Abstract
Background and Objectives:
Opioid-related overdose deaths in North America have increased drastically, partially due to the increased prevalence of illicitly manufactured fentanyl. The current study sought to assess the prevalence and intentionality of fentanyl use among individuals with opioid use disorder (OUD).
Methods:
For this secondary analysis (Study1) we screened a total of 1,118 urine samples from 316 participants with OUD from 2016–2019. Fentanyl knowledge and intentionality of use were assessed in a separate OUD sample (Study 2; N=33).
Results:
In Study 1, 34.6% of all urine samples tested positive for fentanyl. Overall, 149 participants (47.2%) provided ≥1 urine sample that tested fentanyl-positive, and 93 (29.4%) provided ≥2 fentanyl-positive samples. The number of fentanyl-positive samples, relative to the number of samples tested each year, increased by 330% from year 1–3. Study 2 found all participants had pre-existing knowledge that drugs may be adulterated with fentanyl, yet 67% were surprised by their own fentanyl-positive test result.
Discussion and Conclusions:
Like previous studies, our data indicate the high prevalence of fentanyl exposure and low perception of fentanyl-related risk among individuals with OUD, respectively, suggesting that opioid overdose harm reduction efforts may need to focus more on drug users’ understanding of risks related to fentanyl use and adulteration of drugs.
Scientific Significance:
The current studies provide longitudinal data on fentanyl exposure prevalence and risk perception that is uniquely granular by assessing OUD treatment status, and by identifying potential associations between fentanyl exposure with the presence of other drug use and non-fatal overdose.
INTRODUCTION
Initially fueled by the widespread availability of prescription opioids in the mid-1990s, followed by a dramatic rise in heroin-related overdose mortalities in the mid-2000s, the U.S. overdose epidemic has again evolved with the widespread availability of illicitly manufactured fentanyl and its analogs.1–3 Fentanyl is a highly efficacious mu-opioid receptor (MOR) agonist, estimated to be 50–100 times more potent than morphine, with some analogs, like carfentanil, estimated to be 10,000 times more potent.4 Preclinical and clinical studies have yet to provide a definitive consensus on fentanyl’s abuse liability compared to other opioids, but the available data suggest a high potential for non-medical use in humans.4 Given its potency and increasing availability, illicitly manufactured fentanyl has contributed to an evolving and increasingly lethal opioid epidemic.4
Since 2013, the availability of illicitly manufactured fentanyl in the U.S. illicit drug market has grown exponentially.5,6 Data from the Drug Enforcement Agency’s (DEA) National Forensic Laboratory Information Service (NFLIS) has shown an over 1000% increase in fentanyl reported in drug seizures from 2014 (N = 5,531 reports) to 2017 (N = 56,530).7 During this same period of time, overdose-related mortalities also saw a rapid rise. In 2016, the Center for Disease Control (CDC) estimated a 21% increase in drug overdose-related mortalities from 2015, resulting in over 60,000 deaths in the U.S.8 The CDC reported deaths attributed to synthetic opioids (i.e., fentanyl) exponentially increased from July–December 2016 as fentanyl was detected in 56% of 5,152 opioid overdose deaths in 10 states, with an additional 14% of the samples testing positive for fentanyl analogs (e.g., carfentanil).9 Contributing to this picture, data from the National Vital Statistics System—Mortality (NVSS–M) multiple cause-of-death files suggest an increase in drug overdose deaths involving fentanyl from 1,663 in 2011 to 18,335 in 2016, with the greatest increases occurring on the East Coast and in the Upper Midwest regions of the U.S.10,11 In 2017, the New York City Department of Health and Mental Hygiene (NYC DOHMH) reported the highest number of overdose deaths (1,487) since 2000, with the percentage of overdose fatalities involving fentanyl increasing from 2% in 2012 to 57% in 2017.12 Provisional data from the CDC indicates that deaths due to fentanyl continue to rise with 32,299 deaths attributed to synthetic opioids in the 12-month period through June of 2019; an 8.3% increase from the 12 months prior.13 Taken together, these data demonstrate the major role of fentanyl in the ongoing overdose epidemic.
Compounding the epidemic of opioid-related overdose deaths, overdose deaths involving cocaine and other psychostimulants have also significantly increased in the U.S. (by 42.4% from 12,122 in 2015 to 17,258 in 2016),14 despite persistent decreases in overall cocaine use.15 Adulteration of cocaine with fentanyl appears to be a contributing factor to this complicated picture.16 A cross-sectional study using nationally representative urine drug test data found that between 2013 and 2019 positivity rates for non-prescribed fentanyl among cocaine-positive samples increased by 1850%, and by 798% among methamphetamine-positive samples.17 Of note, it cannot be concluded from these data that the increase in fentanyl positivity is due to adulteration rather than use of separate drugs. However, the annual percent change in death rates involving psychostimulants with and without opioids are both on the rise.18
Despite the rapid rise in fentanyl prevalence over the past decade, knowledge of fentanyl among individuals who use opioids, their perception of the related risks, as well as the intentionality of fentanyl use, remain poorly understood.19 Several recent studies indicate reasonable knowledge of fentanyl risks among individuals who use opioids, but lower attribution of personal risk. A Canadian study found nearly 94% of individuals who use illicit substances (heroin, stimulants, prescription opioids, and cannabis) knew the risks associated with fentanyl but 73% of all individuals who use any substance and 60% of individuals who use opioids perceived their own risk of fentanyl-related overdose as low or non-existent.20 Among individuals who use heroin daily, who may be perceived as the highest risk group for unintentional fentanyl exposure, 17% perceived themselves as being at no-to-low risk for fentanyl-related overdose. Another study compared fentanyl beliefs, behaviors, and risk perceptions among patients undergoing short-term inpatient opioid withdrawal management in Massachusetts.21 Almost all patients reported being aware of fentanyl risks, and 87% tested positive for fentanyl. Yet, around 18% of those who tested positive were sure that they had never been exposed to fentanyl and that their test would be negative.
