Abstract
Background
“Big Events” are major disruptions to physical, political, and economic environments that can influence vulnerability to drug-related harms. We reviewed the impacts of Big Events with relevance to the COVID-19 pandemic on drug-related risk and harms and access to drug treatment and harm reduction services.
Methods
We conducted a rapid review of quantitative, qualitative, and mixed methods literature relating to the following Big Events: respiratory infection pandemics, natural disasters, financial crises, and heroin shortages. Included studies reported data on changes to risks, harms, and/or service provisioning for people who use illicit drugs (other than cannabis) in the context of these Big Events. Searches were conducted in PubMed in May 2020, and two reviewers screened studies for inclusion. Peer-reviewed studies published in English or French were included. We used a narrative synthesis approach and mapped risk pathways identified in the literature.
Results
No studies reporting on respiratory infection pandemics were identified. Twelve studies reporting on natural disaster outcomes noted marked disruption to drug markets, increased violence and risk of drug-related harm, and significant barriers to service provision caused by infrastructure damage. Five studies of the 2008 global financial crisis indicated increases in the frequency of drug use and associated harms as incomes and service funding declined. Finally, 17 studies of heroin shortages noted increases in heroin price and adulteration, potentiating drug substitutions and risk behaviors, as well as growing demand for drug treatment.
Conclusion
Current evidence reveals numerous risk pathways and service impacts emanating from Big Events. Risk pathway maps derived from this literature provide groundwork for future research and policy analyses, including in the context of the COVID-19 pandemic. In light of the findings, we recommend responding to the pandemic with legislative and financial support for the flexible delivery of harm reduction services, opioid agonist treatment, and mental health care.
Keywords: People who use drugs, Injecting drug use, Harm reduction, Illicit drugs, COVID-19, Disaster preparedness
In December 2019, a pneumonia outbreak in China led to the isolation of the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Gorbalenya et al., 2020). Infection with this coronavirus manifests in a broad spectrum of clinical symptoms, designated by the World Health Organization (WHO) as coronavirus disease 2019 (COVID-19). COVID-19 was declared a global pandemic by WHO in March 2020 (WHO, 2020). Worldwide public health responses have included the declaration of health emergencies; SARS-CoV-2 case-finding and testing; contact tracing; closures of schools and non-essential businesses; bans on social gatherings; shifting healthcare resources to prepare for possible influxes of COVID-19 patients; restructuring of health and social services to minimize physical interactions; and promotion of “physical distancing” between people outside of the home.
The potential for COVID-19 to disproportionately affect marginalized population groups such as people who use drugs (PWUD) was rapidly recognized in relation to both SARS-CoV-2 exposure risk and broader challenges including potential drug market instability and the decreased capacity of health and social services to carry out their usual functions. For example, the closure of national borders in response to COVID-19 has interrupted global illicit drug supply chains, with uncertain effects for drug availability, price, and purity (Gomis, 2020; UNODC, 2020). Drug market disruption may subsequently increase the risk that people who use drugs will experience withdrawal or will use drugs contaminated by potentially deadly adulterants such as fentanyl (RCCET, 2020).
Compounding this risk, many low-threshold services upon which PWUD may rely to meet essential needs (e.g. food, shelter, medicines) or reduce harms associated with drug consumption (e.g. needle-syringe programs, supervised injection sites, naloxone trainings) have temporarily closed or reduced capacity to accommodate physical distancing requirements (Ahsan, 2020; EMCDDA, 2020; Glick et al., 2020; Jeffords, 2020; Lam, Sankey, Wyman, & Zhang, 2020). Women who use drugs may be particularly affected by these changes given existing gender-related barriers to accessing services and exposure to gendered violence (Collins, Boyd, Czechaczek, Hayashi, & McNeil, 2020; Malinowska-Sempruch, 2015). The impacts of the COVID-19 pandemic are still emerging, but increased risks of overdose and other drug-related harms are expected across a range of outcomes for people who use drugs (Chang, Agliata, & Guarinieri, 2020; Jacka, Phipps, & Marshall, 2020; Schlosser & Harris, 2020).
Using a “Big Events” lens to assess possible impacts of the COVID-19 pandemic
The term “Big Events” is used to refer to environmental, economic, and other major disruptions that create social instability (Friedman, Rossi, & Braine, 2009). Examples include natural disasters, political transitions, and economic recessions. Though their impacts differ, all Big Events have the potential to cause profound changes to the risk environment for drug-related harm (Friedman et al., 2009; Rhodes, 2002). Factors determining likely outcomes may include the particular type of disruption engendered by the event (e.g., physical infrastructure damage vs. social unrest) and the geographic and temporal scales across which destabilizing effects occur. These factors can vary widely; while a natural disaster such as a hurricane may create instability in a city, nation, or region, the impacts of economic recession can reach around the globe. And, though hurricanes generally cause infrastructure damage and population displacement, the time required to rebuild and resettle can range from months to years. Evidently, not all Big Events are created equal. However, even brief periods of social instability can seriously impact marginalized groups of people, whose social precarity leaves them more vulnerable to the harms engendered by major disruptions.
