreaks raised the transmissibility to a high level.
-
•
We observed an increase in transmissibility when NPIs were partially lifted.
-
•
A lower case-fatality ratio in WPR may reflect the health system capacity.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has posed extraordinary challenges to healthcare systems and societies across the globe. By August 7th, the Western Pacific Region (WPR) has accumulated 353,564 cases and 8626 deaths, the least out of the six WHO regions, despite having been fighting the pandemic longer than any of its counterparts with the city of Wuhan in China being the epicentre of the initial outbreak [1]. The region observed its largest accumulation of cases and deaths from January to March, and in response, many of its members put in place a series of non-pharmaceutical interventions (NPIs), including border controls, case detection and management, contact tracing and quarantine, and social distancing with the aim to slow the spread of infection through reduced contact within and between populations in light of limited definitive evidence on prevention and treatment for COVID-19.
Since the emergence of COVID-19, scientists around the world have been examining the impact of NPIs in controlling the outbreak with consistent findings demonstrated in Wuhan, Europe and world-wide cross-country settings [[2], [3], [4], [5]]. However, the impact of NPIs on the epidemics in the broader WPR has not been well-studied. Further, in many jurisdictions of WPR, first COVID-19 cases were confirmed in January 2020 and they had since shared similar trajectories of the epidemics until the end of May, characterized by mainly two waves of cases that first came from regions inside of China and second from the other countries affected by the pandemic. The governments of these jurisdictions enacted suites of NPIs at different stages of the epidemics and most of them started gradually relaxing the NPIs by May as community transmission was brought under control.
One Health, defined as “an approach to designing and implementing programmes, policies, legislation and research in which multiple sectors communicate and work together to achieve better public health outcomes” [30] encompasses the interaction of health between human, animal, and environment. The outbreak of COVID-19, started in Wuhan, China likely from a wet market of live animals has caused a substantial increase in the number of infections and deaths globally. The pandemic emphasizes a need for preparation and response to human diseases originating from indiscriminate contacts with infected animals. The challenges of a concerted global effort for the control of the COVID-19 pandemic will only be assuaged through an effective multi sectorial collaboration in multidisciplinary research and practice [31,32,33]. In this study, we aim to compare, under similar trajectories of the epidemics described above, the impact of NPIs in seven jurisdictions of the WPR by quantifying the transmissibility and severity of COVID-19 infections in different phases of the pandemic during the first five months.
2. Materials and methods
2.1. Selection of jurisdictions
A panel of experts in public health policy, epidemiology and academia from the WPR convened in April comprising the Health System Impact Subgroup under the COVID-19 WHO Research Roadmap Social Science Working Group to study government response actions and synthesise key policy learning in the region. The current study is a complement to the original work by the Subgroup and covers seven jurisdictions including Hong Kong Special Administrative Region, Japan, Malaysia, Shanghai, Singapore, South Korea represented by the members of the study group and Taiwan. They represent a variety of jurisdictions in the WPR outside of the epicentre with well-developed health systems serving reasonably sized populations, and provide opportunities to assess the impact of the combinations of NPIs implemented under different contexts.
2.2. Information on NPIs
The current study focuses on NPIs in two broad categories namely those aimed at travel restrictions and social distancing. The jurisdictions under study implemented these two broad categories of measures in similar order with border control followed by social distancing measures. The experts provided a list of key measures implemented in their jurisdictions for each of the areas above, and the resource considerations for implementation including those relating to human and physical infrastructure. Other sources of information were from the official websites (Appendix Table S1). The timeline of the control measures in different jurisdictions is shown in Appendix Table S2.
2.3. Data on daily number of cases and deaths
We collected the daily number of local and imported cases by their illness onset dates and/or confirmed dates from January 1 to May 31, 2020 to estimate the instantaneous reproduction number (Rt) and piecewise Rt, as common measures of transmissibility by time, and number of deaths to estimate the case-fatality ratio (CFR), as a measure of severity of COVID-19 in the seven jurisdictions. Individual-level data was publicly available in Hong Kong. Numbers of cases and deaths by illness onset date and confirmation date were available in Singapore. In other jurisdictions, only the numbers of cases and deaths by confirmation date were available. The sources of data and remarks were listed in Appendix Table S1.
The Rt is a common measure for monitoring transmissibility of an infectious disease in a population and sufficiency of community measures being carried out to control an epidemic at time t. When Rt falls below its threshold value of one, the disease is unlikely to sustain in a population over time. When Rt approaches zero, the control measures can be regarded as bringing an epidemic under control [6]. Local cases refer to any cases with the infection acquired locally. Imported cases refer to those who are suspected to have contracted the infections outside the jurisdictions and include both residents returning from abroad and visitors / non-residents entering the jurisdictions.
2.4. Comparison of transmissibility in different periods
To facilitate comparison of disease transmission dynamics across jurisdictions, epidemic trajectories were sectioned into five different periods for each jurisdiction: (1) pre-intervention period in the first wave of the epidemic (i.e. from January 1, 2020 to the initial date of implementing NPIs in the first wave), (2) intervention period in the first wave (i.e. from the day after pre-intervention period up to February 20, 2020, a date around the end of epidemic in China) [7], (3) transitional period between the first and second wave (i.e. from the day after the first intervention period to the day before the initial implementation of NPIs in the second wave), (4) intervention period in the second wave (i.e. following period up to the start of relaxing measures), and (5) relaxation period (i.e. following period up to May 31, 2020). We then compared the changes of transmissibility between periods. Three jurisdictions experienced large cluster outbreaks in the study period: South Korea (Shincheonji Church of Jesus), Malaysia (Seri Petaling tabligh cluster), and Singapore (cluster of dormitories). To minimize their effects on the dispersion of transmissibility, they were investigated separately.