Given the increased adulteration of heroin and cocaine with fentanyl and its implications for overdose risks, extended and improved overdose prevention strategies are needed. A greater understanding of the co-use of illicit fentanyl, opioids, and cocaine, as well as intentional fentanyl use and self-perceived risk, is necessary to adapt and improve existing interventions to reduce overdose mortality. The current study, conducted in NYC, aimed to contribute to this goal by using urine toxicology (Utox) screens from individuals with current Opioid Use Disorder (OUD), who completed assessments over 12 months (Study 1). Study 2 assessed self-reported knowledge about fentanyl and intentionality of use from a separate sample of individuals with OUD. As the vast majority of the available national and regional reports on the prevalence of illicit fentanyl rely on post-mortem data from poorly defined populations (e.g., it is unclear whether individuals had OUD), this secondary analysis provides unique data examining the prevalence and intentionality of fentanyl use from a longitudinal perspective in a large sample of both treatment-seeking and non-treatment seeking individuals with clinically confirmed OUD in the largest U.S. metropolitan area, collected during the time period with the most notable increase in the availability of illicitly manufactured fentanyl in the U.S. (2016–2019).
METHOD
The NYSPI Institutional Review Board approved all study procedures (including screening and fentanyl warning procedures) and informed consent was obtained from all participants.
Study 1: Urine Toxicology Data
This is a secondary analysis of data collected as part of a clinical trial that sought to understand the risks and benefits of overdose education and naloxone distribution (OEND) (ClinicalTrials.gov Identifier: NCT02535494). Enrollment at the New York State Psychiatric Institute (NYSPI)/Columbia University Irving Medical Center (CUIMC) began in October 2014 and urine testing for fentanyl was first initiated in August 2016. Thus data for the current analysis include 39 months of the larger study (observation period August 2016 to October 2019). Each participant was followed for 12-months. For more details of the study and study-related procedures see Jones et al., 2017.22
Potential participants were recruited from harm reduction centers, hospitals and through advertisements in local newspapers. Following a telephone screen, in-person screening procedures were conducted at the Division on Substance Use Disorders at NYSPI/CUIMC. Participants were aged 21 to 65 years, had met DSM-IV criteria for OUD within the past 6 months, and were in otherwise good mental health. DSM-IV criteria were used throughout the 5-year study as DSM-5 was not in use yet when the original trial was started. Individuals could be non-treatment seeking or enrolled in agonist maintenance treatment for OUD to be included in the study. Treatment status was determined based on an array of clinical assessments, and participants were defined as being “In Treatment” if they were prescribed a medication to treat opioid use disorder (MOUD). Participants were excluded if they had an active psychiatric disorder that might have interfered with participation or made participation hazardous for them or study staff (e.g., DSM-IV psychotic disorder, active bipolar disorder with mania, or significant history of violent behavior).
Urine Drug Testing & Self-reported Overdose Events
Participants completed a urine drug toxicology (Utox) at each visit over the 12-month study (Baseline, 1-, 3-, 6-, and 12-months). An 11-panel drug urine dipstick test assessed for recent use of: amphetamine, barbiturate, benzodiazepine, buprenorphine, cocaine, methamphetamine, methadone, opiates (e.g., morphine, hydrocodone, dihydrocodeine, codeine, 6-acetylmorphine, and hydromorphone), oxycodone, phencyclidine (PCP), and tetrahydrocannabinol (THC: Alltests North America®). An individual dipstick test was used for fentanyl/norfentanyl (American Screening LLC; see Table 1 for cut-off values). Urine collection was typically unobserved, however, in rare cases, research assistants observed sample collection from participants who were suspected of providing samples that were either manipulated or not their own. All participants were made aware that their Utox results would not impact their participation in the main OEND trial. According to standard laboratory procedures, all urine samples were tested immediately after being obtained.
Table 1.