The COVID-19 pandemic is a major health crisis that has also profoundly disrupted economic systems, physical mobility, and social practices across the globe (Xu, 2020); impacts on local drug-use risk environments may therefore be multifaceted and complex (Rhodes, 2009). Studies of previous Big Events can provide insight into possible short- and medium-term effects of the COVID-19 pandemic on drug markets, people who use drugs, and relevant services. We therefore reviewed original research studies assessing the impacts of Big Events on:
1) risk behaviors and drug-related harms among people who use drugs, and
2) the delivery of harm reduction and drug treatment services
Findings of this review can inform both responses to the COVID-19 pandemic and preparedness for future Big Events.
Methods
This review is registered with PROSPERO (registration no. CRD42020185079), and the protocol is published at https://osf.io/a8qtd/. The design of the review was informed by the Selecting Approaches for Rapid Reviews (STARR) tool (Pandor et al., 2019) and evidence synthesis approaches used in mixed methods syntheses (Hong, Pluye, Bujold, & Wassef, 2017).
Population
Included studies focused on people using illicit drugs (other than cannabis). Studies of people using cannabis, tobacco and/or alcohol without illicit drugs, or in which outcomes specific to illicit drug use could not be ascertained, were excluded.
Included Big Events
To support rapid completion, the review was limited to categories of Big Events with attributes of relevance to the COVID-19 pandemic (Supplementary Figure 1). These were:
Recent respiratory infection pandemics (e.g., SARS, MERS, H1N1). As events within the same Big Event category as the COVID-19 pandemic, these may hold lessons for drug-related risk and service delivery in a pandemic context. Relative to COVID-19, however, previous pandemics were limited in their geographic spread, effects on the global economy, and impact on health and social services.
Natural disasters (e.g., Hurricane Katrina). Major forms of disruption characterizing Big Events in this category include large-scale displacement, traumatic disaster exposure, and sudden and significant damage to physical infrastructure, including housing and hospitals. Severe weather events affect the physical availability of services, which may provide insight into the outcomes of service closures implemented in response to the pandemic. Both natural disasters and the current pandemic represent significant disruptions of daily life. While both may engender psychological distress, however, severe weather events are more likely to potentiate trauma and acute suffering compared to the COVID-19 pandemic.
Economic crises (e.g., the Global Financial Crisis). Major disruptions resulting from an economic crisis include job loss, financial and relational stress, and reduced funding for harm reduction services. COVID-19 is both a health and an economic crisis, with significant impacts on global productivity, financial markets, and the functioning of supply chains (McKibbin & Fernando, 2020). All of these factors affect employment and income opportunities; research on prior economic crises may therefore be pertinent to response planning over time. The Global Financial Crisis, however, reflected market forces, differentiating it from the current economic crisis, engendered by mandates restricting activities that could spread the virus. This distinction may play a role in determining economic recovery and eventual outcomes (Alini, 2020).
The Australian heroin shortage of 2001. This was a sharp, time-limited drug market shock with well-documented consequences for drug-related risk, harms, and service delivery. Heroin shortages represent a major disruption of the drug market, which may manifest in changes to drug prices and purity. While an acute shortage may last only a few months, its reverberations can be felt longer-term as drug markets slowly readapt. Given emerging reports of drug market disruption due to COVID-19 (RCCET, 2020), we considered this literature to have potentially important implications for COVID-19 responses. During study screening, we decided to also include studies reporting on other heroin shortages if they provided information on our outcomes of interest. Unlike the current pandemic, the direct effects of drug shortages are limited to the drug market and do not necessarily impact service availability.
Outcomes
Preliminary searches identified that a broad range of outcomes with implications for COVID-19 responses have been examined in the Big Events literature. We defined two categories of outcomes of interest: 1) changes in drug-related risk and harms following Big Events (e.g., ER visits, overdoses, drug market violence, initiation of injecting among people who use drugs, increased frequency or amount of drug use by individuals) and 2) challenges and responses in harm reduction and drug treatment service delivery following a Big Event (e.g., changes in treatment demand or utilization; resource shortages; service adaptations; changes to clinical guidance). We extracted data for all outcomes that met these definitions, including outcomes assessed both cross-sectionally (e.g., by asking participants to identify changes since a Big Event) and longitudinally (e.g., with pre- and post-Event data collection).
Search strategy
Search strings were developed with reference to those used in previous reviews of the epidemiology of drug-related harms (Degenhardt et al., 2017) and by comparing results to previous ad hoc searches of the Big Events literature to ensure capture of known studies (see supplementary materials). Searches were limited to the PubMed database as test searches found that additional databases (Embase, PsycInfo) did not identify new studies. Reference lists of included papers were hand-searched for additional relevant publications. Two restrictions were pre-specified due to time and resource constraints: studies must have been published in English or French, and in peer-reviewed journals (i.e. no grey literature searches).
Inclusion criteria
Preliminary searches suggested that an inclusive approach was needed to adequately capture relevant data. As such, we included quantitative, qualitative, and mixed methods studies of any design that focused on the outcomes of a Big Event as defined above, and reported data on at least one of the outcome categories listed above.
Study selection
Screening and study selection were completed using Covidence (Veritas Health Innovation). Title and abstract screening, and second-stage full-text review were carried out independently by two reviewers, with disagreements resolved through team discussion.
Quality assessment of included studies
Quality assessment was completed using the Mixed Methods Appraisal Tool, which allows for assessment of quantitative, qualitative and mixed methods studies (Hong et al., 2018). The tool assesses studies based on five domains: 1) approach rationale, 2) data collection methods, 3) data completeness/integration, 4) data interpretation, and 5) coherence of analysis, with domain criteria varying according to the study design. Response options for each domain are “yes”, “no”, and “can't tell.” The authors of the tool discourage the calculation of an overall score, instead encouraging an assessment of strengths and weaknesses of the body of literature under review (Hong et al., 2018).