To estimate piecewise Rt for summarizing the impact of NPIs in different periods, we started with estimating the Rm,t, an instantaneous reproduction number in a jurisdiction m, using the method from Thompson and his colleagues accounting for the transmission potential from the imported cases [8]. We assumed the length of serial interval follows a gamma distribution with mean 6.5 days and a coefficient of variation of 0.62 [4]. We determined the Rm,t starting from the date of illness onset of the first case to May 31, 2020. While illness onset date was available for the cases in Hong Kong and Singapore, only confirmation date was available for the cases in the other jurisdictions. We therefore re-built the epidemic curves for these jurisdictions adjusted with the reporting delay between illness onset and ascertainment of a case using the method from Leung et al. [7]. Based on the individual records that were only available in Hong Kong, we assumed the length of reporting delay follows a gamma distribution with mean of 6.8 and standard deviation (SD) of 4.6 days in the first wave and mean of 3.7 and SD of 4.6 days in the second wave and thereafter. Based on the Rm,t, we obtained the estimated piecewise Rt for summarizing using a similar form of Bayesian regression model from Flaxman and colleagues [4] We sampled the posterior means of the piecewise Rm,t as our estimates with corresponding 95% credible intervals (CrIs).
2.5. Estimation of case-fatality rates
We estimated the crude case fatality rate (CFR) by dividing the cumulative number of deaths by the cumulative number of cases on their date of confirmation. To adjust for the reporting delay between illness onset and death, we also estimated the delay-adjusted CFR (dCFR) using a similar method as above to adjust for reporting delay. The delay between illness onset and death was assumed to follow a gamma distribution with mean of 16 and SD of 6 days [9,10]. Poisson-to-binomial approximation was used to estimate the confidence intervals (CIs) of the CFRs.
