Abstract
COVID-19-associated coagulopathy (CAC) is a feature of COVID-19 that can lead to various thrombotic complications and death. In this review, we briefly highlight possible etiologies, including direct cytotoxicity caused by the SARS-CoV-2 virus, and the activation of proinflammatory molecules such as cytokines, underlying coagulopathy. Endothelial dysfunction has been highlighted as pivotal, irrespective of the mechanism involved in CAC. Specific features of CAC distinguishing it from disseminated intravascular coagulopathy and sepsis or ARDS-associated coagulopathy have been discussed. We have also highlighted some hematological parameters, such as elevated d-dimers and partial prothrombin and prothrombin times prolongation, which can guide the use of anticoagulation in critically ill patients. We conclude by highlighting the importance of prophylactic anticoagulation in all COVID-19 hospitalized patients and reiterate the need for institution-specific guidelines for anticoagulation COVID-19 patients since individual institutions have different patient populations.
Keywords: Covid-19, Sars-cov-2, Anticoagulation, d-dimers, Coagulation, Thrombosis
Introduction
The Coronavirus disease-19 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has since reached pandemic proportions after first reported in Wuhan, China.1 The number of deaths has surpassed 2,000,000 worldwide with more than 400,000 reported in the USA alone, and unfortunately, this number is projected to increase. The case-fatality rate for COVID-19 depends on many factors and ranges from 0.3 deaths per 1000 cases to 304.9 deaths per 1000 cases in patients aged 5–17 years and ≥85 years in the US, respectively. The case fatality is as high as 40% in ICU hospitalized patients.2 , 3
The SARS-CoV-2 virus is known to cause clinical symptoms of varying severity, ranging from common flu-like symptoms to death, especially in the elderly and in patients with comorbidities. However, recent data have shown increased vulnerability of the young and healthy to the virus. A major factor contributing to the difficulty managing COVID-19 is the multifaceted nature of its presentation at different stages.4 One such presentation/complication is COVID-19-associated coagulopathy leading to thrombosis, multi-organ damage, and death. Therefore, it is imperative to have a clear understanding of the mechanisms of COVID-19-associated coagulopathy. Herein, we discuss current knowledge on this topic, including hematologic parameters associated with COVID-19-associated coagulopathy and current guidelines on the use of anticoagulation therapy in affected patients.
Pathogenesis of intravascular coagulation in COVID-19
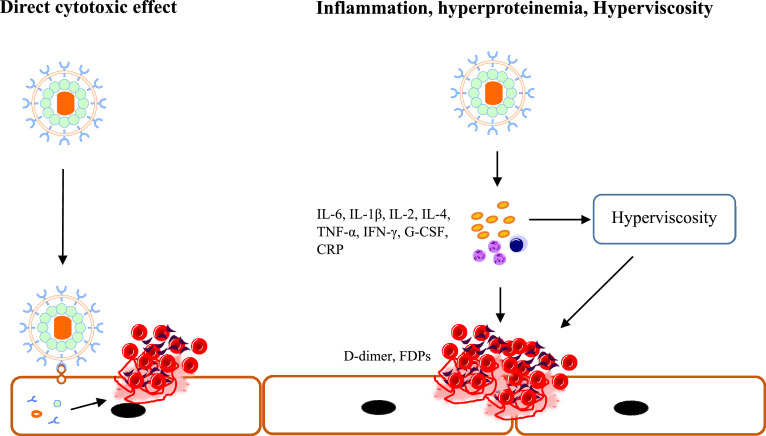
One of the concerning features of COVID-19 is coagulopathy leading to intravascular coagulation thought to be a major contributing factor to mortality. Direct evidence of microvascular thrombosis in COVID-19 patients has been demonstrated in autopsied cadavers.5 The documented characteristic features of COVID-19-associated coagulopathy include elevated d-dimer, fibrinogen, and platelet counts, and prolongation of prothrombin time all promoting a prothrombotic state that favors venous thromboembolism observed in critically ill patients, irrespective of pharmacological thromboprophylaxis.6 , 7 Although the detailed mechanism of COVID-19-associated coagulopathy has not been fully elucidated, the current school of thought implicates endothelial dysfunction as crucial. It has been established that SARS-CoV-2 infection induces a proinflammatory state leading to the activation of proinflammatory molecules including cytokines such as IL-6, IL-1β, IL-2, IL-4, tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), granulocyte-colony stimulating factor, as well as C-reactive protein (CRP), and d-dimer. The changes in proinflammatory cytokines in the early stages of the infection differ from those observed in other viral and bacterial infections and seem to correlate with the severity of the disease; however, as the disease progresses, the cytokine profile becomes more like that seen in ARD.8 , 9 The alterations in inflammatory parameters further promote a pro-inflammatory state with numerous proinflammatory cells in the circulatory system perpetuating endothelial damage and platelet activation leading to aberrant activation of coagulation (Fig. 1 ). Also, this proinflammatory hyperproteinemic state induced by SARS-CoV-2 may lead to a COVID-19-associated hyper-viscous state thought to be an important link between inflammation and coagulopathy in critically ill COVID-19 patients.10
Fig. 1.
