Abstract
In response to the pandemic, an abrupt pivot of Vascular Quality Initiative physician members away from standard clinical practice to a restrictive phase of emergent and urgent vascular procedures occurred. The Society for Vascular Surgery Patient Safety Organization queried both data managers and physicians in May 2020. Approximately three-fourths (74%) of physicians adopted restrictive operating policies for urgent and emergent cases only, whereas one-half proceeded with “time sensitive” elective cases as urgent. Data manager case entry was negatively affected by both low case volumes and staffing due to reassignment or furlough. Venous registry volumes were reduced fivefold in the first quarter of 2020 compared with a similar period in 2019. The consequences of delaying vascular procedures for ambulatory venous practice remain unknown with increased morbidity likely. Challenges to determine venous thromboembolism mortality impact exist given difficulty in verifying “in home and extended care facility” deaths. Further ramifications of a pandemic shutdown will likely be amplified if postponement of elective vascular care extends beyond a short window of time. It will be important to monitor disease progression and case severity as a result of policy shifts adopted locally in response to pandemic surges.
Keywords: COVID-19, Physician survey, VQI venous registry, Clinical practice shift
Article Highlights.
-
•
Type of Research: Society for Vascular Surgery Patient Safety Organization survey of clinical practice effects due to coronavirus, COVID-19 pandemic. Retrospective review of Vascular Quality Initiative (VQI) venous registry volume between the first quarters of 2019 and 2020
-
•
Key Findings: Seventy-four percent of respondents adopted a restrictive pandemic operating policy to urgent and emergent procedures. One-half of surgeons continued in hospital “time sensitive” elective procedures despite policy shift. A fivefold reduction in VQI venous (varicose veins + inferior vena cava filter) procedural volume was noted in the first quarter of 2020 with data manager reassignment/furlough and case volume decline contributing. Survey questions omitted ambulatory practice change impact.
-
•
Take Home Message: VQI venous case volume activity and registry data entry was sharply reduced during the initial phase of the COVID-19 pandemic as many vascular surgeons adopted a restrictive policy on vascular procedures. Ambulatory venous practice decreased significantly.
The coronavirus pandemic has altered our personal and professional lives in ways that were inconceivable only months ago. As the coronavirus (SARS-CoV-2, herein listed as COVID-19) spread across the United States, health care workers found themselves on the front lines of the battle for their patients and, in many cases, their personal well-being and survival.1
On March 13, the American College of Surgeons issued a recommendation to “review all scheduled elective procedures with a plan to minimize, postpone, or cancel electively scheduled operations.”2 On March 14, Dr Jerome Brown, the Surgeon General of the United States, reiterated this plea with a tweet “Hospital & healthcare systems, PLEASE CONSIDER STOPPING ELECTIVE PROCEDURES until we can #FlattenTheCurve!”3
The vascular surgery community quickly responded to these dramatic events. As a result, the Society for Vascular Surgery (SVS) Patient Safety Organization Vascular Quality Initiative (VQI) noted a precipitous decline in registry volumes. The SVS Patient Safety Organization conducted two surveys early in the pandemic to assess changes in practice. We first surveyed VQI data managers to discern pandemic impact on workflow and queried the historical volume of the M2S registry. Second, we surveyed VQI physicians about practice changes altered in response to the pandemic. We report the findings and discuss the implications in this practice management study.
The status quo disrupted
Before the COVID-19 pandemic, physicians treating vascular disease regularly performed a variety of procedures that were elective, urgent, and emergent in nature. Routine elective venous procedures included varicose vein removal, saphenous vein ablation for reflux, mechanical/thrombolytic treatment of venous thromboembolism, venous stenting, and inferior vena cava (IVC) filter insertion or removal. Combined with nonelective arterial disease, urgent and emergent cases for venous thromboembolism and vascular trauma comprise approximately 30%-50% of an active vascular surgery practice case mix.4 Many practitioners who focus on venous pathology dedicate the majority of their case volume to ambulatory venous disease treatment.