Data extraction and synthesis
Data were extracted into a spreadsheet recording study bibliographic details, Big Event type, and findings relevant to the outcomes of interest. During extraction, a team member reviewed the results and discussion sections of each study, noted outcomes of interest, and summarized findings relating to each outcome. To maximize efficiency, data for each study were extracted once and then reviewed by another team member to verify accuracy.
Given the mixed methods nature of this review, we used a narrative synthesis approach (Popay et al., 2006). Extracted data were categorized by event type (e.g., natural disaster, heroin shortage) and by outcome measure (harms/risks or service provision), then summarized and synthesized within each category. Our specific outcomes served as organizing principles for synthesis; grouping all information relating to each outcome allowed us to note patterns across studies. Qualitative and quantitative data from distinct studies often complemented each other to form a more nuanced picture of Big Event outcomes. Where results disagreed regarding the impact of Big Events, the context of each study was considered.
Drawing upon Friedman, Rossi, and Braine's pathways model of Big Events and drug-related harm (Friedman et al., 2009), we developed a map of risks and harms as documented in the literature for each Event type. Using the data extraction spreadsheet and guided by our outcomes of interest, the relationships between antecedents, risk factors, behaviors, and outcomes reported in each study were noted and then represented visually using diagrams.net, a free online diagramming program.
Results
Overview of included studies
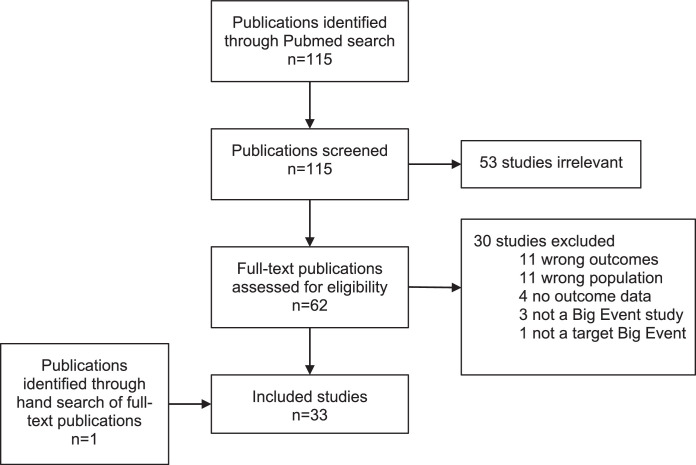
The search identified 116 publications for screening: 115 from the PubMed search, and an additional publication identified through hand searching of reference lists. Thirty-three publications were included after screening and full-text review (Fig. 1 ). Although the search included keywords relating to previous respiratory infection pandemics, we identified no studies reporting on this Big Event type in relation to people who use drugs or drug-related services. Of the three remaining Big Event categories, the largest number of publications related to heroin shortages (n = 17) (Supplementary Figure 2). Of these, one study from Hungary reported on the aftermath of a heroin shortage coinciding with an economic recession and austerity measures. Twelve publications reported on natural disasters, and a further four on economic crises. There were eight qualitative studies, 20 quantitative studies, and four mixed methods studies. Characteristics of included studies are shown in Table 1, Table 2, Table 3 .
Fig. 1.
Study flow diagram.
Table 1.
Characteristics of included publications contributing information on natural disasters.
| First author, year | Country | Big Event studied | Population | Study design and methods | Included outcomes |
|---|---|---|---|---|---|
| Bennett et al., 2011 | USA | Hurricane Katrina | Low-income people who use and sell drugs and were evacuated from New Orleans | Qualitative: cross-sectional ethnographic observation, focus groups, interviews | Changes in the New Orleans drug market and drug use patterns. Drug market violence linked to changing market conditions. |
| Cepeda et al., 2010 | USA | Hurricane Katrina | Low-income Black people who use drugs and were evacuated from New Orleans to Houston | Mixed methods: quantitative & qualitative semi-structured interviews; supplemental qualitative in-depth interviews | Changes in drug use patterns. |
| Dunlap et al., 2012 | USA | Hurricane Katrina | People who use and sell drugs in New Orleans | Qualitative: longitudinal ethnographic observation, focus groups, interviews | Changes in the New Orleans drug market and drug use patterns. Drug market violence linked to changing market conditions. |
| Gupta et al., 2017 | USA | Hurricane Sandy | Staff from two opioid maintenance programs in New York City | Mixed methods: qualitative interviews; quantitative review of local electronic health record data, including urine toxicology and retention rates | Resources shortages (lack of space). Changes in clinical guidance (take-home doses). |
| Kotarba et al., 2010 | USA | Hurricane Katrina | People who use and/or sell drugs in New Orleans relocated to Houston | Qualitative: longitudinal ethnographic observation, interviews | Changes in Houston drug market and drug use patterns following the entry of New Orleanian evacuees. Drug market violence linked to changing market conditions. |
| Matusow et al., 2018 | USA | Hurricane Sandy | Opioid treatment program staff and clients in New York and New Jersey. People not in treatment who use drugs in New York and New Jersey. | Qualitative: cross-sectional interviews; review of emergency plans. | Changes in clinical guidance (take-home doses). Resource shortages (transportation, communication). Changes in drug use patterns as a result of clinical shortages. |
| Maxwellet al., 2009 | USA | Hurricanes Katrina & Rita | Clients and staff of substance misuse treatment programs in Texas | Mixed methods: quantitative analysis of client data; qualitative interviews | Changes in demand for services. Resource shortages (electricity). |
| McClure et al., 2014 | USA | Hurricane Sandy | Providers and administrators of opioid maintenance treatment in New York | Qualitative: interviews | Changes in service operations. Resource shortages (physical space). |
| Pouget et al., 2015 | USA | Hurricane Sandy | People who inject drugs in New York City | Mixed methods: qualitative & quantitative semi-structured interviews | Changes to drug-related risks/harms. Changes to drug market. Changes in clinical guidance (take-home doses). Changes in drug use patterns as a result of clinical shortages. |
| Tofighi, 2014 | USA | Hurricane Sandy | Clients of Bellevue Hospital Center's buprenorphine clinic in New York City | Mixed methods: qualitative & quantitative semi-structured interviews | Changes to service operations. Resource shortages (buprenorphine). Changes in drug use patterns as a result of clinical shortages. |
| Toriello et al., 2007 | USA | Hurricane Katrina | Clients and staff of the Bridge House treatment centre in New Orleans | Qualitative: longitudinal description | Changes in demand for services (client impairment). Resource shortages (staff health/morale). |
| Valdez et al., 2010 | USA | Hurricane Katrina | Latino immigrant day labourers in New Orleans | Qualitative: interviews | Risk of drug use initiation. Risk of BBV. |
Table 2.