The estimation of instantaneous Rt and CFR were programmed using Microsoft Excel (version 2016) and the piecewise Rt was fitted using package ‘brms’ in R (version 3.6.3) [11]. Technical details for the estimations are documented in Appendix.
3. Results
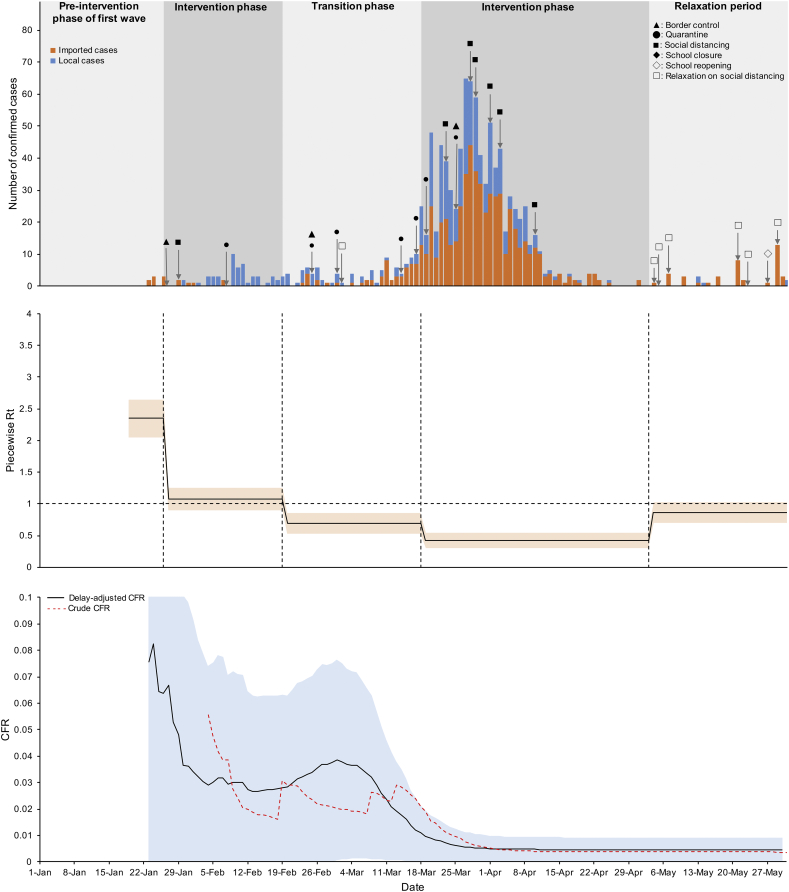
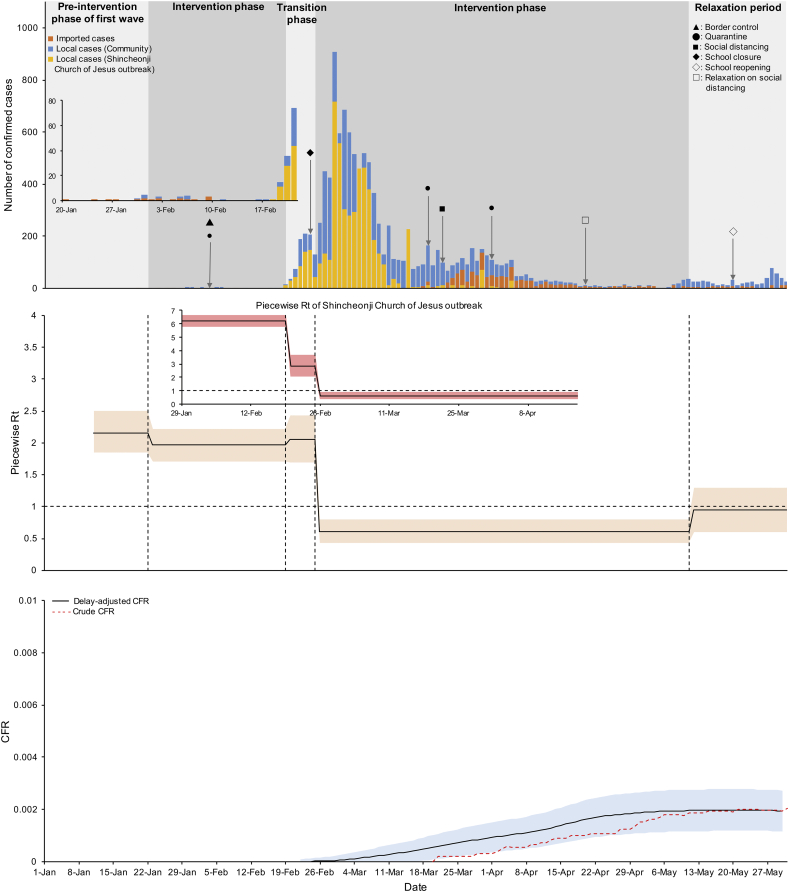
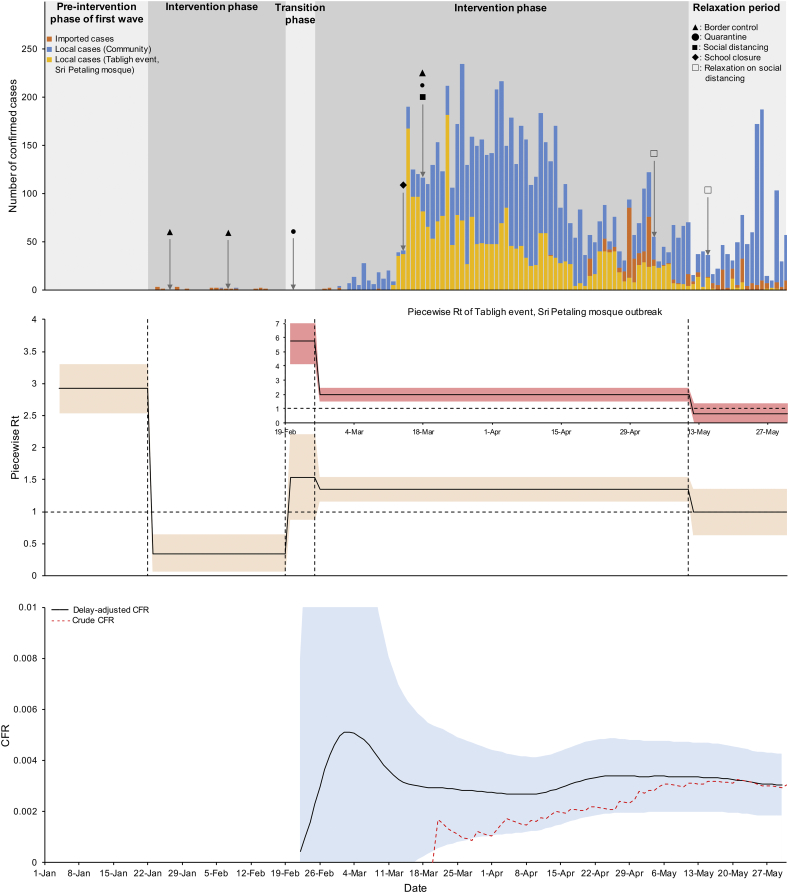
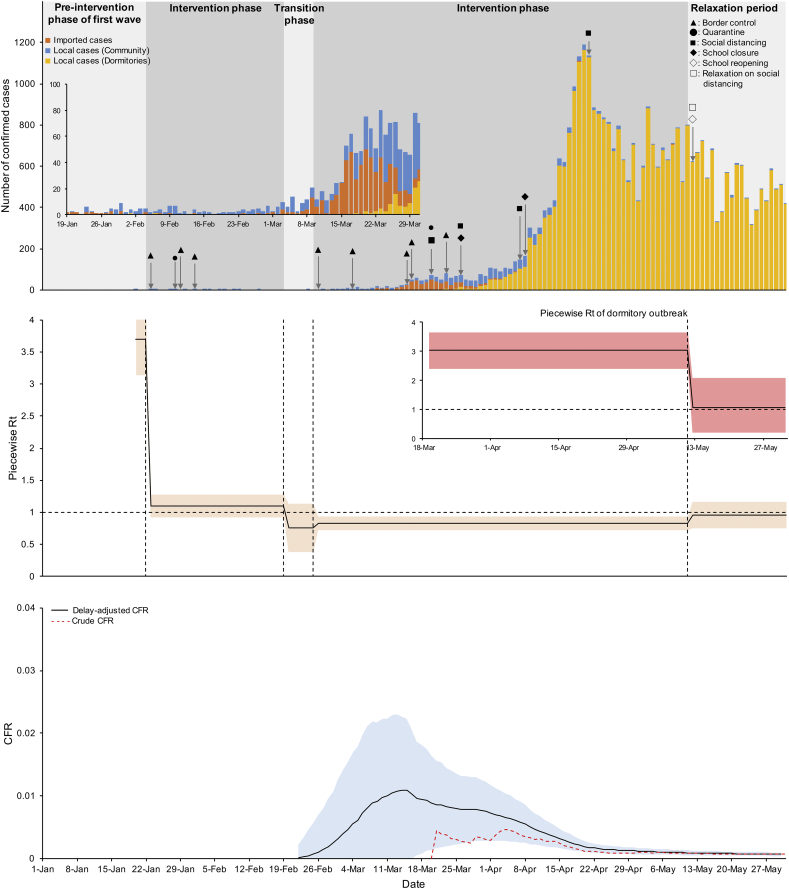
The epidemic curves (top panel), posterior means and 95% CrI of piecewise Rt (middle panel), and CFR (bottom panel) in each of the jurisdictions are shown in Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7. In the first epidemic, outbreaks in different jurisdictions were primarily driven by the imported cases with exposure to Wuhan city or Hubei province in China. Of the seven jurisdictions, the posterior means of piecewise Rt in the pre-intervention phase of the first epidemic were greater than one: 2.35 (95% CrI: 2.35–2.65) in Hong Kong, 1.91 (95% CrI: 1.61–2.21) in Japan, 2.93 (95% CrI: 2.54–3.30) in Malaysia, 3.36 (95% CrI: 3.12–3.59) in Shanghai, 3.70 (95% CrI: 3.14–4.25) in Singapore, 2.15 (95% CrI: 1.85–2.50) in South Korea, and 1.83 (95% CrI: 1.54–2.12) in Taiwan. While imported cases were mostly from a single source country, implementation of border control and quarantine measures in the intervention phase during the first wave reduced the posterior means of piecewise Rt to around one except for South Korea which experienced an outbreak from Shincheonji Church of Jesus in which piecewise Rt was kept at a high level.