The coronavirus pandemic disrupted this status quo threatening the timeliness and efficiency of care. Physicians were confronted with the dilemma of potential COVID-19 exposure to patients by bringing them into a hospital or office setting. This influenced physicians to rethink potential exposure and utilization of hospital resources possibly needed for COVID-19-related admissions.5 Outpatient vascular services and office-based laboratories providing diagnostic and therapeutic services were also dramatically affected and most apparent for elective venous disease treatment primarily residing in the outpatient arena. In a global survey by Ng et al,6 86.9% of vascular surgeons stated that their outpatient services were either suspended or downscaled in response to the pandemic. With little to no preparation, clinical practice for vascular surgeons had to shift away from preferred face-to-face interactions and adopt an “only if your life (or limb) depends on it” policy for direct patient contact. Postoperative follow-up care and chronic disease management evolved rapidly through “remote” medicine. Examples of these include telemedicine through phone calls, video chats, and interactions via the electronic medical record. This rapid pivot in vascular practice management has only been possible due to advances in technology and internet access.
A change in practice
During the Society for Vascular Surgery's webinar conducted on March 27, Dr Benjamin Starnes clearly and passionately stated: “the ultimate role of the surgeon in a pandemic is to help grow hospital capacity by not operating...” to “preserve space, staff and stuff (personal protective equipment).”7 Vascular surgeons across the nation responded to this “call to inaction” by developing triage plans for elective, urgent, and emergency procedures.8 , 9 Surgeons and trainees were called upon to serve in a variety of new roles to combat the pandemic. The abrupt shutdown of elective surgery in all forms allowed hospitals and health care systems to draw up capacity and formulate surge plans in anticipation of an influx of patients with COVID-19.10
Real-time data of survey of data managers
To determine the pandemic impact on VQI workflow, we conducted a survey of VQI centers sent May 8, 2020, and closed June 15, 2020, from over 220 VQI data managers summarized in Appendix A (online only).
-
•
The majority reported that hospital staff, as opposed to contracted vendors, were responsible for data collection.
-
•
At the time of the survey in early May, almost 10% of centers restricted procedures to emergencies only, whereas over 90% of centers performed urgent and emergent operations. Forty percent of centers continued to perform elective procedures with minimal volume reduction. Elective cases were scheduled to resume between May 11 and 24 (53%) and between May 25 and June 7 (13%) of centers. One-quarter (26%) of centers were unable to provide a definitive time for restarting elective procedures.
-
•
Seventy-five percent of abstractors were not furloughed or reassigned. Thirty percent of respondents reported having lower case volumes at the time of the survey.
-
•
Variation in the methods for long-term follow-up (LTFU) was noted. A third of centers responded that they were continuing to do face-to-face follow-up with the remainder adjusting their follow-ups to phone contact, phone/video calls, or electronic medical record review. Twelve percent of the respondents stated that follow-up was currently not possible.
Survey of VQI member physicians
To assess the effect on practice, we conducted a seven-question survey of VQI physicians sent June 2, 2020, and closed July 20, 2020 (Appendix B, online only). The response from over 100 physicians is summarized here:
-
•
A variety of non-mutually-exclusive sources were used to guide pandemic change in operating policy: institutional (61%), societal guidelines (51%), and Center for Disease Control/Center for Medicare Services guidelines (30%).
-
•
The majority (74%) reported operating policy shift to urgent and emergent cases, with 14% restricting to emergency procedures only. Despite this, one-half of respondents performed “elective” procedures, whereas restrictive policies were in place due to perceived need. Urgent cases were interpreted as both symptomatic and “time sensitive” elective cases as mentioned below.
-
1.
Elective procedures considered time-sensitive primarily encompassed dialysis access (de novo 48%, dysfunctional access 72%, asymptomatic [often with larger size criteria] abdominal aortic aneurysm repair 41%, and PVI for threatened grafts 61%).
-
2.
The majority of centers conducted mandatory COVID-19 testing before surgery (79%); 11% reserved testing for symptomatic patients only.
-
3.
A shift to delay repair to a larger size aneurysm was noted in over one-quarter of the respondents.
-
•
The survey did not include questions directed at ambulatory venous practice.