Mechanisms involved in aberrant coagulation in COVID-19
SARS-CoV-2 enters host cells via interaction of its spike protein with the ACE2 receptor on the surface of ECs (left). This entry can cause direct virus-mediated EC damage leading to activation of the coagulation cascade. EC damage and thromboinflammation can also be caused by the hyperinflammatory state, characterized by hyperproteinemia and hyperviscosity, promoted by SARS-CoV-2 which causes inhibition of IFN signaling, while simultaneously promoting the production of proinflammatory cytokines such as IL-6 and TNFα (Right).
SARS-CoV-2; severe acute respiratory syndrome coronavirus 2, EC; endothelial cells, IFN; interferon, IL; interleukin, TNF;tumor necrosis factor, G-CSF; granulocyte colony-stimulating factor, CRP; c-reactive protein.
The direct cytotoxic effects of the SARS-CoV-2 virus on endothelial cells represent another mechanism by which the virus can promote endotheliopathy and coagulopathy. This mechanism is supported by the detection of viral inclusions in endothelial cells from autopsied specimens of COVID-19 patients–vascular endothelial cells express the ACE2 receptor and ACE2 is expressed on the surface of the SARS-CoV-2 virus.11 , 12 Further, Goshua et al. showed that the levels of von Willebrand factor (VWF) antigen, soluble P-selectin, and factor VIII activity, were significantly elevated in laboratory-confirmed COVID-19 patients admitted to the intensive care unit (ICU), further highlighting a state of endothelial activation/damage during infection.13 Of note, mortality was also significantly correlated with the levels of VWF antigen and soluble thrombomodulin in all patients.
Parameters associated with thrombosis in patients with COVID-19
Because dysfunctional activation of coagulation plays a critical role in the etiology of COVID-19, identifying parameters associated with such aberrant activation is critical in mitigating disease course. Using the Padua prediction score, Wang et al. evaluated the risk for venous thromboembolism (VTE) in COVID-19 patients and found that of the 1026 patients included in their study, those with a high score (i.e., Padua score of ≥4) were more likely to be admitted to the ICU, to be mechanically ventilated, and to die of COVID-19 or its complications, such as VTE.14 Of note, when compared with low-risk patients and after adjusting for age, those at a high risk of VTE had abnormal levels of aspartate aminotransferase (ASP), alanine aminotransferase, and C-reactive protein as seen in earlier results from Wuhan, China demonstrating elevated ASP in COVID-19.15
Studies showing hematological parameters associated with an increased risk for coagulopathy and widespread arterial and venous thrombosis have been done. Tang et al. retrospectively analyzed data from 183 COVID-19 patients and found that in the non-survivors, who constituted 11.5% of their study population, significantly higher d-dimer and fibrin degradation product (FDP) levels, longer prothrombin time (PT), and activated partial thromboplastin (APTTT) time were noted, when compared with survivors. Interestingly, >70% of non-survivors met criteria for disseminated intravascular coagulopathy (DIC), with only <1% of their surviving counterparts meeting the same criteria.16 Cui et al. also reported significant longer APTT and higher D‐dimer concentrations in severe COVID-19 cases and further noted that when a 1.5 µg/mL d-dimer cut-off value for predicting VTE was implemented in their cohort, the sensitivity, specificity, and the negative predictive value was 85.0%, 88.5%, and 94.7%, respectively.17 Several other studies have shown d-dimer levels, fibrinogen levels, and APTT, as good indices for identifying patients at high-risk for VTE and in predicting disease severity.18 , 19 These studies, therefore, implicate dysregulated coagulation as an essential aspect in the evolution of COVID-19 since it is associated with both disease severity and mortality. Therefore, earlier stratification of patients, based on these parameters, can be critical in decreasing mortality.
