Abstract
Objective
To investigate mental health status and associated factors among caregivers of older adults during the COVID-19 epidemic in China.
Methods
From March 1 to 31, 2020, 916 caregivers of older adults participated in an online cross-sectional survey on the prevalence of anxiety, depression, and sleep problems. The seven-item Generalized Anxiety Disorder Scale (GAD-7) was administered to measure anxiety symptoms, the two-item Patient Health Questionnaire (PHQ-2) was used to assess depressive symptoms, and a self-developed questionnaire was used to assess sleep quality and duration. Six questions about COVID-19-related experiences were used to assess community-level infection contact and the level of exposure to media information. The prevalence rates of anxiety, depression and sleep problems were computed. The Wald χ2 were applied to compare the differences between subgroups. Multiple logistic regression analyses were performed to investigate factors associated with anxiety, depression, sleep problems, and multimorbidity.
Results
The prevalence rates of anxiety, depression, and sleep problems were 46.8%, 29.8%, and 10.8%, respectively. Approximately 263 participants (28.7%) presented with two or more mental health problems. Being female (OR, 2.254; 95% CI, 1.510–3.363), having community-level COVID-19 contact (OR, 1.856; 95% CI, 1.189–2.898), and having a mental disorder (OR, 3.610; 95% CI, 1.644–7.930) were associated with increased risk of multimorbidity among caregivers. Caregivers who preferred positive information (OR, 0.652; 95% CI, 0.472–0.899) had reduced risk of multimorbidity.
Conclusion
Anxiety and depression were common among caregivers of older adults during the COVID-19 epidemic. Being female and having community-level COVID-19 contact were independent risk factors for experiencing multiple mental health problems. Preexisting mental disorders increased the risk of multimorbidity among caregivers, while enhanced access to positive media information decreased the risk of multimorbidity.
KEY WORDS: COVID-19, anxiety, depression, multimorbidity, caregiver, older adults
INTRODUCTION
Since the outbreak of COVID-19, older adults who are exposed have been at high risk of infection and death.1 Caregiver roles can have adverse consequences, causing caregivers to experience higher levels of depression and anxiety and poorer physical health than other populations.2 During the period of social distancing due to the COVID-19 outbreak, caregivers of older adults were exposed to double stress: fear of infection and concern about the elderly individuals’ conditions.3 , 4 However, mental health status among caregivers of older adults was not fully attended in January and February 2020.
Of note, the general population has not been spared from the psychological consequences of the COVID-19 outbreak.5 Caring staff can experience a state of physical and mental stress and feel isolated and helpless in the face of health threats and pressures because of the high-intensity work necessitated by such public health emergencies.6 Previous studies have shown that caregivers and nurses suffer from loneliness, anxiety, fear, fatigue, sleep disorders, and other mental health problems when in close contact with patients with emerging infectious diseases such as SARS,7 MERS-CoV infection,8 , 9 Ebola,10 and H1N1 infection.11 These problems can be related to various factors during such outbreaks, including disruption of the usual routine of life because of isolation,12 grief and loss.13 Direct contact with elderly individuals who are strongly suspected of having an infectious disease is also stressful for caregivers. Previous studies have shown that factors associated with stress among caregivers include long work hours, high workloads, a lack of decision-making flexibility at work and a lack of experience with similar situations.14 , 15
In addition, the threat of infectious disease can create strong negative feelings including intense fear, and fear-related public ostracism can lead to psychological pain and other negative effects.6 , 16 These psychological responses affect the wellbeing of the individual and community and can persist long after an outbreak subsides.17
The psychological experiences of caregivers for patients with COVID-19 can be summarized into several themes. First, as the number of patients has continued to rise and as quarantines have been put into place,1 , 18 the workloads of caregivers have increased rapidly from normal levels, and the contact time with elderly individuals has proportionally increased, increasing the likelihood of conflict with the elderly individuals.4 , 19 In addition, the caregivers have experienced a strong sense of fear when protective equipment has been in short supply. The failure to meet physical and psychological needs has brought about a sense of helplessness.20 Most caregivers taking care of older adults in an isolated environment have been concerned mainly about the unknown conditions of severe emergencies and about work-related processes and routines. As with any emerging infectious disease, these concerns need to be addressed while the caregivers are working. Moreover, most caregivers have also been concerned about the impacts of the outbreak on the health of their families, and their families have likewise been worried about them. A previous study has also noted that the traumatic experience of the death of a loved one can cause severe psychological, physical, and behavioral consequences in caregivers.21 Additionally, previous studies have found that sensationalized media reporting and access to channels disseminating unofficial information about an outbreak frequently leads to general panic that often extends far beyond the geographical location of the actual epidemic.22, 23, 24
Besides, preexisting mental disorders might have negative impact on the caregivers’ mental health status. Disasters disproportionately affect poor and vulnerable populations, and patients with severe mental illness may be among the hardest hit.25 For example, individuals with severe mental illnesses who are employed may have difficulty taking time off from work and may lack sufficient insurance coverage to cover testing or treatment.26
However, it has remained unclear how common mental health problems are among caregivers of older adults and how frequently such caregivers present with more than one mental health problem. Additionally, whether COVID-19-related experiences are associated with the presence of multiple mental health problems has not been fully investigated.