Characteristics of included publications contributing information on the 2008 global financial crisis.
| First author, year | Country | Population | Study design and methods | Included outcomes |
|---|---|---|---|---|
| (Lakhdar & Bastianic, 2011) | France | People who use drugs in France | Quantitative: longitudinal review of national data; review of specialist/ethnographic studies | Changes in drug use patterns. |
| (Bruguera et al., 2018) | England, Spain, and Poland | People attending substance treatment services in England, Catalonia, and Poland | Quantitative: cross-sectional surveys | Changes in drug use patterns. |
| Paraskevis et al., 2013 | Greece | People who inject drugs in Athens | Quantitative: longitudinal administrative data | Changes in blood borne virus incidence. Changes in drug use risk behaviors. Resource shortages (syringe exchange services). |
| Pavarin et al., 2020 | Italy | People who use cocaine in northern Italy | Quantitative: archival, retrospective cohort | Changes to overdose rates. Changes to drug use patterns. |
| Tarjan et al., 2015 | Hungary | People who inject drugs in Hungary | Quantitative: serial cross-sectional survey, administrative time series data | Changes in drug use patterns. Changes to HCV incidence. Resource shortages (syringe exchange services). |
Table 3.
Characteristics of included publications contributing information on heroin shortages.
| First author, year | Country | Population | Study design and methods | Included outcomes |
|---|---|---|---|---|
| (Day et al., 2003) | Australia | People who inject drugs in Australia | Quantitative: cross-sectional survey | Changes in drug market and drug use patterns. Drug market violence linked to changing market conditions. |
| Day et al., 2005 | Australia | People who inject drugs in Australia | Quantitative: administrative time series data | Changes in HCV notifications. Changes in hospital visits for injection-related problems. |
| Day, Degenhardt, & Hall, 2006 | Australia | People who inject drugs in Australia | Quantitative: administrative time series data; cross-sectional interviews | Changes in drug availability, purity, and price. |
| Degenhardt, Day, Dietze, et al., 2005 | Australia | People seeking treatment for heroin dependence in Australia | Quantitative: administrative time series data, serial cross-sectional interviews with people who inject drugs | Changes in drug use patterns. Changes in drug-related crime. |
| Degenhardt, Day, Hall, et al., 2005 | Australia | People who inject drugs in Australia; people entering treatment for heroin dependence | Quantitative: administrative time series data, serial cross-sectional interviews with people who inject drugs | Changes in drug use patterns. Changes in drug-related mortality and crime. Changes in treatment-seeking for heroin dependence. |
| Degenhardt, Day, Conroy, et al., 2005 | Australia | People in treatment for drug dependence in Australia | Quantitative: administrative time series data | Changes in drug-related mortality. |
| Degenhardt, Day, Hall, et al., 2005 | Australia | People entering treatment for opioid dependence in New South Wales | Quantiative: longitudinal, retrospective cohort data | Treatment engagement and retention. |
| Gilmour et al., 2006 | Australia | People charged with cocaine or heroin possession in Australia | Quantitative: administrative time series data | Changes in drug use patterns. |
| Harris et al., 2015 | UK | People who inject drugs in London | Qualitative: interviews | Changes to drug use patterns and drug market. |
| Horyniak et al., 2015 | Australia | People who inject drugs in Melbourne | Quantitative: cross-sectional survey | Changes in drug use patterns. |
| Mital et al., 2016 | Kenya | People who use heroin in Kenya | Qualitative: cross-sectional interviews | Changes to drug use patterns and drug market. Changes in blood borne virus risk behaviors. Treatment access. |
| Pong et al., 2010 | Australia | Mothers who use drugs at the Royal Hospital for Women in New South Wales | Quantitative: administrative time series data | Changes in drug use patterns. Changes in withdrawal treatment for newborns. |
| Smithson et al., 2004 | Australia | People using heroin in Australia | Quantitative: administrative time series data | Changes in drug market. Changes in overdose rates. Changes in treatment-seeking. |
| Tarjan et al., 2015 | Hungary | People who inject drugs in Hungary | Quantitative: serial cross-sectional survey, administrative time series data | Changes in drug use patterns. Changes to HCV incidence. Resource shortages (syringe exchange services). |
| Topp et al., 2003 | Australia | People who inject drugs in Australia | Quantitative: serial cross-sectional survey | Changes in drug use patterns. |
| (Weatherburn et al., 2003) | Australia | People who use heroin in south-western Sydney | Quantitative: administrative data time series, interviews | Changes in drug use patterns and in drug market. |
| Wood et al., 2006 | Canada | People who inject drugs in Vancouver | Quantitative: administrative time series data, longitudinal survey data | Changes in drug-related mortality. Changes in drug use patterns. |
Study quality assessment
Given the unpredictable nature of Big Events, and the inherent difficulties in retrospectively studying the outcomes of an event, some methodological weaknesses were anticipated. While the included qualitative studies largely addressed the five study quality domains identified in the Mixed Methods Appraisal Tool, quantitative studies were commonly lacking in their approach to accounting for confounding. The mixed methods studies varied widely in their quality assessment, with each study judged to be lacking in at least one assessed domain (Supplementary Table 1).