Urine toxicology cut-off values for each substance (ng/mL)
| Drug | Cut-off (ng/mL) |
|---|---|
| Amphetaminea | 1000 |
| Barbituratea | 300 |
| Benzodiazepinea | 300 |
| Buprenorphinea | 10 |
| Cocainea | 300 |
| Methamphetaminea | 1000 |
| Methadonea | 300 |
| Opiatesa | 300 |
| Oxycodonea | 100 |
| Phencyclidine (PCP)a | 300 |
| Tetrahydrocannabinol (THC)a | 50 |
| Fentanyl/ /Norfentanylb | 200 |
11-panel drug urine dipstick test obtained from Alltests North America®
Fentanyl urine dipstick test obtained from American Screening LLC
Study staff inquired about overdose events (self-experienced and witnessed) in the preceding time period at each visit, using an overdose tracking form provided by the NYC DOHMH. Participants were also encouraged to contact study staff immediately if they experienced (or witnessed) an overdose. For the current analysis, we included reports on self-experienced overdose events only.
Study 2: Fentanyl Knowledge & Intentionality of Use
In August 2018, the Division on Substance Use Disorders recommended a warning be provided to all participants who tested positive for fentanyl. Participants were informed about the risks involved with fentanyl ingestion and harm-reduction strategies to mitigate fentanyl-overdose risk. We additionally asked a sample of participants who received a fentanyl warning about their previous knowledge of fentanyl and intentional use of fentanyl or fentanyl-adulterated heroin (Study 2, N = 33). While participants might have received multiple warnings – in case they provided multiple fentanyl positive samples – knowledge and intentionality data were only collected after the first warning. Self-reports on fentanyl knowledge and intentionality of use were derived from different participants than those included in Study 1. Nonetheless, the Study 2 sample met the same inclusion and exclusion criteria as the Study 1 sample, which is why the investigators decided to present these cross-sectional data here as a complementary sources of information on fentanyl risk and exposure.
Data Analysis
Continuous and categorical demographic variables, Utox, and self-report data were summarized descriptively. Comparisons based on sex and treatment status (participants receiving MOUD and non-treatment seekers) were conducted using multivariate analysis of variance (MANOVA), with positive Utox for any substance (excluding methadone and buprenorphine), fentanyl, cocaine, and opiates as dependent variables. Missing Utox samples were treated as missing (not as positive Utox screens). The significance criterion was α=0.05. Statistical analyses were performed using SPSS® version 18.
RESULTS
Study 1: Urine Toxicology Data