A recent study by Lioa et al. of 380 COVID-19 patients showed that thrombocytopenia (i.e., a platelet count <100 × 109 cells/L), prolonged prothrombin time (i.e., >16 s), and increased d-dimer levels were significantly higher in those with critical disease and associated with increased mortality. Significantly higher levels of fibrin degradation products were associated with disease severity as well and, interestingly, death was associated with an increased neutrophil to lymphocyte ratio (i.e., a ratio ≥9).18 Other hematological parameters not directly linked to the coagulation cascade have been associated with disease severity and mortality in COVID-19 patients and these parameters, in addition to the ones discussed above, have been summarized in table 1 .
Table 1.
Hematologic parameters associated with COVID-19 coagulopathy.
| Parameters | Association | Reference |
|---|---|---|
|
Disease severity, mortality | 18 |
|
Organ dysfunction and mortality | 42 |
|
Severity and mortality | 18 |
|
Severity and mortality | 18 |
|
Mortality | 18 |
|
Disease severity, mortality | 6,18 |
|
Unknown association | 20, 36, 43 |
PT; prothrombin time: APTT; activated partial thromboplastin time: FDPs; fibrinogen degradation products: vWF; von Willebrand Factor.
It is important to highlight that the coagulopathy observed in COVID-19 is different from classic DIC seen in bacterial sepsis. The most common pattern of COVID-19-associated coagulopathy in mild to moderate cases is characterized by elevated fibrinogen and d-dimer levels along with the rise in parameters of inflammation such as CRP. The prolongation of the aPTT and/or PT is only minimal, and thrombocytopenia is mild with platelet counts of about 100 × 109/L. In critically ill COVID-19 patients, coagulopathy is characterized by moderate to severe thrombocytopenia, i.e., platelet count <50 × 109/L, prolongation of the PT and aPTT, higher levels of d-dimer, and fibrinogen < 1.0 g/L, resembling overt DIC. It has been recently suggested that the prolongation of aPTT is caused by the presence of lupus anti-coagulant after one study found that of 35 patients with prolonged aPTT on admission, more than 90% were positive for lupus anticoagulant, the presence of which, if persistent, can be associated with a thrombotic tendency within the antiphospholipid syndrome.20
Current anticoagulation guidelines for COVID-19 patients
Since the initial report from Wuhan suggested that elevated d-dimers and prolonged PT were among the baseline features of critically ill COVID-19 patients,15 the actual burden of VTE complications in these patients has been confirmed, and the current incidence is between 16 and 49% in ICU admitted COVID-19 patients.21 , 22 Current evidence, seen on autopsied lung specimens, indicate microvascular thrombosis as a contributor to hypoxemic respiratory failure in COVID-19 patients.5 Thus, therapeutic anticoagulation is expected to positively impact outcomes in COVID-19 patients. However, the benefit of therapeutic anticoagulation is currently controversial based on the retrospective and cross-sectional studies that have been carried out.23 , 24 While awaiting concrete data from randomized controlled trials to support changes in current practice, current guidelines support anticoagulating critically ill COVID-19 patients. Whether critically ill COVID-19 patients should receive therapeutic anticoagulation in the absence of confirmed VTE remains unknown at large.