Fig. 1.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Hong Kong.
Interventions on first wave:
▲ (27 Jan): Entry restrictions on Hubei.
◼ (29 Jan): Special work arrangements for civil servants until 2 Mar.
● (8 Feb): 14-day mandatory quarantine on the Mainland China.
☐ (2 Mar): Resume normal work arrangements for civil servants.
Interventions on second wave:
▲ (25 Feb): Entry restrictions on non-HK residents coming from Korea or having visited Korea in the past 14 days.
● (25 Feb): All HK residents coming back from Korea will be put on medical surveillance for 14 days, while those HK residents having visited Daegu or Gyeongsangbuk-do will be sent to quarantine centres for compulsory quarantine for 14 days.
● (1 Mar): Issued quarantine orders to people arriving Hong Kong who have been to the three regions in Italy or to Iran where the Red OTA remains in force in the past 14 days (regardless of whether they are Hong Kong residents).
● (14 Mar): Issued quarantine orders to people arriving Hong Kong who have been to some regions in France, Germany, Japan and Spain as well as on the entire country of Italy in the past 14 days (regardless of.
whether they are Hong Kong residents).
● (17 Mar): Issued quarantine orders to people arriving Hong Kong who have been to 26 European countries in the Schengen Area in the past 14 days (regardless of whether they are Hong Kong residents).
● (19 Mar): 14-day mandatory quarantine on all overseas countries/territories.
◼ (23 Mar): Special work arrangements for civil servants until 4 May.
▲ (25 MAr): All non-Hong Kong residents coming from overseas countries and regions by plane will be denied entry to Hong Kong; non-Hong Kong Residents coming from the Mainland, Macao and Taiwan will be denied entry to Hong Kong if they have been to any overseas countries and regions in the past 14 days; all transit services at Hong Kong International Airport will be suspended.
● (25 Mar): All travelers coming from Macao and Taiwan will be subject to compulsory quarantine.
◼ (28 Mar): Six types of premises (i.e. amusement game centres, bathhouses, fitness centres, places of amusement, places of public entertainment and premises for hire for holding social gatherings) closed from 6 p.m. on March 28.
◼ (29 Mar): Prohibition on group gathering of >4 people in public places.
◼ (1 Apr): Karaoke establishments, mahjong‑tin kau establishments and nightclubs closed from 6 p.m. on April 1.
◼ (3 Apr): Bars closed from 6 p.m. on 3 April.
◼ (10 Apr): Closure of beauty parlours and massage establishments from midnight on 10 April.
Interventions on relaxation period:
☐ (4 May): Resume normal work arrangements for civil servants.
☐ (5 May): Prohibition on group gathering of >8 people in public places until 18 Jun.
☐ (7 May): Reopening of entertainment facilities; Allowing the reopening, subject to compliance with certain requirements, of seven types of business premises including amusement game centres, fitness centres, places of amusement, places of public entertainment (such as cinemas), beauty parlours, massage establishments and mahjong‑tin kau premises; allowing bars and pubs to resume operations subject to compliance with more stringent requirements.
☐ (21 May): Reopen most public swimming pools and barbecue sites.
☐ (23 May): Reopen beaches.
◇ (27 May): Reopening of schools.
☐ (29 May): Allow bathhouses, party rooms, clubs or nightclubs and karaoke establishments to resume operation.
Fig. 2.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Shanghai.
Interventions on first wave:
◼ (24 Jan): Extended return-to-work date from Chinese New Year (CNY) and work from home until Feb 9; Close all business premises except healthcare, pharmacists, supermarkets, wet markets, grocery and convenience stores until Feb 9; Cancel centralized meetings and collective activities until May 9; Cancel offline training until May 18; Closure of indoor culture facilities (Library, art gallery, museum) and entertainment facilities until May 9; and closure of theaters.
◆ (24 Jan): Extended return-to-school date from CNY until Apr 27.
● (27 Jan): Mandatory 14-day quarantine for people who lived or traveled in Hubei (except Wuhan) within 14 days until Mar 18; and mandatory 14-day quarantine for people who lived or traveled in Wuhan within 14 days until April 8.
☐ (9 Feb): Return-to-work; Reopening of business.
Interventions on second wave:
● (26 Mar): Mandatory 14-day quarantine for arriving people from all overseas countries/ territories.
▲ (29 Mar): Reduced the number of international flights (each international airline can only keep 1 route, and each route can only operate 1 flight per week), and occupancy rate no more than 75%. From June 8, 2020, flight incentives and fuse measures will be implemented (Incentives: If the number of passengers who have a positive nucleic acid test result is zero for three consecutive weeks on the same route, the airline may increase the number of flights to a maximum of 2 flights per week; Fused measures: for airlines on the same route, if the number of passengers with positive nucleic acid test results reaches 5, the company will suspend the operation of this route for 1 week; if it reaches 10, suspend for 4 weeks) until Jun 8.
Interventions on relaxation period:
☐ (27 Apr): Avoiding concentrated dining by canteen delivery or off-peak dining.
◇ (27 Apr): Reopening of schools (registration when enter and leave school).
☐ (9 May): Reopening of indoor culture facilities (Library, art gallery, museum) and entertainment facilities; and allow centralized meetings and collective activities.
Fig. 3.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Taiwan.
Interventions on first wave:
▲ (23 Jan): Decline entry of people who resides or originally resided in Wuhan.
▲ (25 Jan): Decline entry of people who resides or originally resided in Hubei.
● (26 Jan): Residences from China and chinese people undergo mandatory 14-day home quarantine;
◆ (3 Feb): Postponed the opening of University and Collegue until Feb 25.
◆ (11 Feb): Postponed the opening of schools until Feb 25.
◇ (25 Feb): Reopening of schools.
Interventions on second wave:
▲ (19 Mar): Banning foriegners entering except those carrying out terms of a business contract, holding valid Alien Resident Certificates, diplomatic credentials, or other official documentation and special permits.
● (21 Mar): Inbound travelers from US and East Asia between 8 and 18/3 and developed symptoms in the said period of time are required to undergo home quarantine, and be tested for retrospective investigation.
◼ (25 Mar): Indoor events that are attended by >100 people and outdoor gatherings that are attended by >500 people be suspended.
◼ (9 Apr): Host and hostess clubs and ballrooms will suspend operations.
◼ (10 Apr): Crowd control measures have been imposed at public places where large crowds can gather including renowned tourist attractions, national parks, recreational areas, night markets and temples.
● (1 May): Monitoring travelers to Wuhan within fourteen days and exhibited a fever or symptoms of upper respiratory tract infections. They were screened for 26 known pathogens, including SARS and MERS, and those testing positive were quarantined.
● (4 May): Inbound travelers should stay at the dedicated qurantine hotels if they live with people who are 65 years old or older, children 6 years old or under, persons with chronic disease (such as cardiovascular diseases, diabetes or lung disease), or persons who don't have a separate room (including a separate bathroom).
Interventions on relaxation period:
☐ (7 May): Applications for the lodging sites in Yushan National Park, Taroko National Park and Shei-Pa National Park will be accepted.
Fig. 4.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in South Korea.
Interventions on first wave:
▲ (4 Feb): Entry ban on foreigners with travel history to Hubei, China.
● (4 Feb): Special entry procedure for arriving persons from Mainland China (Which includes body temperature screening, medical questionnaire, and installing ‘Self-quarantine safety protection App’) - for both non-residents and residents.
◆ (24 Feb): School closure.
Interventions on second wave:
● (19 Mar): Special entry procedure for persons arriving from all overseas countries/ territories (Which includes body temperature screening, medical questionnaire, and installing ‘Self-quarantine safety protection App’) - For both non-residents and residents.
● (1 Apr): Mandatory 14-day quarantine for persons arriving from all overseas countries/ territories.
Interventions on relaxation period:
☐ (20 Apr): Relieved recommendation of closing indoor sports facilities, recreational facilities and religious facilities.
◇ (20 May): Started re-opening schools, starting with high school grade 3 students.
Fig. 5.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Malaysia.
Interventions on first wave:
▲ (27 Jan): Bans visitors from Wuhan, Hubei.
▲ (7 Feb): Bans visitors from other areas under Chinese lockdown.
● (21 Feb): Malaysians from China arriving in Malaysia - to be tested and if negative to undergo mandatory 14-day quarantine.
Interventions on second wave:
◆ (14 Mar): School closure: Schools have been closed since the start of the 1st term holidays (14th March 2020). However, upper secondary classes (Forms 5 & 6) where students will be sitting major public examination reopened on 24th June 2020.
▲ (18 Mar): Entry restrictions on foreign visitors and tourists from countries/territories.
● (18 Mar): Malaysians arriving in Malaysia - mandatory 14-day quarantine.
◼ (18 Mar): Movement Control Order (MCO); All mass gathering banned; Work from home for civil service and private sector except essential services until May 3; Close all business premises except supermarkets, wet markets, grocery and convenience stores. Food outlets are allowed to serve take-away customers only until May 3; Closure of hair salons, barbers, open-air markets; All mass gathering banned until June 15; Closure of all indoor entertainment/recreational facilities including swimming pools and cinemas Jul 1; and closure of gyms, indoor sports venues and snooker centres until Jun 15.
Interventions on relaxation period:
☐ (4 May): Conditional Movement Control Order (CMCO) until June 6; Civil servants to work from home, staggered working hours or working in the ofiice on alternate days. Similar arrangements encouraged for the private sector; and reopening of most businesses, including childcare centres, provided they are able to abide by rules for hygiene and social distancing. Exceptions include indoor entertainement centres (eg cinemas and gyms) remain closed.
☐ (15 May): Mosque prayers allowed for limited number of attendees.
Fig. 6.
Number of cases by illness onset date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Singapore.
Interventions on first wave:
▲ (23 Jan): Suspended all flights between Singapore and Wuhan.
● (28 Jan): Mandatory quarantine for persons with recent travel history to Hubei.
▲ (29 Jan): Barred entry of visitors with recent travel history to Hubei.
▲ (1 Feb): Border restrictions expanded to mainland China.
Interventions on second wave:
▲ (26 Feb): Border restrictions expanded to Daegu city and Cheongdo county, Republic of Korea.
▲ (4 Mar): Border restrictions expanded to Iran, Northern Italy and Republic of Korea.
▲ (15 Mar): Border restrictions expanded to Italy, France, Spain and Germany.
▲ (16 Mar): Border restrictions expanded to ASEAN countries, Japan, Switzerland and United Kingdom.
● (20 Mar): Visitors and returning residents from all other countries placed on 14-day Stay-Home Notice (SHN).
◼ (20 Mar): Suspension of all events/gatherings with 250 or more participants; and separation of at least 1 m between patrons at public venues.
▲ (23 Mar): Barred entry of visitors from all countries.
◼ (26 Mar): Limit gatherings outside work and school to 10 people or fewer; Closure of bars and entertainment venues (night clubs, cinemas, theaters, karaoke outlets); Reduce operating capacity of malls, museums and attractions to one person per 16 sqm; Suspend all religious services and congregations; and cancel all events and mass gatherings (conferences, exhibitions, festivals, concerts, sporting events).