Therefore, we conducted this cross-sectional survey to estimate the prevalence of anxiety, depression, and sleep problems and the coexistence of these three common mental health problems among caregivers of older adults during the COVID-19 epidemic. In addition, our study explored the potential risk factors for these mental health problems with particular emphasis on COVID-19-related experiences.
METHODS
This cross-sectional survey was conducted through the Questionnaire Star online survey platform from March 1 to 31, 2020. The URL link was distributed through the geriatric mental health service network by members of the Chinese Society of Geriatric Psychiatry.
Study Participants
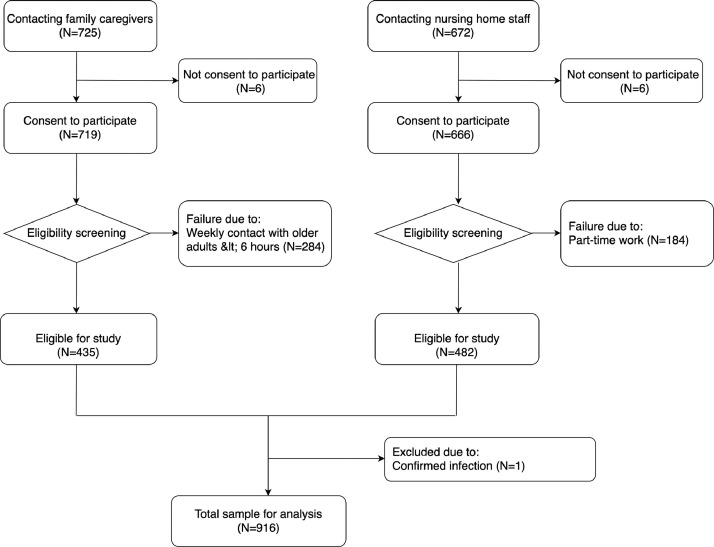
During the survey period, 1,385 participants accessed the screening page of the online questionnaire. As illustrated in Figure 1 , 916 participants, including 434 family caregivers and 482 nursing home staff, were eligible for the study. The inclusion criteria for family caregivers included family members or care workers who 1) took care of older adults at home and 2) spent at least 6 hours per week with care recipients. Besides, full-time care workers at nursing home were eligible to attend the survey. All caregivers were required to have basic listening, speaking, reading and writing abilities and to be able to use a smartphone or computer to ensure their completion of the self-reported questionnaire and online surveys.
FIGURE 1.
Flow chart of subject recruitment and participation in the online survey.
The ethics committee of Peking University Sixth Hospital approved the study protocol. All subjects provided their consent by answering the screening question “Are you willing to participate in the survey?” The survey was anonymous. No personal information could be identified through the questionnaire.
Instruments for Mental Health Problem Assessment
Seven-item Generalized Anxiety Disorder Scale (GAD-7)
The GAD-7 was designed to identify probable cases of generalized anxiety disorder and to assess symptom severity. The cutoff score for anxiety was greater than 5.27
Two-item Patient Health Questionnaire (PHQ-2)
The PHQ-2 included the first two items of the PHQ-9, i.e., “little interest or pleasure in doing things” and “feeling down, depressed, or hopeless”, for the previous 2 weeks. The cutoff score for depression was greater than 2.28 , 29
Questions on sleep problems
Two questions were used to screen sleep problems: “How long on average did you sleep per day in the past month?” and “How has your sleep quality changed in the past month?” Sleep problems were defined as follows: 1) a daily average duration of sleep less than 4 hour or more than 8 hour and 2) poorer sleep quality than before.30
Assessment of COVID-19-Related Experiences
Community-level infection contact
Two questions were used to examine the degree of community-level infection contact: “Did you have close contact with any individual with confirmed or suspected COVID-19?” and “Was there anyone confirmed or suspected with COVID-19 in your community and neighborhood?”. A response of “yes” to either question was considered a positive indication of community-level infection contact.
Exposure to epidemic-related information
Four questions were used to measure the level of exposure to media information, including questions regarding the time spent browsing information per day (<1 hour, 1–3 hour, 3–6 hour, or >6 hour), the preference of the individual for the nature of information (primarily positive, half positive or half negative or primarily negative), the number of channels used to obtain information (including TV news, the internet, social media platforms such as WeChat and WeBlog, the newspaper, relatives and friends, community workers, or others), and the reliability of the information obtained (information from TV, newspaper, and community workers was classified as highly reliable; information from other channels was classified as potentially reliable).
Medical History Assessment
Two questions were used to identify the medical history of physical and mental conditions: “Have you ever been diagnosed with any of the following physical diseases?” and “Have you ever been diagnosed with any of the following mental disorders?”.
Statistical Analysis
Data analysis was performed using SPSS statistical software version 26.0. The significance level was set at p = 0.05.
Participants were classified as having any single mental health problem or as having two or more mental health problems, which was considered multimorbidity. The χ2 was applied to compare the subjects’ demographic characteristics (age, sex, education level, marital status, place of residence, and medical history), and degree of community-level infection contact between subgroups with and without anxiety, depression and sleep problems. The Kruskal-Wallis test was applied to compare the time of exposure to epidemic information between subgroups.