During the 39-month observation period, 1,118 urine samples from 316 participants were tested. Participants were predominantly male (78.8%) and had a mean age at baseline of 47.3 years (SD = 9.6). The majority of participants were Black/African-American (47.5%), 27.9% were Hispanic/Latino, 17.0% were White/Caucasian, and 5.6% self-identified as multi-racial. At baseline, participants had been using heroin for an average of 15.7 years (SD = 11.5). Participants spent an average of $34.10/day on heroin (SD = $43.00), which in the region costs ~$0.99 per mg.23 At baseline, approximately half of participants were not seeking treatment (48.7%), 39.5% received MOUD, and 11.8% had recently undergone opioid detoxification.
Of all urine samples tested for fentanyl (N = 1,118), 387 (34.6%) tested positive for fentanyl. Overall, 149 participants (47.2%) provided at least one urine sample that was fentanyl-positive, and 93 (29.4%) provided two or more fentanyl-positive samples. Figure 1 illustrates urine samples positive for any substance, fentanyl, opiates, and cocaine as a percentage of all urine samples tested throughout the 39-month observation period. The number of urine samples positive for fentanyl relative to the number of urine samples tested each year increased by 330% from year 1 to year 3 of observation. A similar trend was observed for cocaine-positive urine samples, with an overall increase of 391% from year 1 to year 3. Urine samples positive for opiates increased by 26% from year 1 to year 3.
Figure 1.
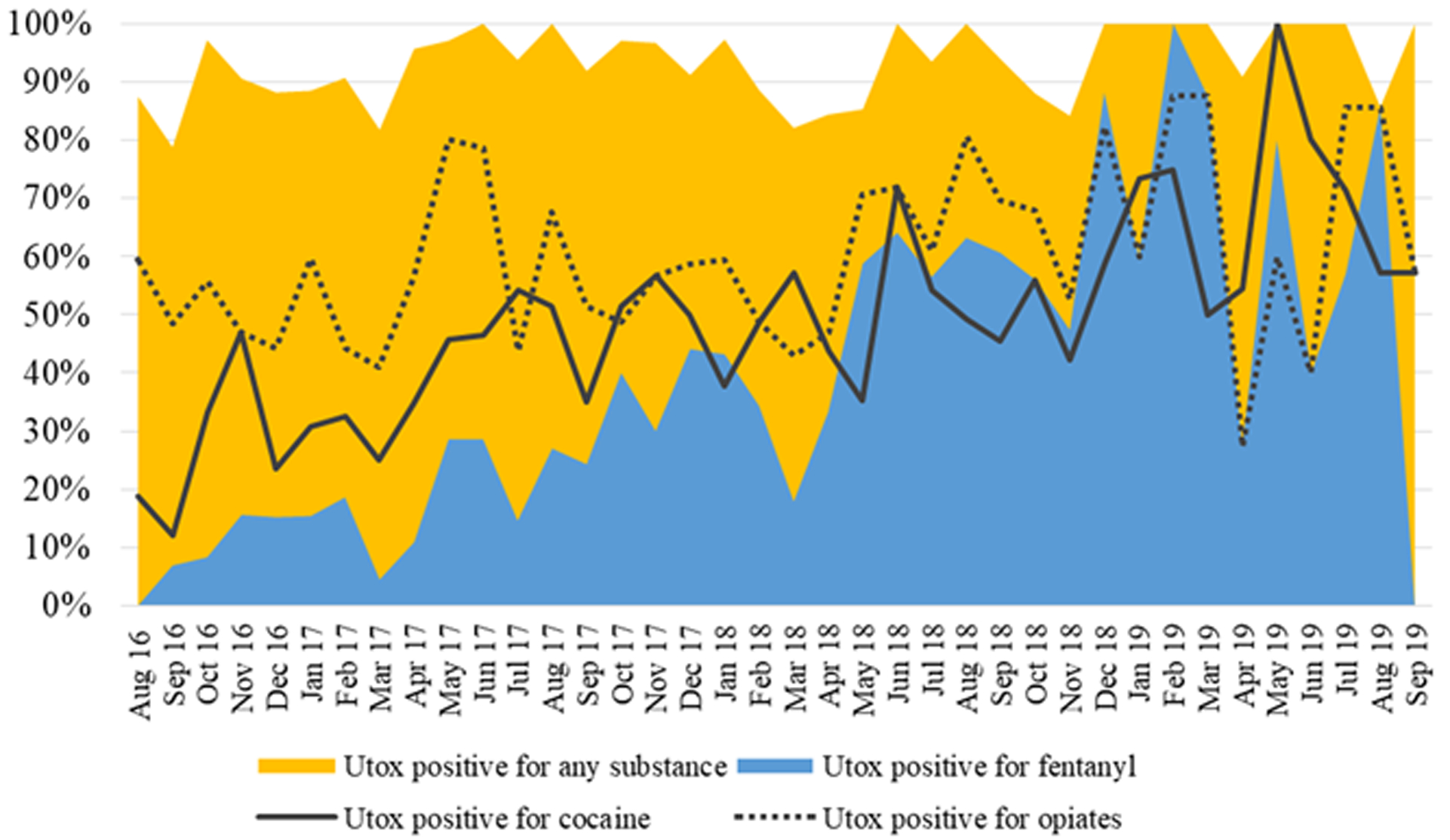
Urine samples positive for any substance1 (yellow area), fentanyl (blue area), opiates (dotted line), and cocaine (solid line) in percent of all urine samples tested over the course of the observation period (August 2016 to October 2019)
1Amphetamine, barbiturate, benzodiazepine, buprenorphine, cocaine, methamphetamine, methadone, morphine, oxycodone, phencyclidine, tetrahydrocannabinol, fentanyl
Among the drugs detected in all urine samples, opiates were the most common (59.1%) along with cocaine (44.3%). As almost half of our participants were receiving MOUD, methadone (44.9%) was also frequently detected. Fentanyl-positive urine samples most frequently contained opiates (93.8% of all fentanyl-positive samples), followed by cocaine (53.7%) and methadone (45.5%; see Figure 2). Overall, 167 fentanyl-positive samples contained opiates but not cocaine, 12 contained cocaine but not opiates, another 12 fentanyl-positive samples contained neither cocaine nor opiates, and two urine samples tested positive exclusively for fentanyl. There was no statistically significant difference between women and men on the combined dependent variables [positive Utox for any substance (excluding methadone and buprenorphine), fentanyl, cocaine, and opiates], F(4,296) = 0.51, p = .728, Wilks’ Λ = .993, partial η2 = .007, and no significant between subjects effects.
Figure 2.
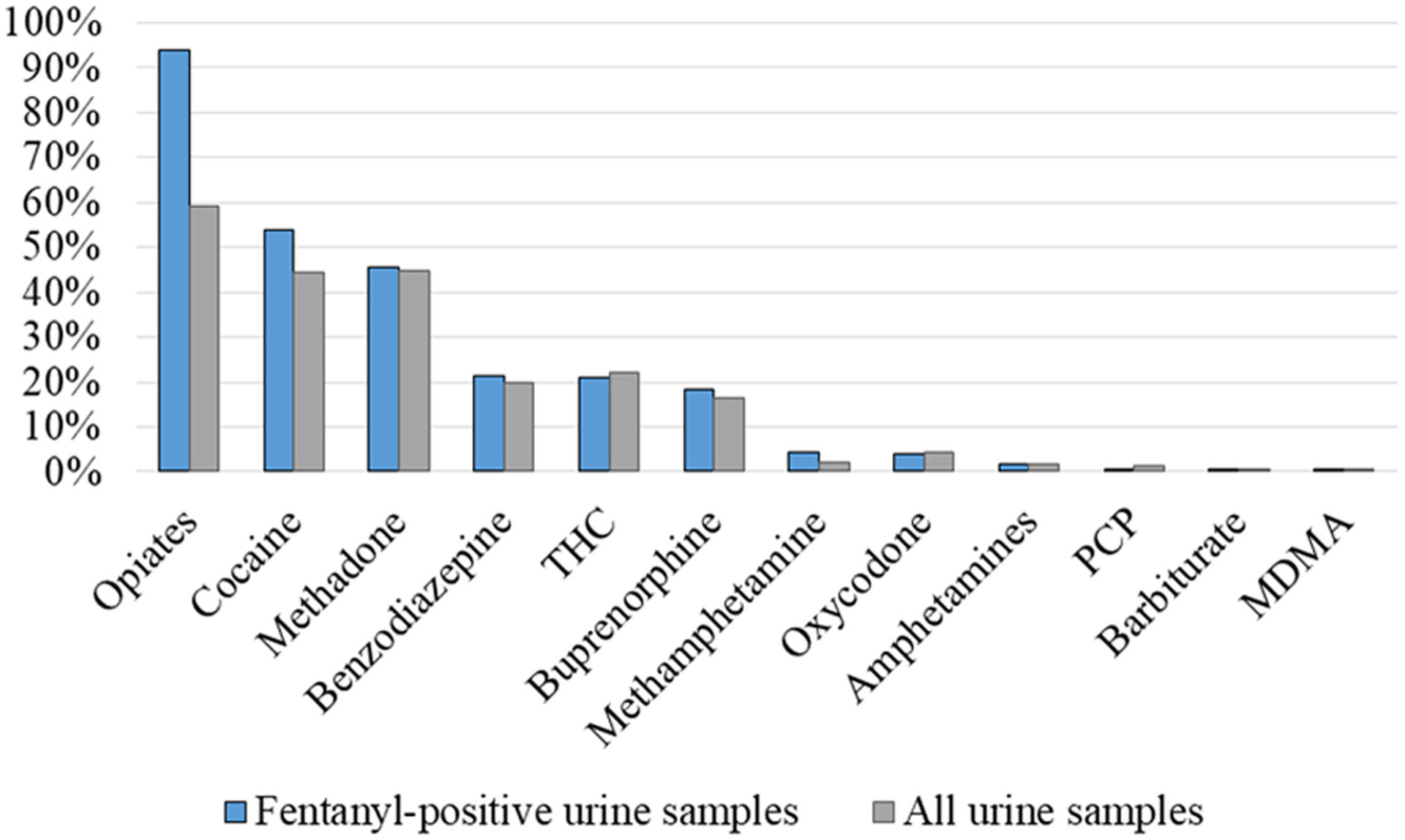
Substances detected in all urine samples (N = 1,143, grey bars) and in fentanyl-positive urine samples (N = 387, blue bars)
PCP: Phencyclidine; THC: Tetrahydrocannabinol; MDMA: Methylenedioxymethamphetamine
There was no statistically significant difference between participants who were non-treatment seeking at baseline and those receiving MOUD on the combined dependent variables [positive Utox for any substance (excluding methadone and buprenorphine), fentanyl, cocaine, and opiates], F(4,255) = 2.05, p = .088, Wilks’ Λ = .969, partial η2 = .031. However, tests of between-subjects effects indicated that participants who received MOUD at baseline had fewer opiate-positive Utox screens, F(4,258) = 4.61, p = .033, as well as fewer fentanyl-positive Utox screens, F(1,258) = 5.34, p = .022.
Of all participants included in Study 1, 26 (8.2%) indicated that they experienced a non-fatal drug overdose while being enrolled in the study. The vast majority of these participants (N = 23; 88.5%) provided at least one urine sample that tested positive for fentanyl, 15 (57.7%) provided more than one, and 13 (50.0%) provided more than two fentanyl-positive samples.
Study 2: Fentanyl Knowledge & Intentionality of Use
Overall, 33 participants (12.1% female) who tested positive for fentanyl completed the self-report questionnaire, collected between August 2018 and December 2019. Participants were predominantly male (87.9%) and aged 45.9 years (SD = 9.7). More than one-third of participants were Black/African-American (36.4%), 21.2% were White/Caucasian, 15.2% Hispanic, and 27.3% self-identified as multi-racial or as another ethnic/racial group. Most participants (66.7%) reported that they were surprised by the fact that their urine sample tested positive for fentanyl. All participants indicated that they had previous knowledge of the risk that heroin and other drugs may be adulterated with fentanyl. The majority of participants reported that they had heard about fentanyl in the news (N = 13) or in “the streets” (N = 9). Another frequent source of information were friends or relatives (N = 8). Others had heard about fentanyl in a treatment program (N = 1) or from their dealer (N = 1), and one participant did not remember where s/he learned about fentanyl. Seven participants (21.2%) affirmed that they had intentionally sought out fentanyl, all of whom implicated the strength or potency of fentanyl as the primary motivator for doing so.
DISCUSSION
Our findings demonstrate the increasing frequency of fentanyl exposures among individuals with OUD in NYC from 2016 to 2019. This study replicates other findings from this region12 and our results are consistent with trends across North America.7,24 Fentanyl was detected in more than a third of the specimens collected in the current study, with men and women at similar risk of fentanyl exposure. Additionally, there was a marked increase of over 300% in fentanyl-positive urine samples from year 1 (2016) to year 3 (2019) of observation. While “opiates” were the most common substance detected in fentanyl-positive samples (most likely the result of heroin use, based on self-report during clinical interviews and assessments), more than half also contained cocaine. Furthermore, there was a similar increase in cocaine and fentanyl positivity among our sample over time. The increase in cocaine-positive urine samples coincides with reports of a dramatic rise in the supply of cocaine due to increases in cultivation after 2015.25
Our data provide further evidence of the proliferation of illicitly manufactured fentanyl in the NYC drug market, which appears to be largely through the adulteration of both heroin and cocaine.5,6,16 National and regional reports show an increasing involvement of fentanyl in overdose deaths.8–11 While we do not know if fentanyl was involved in the overdose events reported in the current study, almost all participants who had experienced a non-fatal overdose provided at least one fentanyl-positive urine sample (89%). Concerningly, nearly a fifth of all Utox screens were also positive for benzodiazepines, which can further increase opioid overdose risk.26
Improving access to MOUD is a key focus of the National Institutes of Health and U.S. Department of Health and Human Services.27 Our results support this effort by showing that participants receiving MOUD at baseline were less likely to provide a urine sample positive for fentanyl than those who were not seeking treatment. Although treatment status was determined at baseline, for many participants status may have changed over the 1-year follow-up period as OUD often involves cycles of relapse and remission.28 While no definitive conclusions can be drawn based on this secondary data analysis, the protective effect of MOUD against fentanyl exposure may be more pronounced when continuous enrollment in treatment is ensured. In addition, overdose-harm reduction strategies, including OEND, traditionally target people who use opioids. However, more than half of all fentanyl-positive samples also contained cocaine, which indicates a potential need to broaden harm reduction messaging and services to people who use psychostimulants. Of note, the majority of individuals in our sample who tested positive for cocaine also tested positive for opiates, and thus we cannot retrace the source of fentanyl adulteration.
The results of Study 2 suggest that individuals with OUD in NYC have basic knowledge of fentanyl. While a previous study found that 13% of participants did not know anything about fentanyl,29 it is to be expected that individuals who use drugs become more aware of fentanyl over time as its prevalence increases. Furthermore, public health campaigns in NYC and elsewhere increasingly focus on the dangers of fentanyl.30 Yet, our participants’ general knowledge of fentanyl and its related risks did not directly translate to awareness of their own exposure risk. Over two-thirds of the Study 2 sample were surprised by their fentanyl-positive test result, consistent with results from earlier studies.20,29 Presenting individuals who use opioids with Utox-based evidence that their drug supply contains fentanyl may help close the gap between their general knowledge about fentanyl-related risks and the risk they perceive for themselves. In addition, this might present a window of opportunity to discuss harm-reduction strategies and/or the initiation of longer-term interventions such as MOUD. Another approach to raise awareness of the risk of fentanyl exposure prior to consumption may be provision of rapid, at-home fentanyl test strips.32,33 However, the existing research on this novel harm reduction approach is limited to acceptability studies;34,35 we do not yet know if and how at-home fentanyl testing may change drug use behavior.
The majority of participants in Study 2 did not endorse actively seeking fentanyl. While the presented findings contribute to our growing understanding of the intentionality of fentanyl use and the knowledge of related risks among individuals with OUD,29,21 it needs to be noted that the present results are based on a small sample. Qualitative investigations have provided some insight into fentanyl-seeking motivations, including fentanyl’s ability to overcome heroin tolerance,29,36–38 which were similar to those cited in the current investigation.
The current analysis provides unique data on the prevalence of fentanyl in a large sample of both treatment and non-treatment seeking individuals with OUD from NYC, collected during the time period with the greatest increase in illicitly manufactured fentanyl on the U.S. illicit drug market. Our use of a urine dipstick test did not permit detection of fentanyl’s numerous analogs. Additionally, at the time, there were limited options for fentanyl dipstick tests, and the test we used is less sensitive than those more recently available.39 In combination with the rapid clearance of fentanyl by the kidneys, the current study likely underestimates the prevalence of fentanyl and its analogs. Another limitation is that the Study 1 sample was composed of individuals with OUD who were willing and able to participate in a 1-year study. As such, the sample may differ from individuals presenting acutely to an outpatient clinic or emergency department with opioid overdose or withdrawal. Furthermore, self-reported fentanyl knowledge and intentionality of use (Study 2) were only available from a separate sample of individuals with OUD but not from participants who provided urine samples for the prospective trial. Additionally, due to potential reporting bias (i.e., socially desirable reporting) participants’ knowledge about fentanyl and intentionality of use could have been misreported. Nonetheless, our results may have important implications for overdose harm reduction approaches by emphasizing the high prevalence of fentanyl exposure among individuals with OUD, in addition to lower perception of their own individual risk. This implies that providing information about the proliferation of fentanyl and its risks is likely not sufficient to change risky drug use behavior.
Finally, from the current data we cannot determine if the increasing prevalence of fentanyl among our sample is the result of increasing fentanyl adulteration of heroin or psychostimulant drugs. Nonetheless, given the evidence of increasing fentanyl adulteration of the psychostimulant drugs supply,17 the field should focus on ways to reduce opioid overdose risk (i.e., naloxone distribution, and promotion of harm reduction strategies such as not using drug alone and – wherever possible - observed consumption sites) among individuals who use psychostimulants in addition to those who use opioids.
Acknowledgments
The authors would like to thank all research volunteers for participating in the study; and, Jeanne Manubay, MD, Gregory Cortorreal BA, Nicholas Allwood BA, Benjamin Foote BA, Claudia Tindall, NP, Ida Holt, RN and Janet Murray, RN for their technical assistance on the trial.
Funding Source
This work was supported by the National Institute on Drug Abuse of the National Institutes of Health [Grant R01DA035207] to Dr. Sandra Comer. Laura Brandt is funded by an Erwin Schroedinger Fellowship by the Austrian Science Fund (ASF).
Footnotes
Declaration of Interest
Within the past three years Dr. Jones received compensation (in the form of partial salary support) from a study partially supported by Cerecor Inc. Within the past three years, Dr. Comer has received research funding from Alkermes, Braeburn Pharmaceuticals, Cerecor Inc., Corbus, Go Medical, Intra-cellular Therapies, and Lyndra. In addition, Dr. Comer has also consulted for: Alkermes, Charleston Labs, Clinilabs, Collegium, Daiichi Sankyo, Depomed, Egalet, Endo, Epiodyne, Inspirion Delivery Sciences, Janssen, KemPharm, Mallinckrodt, Nektar, Neurolixis, Newron, Opiant, Otsuka, Pfizer, and Sun Pharma. She also has received honoraria from the World Health Organization. The other authors (SM, LB, AC, RA) have no conflicts to report.
References
- 1.Alexander MJ, Kiang MV., Barbieri M. Trends in Black and White Opioid Mortality in the United States, 1979–2015. Epidemiology. 2018;29(5):707–715. doi: 10.1097/EDE.0000000000000858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unick GJ, Ciccarone D. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int J Drug Policy. 2017;46:112–119. doi: 10.1016/j.drugpo.2017.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paulozzi LJ. Opioid Analgesic Involvement in Drug Abuse Deaths in American Metropolitan Areas. Am J Public Health. 2006;96(10):1755–1757. doi: 10.2105/AJPH.2005.071647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comer SD, Cahill CM. Fentanyl: Receptor pharmacology, abuse potential, and implications for treatment. Neurosci Biobehav Rev. 2019;106:49–57. doi: 10.1016/j.neubiorev.2018.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ciccarone D Editorial for “US heroin in transition: Supply changes, fentanyl adulteration, and consequences” IJDP special section. Int J Drug Policy. Published online 2017. doi: 10.1016/j.cogdev.2010.08.003.Personal [DOI] [Google Scholar]
- 6.Gladden RM, Martinez P, Seth P. Fentanyl Law Enforcement Submissions and Increases in Synthetic Opioid–Involved Overdose Deaths — 27 States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837–843. doi: 10.15585/mmwr.mm6533a2 [DOI] [PubMed] [Google Scholar]
- 7.National Forensics Laboratory Information Service. Tracking Fentanyl and Fentanyl-Related Substances Reported in NFLIS-Drug by State, 2016–2017. Published 2019. Accessed July 13, 2020 https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/NFLISDrugSpecialRelease-Fentanyl-FentanylSubstancesStateMaps-2016-2017.pdf
- 8.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152). doi: 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths Involving Fentanyl, Fentanyl Analogs, and U-47700 — 10 States, July–December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197–1202. doi: 10.15585/mmwr.mm6643e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell D, Noonan RK, Houry D. Underlying Factors in Drug Overdose Deaths. JAMA. 2017;318(23):2295. doi: 10.1001/jama.2017.15971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H. Drug overdose deaths involving fentanyl, 2011–2016 National Vital Statistics Reports; vol 68 no 3 Hyattsville, MD: National Center for Health Statistics; 2019. [PubMed] [Google Scholar]
- 12.Colon-Berezin C, Nolan ML, Blachman-Forshay J, Paone D. Overdose Deaths Involving Fentanyl and Fentanyl Analogs — New York City, 2000–2017. MMWR Morb Mortal Wkly Rep. 2019;68(2):37–40. doi: 10.15585/mmwr.mm6802a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention & National Center for Health Statistics. Provisional Drug Overdose Death Counts. Published 2020. Accessed February 3, 2020 https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 14.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential — United States, 2003–2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388–395. doi: 10.15585/mmwr.mm6817a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCall Jones C, Baldwin GT, Compton WM. Recent Increases in Cocaine-Related Overdose Deaths and the Role of Opioids. Am J Public Health. 2017;107(3):430–432. doi: 10.2105/AJPH.2016.303627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Busardò FP, Pichini S, Pacifici R, Karch SB. The Never-Ending Public Health Issue of Adulterants in Abused Drugs. J Anal Toxicol. 2016;40(7):561–562. doi: 10.1093/jat/bkw051 [DOI] [PubMed] [Google Scholar]
- 17.LaRue L, Twillman RK, Dawson E, et al. Rate of Fentanyl Positivity Among Urine Drug Test Results Positive for Cocaine or Methamphetamine. JAMA Netw Open. 2019;2(4):e192851. doi: 10.1001/jamanetworkopen.2019.2851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoots B, Vivolo‐Kantor A, Seth P. The rise in non‐fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction. 2020;115(5):946–958. doi: 10.1111/add.14878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cicero TJ, Ellis MS, Kasper ZA. Increases in self-reported fentanyl use among a population entering drug treatment: The need for systematic surveillance of illicitly manufactured opioids. Drug Alcohol Depend. 2017;177:101–103. doi: 10.1016/j.drugalcdep.2017.04.004 [DOI] [PubMed] [Google Scholar]
- 20.Moallef S, Nosova E, Milloy MJ, et al. Knowledge of Fentanyl and Perceived Risk of Overdose Among Persons Who Use Drugs in Vancouver, Canada. Public Health Rep. 2019;134(4):423–431. doi: 10.1177/0033354919857084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD. Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J Subst Abuse Treat. 2018;86:65–69. doi: 10.1016/j.jsat.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones JD, Campbell A, Metz VE, Comer SD. No evidence of compensatory drug use risk behavior among heroin users after receiving take-home naloxone. Addict Behav. 2017;71:104–106. doi: 10.1016/j.addbeh.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drug Enforcement Administration. 2016 Heroin Domestic Monitor Program. Published 2018. Accessed July 13, 2020 https://www.dea.gov/sites/default/files/2018-10/HeroinDomesticMonitorReportDEA-GOVFINAL.pdf [Google Scholar]
- 24.Karamouzian M, Papamihali K, Graham B, et al. Known fentanyl use among clients of harm reduction sites in British Columbia, Canada. Int J Drug Policy. 2020;77:102665. doi: 10.1016/j.drugpo.2020.102665 [DOI] [PubMed] [Google Scholar]
- 25.Maxwell JC. Is Cocaine Coming Back? A Commentary. Subst Use Misuse. Published online 2020. doi: 10.1080/10826084.2019.1664592 [DOI] [PubMed] [Google Scholar]
- 26.Jones JD, Mogali S, Comer SD. Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125(1–2):8–18. doi: 10.1016/j.drugalcdep.2012.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute on Drug Abuse. Opioid Overdose Crisis. Published 2020. Accessed July 13, 2020 https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis
- 28.Fleury M-J, Djouini A, Huỳnh C, et al. Remission from substance use disorders: A systematic review and meta-analysis. Drug Alcohol Depend. 2016;168:293–306. doi: 10.1016/j.drugalcdep.2016.08.625 [DOI] [PubMed] [Google Scholar]
- 29.Arfken CL, Suchanek J, Greenwald MK. Characterizing fentanyl use in methadone-maintained clients. J Subst Abuse Treat. 2017;75:17–21. doi: 10.1016/j.jsat.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 30.New York State Department of Health. Opioid Prevention Program : Data to Action Fentanyl-related deaths in New York State outside of New York City , 2015–2017 Fentanyl with Other Substances. Published 2019. Accessed July 13, 2020 https://www.health.ny.gov/statistics/opioid/data/pdf/nysdoh_dta1_fentanyl.pdf
- 31.NYC Health. Fentanyl. Published 2019. Accessed July 13, 2020 https://www1.nyc.gov/site/doh/health/health-topics/fentanyl.page
- 32.Goldman JE, Waye KM, Periera KA, Krieger MS, Yedinak JL, Marshall BDL. Perspectives on rapid fentanyl test strips as a harm reduction practice among young adults who use drugs: a qualitative study. Harm Reduct J. 2019;16(1):3. doi: 10.1186/s12954-018-0276-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McGowan CR, Harris M, Platt L, Hope V, Rhodes T. Fentanyl self-testing outside supervised injection settings to prevent opioid overdose: Do we know enough to promote it? Int J Drug Policy. 2018;58:31–36. doi: 10.1016/j.drugpo.2018.04.017 [DOI] [PubMed] [Google Scholar]
- 34.Krieger MS, Goedel WC, Buxton JA, et al. Use of rapid fentanyl test strips among young adults who use drugs. Int J Drug Policy. 2018;61:52–58. doi: 10.1016/j.drugpo.2018.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: Findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122–128. doi: 10.1016/j.drugpo.2018.08.007 [DOI] [PubMed] [Google Scholar]
- 36.Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin.’ Int J Drug Policy. 2017;46:146–155. doi: 10.1016/j.drugpo.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller JM, Stogner JM, Miller BL, Blough S. Exploring synthetic heroin: Accounts of acetyl fentanyl use from a sample of dually diagnosed drug offenders. Drug Alcohol Rev. 2018;37(1):121–127. doi: 10.1111/dar.12502 [DOI] [PubMed] [Google Scholar]
- 38.Carroll JJ, Marshall BDL, Rich JD, Green TC. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. Int J Drug Policy. 2017;46:136–145. doi: 10.1016/j.drugpo.2017.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dezman ZDW, Felemban W, Bontempo LJ, Wish ED. Evidence of fentanyl use is common and frequently missed in a cross-sectional study of emergency department patients in Baltimore, Maryland. Clin Toxicol. 2020;58(1):59–61. doi: 10.1080/15563650.2019.1605078 [DOI] [PubMed] [Google Scholar]