Natural disasters
Of the 12 included publications pertaining to natural disasters, five concerned Hurricane Sandy, seven Hurricane Katrina, and one both Hurricanes Katrina and Rita. Seven articles used qualitative methods (Bennett, Golub, & Dunlap, 2011; Dunlap, Graves, & Benoit, 2012; Kotarba, Fackler, Johnson, & Dunlap, 2010; Matusow, Benoit, Elliott, Dunlap, & Rosenblum, 2018; McClure, Mendoza, Duncan, Rotrosen, & Hansen, 2014; Toriello, Morse, Morse, Kissinger, & Pedersen-Wasson, 2007; Valdez, Cepeda, Negi, & Kaplan, 2010) and five used a mix of qualitative and quantitative measures (Cepeda, Valdez, Kaplan, & Hill, 2010; Gupta, Hansen, Mendoza, Chen, & Swift, 2017; Maxwell, Podus, & Walsh, 2009; Tofighi, 2014; Pouget et al., 2015) (Table 1).
Drug-related risk and harms
Drug market disruption and violence. Research on Hurricane Katrina, which made landfall in New Orleans, Louisiana in 2005, found that established modes and networks of drug distribution were disrupted by the disaster, thereby increasing drug prices and the risk of violence related to drug acquisition (Dunlap et al., 2012). Participants in one study reported chaotic attempts to find and buy drugs and described witnessing people stealing drugs from those perceived as “weak,” particularly women (Dunlap et al., 2012). As weeks passed, new actors entered the previously hierarchical New Orleans drug market with a freelance style of drug distribution that engendered violence over turf, customers, and product (Bennett et al., 2011). Furthermore, as New Orleanians evacuated their city, New Orleanian drug sellers relocated to new markets, such as Houston, Texas. This displacement was linked to increased violence in the Houstonian market, leading to increased police surveillance of areas where drugs were sold, as well as harsher prosecutions of drug sellers (Kotarba et al., 2010).
Frequency of drug use. A moderate increase in drug use was reported by low-income New Orleanian evacuees living in Houston in the year following Hurricane Katrina (Cepeda et al., 2010; Maxwell et al., 2009). Some authors posit that substances were used to cope with traumatic experiences during and after the hurricane (Tkzello et al., 2007).
Changes in drugs used. Population displacement following a natural disaster may cause long-term shifts in the types of drugs used within a particular geographic area. Two years after the evacuation of many New Orleanians to Houston, patterns of drug consumption in Houston represented an integration of typical “Houstonian” and “New Orleanian” drug preferences (Kotarba et al., 2010). In the years following the hurricane, people returning to New Orleans brought with them new drug tastes, use patterns, and connections to drug suppliers (Dunlap et al., 2012; Kotarba et al., 2010).
Initiation of drug use. One study reported on initiation of crack cocaine use among Latino day laborers who had migrated to help rebuild New Orleans after Hurricane Katrina. Initiation was linked to the low price and high availability of crack cocaine, with some individuals escalating to regular use in an effort to cope with social isolation and marginalization in an unfamiliar context (Valdez et al., 2010). This was a group that was not directly affected by the Big Event in question, but their vulnerability combined with the availability of drugs in the post-disaster context contributed substantially to the likelihood of drug use.
Risk behaviors. Following Hurricane Sandy in 2012, people who inject drugs (PWID) in New York City reported sharing and re-using equipment, as well as injecting with people they would not usually inject with, due to difficulties accessing sterile syringes and displacement from their usual injecting locations (Pouget, Sandoval, Nikolopoulos, & Friedman, 2015). However, participants also reported exchanging sex for money, drugs, or other goods less frequently after the hurricane (Pouget et al., 2015).
Delivery of harm reduction / treatment services
Drug treatment engagement. In the wake of Hurricane Katrina, New Orleanian evacuees in Texas were more likely to drop out of drug treatment programs than Texan clients (Maxwell et al., 2009). Disasters on the scale of Hurricane Katrina, in which disruption and displacement occurs across many aspects of life, may engender greater physical and psychological impairment and necessitate more intensive responses to retain people in treatment (Toriello et al., 2007).