The differences among those without mental health problems, those with any single mental health problem, and those having two or more mental health problems were investigated with χ2. The continuous variables were compared with ANOVA test. Bonferroni correction was used for post-hoc tests.
Multiple logistic regression analysis was performed to examine the potential factors associated with the risks of anxiety, depression, and multimorbidity. As there were no significant differences in any of the studied variables between the subgroups with and without sleep problems, we did not perform multiple logistic regression analysis of factors associated with sleep problems. The odds ratios (ORs) and 95% confidence intervals (CIs) were computed and are presented.
RESULTS
Demographic Characteristics
As presented in Table 1 , approximately three-quarters of caregivers were women, and most participants were younger than 60 years old, married and residing in cities. Approximately one-fifth of the caregivers had physical conditions, and approximately 4.6% had mental disorders.
TABLE 1.
Demographic Characteristics of All Study Participants and Comparison Between Mental Health Status Subgroups
| Variable | All Participants (N=916) | N (%) |
χ2 | p-value | N (%) |
χ2 | p-Value | N (%) |
χ2 | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety |
Depression |
Sleep Problems |
|||||||||||
| No (N=487) | Yes (N=429) | No (N=643) | Yes (N=273) | No (N=817) | Yes (N=99) | ||||||||
| Age | |||||||||||||
| <60 years | 812 (88.7%) | 434 (53.4%) | 378 (46.6%) | 0.229 | 0.632 | 568 (70.0%) | 244 (30.0%) | 0.206 | 0.650 | 722 (88.9%) | 90 (11.1%) | 0.565 | 0.452 |
| ≥60 years | 104 (11.3%) | 53 (51.0%) | 51 (49.0%) | 75 (72.1%) | 29 (27.9%) | 95 (91.3%) | 9 (8.7%) | ||||||
| Gender | |||||||||||||
| Men | 227 (24.8%) | 149 (65.6%) | 78 (34.4%) | 18.855 | <0.001 | 176 (77.5%) | 51 (22.5%) | 7.764 | 0.005 | 200 (88.1%) | 27 (11.9%) | 0.370 | 0.543 |
| Women | 689 (75.2%) | 338 (49.1%) | 351 (50.9%) | 467 (67.8%) | 222 (32.2%) | 617 (89.6%) | 72 (10.4%) | ||||||
| Schooling educational level | |||||||||||||
| ≤9 years | 467 (51.0%) | 235 (50.3%) | 232 (49.7%) | 3.096 | 0.078 | 338 (72.4%) | 129 (27.6%) | 2.165 | 0.141 | 428 (91.6%) | 39 (8.4%) | 5.965 | 0.015 |
| >9 years | 449 (49.0%) | 252 (56.1%) | 197 (43.9%) | 305 (67.9%) | 144 (32.1%) | 389 (86.6%) | 60 (13.4%) | ||||||
| Marital status | |||||||||||||
| Married | 751 (82.0%) | 405 (53.9%) | 346 (46.1%) | 0.973 | 0.324 | 539 (71.8%) | 212 (28.2%) | 4.940 | 0.026 | 670 (89.2%) | 81 (10.8%) | 0.002 | 0.963 |
| Single/divorced/widowed | 165 (18.0%) | 82 (49.7%) | 83 (50.3%) | 104 (63.0%) | 61 (37.0%) | 147 (89.1%) | 18 (10.9%) | ||||||
| Residence | |||||||||||||
| Urban | 722 (78.8%) | 373 (51.7%) | 349 (48.3%) | 3.096 | 0.078 | 496 (68.7%) | 226 (31.3%) | 3.659 | 0.056 | 639 (88.5%) | 83 (11.5%) | 1.674 | 0.196 |
| Suburban/rural | 194 (21.2%) | 114 (58.8%) | 80 (41.2%) | 147 (75.8%) | 47 (24.2%) | 178 (91.8%) | 16 (8.2%) | ||||||
| Physical Conditions | |||||||||||||
| Yes | 197 (21.5%) | 85 (43.1%) | 112 (56.9%) | 10.117 | 0.001 | 130 (66.0%) | 67 (34.0%) | 2.123 | 0.145 | 182 (92.4%) | 15 (7.6%) | 2.655 | 0.103 |
| No | 719 (78.5%) | 402 (55.9%) | 317 (44.1%) | 513 (71.3%) | 206 (28.7%) | 635 (88.3%) | 84 (11.7%) | ||||||
| Pre-existing mental disorders | |||||||||||||
| Yes | 42 (4.6%) | 17 (40.5%) | 25 (59.5%) | 2.847 | 0.092 | 19 (45.2%) | 23 (54.8%) | 13.106 | <0.001 | 34 (81.0%) | 8 (19.0%) | 3.100 | 0.078 |