◆ (26 Mar): Suspend all tuition and enrichment centre classes.
◼ (7 Apr): Start of “circuit breaker”; Closure of workplaces/retail outlets except essential services and selected economic sectors; Stay at home except for essential purposes; No social gatherings beyond immediate family; F&B outlets open for takeaway or delivery only; and closure of all attractions, theme parks, museums, casinos, sports and recreation facilities, places of worship.
◆ (8 Apr): Full home-based learning for schools and institutes of higher learning; and closure of pre-schools and student care centres.
◼ (21 Apr): Lockdown of all dormitories; and mandatory Stay-Home Notice for migrant workers in the construction sector.
Interventions on relaxation period:
☐ (12 May): Allow home-based food businesses, confectioneries, hairdressers and laundry services to resume operations.
◇ (12 May): Small group lessons for students in graduating cohorts.
Fig. 7.
Number of cases by confirmation date (top), piecewise reproduction number (Rt) (middle), and case-fatality ratios (CFRs) (bottom) in Japan.
Interventions on first wave:
▲ (31 Jan): Immigrant restriction from Wuhan and surrounding district.
Interventions on second wave:
◆ (2 Mar): Suspension of all school and learning.
● (6 Mar): 14 days quarantine at designated places, no public transportation use from mainland China and South Korea.
● (19 Mar): 14 days quarantine at designated places, no public transportation use from almost all overseas countries/territories.
▲ (27 Mar): Immigrant restriction from non-resident travelers from Italy, France, Germany, and designated European countries.
▲ (3 Apr): Immigrant restriction from mainland China, UK, and USA.
◼ (7 Apr): Work from home, flexible working hours, split commune time.
Interventions on relaxation period:
☐ (14 May): Re-open shops (recommendation).
With the effect from the prolonged NPIs in the first wave, the estimated piecewise Rt dropped gradually in Hong Kong (posterior mean = 0.42, 95% CrI: 0.29–0.55), Shanghai (0.28, 95% CrI: 0.10–0.46), Singapore (0.75, 95% CrI: 0.38–1.14), and Taiwan (0.41, 95% CrI: 0.17–0.65) in the transition phase. In Malaysia and South Korea where large cluster outbreaks were reported, their piecewise Rt were greater than one.
Although cases were imported from countries worldwide, NPIs were associated with different levels of reductions in estimated Rt in different jurisdictions (except Japan) during the intervention phase of the second wave. Some of their posterior means of piecewise Rt were below one: 0.42 (95% CrI: 0.29–0.55) in Hong Kong, 0.09 (95% CrI: 0.00–0.24) in Shanghai, 0.96 (95% CrI: 0.75–1.16) in Singapore, 0.12 (95% CrI: 0.01–0.28) in Taiwan, and 0.61 (95% CrI: 0.43–0.80) in South Korea. In Singapore and Malaysia, where large cluster outbreaks were observed and their piecewise Rt were 3.02 (95% CrI: 2.39–3.65) and 5.73 (95% CrI: 4.10–7.26) respectively. With control measures implemented targeting these clusters, reductions in reported cases were observed but their piecewise Rt were still above one.
We observed that relaxing the NPIs resulted in increase of transmissibility in some jurisdictions. For example, in Hong Kong when social distancing measures were eased, the piecewise Rt increased slightly to 0.86 (95% CrI: 0.70–1.03).
To assess the severity of COVID-19, we estimated the CFRs and they were similar among the jurisdictions among 6 of the 7 jurisdictions. In mid-May when the stochastic uncertainty has been much reduced owing to an accumulation of reported cases, the estimated dCFR was 0.47% (95% CI: 0.01%–0.93%) in Hong Kong, 5.31% (95% CI: 4.97%–5.65%) in Japan, 0.33% (95% CI: 0.20%–0.47%) in Malaysia, 1.05% (95% CI: 0.27%–1.82%) in Shanghai, 0.09% (95% CI: 0.05%–0.12%) in Singapore, 0.20% (95% CI: 0.11%–0.28%) in South Korea, and 1.59% (95% CI: 0.43%–2.75%) in Taiwan.
4. Discussion
In this study, we assessed transmissibility and severity of COVID-19 in different phases of epidemics in seven jurisdictions of the WPR during the first five months. According to our empirical findings, NPIs were generally able to control the transmissibility during the two waves of the epidemic in the WPR jurisdictions. However, if control measures only targeted case importation without adequate social distancing measures, large clusters could emerge (e.g. the dormitory outbreaks in Singapore) which substantially increase transmissibility to a high level even though the reproduction number outside the clusters may be below the threshold value of one [12]. Over-dispersed transmission patterns were seen in SARS and recently noted for COVID-19 outside China [13,14]. In Singapore, owing to an early ban of visitors with travel history to Hubei and mainland China, the first wave of epidemic was well-managed given that Rt was greatly reduced to around one. However, border control measures can rarely be complete in curtailing the risk of outbreaks in the community. For Singapore, a few unidentified cases from overseas were the suspected cause for the large cluster outbreaks among migrant workers living in purpose-built mega dormitories [15]. Similarly, South Korea had a high level of transmissibility in the first wave owing to a super-spreading event in February involving the Shincheonji Church of Jesus cluster to which thousands of cases were linked. This is in line with Lai et al. [16], which suggested that compared with travel restrictions, social distancing measures aiming to reduce contacts between individuals are more effective in curbing the spread of COVID-19 in the wider community [17], This is achieved through lowering the potential of domestic symptomatic transmissions, as well as that of transmissions from asymptomatic or mild cases. Early investigations on the influenza A/H1N1 pandemic indicated travel restrictions were more effective in deferring an epidemic than on reducing the epidemic size [18,19]. Therefore, it should be emphasized that NPIs aiming to reduce introduction of infections from external sources as well as transmission in the community should be deployed as an integrated package, in line with WHO's recommendations [20].