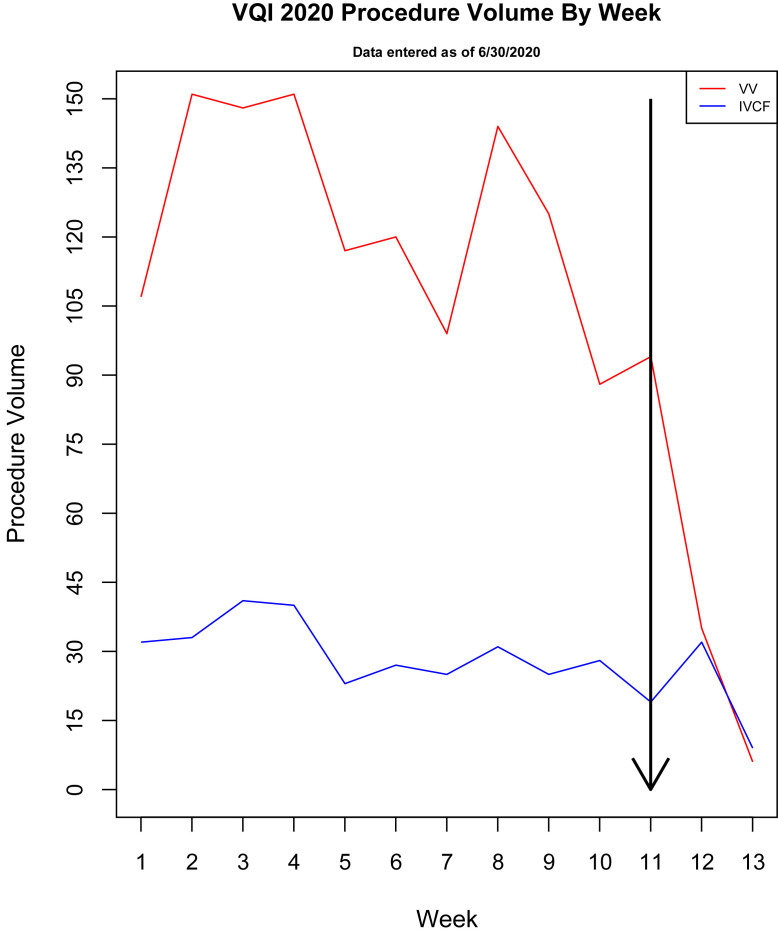
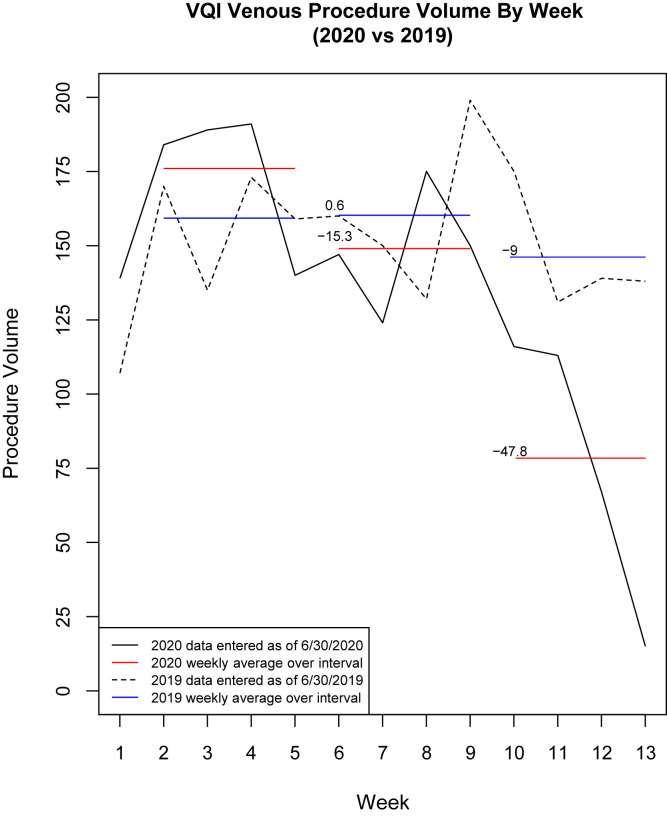
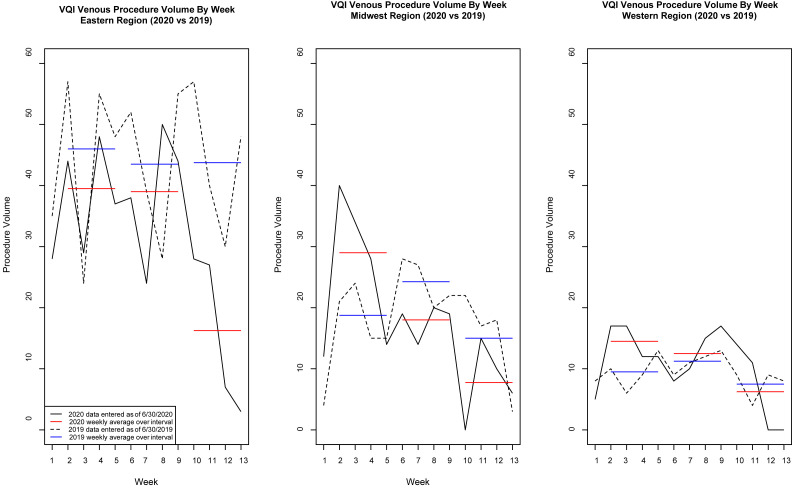
In response to the pandemic, the SVS VQI noted precipitous global declines in all registries including varicose veins (VV) and IVC filter placement, as shown in Fig 1 . Operations for VV and IVC registries were compared on a week-by-week basis with the first quarter of 2019, as shown in Fig 2 . Individually, the VV registry noted a greater decline than did IVC registry volumes by a factor of 6.2-1.8 reduction, respectively (Table ). Combining VV and IVC volumes, a nearly fivefold reduction in average weekly venous procedures was recorded from weeks 6-9 to weeks 10-13 in 2020 (149 to 77.75, 47.8% decrease) when compared with the same period in 2019 (160.25 to 145.75, 9.0% decrease). Geographic differences of the highest performing regional groups from East and West Coast and Midwest demonstrated nearly identical curves to registry volume decline, as shown in Fig 3 . Although delay in data entry may explain part of this decline, such delay would not account for the nearly fivefold decrease in average 2020 weekly venous procedural volumes when compared with the first quarters of both 2018 and 2019. We attribute a significant part of the decline to procedural shutdown across registries for this period. This is supported by over 75% of data managers who were "not reassigned or furloughed" remained active and given reduced case volumes, likely had sufficient time for case entry.
Fig 1.
Graph showing Vascular Quality Initiative (VQI) registry data of weekly vascular surgical procedure volumes during the COVID-19 pandemic. Week 1 = January 4; week 5 = February 1. Line at week 11 showing a steep drop-off in case volume after March 15, 2020. IVCF, Inferior vena cava filter; VV = varicose vein.
Fig 2.