| No | 874 (95.4%) | 470 (53.8%) | 404 (46.2%) | 624 (71.4%) | 250 (28.6%) | 783 (89.6%) | 91 (10.4%) | ||||||
| Community-level infection contact | |||||||||||||
| Yes | 127 (13.9%) | 58 (45.7%) | 69 (54.3%) | 3.328 | 0.068 | 75 (59.1%) | 52 (40.9%) | 8.748 | 0.003 | 114 (89.8%) | 13 (10.2%) | 0.050 | 0.823 |
| No | 789 (86.1%) | 429 (54.4%) | 360 (45.6%) | 568 (72.0%) | 221 (28.0%) | 703 (89.1%) | 86 (10.9%) | ||||||
| Time spent browsing informationa | |||||||||||||
| <1 h | 243 (26.5%) | 139 (57.2%) | 104 (42.8%) | 2.294 | 0.514 | 173 (71.2%) | 70 (28.8%) | 2.309 | 0.511 | 213 (87.7%) | 30 (12.3%) | 1.714 | 0.634 |
| 1-3 h | 512 (55.9%) | 265 (51.8%) | 247 (48.2%) | 359 (70.1%) | 153 (29.9%) | 458 (89.5%) | 54 (10.5%) | ||||||
| 3-6 h | 103 (11.3%) | 52 (50.5%) | 51 (49.5%) | 67 (65.0%) | 36 (35.0%) | 95 (92.2%) | 8 (7.8%) | ||||||
| >6 h | 58 (6.3%) | 31 (53.4%) | 27 (46.6%) | 44 (75.9%) | 14 (24.1%) | 51 (87.9%) | 7 (12.1%) | ||||||
| Preference for the nature of information | |||||||||||||
| Primarily positive | 528 (57.6%) | 297 (56.3%) | 231 (43.8%) | 4.762 | 0.029 | 389 (73.7%) | 139 (26.3%) | 7.206 | 0.007 | 479 (90.7%) | 49 (9.3%) | 3.017 | 0.082 |
| Half positive/half negative or primarily negative | 388 (42.4%) | 190 (49.0%) | 198 (51.0%) | 254 (65.5%) | 134 (34.5%) | 338 (87.1%) | 50 (12.9%) | ||||||
| Number of channels used to obtain information | 3.05±1.477 | 3.17±1.583 | -1.256* | 0.209 | 3.10±1.515 | 3.12±1.560 | -0.132* | 0.895 | 3.08±1.531 | 3.31±1.496 | -1.422* | 0.155 | |
| Reliability of the information obtained | 2.16±1.104 | 2.24±1.211 | -1.014* | 0.311 | 2.21±1.141 | 2.17±1.189 | 0.471* | 0.638 | 2.18±1.158 | 2.34±1.127 | -1.265* | 0.206 | |
Notes: χ2, df=1
df=3, * independent samples t test, t-value, df=914
Further analysis showed that gender, marital status, physical conditions, preexisting mental disorders, and time spent browsing information were significantly different between older and younger groups (see Supplemental Table S1).
Prevalence of Anxiety, Depression, and Sleep Problems
Of all study participants, 429 (46.8%) presented with anxiety, 273 (29.8%) had depression, and 99 (10.8%) reported sleep problems.
As shown in Table 1, anxiety was more frequent among women than among men and among caregivers with physical conditions than among those who were healthy. Caregivers with preference for positive information had lower prevalence of anxiety.
Depression was more common among women than among men, among caregivers with mental disorders than among those without and among caregivers with community-level infection contact than among those without. Caregivers who were married and preferred to obtain positive information had a lower prevalence of depression.
Sleep disturbance was more frequent among those with higher educational levels.
Prevalence and Profiles of Mental Health Multimorbidity
Among those reporting mental health problems, 249 (27.2%) presented with a single problem, and 263 (28.7%) had two or more problems.
Among the 263 participants who had two or more mental health problems, 220 (83.6%) had anxiety and depression, 5 (1.9%) had depression and sleep problems, 12 (4.6%) had anxiety and sleep problems, and 26 (9.9%) had all three problems.
As shown in Table 2 , multimorbidity was more prevalent among women than among men, among those with community-level COVID-19 contact than among those without, and among those with preexisting mental disorders than among those without. It was less common among individuals who preferred to read positive messages than among those who did not.
Table 2.