Flexibility of service providers. Literature on provision of opioid agonist treatment (OAT) during and after natural disasters highlighted the importance of flexibility on the part of treatment providers (Matusow et al., 2018; McClure et al., 2014; Pouget et al., 2015). Following Hurricane Sandy, clinics that were able to work within or around standard guidelines regarding take-home doses were better able to provision their clients during the disaster (Gupta et al., 2017), in contrast to restrictive models (e.g. requiring buprenorphine prescriptions to be filled at hospitals) that impeded care (McClure et al., 2014). The need for cross-coverage agreements between clinics, and especially for a centralized patient database to verify dosage, was discussed in response to both Hurricanes Katrina and Sandy (Gupta et al., 2017).
Communication. Natural disasters present numerous barriers to communication between service providers and clients. Following Hurricane Sandy, some OAT recipients were not aware of the closure of their clinic or whether there were alternate clinics available to them (Gupta et al., 2017). Power outages impeded communication, and as many as one-third of clients that reported communication difficulties dropped out of treatment for some length of time (Matusow et al., 2018; McClure et al., 2014). Some providers additionally reported difficulties communicating with regulatory agencies due to damaged telephone infrastructure, compounding confusion around the appropriate implementation of clinical guidelines during the emergency (Gupta et al., 2017).
Physical accessibility. Following Hurricane Sandy, transportation issues disproportionately affected methadone maintenance clients who were required to attend the clinic for daily dosing (McClure et al., 2014). Patients reported experiencing withdrawal symptoms and using illicit drugs when transportation issues made it difficult or impossible for them to reach their prescribing clinic (Matusow et al., 2018). Other patients who were unable to access clinics, prescribers, or usual medication supplies reported reducing their daily dose in order to prolong their supply (Tofighi, 2014). When clients could reach a clinic, staff and space shortages both contributed to longer wait times (Gupta et al., 2017). Additionally, Big Events have been shown to significantly affect access to antiretroviral treatment: during the week following Hurricane Sandy, 43% of HIV-positive PWID reported missing doses of their HIV medication (Pouget et al., 2015).
Changing patient populations and needs. The need to consider the experience of trauma as the result of a natural disaster is pertinent to both clients and staff of harm reduction and drug treatment services. Clients may increase substance use to cope with their disaster experiences, as was reported by Hurricane Katrina evacuees (Maxwell et al., 2009). At the same time, staff experiencing post-traumatic stress symptoms may struggle to address clients’ needs as well as their own (Toriello et al., 2007). Group counselling was recommended in the aftermath of Hurricane Sandy when individual counselling was precluded by lack of space (Gupta et al., 2017). Finally, some Big Events may affect the demographics of the population accessing a service. For example, New Orleanian evacuees seeking OAT in Texas were significantly more likely to be male, Black, older, and married than non-disaster-related clients; OAT providers noted that cultural sensitivity training would have been useful when serving this new population (Maxwell et al., 2009).
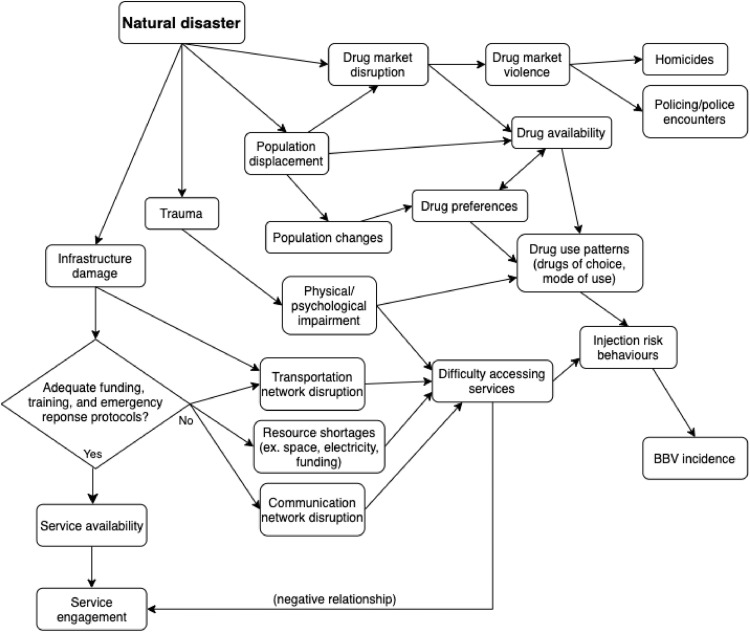
Risk pathways identified in studies of natural disasters
The risk pathway map developed based on this group of studies is presented in Fig. 2 . Key risk factors are infrastructure damage, trauma, population displacement, and drug market disruption. Important outcomes include BBV incidence, drug market violence, police encounters, and service engagement. Risk factors and outcomes are somewhat interrelated, particularly in relation to pathways leading from drug market disruption and population displacement to changes in drug use patterns. The paths from infrastructure damage to either service engagement or injection risk behaviors are more straightforward, and are determined by adequate funding, training, and emergency response protocols in place at harm reduction and treatment services. Thus, the map highlights the myriad risk factors that can lead to injection risk behaviors, especially in contrast with the lone pathway leading to increased service engagement.
Fig. 2.
Risk pathway map for natural disasters.