Among the jurisdictions we studied, Japan had an estimated CFR of around 5% in mid-May and a relatively higher Rt in the intervention period of second epidemic. From our observation, the viral testing rate per person in Japan remained the lowest among the jurisdictions even during the peak of the epidemic in April (Appendix Fig. S1). Selective testing for high risk segment may allow a large proportion of undetected asymptomatic cases to sustain a transmission in the community [21], Apart from that, with fewer tests performed, there could have been a lower total number of confirmed cases relative to the proportion of severe cases that leads to death, hence increasing the CFR. We also postulate that delayed and flexible implementation of NPIs, which highly depended on voluntary compliance, was another possible cause. Echoing the studies by Matrajt and Leung [22], the timing and aggressiveness of NPIs could greatly affect the epidemic curve in terms of peak time deferral and peak size. A simulation study suggested that delaying the introduction of NPIs by even a single week could have led to 3-fold increase in the number of reported cases [16].
When the NPIs were partially lifted in Hong Kong, Singapore and South Korea, we observed an increase in transmissibility which highlighted a risk of potential resurgence of local transmission. Although the changes were not substantial, a potential rebound in transmissibility may have resulted from reintroduction of imported cases from other high-risk places, especially when many countries across the globe are experiencing outbreaks. Recent investigations have documented that lifting NPIs prematurely could lead to an earlier secondary peak [23]. Another study even suggested that maintaining NPIs for 18 months is necessary [2]. Nevertheless, sustaining aggressive NPIs over several months may not be feasible socially and economically. Our findings are in concurrence with another study [7], which indicated that close monitoring of disease transmissibility is recommended especially to allow public health officials to design strategies for relaxation of NPIs while keeping Rt below one for the resumption of economic activities.
The control of the pandemic of COVID-19 also requires a One Health approach to guard against the reintroduction of SARS CoV-2 into the human population. Infections of pets in Hong Kong [34] and outbreaks in mink farms [35] were successively reported indicating a potential a risk of SARS-CoV-2 infecting different animal species which could be potential reservoirs of infection for humans. A cross sectorial collaboration and multidisciplinary research and practice is required in a One Health approach in addressing the ongoing threats of emerging and reemerging infections arising from interconnectedness of human, animal and environmental health [30].
Using the CFR as an indicator of exhaustion of healthcare facilities, our estimates ranged from 0.09% to 1.59% among the WPR jurisdictions (except Japan) which were much lower than that in the United Kingdom, Belgium, Italy, France, and Netherlands where healthcare resources were overwhelmed resulting in CFR >10% [24]. Our estimates were also lower than those in Canada and the United States [25]. Compared with the CFR observed that ranged between 7% and 12% in the original epicentre of the pandemic, Wuhan [26,27], our estimates were lower although the CFR in Wuhan could be substantially lower if the clinically unobserved cases were taken into account [28]. Nevertheless, we acknowledged that CFR could vary by population composition (e.g. proportion of elderly in Japan is the highest in the world), ascertainment bias, and climatic conditions [25].
4.1. Limitations
There are some limitations in our study. First, our estimates were based on reported cases provided by official sources so the CFR may be subjected to underestimation from unreported deaths. As healthcare facilities in the studied jurisdictions were not overwhelmed, we believe the impact on the estimated CFR is rather limited when compared to other countries with more deaths outside hospital. Instead, as with many similar studies, we acknowledged that asymptomatic or mildly symptomatic unreported cases could affect the estimates we presented [29]. Under this circumstance, infection-fatality rate as an alternative severity measure is usually recommended [28], though a reconciliation of the full infection spectrum from mass serologic surveys is required. Second, compared with the European study [4], we chose not to pool information from all WPR jurisdictions at once to assess the independent effect size of each NPI. This was because of the inconsistent pattern of transmissibility across jurisdictions, different intensities of NPIs implemented and unconsolidated data source. Our investigation employed data up to the end of May when measures in some jurisdictions have not been relaxed yet. As more data become available, it will be possible to have a more conclusive understanding of the impact of NPIs relaxation.
5. Conclusions
Our retrospective study provided empirical evidence that the NPIs were able to reduce the transmissibility of COVID-19 in seven jurisdictions of the WPR. A comparatively lower CFR may reflect the health system capacity of these jurisdictions. While border control measures are necessary to reduce the potential of local outbreak seeded by imported cases, case finding by rapid tests and contact tracing along with other NPIs including stringent social distancing measures are required to prevent subsequent large cluster outbreaks in the community and transmissions from undetected cases. Moreover, due to the global circulation of COVID-19, relaxation of NPIs should be risk-assessed, monitored, and evaluated. A close monitoring of disease transmissibility is highly recommended in the relaxation phase to keep track of sustained disease transmission due to resumption of economic activities. Being among the first places that started the battle with the pandemic and entered the period of relaxation of social distancing, the seven jurisdictions in the study offered valuable lessons on the impact of NPIs to respond to resurgence of cases, although their implementation of NPIs differed, they were appropriate for their stage of transmission. This sheds light on when and how best to turn these “control levers” to prevent community transmission, so society can assume a new normalcy to life. To respond to global healthcare challenges from the COVID-19 pandemic, and guard against the reintroduction of SARS CoV-2, a One Health approach for the infectious disease control in a regional collaboration is critical.
Funding
This work was supported by Health and Medical Research Fund by the Food and Health Bureau, The Hong Kong Special Administrative Region [grant numbers COVID190105, INF-CUHK-1, 19181132]. The funder of the study had no role in study design, data collection, data analysis, data interpretation, writing of the manuscript, or the decision to submit for publication. All authors had full access to all the data in the study and were responsible for the decision to submit the manuscript for publication.
Data availability
All data are publicly available and can be downloaded from the official websites listed in the Appendix.
Declaration of Competing Interest
We declare no competing interests.