Comparisons of Demographic Characteristics and COVID-19-related Experiences Among Normal Comparison, Those With Single Morbidity and Those With Mental Health Multimorbidity
| Variable | Normal Comparison (N=404) | Single Morbidity (N=249) | Multimorbidity# (N=263) | χ2 | p-Value |
p-Value |
||
|---|---|---|---|---|---|---|---|---|
| NC vs SM | NC vs MM | SM vs MM | ||||||
| Age | ||||||||
| <60 years | 359 (44.2%) | 218 (26.9%) | 235 (28.9%) | 0.447 | 0.800 | |||
| ≥60 years | 45 (43.3%) | 31 (29.8%) | 28 (26.9%) | |||||
| Gender | ||||||||
| Women | 287 (41.7%) | 181 (26.3%) | 221 (32.1%) | 15.594 | <0.001 | 0.649 | <0.001 | 0.002 |
| Men | 117 (51.5%) | 68 (30.0%) | 42 (18.5%) | |||||
| Schooling educational level | ||||||||
| ≤9 years | 200 (42.8%) | 142 (30.4%) | 125 (26.8%) | 5.250 | 0.072 | |||
| >9 years | 204 (45.4%) | 107 (23.8%) | 138 (30.8%) | |||||
| Marital status | ||||||||
| Married | 337 (44.9%) | 208 (27.7%) | 206(27.4%) | 3.348 | 0.188 | |||
| Single/divorced/widowed | 67 (40.6%) | 41 (24.9%) | 57 (34.5%) | |||||
| Residence | ||||||||
| Urban | 308 (42.7%) | 194 (26.9%) | 220 (30.5%) | 5.413 | 0.067 | |||
| Suburban/rural | 96 (49.5%) | 55 (28.3%) | 43 (22.2%) | |||||
| Physical conditions | ||||||||
| Yes | 74 (37.6%) | 55 (27.9%) | 68 (34.5%) | 5.431 | 0.066 | |||
| No | 330 (45.9%) | 194 (27.0%) | 195 (27.1%) | |||||
| Pre-existing mental disorders | ||||||||
| Yes | 10 (23.8%) | 11 (26.2%) | 21 (50.0%) | 11.075 | 0.004 | 0.172 | 0.001 | 0.096 |
| No | 394 (45.1%) | 238 (27.2%) | 242 (27.7%) | |||||
| Community-level infection contact | ||||||||
| Yes | 46 (36.2%) | 31 (24.4%) | 50 (39.4%) | 8.329 | 0.016 | 0.682 | 0.006 | 0.042 |
| No | 358 (45.4%) | 218 (27.6%) | 213 (27.0%) | |||||
| Time spent browsing informationa | ||||||||
| <1 h | 110 (45.3%) | 67 (27.6%) | 66 (27.2%) | 0.606 | 0.895 | |||
| 1-3 h | 224 (43.8%) | 139 (27.1%) | 149 (29.1%) | |||||
| 3-6 h | 45 (43.7%) | 24 (23.3%) | 34 (33.0%) | |||||
| >6 h | 25 (43.1%) | 19 (32.8%) | 14 (24.1%) | |||||
| Preference for the nature of information | ||||||||
| Primarily positive | 253 (47.9%) | 140 (26.5%) | 135 (25.6%) | 8.602 | 0.014 | 0.105 | 0.004 | 0.267 |
| Half positive/half negative or primarily negative | 151 (38.9%) | 109 (28.1%) | 128 (33.0%) | |||||
| Number of channels used to obtain informationb | 3.01±1.51 | 3.24±1.48 | 3.13±1.60 | 1.905 | 0.149 | |||
| Reliability of the information obtainedb | 2.14±1.12 | 2.31±1.13 | 2.19±1.23 | 1.742 | 0.176 | |||
Notes: NC: normal comparison; SM: single morbidity; MM: multimorbidity. Most group comparisons (exceptions indicated otherwise) were conducted with χ2, df=2
Kruskal-Wallis test, df=3
ANOVA analysis, df (between groups) =2, df (within groups) = 913.
Factors Associated With Anxiety, Depression and Sleep Problems
Multiple logistic regression analyses showed that female sex (OR=2.068, 95% CI=1.508–2.838) and physical conditions (OR=1.727, 95% CI=1.249–2.388) were associated with increased risk of anxiety. Preference for positive information was associated with lower risk of anxiety (OR=0.747, 95% CI=0.572–0.977). Female sex (OR=1.732, 95% CI=1.212–2.477), community-level COVID-19 contact (OR=1.770, 95% CI=1.192–2.630), and preexisting mental disorders (OR=3.156, 95% CI=1.665–5.981) were associated with increased risk of depression. Being married (OR=0.680, 95% CI=0.473–0.978) and preferring to positive messages (OR=0.714, 95% CI=0.533–0.956) may have reduced the risk of depression. A higher educational level was associated with increased risk of sleep problems (OR=1.693, 95% CI=1.106–2.591) (see Supplemental Table S2).
Factors Associated With Multimorbidity of Mental Health Problems
As summarized in Table 3 , in comparison with the normal comparison, women (OR=2.254, 95% CI=1.510–3.363), individuals with community-level COVID-19 contact (OR=1.856, 95% CI=1.189–2.898), and individuals with preexisting mental disorders (OR=3.610, 95% CI=1.644–7.930) exhibited increased risk of multimorbidity. A preference for positive information was associated with lower risk of multimorbidity (OR=0.652, 95% CI=0.472–0.899). Women (OR=2.042, 95% CI=1.321–3.155) and individuals with community-level COVID-19 contact (OR=1.705, 95% CI=1.041–2.792) were at elevated risk of developing more than one mental health problem.
Table 3.
Multiple Logistic Regression Analyses of Factors Associated With Mental Health Multimorbidity
| Variable | Wald χ2 | p-Value | OR (95%CI) |
|---|---|---|---|
| Comparison with normal comparison | |||
| Gender, women | 15.821 | <0.001 | 2.254 (1.510-3.363) |
| Pre-existing mental disorders | 10.225 | 0.001 | 3.610 (1.644-7.930) |
| Community-level COVID-19 contact | 7.400 | 0.007 | 1.856 (1.189-2.898) |
| Preference for positive information | 6.795 | 0.009 | 0.652 (0.472-0.899) |
| Comparison with single morbidity | |||
| Gender, women | 10.337 | 0.001 | 2.042 (1.321-3.155) |
| Community-level COVID-19 contact | 4.490 | 0.034 | 1.705 (1.041-2.792) |
Notes: Multiple logistic regression analysis, df=1.