Note. Natural disasters can engender infrastructure damage, psychological trauma, population relocation, and drug market disruption. The map highlights the myriad risk factors that can lead to injection risk behaviors, especially in contrast with the limited pathway leading to service engagement.
Economic crises
Five quantitative publications provided information on the aftermath of the 2008 global financial crisis in France, Greece, Hungary, Italy, and Europe overall (Table 2 ).
Drug-related risk and harms
Frequency of drug use. As financial and social environments change in response to Big Events, people may adapt their drug use patterns in response. Clients of drug treatment centres in Europe, reflecting in 2015 and 2016 on their subjective experiences of the global financial crisis, reported that increases in free time as well as financial, social, and relational stress contributed to an increased frequency of drug use (Bruguera et al., 2018).
Changes in drugs used. In Hungary, heroin availability declined and rates of stimulant injecting increased between 2010 and 2012 (Tarjan et al., 2015). Similarly, heroin and cocaine use decreased and amphetamine use increased in northern Italy from 2009 to 2012 (Pavarin et al., 2020). Authors of both studies noted that these changes may be attributable to people choosing a cheaper, more readily available drug over more expensive, less accessible ones as incomes declined and cost of living rose (Pavarin et al., 2020; Tarjan et al., 2015).
Risk behaviors. In Hungary, the proportion of people who inject drugs that reported sharing injecting equipment increased between 2009 and 2011, even as the number of syringes distributed increased during the same period (Tarjan et al., 2015). The authors attributed the increase in equipment sharing to drug market disruption (and resulting changes in drugs used) caused by the global financial crisis.
Blood-borne viruses. The 2008 financial crisis in Greece was associated with a dramatic increase in HIV prevalence between 2008 and 2012, as well as increased HCV prevalence among people who inject drugs, including new drug injectors (Paraskevis et al., 2013). The recession left a higher proportion of people who inject drugs jobless and without accommodation, and the article's authors suggest that this increased economic difficulty facilitated a substantial expansion of HIV transmission networks, from two people on average between 1985 and 2007 to 34 people on average from 2008 to 2012 (Paraskevis et al., 2013). While the overall prevalence of HCV infection remained relatively stable in Hungary between 2006 and 2011, prevalence increased among stimulant injectors, a fact consistent with the increase in risk behaviors that seemed to result from drug market disruption (Tarjan et al., 2015).
Mortality rates. A retrospective study of mortality risk among people who use drugs in Italy reported that cocaine-related mortality risk decreased during the period from 2009 to 2012. The authors attributed this finding to reduced purchasing power as salaries declined during the financial crisis (Pavarin et al., 2020).
Delivery of harm reduction / treatment services
Funding. Funding for low-threshold drug treatment and harm-reduction services is an ongoing issue that can be exacerbated by poor economic conditions. In Hungary, syringe exchange programs increased their distribution during the financial crisis from 2008 to 2011. However, austerity measures imposed in the wake of the crisis necessitated shutdowns and restrictions of harm reduction services; syringe exchange programs reported having to reduce both their operating hours and the number of syringes distributed per contact. Between 2011 and 2012, the number of syringes distributed in Hungary dropped by 35%, despite a stable level of demand (Tarjan et al., 2015).
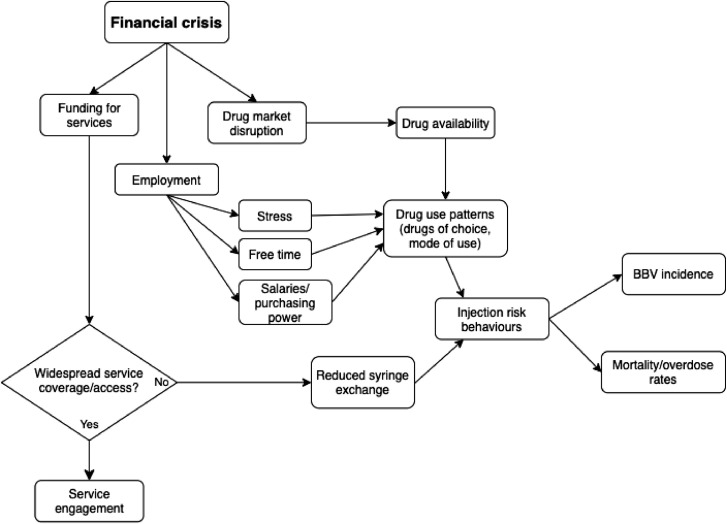
Risk pathways identified in studies of economic crises
Reviewed literature regarding the impact of financial crises on people who use drugs was synthesized to create a risk pathway map (Fig. 3 ). Financial crises directly impact employment, the drug market, and funding for harm reduction services. Both drug market disruption and factors related to employment affect drug use patterns. Important outcomes include incidence of blood-borne virus (BBV) infection, mortality and overdose rates, and service engagement. Service engagement appears to depend on widespread service coverage and accessibility.
Fig. 3.
Risk pathway map for financial crises.
Note. Financial crises directly impact employment, the drug market, and funding for harm reduction and treatment services. Service engagement is dependent on widespread service coverage and access.