Current general guidelines for managing coagulopathy in COVID-19 patients have been set forth by leading societies in the field, such as the American society of hematology (ASH), International Society of Thrombosis and Haemostasis (ISTH), and the American College of Cardiology.25., 26., 27. Per the current recommendations, prophylactic dose LMWH is recommended for all hospitalized COVID-19 patients in the absence of active bleeding or except when the platelet count is < 25 × 109/L or fibrinogen levels is < 0.5 g/L. Per these guidelines, abnormal PT or aPTT is not a contraindication for pharmacological thromboprophylaxis, and when pharmacological thromboprophylaxis is contraindicated, mechanical thromboprophylaxis should always be used. These guidelines are based on evidence that markedly elevated D‐dimer levels are associated with increased mortality in COVID‐19 patients, and that multi‐organ failure is more likely in septic patients who develop coagulopathy; therefore, inhibiting thrombin generation may reduce mortality.28 , 29 Besides, LMWH is known to have anti‐inflammatory properties which could provide added benefit to COVID patients who have marked elevation of pro‐inflammatory cytokines.15 , 25 , 30 , 31
The current guidelines endorsed by these societies are general, leaving room for modifications to meet the needs of specific institutions. For example, specifics on when and how often d-dimers should be measured are institution-specific. However, when patients present to the emergency department or outpatient clinic, obtaining a baseline d-dimer level is considered appropriate and studies have established that a cut off value of >1 μg/mL can stratify patients at higher risk of poor outcomes.17 For institution-specific guidelines, the reader is directed to the websites of different institutions such as the Brigham and Women's Hospital, Massachusetts General Hospital, and the University of Washington to access the most recent up to date protocols and guidelines.32., 33., 34.
Though the benefits of anticoagulating COVID-19 patients still need validation via randomized clinical trials, promising outcomes have already been documented in small scale studies such as that by Tang et al.35 However, as demonstrated by another study, prophylactic anticoagulation can be insufficient in most COVID-19 patients with ARDS, suggesting that therapeutic doses may be needed.36 Randomized clinical trials to compare the efficacy and safety of high versus low LMWH dosages in hospitalized patients with severe COVID-19 pneumonia and coagulopathy are ongoing.37 Such studies, in addition to ongoing ones interrogating the use of other treatment modalities such as convalescent plasma, ramdesevir, and dexamethasone will shed more light on how COVID-19 coagulopathy can be better managed.38., 39., 40., 41., 42., 43.
In conclusion, COVID-19 represents a hypercoagulable state that contributes to increased mortality. The pathways causing aberrant coagulation in COVID-19 involve a complex interplay of multiple pathways. Clinical trials are ongoing to fully elucidate these pathways, determine optimal doses of anticoagulation therapies, and study other treatment modalities. In the meantime, general guidelines for anticoagulation have been put in place by societies such as ASH and ISTH, with modifications to suit the needs of specific institutions encouraged.
Declaration of Competing Interest
None.