DISCUSSION
To our knowledge, this is the first study to investigate mental health problems among caregivers of older adults during the COVID-19 epidemic. Mental health problems, especially anxiety and depression, were common among all study participants. The study also found that being female, having community-level COVID-19 contact and having preexisting mental disorders increased the risk of depression. In particular, being female and having community-level COVID-19 contact were independent risk factors for experiencing multiple mental health problems. Compared with normal comparison, caregivers with preexisting mental disorders exhibited increased risk of multimorbidity, while those who obtained access to more positive media information exhibited decreased risk of multimorbidity.
In this study, caregivers were not free from the psychological consequences of the outbreak, as the results revealed a high prevalence of mental health symptoms during the COVID-19 epidemic. Almost half of the participants presented anxiety symptoms, and one-third of them experienced depressive symptoms. Similarly, the anxiety levels of caregivers were found to be significantly higher than those of the general community during the SARS outbreak in Cheng et al.’s study.31 The prevalence rate of anxiety and depression was higher than those reported in general populations5 , 32 and similar to that among healthcare workers exposed to COVID-19.33 It highlights that the mental health needs of elder caregivers should be addressed timely.
Previous studies have shown that caregivers who are female and who have chronic illnesses prior to an outbreak are more likely to experience anxiety.34, 35, 36 Moreover, caregivers who are female and who have preexisting mental health problems have been found to exhibit significant rates of depression, while being married has been found to be protective against depression. Our study had similar observations. In addition, education level was found to be inversely associated with caregivers’ sleep problems in the current study. These findings are similar to previous reports.35 Despite the possible differences related to culture, the results indicate that higher education levels may facilitate timely acquisition of COVID-19-related information, which might increase fear if the nature of information was not well discerned and the information was misinterpreted.37
Furthermore, we found that having community-level COVID-19 contact was an independent risk factor for experiencing multiple mental health problems. A study on the Ebola virus has noted that direct contact with highly infectious patients is associated with stress.16 Previous studies have also shown that close contact with patients with emerging infectious diseases such as SARS causes individuals to suffer from loneliness, anxiety, fear, sleep disorders, and other mental health problems.38
Caregivers who had preexisting mental health problems in this study had a high propensity to develop multimorbidity, especially comorbidity of anxiety and depression. Disasters disproportionately affect caregivers, especially those with severe mental illness.26 , 39 , 40 Such mental health problems may not only lead to job dissatisfaction and possibly impair work performance but also aggravate burnout, which have likely been prominent problems during the outbreak of COVID-19. Other research also found that mental problems were part of the long-term burdens on caregivers.41 These findings highlight the need to maintain the continuity of mental health services, especially for those with preexisting mental illnesses who may be affected by the COVID-19 pandemic.
A flood of evolving information, as well as potentially damaging misinformation, has accompanied the coronavirus pandemic.42 Interestingly, our study revealed that access to more positive media information decreased the risk of multimorbidity. The media play a key role in disseminating information about epidemics, including information about the spread, characteristics, transmission, and human impacts of diseases.43 Previous studies found that the more frequently people paid attention to the epidemic information of COVID-19 outbreak, the more negative the information they received, and the more anxious they would be.44 Another survey noted that useful and supportive information was associated with less panic from epidemic diseases and increased confidence to fight against the disease.45 Consistent with these previous studies, our study might imply the potential buffering effect of preference for positive information.
LIMITATIONS
This study has several limitations. First, this cross-sectional survey was conducted through the Questionnaire Star online survey platform, and the URL link was distributed through the geriatric mental health service network by members of the Chinese Society of Geriatric Psychiatry. All response participants were willing to actively engage in the discussion on psychology-related topics related to the effects of COVID-19. Response bias may exist if the nonrespondents lacked external support resources or avoided the topic of mental health. Second, our study implied that the age differences of demographic characteristics and COVID-19 related experiences might buffer the stressful response and the effect of COVID-19 on mental health status. However, the uneven distribution of age in this study sample did not allow further statistical analysis. Therefore, further exploration on the age-related mental health status among caregivers was warranted. Third, Type I error rate may have arisen due to the multiple group comparisons of the participants’ demographic characteristics, and the degree of community-level infection contact. Last, our study was conducted during the period in which the strictest epidemic prevention and control management measures were implemented, so there were no responses from Hubei Province. More than 400 mental health workers were sent to Hubei Province to provide psychological rescue. The local residents might have received timely psychological support to some extent. Also, the local residents may be primarily concerned about their physical health after the epidemic; mental health problems may not be the priority. In the future, it may be worthwhile to conduct in-depth studies to explore the trajectory of mental health status.
CONCLUSION
In this survey of caregivers of older adults during the COVID-19 epidemic, caregivers responding to the spread of COVID-19 reported high rates of mental health problems. Being female and having community-level COVID-19 contact were independent risk factors for experiencing multiple mental health problems. Compared with normal comparison, caregivers with preexisting mental disorders exhibited increased risk of multimorbidity, while those who accessed more positive media information exhibited decreased risk of multimorbidity. We suggest taking preventive and early intervention measures to support caregivers during the postepidemic era.
DECLARATIONS
Ethics Approval and Consent to Participate
The study was approved by the research ethics committee of Peking University Institute of Mental Health (Sixth hospital), and all participants provided informed consent through online survey system.
Consent for Publication
Not applicable.
Availability of Data and Material
The dataset generated and analyzed during the current study are not publicly available because we are preparing an additional manuscript. However, they are available upon the reasonable request to the corresponding author.
Funding
The data collection and analysis were supported by the National Key Research and Development Project, Ministry of Science and Technology of China (2017YFC1311100) and Beijing Municipal Science and Technology Commission (D171100008217007). The funding agency had no role in the design of the study, in collection, analysis or interpretation of the data, in the writing, approval of the paper, or decision to submit the manuscript for publication.
Authors’ Contributions
QL and HZ contributed to the study design, data collection, analysis and interpretation, and drafted the manuscript. MZ, TL and WM contributed to the study design, data collection, analysis and interpretation. CA, YC, SL and WK contributed to the data collection, analysis and interpretation. XY and HW conceived the study and contributed to the interpretation of data and critical revision of the manuscript. All authors read and approved the final manuscript. HW had primary responsibility for the final content.
We thank the participants of the study for their time and the members of Chinese Society of Geriatric Psychiatry for their support for the subject recruitment.
The authors declare that they have no competing interests.
Footnotes
No Disclosures to Report.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jagp.2021.01.006.
Appendix. SUPPLEMENTARY MATERIALS
Table S1. Comparisons of demographic characteristics and COVID-19-related experiences among those aged below and over 60 years. Table S2. Univariate and multiple logistic regression analysis of factors associated with anxiety, depression, and sleep problems.
REFERENCES
- 1.The novel coronavirus pneumonia emergency response epidemiology team, Chinese Center for Disease Control and Prevention: [the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Chinese J Epidemiol. 2020;41:145–151. [PMC free article] [PubMed] [Google Scholar]
- 2.Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12:240–249. [PubMed] [Google Scholar]
- 3.Wang H, Li T, Barbarino P, Gauthier S. Dementia care during COVID-19. Lancet. 2020;395:1190–1191. doi: 10.1016/S0140-6736(20)30755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H, Li T, Gauthier S. Coronavirus epidemic and geriatric mental healthcare in China: how a coordinated response by professional organizations helped older adults during an unprecedented crisis. Int Psychogeriatrics. 2020;32:1117–1120. doi: 10.1017/S1041610220000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qiu J, Shen B, Zhao M. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Boyle C, Robertson C, Secor-Turner M. Nurses’ beliefs about public health emergencies: fear of abandonment. Am J Infect Control. 2006;34:351–357. doi: 10.1016/j.ajic.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Chung BPM, Wong TKS, Suen ESB. SARS: caring for patients in Hong Kong. J Clin Nurs. 2005;14:510–517. doi: 10.1111/j.1365-2702.2004.01072.x. [DOI] [PubMed] [Google Scholar]
- 8.Khalid I, Khalid TJ, Qabajah MR. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim Y. Nurses’ experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control. 2018;46:781–787. doi: 10.1016/j.ajic.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu C, Wang H, Zhou L. Sources and symptoms of stress among nurses in the first Chinese anti-Ebola medical team during the Sierra Leone aid mission: a qualitative study. Int J Nurs Sci. 2019;6:187–191. doi: 10.1016/j.ijnss.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Honey M, Wang WY. New Zealand nurses perceptions of caring for patients with influenza. A (H1N1) Nurs Crit Care. 2013;18:63–69. doi: 10.1111/j.1478-5153.2012.00520.x. [DOI] [PubMed] [Google Scholar]
- 12.Chan SSC, Leung D, Chui H. Parental response to child's isolation during the SARS outbreak. Ambul Pediatr. 2007;7:401–404. doi: 10.1016/j.ambp.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwerdtle PM, De Clerck V, Plummer V. Experiences of Ebola survivors: causes of distress and sources of resilience. Prehosp Disaster Med. 2017;32:234–239. doi: 10.1017/S1049023X17000073. [DOI] [PubMed] [Google Scholar]
- 14.Chan SWC. Family caregiving in dementia: the Asian perspective of a global problem. Dement Geriatr Cogn Disord. 2011;30:469–478. doi: 10.1159/000322086. [DOI] [PubMed] [Google Scholar]
- 15.Caswell LW, Vitaliano PP, Croyle KL. Negative associations of chronic stress and cognitive performance in older adult spouse caregivers. Exp Aging Res. 2003;29:303–318. doi: 10.1080/03610730303721. [DOI] [PubMed] [Google Scholar]