Heroin shortages
Seventeen publications reported on heroin shortages, including 13 quantitative publications pertaining to the 2001 Australian heroin shortage (Day, Degenhardt, Gilmour, & Hall, 2005; Day, Degenhardt, & Hall, 2006; Day et al., 2003; Degenhardt, Conroy, Day, Gilmour, & Hall, 2005; Degenhardt, Day, Conroy, Gilmour, & Hall, 2005; Degenhardt, Day, Dietze, et al., 2005; Degenhardt, Day, Hall, Conroy, & Gilmour, 2005; Gilmour, Degenhardt, Hall, & Day, 2006; Horyniak et al., 2015; Pong et al., 2010; Smithson, McFadden, Mwesigye, & Casey, 2004; Topp, Day, & Degenhardt, 2003; (Weatherburn et al., 2003)), and one publication from each of western Canada (quantitative, Wood et al., 2006), the UK (qualitative, Harris et al., 2015), Kenya (qualitative, Mital et al., 2016), and Hungary (quantitative, Tarjan et al., 2015) (Table 3 ).
Drug-related risk and harms among people who use drugs
Drug market disruption. The 2001 Australian heroin shortage was characterized by a rapid decline in heroin availability and purity, as well as increases in the price of heroin and time needed to acquire it (Degenhardt, Day, Dietze, et al., 2005). Heroin price increases were also reported during heroin shortages in the UK (Harris, Forseth, & Rhodes, 2015) and Kenya (Mital, Miles, McLellan-Lemal, Muthui, & Needle, 2016).
Drug-related offending. The Australian heroin shortage was associated with a short-lived increase in burglary and robbery offences, assumed to be linked to the need to generate additional income to support drug purchases (Day et al., 2003). Some authors suggest that increased cocaine use among people who inject drugs led to the increase in robberies with a weapon (Degenhardt, Day, Hall, et al., 2005). However, other authors noted no major differences in crime rates before and after the shortage (Weatherburn et al., 2003) .
Changes in drugs used. Reductions in the supply of one drug may serve to increase the use of others. During the Australian heroin shortage, some people who inject drugs reported using heroin less often and increasing their use of cocaine, benzodiazepines, and cannabis (Day et al., 2003). This finding was corroborated by a 45% decrease in heroin possession charges during the five months following the shortage, while cocaine possession charges increased by 207% (Gilmour et al., 2006). Additionally, people who initiated injecting during this period were more likely to do so using methamphetamine than heroin (Horyniak et al., 2015). Similarly, transitions to poly-drug use were common during a heroin shortage in the United Kingdom, with cocaine and alcohol being the most commonly used substances in addition to heroin (Harris et al., 2015). In Hungary, where a dramatic reduction in heroin availability coincided with a period of economic austerity following the 2008 financial crisis, some people who inject drugs switched from heroin to synthetic cathinones (Tarjan et al., 2015).
Changes in route of administration. Evidence for transitions to or away from injecting drug use during a heroin shortage differed across settings. In Kenya, people who use heroin reported switching from smoking to injecting during a shortage in order to compensate for the reduced quality and quantity of heroin available (Mital et al., 2016). During the UK heroin shortage, however, some people who use heroin reported switching from injecting to smoking to protect their veins when heroin quality appeared poor (Harris et al., 2015). In Australia, the reduced availability of heroin in 2001 was linked to reduced demand for needle and syringe exchange, suggesting an overall reduction in the prevalence of injection drug use (Degenhardt, Day, Dietze, et al., 2005).
Risk behaviors. While a heroin shortage may be relatively short-lived, resulting changes in drug use patterns can have long-lasting implications. For instance, people who initiated injecting during the Australian heroin shortage were more likely than those with a longer injecting history to maintain poly-drug use and syringe-sharing behaviors after the shortage ended (Horyniak et al., 2015). Similarly, people who use heroin in Kenya reported riskier injection practices during the heroin shortage, including increases in equipment sharing and injecting the blood of people who had recently injected heroin (“flashblood”). The practice of “flashblood” continued after the shortage ended, suggesting that the shortage may have established new norms of drug use (Mital et al., 2016).
Injection-related harms. Increased stimulant injection was reported during the heroin shortages in both Australia and the UK (Day et al., 2003, Harris et al., 2015). People who inject stimulants often do so at a higher frequency relative to opioid injecting, increasing the risk of venous damage and soft tissue infection (Harris et al., 2015; Tarjan et al., 2015).
Blood-borne viruses. Although no immediate change in HCV notifications was observed during the 2001 Australian heroin shortage, a decrease in HCV notifications during the two years following the shortage may be related to reduced injecting drug use (Day et al., 2005). For people already living with HCV, however, shifting patterns of drug use may themselves cause harm. People who use drugs in the UK, for example, reported heavier alcohol use during the heroin shortage there, which can accelerate disease progression and cirrhosis for people with Hepatitis C (Harris et al., 2015).
Overdose and mortality rates. During the Australian heroin shortage, both fatal and non-fatal heroin overdoses decreased at the population level, with no recorded increases in overdoses or deaths related to cocaine, methamphetamine, or benzodiazepines (Degenhardt, Day, Dietze, et al., 2005; (Weatherburn et al., 2003)). Heroin-related ambulance call-outs also declined (Smithson et al., 2004). Changes in overdose mortality were most apparent in younger people: heroin-related deaths decreased for 15–24 year olds by 65%, while there was no change in drug-related deaths for other age groups (Degenhardt, Day, Conroy, et al., 2005). A decline in overdose mortality rates was also observed in western Canada during the Australian heroin shortage, suggesting a wider scope for this Big Event than previously considered (Wood, Stoltz, