Dear Editor,
Vitiligo is an acquired depigmentation disorder resulting from progressive destruction of epidermal melanocytes. Current therapeutic approaches include immunomodulation or immunosuppression therapy, antioxidant agents, phototherapy and melanocytes transplantation. 1 Repigmentation of the vitiligo lesions is often difficult to achieve; therefore, there is no treatment to ensure complete cure of this disease. Herein, we report that a 32‐year‐old stable vitiligo patient showed successful repigmentation treated with electrocautery needling.
A 32‐year‐old female patient presented with 2‐year history of vitiligo localized to bilateral breast. The patient had no systemic diseases or other family history of significance. Vitiligo lesions showed mild response to conventional therapies over the past 1 year, including topical halometasone, 0.1% tacrolimus and 308‐nm excimer light. Despite all this, the spread of vitiligo lesions ceased but without effect on repigmentation. Then, she presented to us for Chinese medicine treatment. Cutaneous examination revealed multiple scattered depigmented patches with sharply demarcated borders involving bilateral breast (Figure 1A,E). Routine blood test, serum alanine transaminase, serum aspartate aminotransferase, serum creatinine, urinalysis, stool test, thyroid function test and immunohistochemistry revealed no abnormalities.
FIGURE 1.
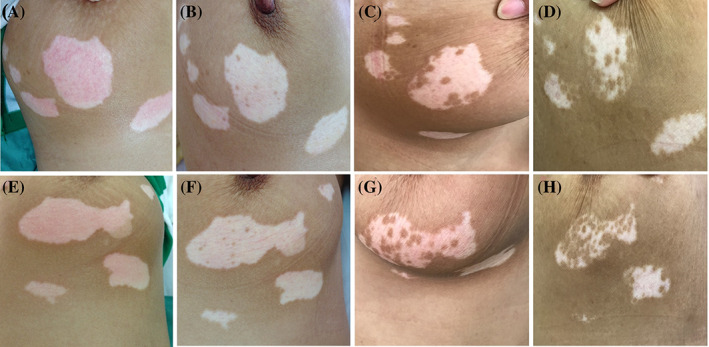
The patient presented with depigmented patches on bilateral breast (A‐D: right breast; E‐H: left breast) and treated with electrocautery needling technique. A, E, Depigmented patches on bilateral breast prior to therapy. B, F, Repigmentation of the lesions showing multiple small pigmented island in perifollicular pattern after 3 weeks of therapy. C, G, Thirty percent improvement of repigmentation after 3 months of therapy. D, H, Coalescence of multiple pigmentary islands leads to approximately 50% to 70% repigmentation at 1‐year follow‐up
The patient was treated with biweekly electrocautery needling therapy and the previous treatment was discontinued. The depigmented patches were anesthetized with local anesthetic 60 minutes prior to the procedure. It was performed biweekly using monopolar electrocautery device with minimum output power (1‐2 W). The vitiligo lesions were swiftly pricked to a superficial depth of approximately 1 mm until the lesions covered with pricking points spaced 3 to 5 mm apart. The patient felt burning sensation and pain during treatment; no blister, infection and systemic side effects developed at the end of the therapeutic course.
An initial regimentation of vitiligo lesions on bilateral breast was noticeable 3 weeks later due to the presence of repigmented islands in perifollicular pattern (Figure 1B,F). Within 3 months, further repigmentation progressed with significant improvement of 30% (Figure 1C,G). However, treatment was terminated as the patient moved to another city due to career change. The patient did not receive any treatment during this period and returned for follow‐up after 1 year. Despite termination of electrocautery needling therapy, vitiligo lesions showed continuous improvement in repigmentation; as a result, approximately 50% to 70% repigmentation of the lesion was achieved (Figure 1D,H).
Electrocautery needling technique is inspired by fire needle therapy which has been frequently used for vitiligo in traditional Chinese medicine. 2 Fire needle therapy uses hot‐red acupuncture needles heated by ethanol flame to perform superficial prick on vitiligo lesions. Whereas, electrocautery used electricity to generate heat in metal probe to superficially cauterized skin lesions, which mimics the effect of superficial prick caused by heat and mechanical injury from fire needling. Thus, electrocautery needling was demonstrated in this case.
Despite our patient had used conventional therapies such as topical corticosteroids, calcineurin inhibitors and 308‐nm excimer phototherapy, no repigmentation occurred. Whereas, electrocautery needling promoted rapid repigmentation, and repigmentation continued to occur although the treatment was terminated for 1 year. We speculated the induction of repigmentation was associated with heat and minor mechanical injury to the skin caused by electrocautery needling. The exact mechanism of this treatment had not been thoroughly studied. A study described that pigmentation after needling induced minimal epidermal damage 3 inciting melanocytes regeneration via Wnt signaling pathway during wound healing cascade. 4 The migration of melanoblast and melanocytes toward injury site had been observed under live imaging. 5 Furthermore, cytokines secreted during inflammatory phases in wound healing process stimulate migration of melanocytes from the pigmented area or boundary of vitiligo patches toward depigmented area. 6 Nevertheless, further studies are needed to elucidate the exact mechanism of electrocautery needling in repigmentation of vitiligo.
In conclusion, electrocautery needling could act as an adjuvant therapy to complement the conventional therapies in refractory vitiligo due to its high repigmentation rate, simple operating procedure and low therapeutic cost.
Informed consent and permission for publication of medical images was taken from the patient.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Lili Yang and Pui Mun Wong contributed to conception and wrote the manuscript with input from all authors, thus both are considered as co‐first authors. Lingli Yang and Ichiro Katayama designed the figure. Huali Wu analyzed the data. Huimin Zhang was involved in planning and supervised the project. All authors have read and agreed to the published version of the manuscript.
Lili Yang and Pui Mun Wong contributed equally to this work and should be considered co‐first authors.
Funding information High‐Level University Summit Project (Huimin Zhang, Summit Plateau Team); National Natural Science Foundation of China, Grant/Award Number: 81972932; Shanghai Municipal Health Committee Traditional Chinese Medicine Technology Promotion Project, Grant/Award Number: zyjx‐2017005; Three‐Year Action Plan to Further Speed Up the Development of Traditional Chinese Medicine in Shanghai, the Construction and Cultivation Project of Dominant Diseases of Traditional Chinese Medicine, Grant/Award Number: ZY(2018‐2020)‐ZYBZ‐10
REFERENCES
- 1. Bleuel R, Eberlein B. Therapeutic management of vitiligo. J Dtsch Dermatol Ges. 2018;16(11):1309‐1313. [DOI] [PubMed] [Google Scholar]
- 2. Wang T, Ren Y, Di D, Zhu Q, Luo G. Segmental vitiligo treated by fire needle therapy: a case series. Eur J Dermatol. 2018;28(1):118‐119. [DOI] [PubMed] [Google Scholar]
- 3. Iriarte C, Awosika O, Rengifo‐Pardo M, Ehrlich A. Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. 2017;10:289‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sun Q, Rabbani P, Takeo M, et al. Dissecting Wnt signaling for melanocyte regulation during wound healing. J Invest Dermatol. 2018;138(7):1591‐1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levesque M, Feng Y, Jones RA, Martin P. Inflammation drives wound hyperpigmentation in zebrafish by recruiting pigment cells to sites of tissue damage. Dis Model Mech. 2013;6(2):508‐515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zawar VP, Karad GM. Needling in unresponsive stable vitiligo. J Am Acad Dermatol. 2016;75(5):e199‐e200. [DOI] [PubMed] [Google Scholar]