- 16.Matua GA, Van Der Wal DM. Living under the constant threat of ebola: a phenomenological study of survivors and family caregivers during an ebola outbreak. J Nurs Res. 2015;23:217–224. doi: 10.1097/jnr.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 17.Chew QH, Wei KC, Vasoo S. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Med J. 2020:1–31. doi: 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Varalakshmi R, Swetha R. Covid-19 lock down: people psychology due to law enforcement. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Yu E, Tang Y, editors. Psychological Support and Counseling for Older Adults during the Outbreak of COVID-19. 1st ed. Chinese Medical Multimedia Press; Beijing: 2020. [Google Scholar]
- 20.Vahia IV, Blazer DG, Smith GS. COVID-19, mental health and aging: a need for new knowledge to bridge science and service. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He L, Tang S, Yu W. The prevalence, comorbidity and risks of prolonged grief disorder among bereaved Chinese adults. Psychiatry Res. 2014;219:347–352. doi: 10.1016/j.psychres.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 22.McCauley M, Minsky S, Viswanath K. The H1N1 pandemic: media frames, stigmatization and coping. BMC Public Health. 2013;13:1116. doi: 10.1186/1471-2458-13-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018;15:1643. doi: 10.3390/ijerph15081643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MacNeil A, Rollin PE. Ebola and marburg hemorrhagic fevers: neglected tropical diseases? PLoS Negl Trop Dis. 2012;6:1–7. doi: 10.1371/journal.pntd.0001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J, Ren Y, Huang H. Timely psychological care for patients with severe mental illness during COVID-19 epidemic. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;323:1343. doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- 27.He X, Li C, Qian J. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry. 2010;22:200–203. [Google Scholar]
- 28.Mitchell AJ, Yadegarfar M, Gill J. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open. 2016;2:127–138. doi: 10.1192/bjpo.bp.115.001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang YL, Liang W, Chen ZM. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pacific Psychiatry. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 30.Virta JJ, Heikkilä K, Perola M. Midlife sleep characteristics associated with late life cognitive function. Sleep. 2013;36:1533–1541. doi: 10.5665/sleep.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng SKW, Sheng B, Lau KK. Adjustment outcomes in Chinese patients following one-month recovery from severe acute respiratory syndrome in Hong Kong. J Nerv Ment Dis. 2004;192:868–871. doi: 10.1097/01.nmd.0000147169.03998.dc. [DOI] [PubMed] [Google Scholar]
- 32.Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai J, Ma S, Wang Y. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duarte ESR, Silveira LVDA, Cítero V de A. Common mental disorder among family carers of demented older people in Brazil. Dement e Neuropsychol. 2018;12:402–407. doi: 10.1590/1980-57642018dn12-040010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elizarrarás-Rivas J, Vargas-Mendoza JE, Mayoral-García M. Psychological response of family members of patients hospitalised for influenza A/H1N1 in Oaxaca. Mexico. BMC Psychiatry. 2010:10. doi: 10.1186/1471-244X-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu HZY, Low L-F, Xiao S. Differences in psychological morbidity among Australian and Chinese caregivers of persons with dementia in residential care. Int J Geriatr Psychiatry. 2009;24:1343–1351. doi: 10.1002/gps.2264. [DOI] [PubMed] [Google Scholar]
- 37.Krause NM, Freiling I, Beets B. Fact-checking as risk communication: the multi-layered risk of misinformation in times of COVID-19. J Risk Res. 2020;0:1–8. [Google Scholar]
- 38.McAlonan GM, Lee AM, Cheung V. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 39.Chatterjee SS, Barikar CM, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J Psychiatr. 2020;51:2018–2019. doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xiang YT, Zhao YJ, Liu ZH. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. 2020;16:1741–1744. doi: 10.7150/ijbs.45072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhu H. Unmet needs in long-term care and their associated factors among the oldest old in China. BMC Geriatr. 2015;15:1–11. doi: 10.1186/s12877-015-0045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Armitage L, Lawson BK, Whelan ME. Paying SPECIAL consideration to the digital sharing of information during the COVID-19 pandemic and beyond. BJGP Open. 2020 doi: 10.3399/bjgpopen20X101072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Majumder MS, Mandl KD. Early in the epidemic: impact of preprints on global discourse about COVID-19 transmissibility. Lancet Glob Heal. 2020;8:e627–e630. doi: 10.1016/S2214-109X(20)30113-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun M, Li S, Yue H. Analysis on anxiety status of Chinese Netizens under the outbreak of the Coronavirus disease 2019 (COVID-19) and its influencing factors. Modernization of Traditional Chinese Medicine and Materia Materia—World Science and Technology, 2020;22:703–708. [Google Scholar]
- 45.Wei N, Yang C, Wang X. The influence of the release of government information on public psychology during major public emergencies: data analysis based on the COVID-19 pandemic. Jiangsu Soc Sci. 2020;03:10–22. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Comparisons of demographic characteristics and COVID-19-related experiences among those aged below and over 60 years. Table S2. Univariate and multiple logistic regression analysis of factors associated with anxiety, depression, and sleep problems.
Data Availability Statement
The dataset generated and analyzed during the current study are not publicly available because we are preparing an additional manuscript. However, they are available upon the reasonable request to the corresponding author.