Acknowledgments
We would like to thank Shoki Kusaka, Sunghun Yun, Sanjay Rampal, Francisco TT Lai, Dong Dong, Tony Sun for their contributions and support in data collection, Shi Zhao in reviewing the methodology, Kirran Mohammad in editing the manuscript, and Emily Chan and Nina Gobat in reviewing the drafted manuscript. The Centre for Health Systems and Policy Research is funded by Tung Foundation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2021.100213.
Appendix A. Supplementary data
Supplementary material
References
- 1.World Health Organisation Coronavirus Disease 2019 (COVID¬19) Situation Report – 177. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200715-covid-19-sitrep-177.pdf?sfvrsn=b1a193f3_2
- 2.Chowdhury R., Heng K., Shawon M.S.R. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries. Eur. J. Epidemiol. 2020;35:389–399. doi: 10.1007/s10654-020-00649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kucharski A.J., Russell T.W., Diamond C. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect. Dis. 2020;20:553–558. doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaxman S., Mishra S., Gandy A. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020 doi: 10.1038/s41586-020-2405-7. published online June 8. [DOI] [PubMed] [Google Scholar]
- 5.Pan A., Liu L., Wang C. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323:1915. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cori A., Ferguson N.M., Fraser C., Cauchemez S. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am. J. Epidemiol. 2013;178:1505–1512. doi: 10.1093/aje/kwt133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung K., Wu J.T., Liu D., Leung G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020;395:1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson R.N., Stockwin J.E., van Gaalen R.D. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019;29:100356. doi: 10.1016/j.epidem.2019.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalili M., Karamouzian M., Nasiri N., Javadi S., Mirzazadeh A., Sharifi H. Epidemiological characteristics of COVID-19: a systematic review and meta-analysis. Epidemiol. Infect. 2020;148 doi: 10.1017/S0950268820001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen T., Wu D., Chen H. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bürkner P.C. Brms: an R package for Bayesian multilevel models using Stan. J. Stat. Softw. 2017;80:1–28. [Google Scholar]
- 12.Kucharski A.J., Althaus C.L. The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission. Euro Surveill. 2015;20:1–5. doi: 10.2807/1560-7917.es2015.20.25.21167. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd-Smith J.O., Schreiber S.J., Kopp P.E., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Endo A., Abbott S., Kucharski A.J., Funk S. Estimating the overdispersion in COVID-19 transmission using outbreak sizes outside China. Wellcome Open Res. 2020;5:67. doi: 10.12688/wellcomeopenres.15842.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chew M., Koh F.H., Wu J. Clinical assessment of COVID-19 outbreak among migrant workers residing in a large dormitory in Singapore. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.05.034. published online May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lai S., Ruktanonchai N.W., Zhou L. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020 doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J., Litvinova M., Liang Y. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chong K.C., Chung B., Zee Y. Modeling the impact of air, sea, and land travel restrictions supplemented by other interventions on the emergence of a new influenza pandemic virus. BMC Infect. Dis. 2012;12:309. doi: 10.1186/1471-2334-12-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mateus A.L.P., Otete H.E., Beck C.R., Dolan G.P., Nguyen-Van-Tam J.S. Effectiveness of travel restrictions in the rapid containment of human influenza: a systematic review. B World Health Organ. 2014;92:868–880. doi: 10.2471/BLT.14.135590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- 21.Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matrajt L., Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Dis. 2020;26:1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prem K., Liu Y., Russell T.W. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.John Hopkins University & Medicine Mortality Analyses. 2020. https://coronavirus.jhu.edu/data/mortality (5 August 2020, date last accessed)
- 25.Abdollahi E., Champredon D., Langley J.M., Galvani A.P., Moghadas S.M. Temporal estimates of case-fatality rate for COVID-19 outbreaks in Canada and the United States. CMAJ. 2020;192:E666–E670. doi: 10.1503/cmaj.200711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mizumoto K., Chowell G. Estimating risk for death from coronavirus disease, China, January-February 2020. Emerg. Infect. Dis. 2020;26:1251–1256. doi: 10.3201/eid2606.200233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng X., Yang J., Wang W. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa578. published online May 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu J.T., Leung K., Bushman M. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat. Med. 2020;26:506–510. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verity R., Okell L.C., Dorigatti I. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization . WHO; 2020. One Health.http://www.who.int/features/qa/one-health/en/ Accessed 21 December. [Google Scholar]
- 31.de Garine-Wichatitsky M., Binot A., Morand S., Kock R., Roger F., Wilcox B.A., Caron A. Will the COVID-19 crisis trigger a one health coming-of-age? Lancet Planet Health. 2020;4:e377–e378. doi: 10.1016/S2542-5196(20)30179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bonilla-Aldana D.K., Holguin-Rivera Y., Perez-Vargas S., Trejos-Mendoza A.E., Balbin-Ramon G.J., Dhama K., Barato P., Lujan-Vega C., Rodriguez-Morales A.J. Importance of the one health approach to study the SARS-CoV-2 in Latin America. One Health. 2020;10:100147. doi: 10.1016/j.onehlt.2020.100147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmiege D., Arredondo A.M., Ntajal J., Paris J.M., Savi M.K., Patel K., Yasobant S., Falkenberg T. One health in the context of coronavirus outbreaks: a systematic literature review. One Health. 2020;26:100170. doi: 10.1016/j.onehlt.2020.100170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong Kong Government . 2020. COVID-19 Dog Case Explained. https://www.news.gov.hk/eng/2020/03/20200304/20200304_212513_790.html. Accessed 21 December. [Google Scholar]
- 35.Koopmans M. SARS-CoV-2 and the human-animal interface: outbreaks on mink farms. Lancet Infect. Dis. 2020;21(1):18–19. doi: 10.1016/S1473-3099(20)30912-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
All data are publicly available and can be downloaded from the official websites listed in the Appendix.