Acknowledgments
This work was supported by HCA Healthcare and/or an HCA healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus Disease 2019 (COVID-19): a Review. JAMA. 2020 doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 3.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A., Madhavan M.V., K Sehgal, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. (2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox E.S., Akmatbekov A., Harbert J.L., et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8:681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panigada M., Bottino N., Tagliabue P., et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song J.W., Zhang C., Fan X., et al. Immunological and inflammatory profiles in mild and severe cases of COVID-19. Nat Commun. 2020;11:3410. doi: 10.1038/s41467-020-17240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson J.G., Simpson L.J., Ferreira A., et al. Cytokine profile in plasma of severe COVID-19 does not differ from ARDS and sepsis. JCI Insight. 2020 doi: 10.1172/jci.insight.140289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maier C.L., Truong A.D., Auld S.C., et al. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? Lancet. 2020;395:1758–1759. doi: 10.1016/S0140-6736(20)31209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ackermann M., Verleden E.S., Kuehnel M., et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varga Z., Flammer A.J., Steiger P., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goshua G., Pine A.B., Meizlish M.L., et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T., Chen R., Liu C., et al. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol. 2020;7:e362–e363. doi: 10.1016/S2352-3026(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang N., Li D., Wang X., Sun Z., et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cui S., Chen S., Li X., Liu S., Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liao D., Zhou F., Luo L., et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 2020:S2352–S3026. doi: 10.1016/S2352-3026(20)30217-9. 30217-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowles L., Platton S., Yartey N., et al. Lupus anticoagulant and abnormal coagulation tests in patients with Covid-19. N Engl J Med. 2020;383:288–290. doi: 10.1056/NEJMc2013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nahum J., Morichau-Beauchant T., Daviaud F., et al. Venous thrombosis among critically Ill patients with Coronavirus Disease 2019 (COVID-19) JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paranjpe I., Fuster V., Lala A., et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pesavento R., Ceccato D., Pasquetto G., et al. The hazard of (sub)therapeutic doses of anticoagulants in non-critically ill patients with Covid-19: the Padua province experience. J Thromb Haemost. 2020 doi: 10.1111/jth.15022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thachil J., Tang N., Gando S., et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bikdeli B., Madhavan M.V., Jimenez D., et al. COVID-19 and Thrombotic or Thromboembolic Disease: implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shankar-Hari M., Phillips G.S., Levy M.L., et al. Developing a new definition and assessing new clinical criteria for septic shock for the third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iba T., Levy J.H., Warkentin T.E., et al. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17:1989–1994. doi: 10.1111/jth.14578. [DOI] [PubMed] [Google Scholar]
- 30.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Poterucha T.J., Libby P., Goldhaber S.Z. More than an anticoagulant: do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017;117:437–444. doi: 10.1160/TH16-08-0620. [DOI] [PubMed] [Google Scholar]
- 32.Hematology . 2020. Brigham and Women's Hospital COVID-19 Clinical Guidelines.https://covidprotocols.org/protocols/hematology Accessed September 23. [Google Scholar]
- 33.COVID-19 Treatment Guidance. https://www.massgeneral.org/news/coronavirus/treatment-guidance. Accessed September 23, 2020.
- 34.19 Resource Site . 2020. COVID.https://covid-19.uwmedicine.org/Pages/default.aspx Accessed September 23. [Google Scholar]
- 35.Tang N., Bai H., Chen X., et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helms J., Tacquard C., Severac F., et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marietta M., Vandelli P., Mighali P., et al. Randomised controlled trial comparing efficacy and safety of high versus low Low-Molecular Weight Heparin dosages in hospitalized patients with severe COVID-19 pneumonia and coagulopathy not requiring invasive mechanical ventilation (COVID-19 HD): a structured summary of a study protocol. Trials. 2020;21:574. doi: 10.1186/s13063-020-04475-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Banwait R.S., Salabei J.K., Fishman T.J., Iyer U.G. Convalescent plasma in COVID-19. HCA Healthc J Med. 2020;1:139–146. doi: 10.36518/2689-0216.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Y., Zhang D., Du G., et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y., Zhou F., Zhang D., et al. Evaluation of the efficacy and safety of intravenous remdesivir in adult patients with severe COVID-19: study protocol for a phase 3 randomized, double-blind, placebo-controlled, multicentre trial. Version 2. Trials. 2020;21:422. doi: 10.1186/s13063-020-04352-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abdolahi N., Kaheh E., Golsha R., et al. Letter to the editor: efficacy of different methods of combination regimen administrations including dexamethasone, intravenous immunoglobulin, and interferon-beta to treat critically ill COVID-19 patients: a structured summary of a study protocol for a randomized controlled trial. Version 2. Trials. 2020;21:549. doi: 10.1186/s13063-020-04499-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu C., Chen X., Cai Y., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:1–11. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Y., Xiao M., Zhang S., et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]