Graph comparing 4-week average procedural volume in 2019 for varicose vein (VV) and inferior vena cava (IVC) registries to Vascular Quality Initiative (VQI) data during the COVID-19 pandemic in 2020. The number over the red and blue lines represents percent change in a 4-week volume during weeks 5-8 and weeks 10-13. For reference: week 1 = January 4; week 5 = February 1; March 15 = week 11 when national shutdown occurred.
Table.
Average weekly registry procedure volumes 2018-2020
| Procedure volume | Weeks 6-9 | Weeks 10-13 | Comparison change (%) |
|---|---|---|---|
| 2018 | |||
| VV | 120 | 127.75 | 6.5 |
| IVC | 33 | 31.5 | −4.5 |
| 2019 | |||
| VV | 126.25 | 115.25 | −8.7 |
| IVC | 34 | 30.5 | −10.3 |
| 2020 | |||
| VV | 122 | 55.75 | −54.3 |
| IVC | 27 | 22 | −18.5 |
IVC, Inferior vena cava; VV, varicose vein.
Table demonstrating average weekly volumes for weeks 6-9 and weeks 10-13 in the first quarter of 2018-2020. A 6.2-fold decrease in VV volume and a 1.8-fold decrease in IVC filter volume from 2019 to 2020 are demonstrated. This represents a fivefold reduction for all 2020 venous procedures compared with 2019.
Fig 3.
Graph demonstrating a sample of regional distribution from high procedural volume centers of varicose vein (VV) and vena cava filter insertion. The first quarter weeks 1-13 listed for 2019 and 2020. March 15 = week 11 when national shutdown occurred. VQI, Vascular Quality Initiative.
Our abbreviated survey did not inquire about ambulatory practice revisions or office-based laboratory performance. Thus, the full impact on venous practice cannot be fully assessed. Given the unprecedented shutdown to all nonessential services nationally, it is reasonable to surmise that ambulatory treatment of venous disorders lessened significantly, as we continue to hear anecdotally of ongoing treatment of acute thrombophlebitis, infected venous ulcers, and other urgent conditions (JE-J).
The downstream secondary effects of suspending operations are unknown. Approximately 20% of venous disorders require emergent treatment (thrombolysis, IVC filter insertion/removal, thrombectomy) requiring hospitalization. Most can still be performed percutaneously and contribute to a reduced procedural length of stay. Increased usage of outpatient low-molecular-weight heparin injection/oral anticoagulant drug medication in place of inpatient continuous intravenous heparin infusions can also reduce inpatient bed utilization.
COVID-19 and peripheral venous complications
Recent research has demonstrated the coronavirus's ability to produce thrombotic complications due to the cytokine storm triggering a systemic immune response.11 As a result, infected patients are at higher risk of developing a hypercoagulable state with arterial and venous thrombosis. Excessive inflammation, platelet activation, endothelial dysfunction, and stasis have been postulated as mechanisms.12 Venous thromboembolic events appear more common than arterial thromboembolism yet few vascular beds have been spared.13, 14, 15, 16 Going forward, vascular surgeons will need to assess both a patient's response to a venous procedure and if prior or current COVID-19 infection has altered coagulation. Unknown dilemmas such as proper timing to safely perform a venous ablation in patients who have contracted COVID-19 yet are clinically asymptomatic are not presently clear. It is becoming apparent that COVID-19's hypercoagulable duration may extend beyond acute hospitalization and into the convalescent stage; thus anticoagulation may need to be extended beyond current accepted guidelines. The SVS VQI is partnering with the Vascular Surgery COVID-19 Collaborative to learn more about the long-term impact on vascular patients.17 The VQI has incorporated variables in all procedural registries by late August to early September 2020 on COVID-19 status, infection history, and impact for ongoing monitoring at the time of procedure and at LTFU.
Of concern are the unknown number of patients who may delay treatment for health issues because of fear of contracting COVID-19 by seeking medical attention. Emergency department visits for acute cardiac events have had a notable decline during the pandemic while a reciprocal rise in “at home” deaths have been reported.13 , 18 The health care impact of COVID-19 will need to take into account indirect collateral morbidity and mortality rates due to patient reluctance or refusal to seek timely medical attention.19 , 20
Invariably, as health care systems look ahead to a return to the business of medicine, guidelines have been developed for a return to resuming operations.10 Hospitals and surgeons may adapt to elective procedure backlogs and clinic visits in any number of ways including longer weekday hours or weekend surgery.
The present analysis is limited by the subjective nature of an elective survey and our attempt to correlate these results with actual workload volumes in the VQI procedure-driven registry. Attributing a nearly fivefold difference in venous case volume drop to lack of data entry alone should be viewed with caution as events surrounding responses to the COVID-19 crises are clearly multifactorial, noting that 40% of centers continued elective work during this time. Changes in data manager workflow and LTFU will need to be considered for future quality reporting and VQI clinical research studies. Survey questions were also directed primarily to the inpatient setting with an emphasis on arterial procedures and thus did not completely capture ambulatory venous changes in surgical centers and office-based laboratories. Given survey focus, we also cannot comment on indications or results of venous procedures performed during this time. That will require ongoing analysis of center-specific data.
Although we analyzed geographic regions by coastal and Midwest locations, we cannot determine regional distribution to the survey responses at the center level. VQI centers are in all 50 states. Each geographic location demonstrated similar rates of decline after mid-March, indicating the national shutdown-affected regions equally. We were unable to determine on a more granular level the impact on individual centers. A more detailed reporting of regional differences in practice variation during pandemic restrictions will require further trend analysis near the end of 2020, not available at the time this manuscript was written. Given the uncertain future over the coming 1-2 years, the U.S. health care system will face ongoing challenges. The authors expect these challenges to be unevenly distributed over place and time given variations in state and local guidelines for practice restrictions. Localized outbreaks with clusters of infection or a resurgence of epidemics may necessitate a similar regional response with a reduction in elective surgery.
Research into the ramifications of the coronavirus pandemic on all facets of vascular care will help us provide the best care to our patients. Venous treatment delays may lead to progression of thrombotic disease, embolization, or worsen morbidity of postphlebitic limbs. Vascular surgeon's partnership with public health experts and epidemiologists to study the pandemic impact and our response to the public health crisis should be ongoing. Most importantly, we must look for new and innovative ways to practice in what will likely be a “new abnormal.”
Conclusions
The vascular surgery community response to the global COVID-19 pandemic during the national shutdown resulted in a dramatic reduction in elective case volumes with most practitioners performing emergency and select urgent procedures only. A fivefold reduction in venous registry case volumes was noted when compared with the same period in 2019. The potential impact of delaying treatment on vascular disease remains unknown and will require further analysis. The VQI is moving forward with regional virtual meetings that will provide a forum for study, reflection, communication, and discussion.
Author contributions
Conception and design: AM, JN, DB, JE, GL
Analysis and interpretation: AM, JN, DB, KH, JE, GL
Data collection: KH
Writing the article: AM, JN, DB, KH, JE, GL
Critical revision of the article: DB, KH, JE, GL
Final approval of the article: AM, JN, DB, KH, JE, GL
Statistical analysis: KH
Obtained funding: Not applicable
Overall responsibility: GL
Footnotes
Author conflict of interest: none.
Additional material for this article may be found online at www.jvsvenous.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Additional material for this article may be found online at www.jvsvenous.org.
Appendix (online only).
References
- 1.National Center for Immunization and Respiratory Diseases Cases in the U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Available at:
- 2.American College of Surgeons COVID-19: recommendations for management of elective surgical procedures. ACS: COVID-19 and Surgery. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at:
- 3.Brown, Jerome (@Surgeon_General) “Hospital & healthcare systems, PLEASE CONSIDER STOPPING ELECTIVE PROCEDURES until we can #FlattenTheCurve!”. March 14, 2020. 8:14 am. Tweet. [Google Scholar]
- 4.American College of Surgeons COVID-19 guidelines for triage of vascular surgery patients. ACS: COVID-19 and Surgery. https://www.facs.org/covid-19/clinical-guidance/elective-case/vascular-surgery Available at:
- 5.Al-Jabir A., Kerwan A., Nicola M., Zaid A., Mehdi K., Sohrabi C. Impact of the coronavirus (COVID-19) pandemic on surgical practice: part 2 (surgical prioritisation) Int J Surg. 2020;79:233–248. doi: 10.1016/j.ijsu.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng J.J., Ho P., Dharmaraj R.B., Wong J.C.L., Choong A.M.T.L. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183.e1. doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lumsden A., Hodgson K., Irshad A., Forbes T.L., Starnes B.W., McDevitt D. Society for Vascular Surgery; USA: 2020. Early Vascular Surgeon Experiences with COVID-19 (Kim Hodgson, MD & Alan Lumsden, MD) March 27, 2020 [YouTube] [Google Scholar]
- 8.Society for Vascular Surgery COVID-19 resources for members. https://vascular.org/news-advocacy/covid-19-resources Available at:
- 9.CMS News and Media Group Press release CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. CMS releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental Available at:
- 10.American College of Surgeons Joint statement: roadmap for resuming elective surgery after COVID-19 pandemic. ACS: COVID-19 and Surgery. https://www.facs.org/covid-19/clinical-guidance/roadmap-elective-surgery Available at:
- 11.Gralinski L.E., Baric R.S. Molecular pathology of emerging coronavirus infections. J Pathol. 2015;235:185–195. doi: 10.1002/path.4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teo K.C., Leung W.C.Y., Wong Y.K., Liu R., Chan A., Choi O. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kashi M., Jacquin A., Dakhil B., Zaimi R., Mahe E., Tella E. Severe arterial thrombosis associated with Covid-19 infection. Thromb Res. 2020;192:75–77. doi: 10.1016/j.thromres.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mestres G., Puigmacià R., Blanco C., Yugueros X., Esturrica M., Riambau V. Risk of peripheral arterial thrombosis in COVID-19. J Vasc Surg. 2020;72:756–757. doi: 10.1016/j.jvs.2020.04.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomez-Arbelaez D., Ibarra-Sanchez G., Garcia-Gutierrez A., Comanges-Yeboles A., Ansuategui-Vicente M., Gonzalez-Fajardo J.A. COVID-19-related aortic thrombosis: a report of four cases. Ann Vasc Surg. 2020;67:10–13. doi: 10.1016/j.avsg.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vascular Surgery COVID-19 Collaborative (VASCC) https://medschool.cuanschutz.edu/surgery/specialties/vascular/research/vascular-surgery-covid-19-collaborative/vascc Available at: [DOI] [PMC free article] [PubMed]
- 18.Marijon E., Karam N., Jost D., Perrot D., Frattini B., Derkenne C. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastion T. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatt A.S., Moscone A., McElrath E.E., Varshney A., Claggett B., Bhatt D. Declines in hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic: a multicenter tertiary care experience. J Am Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.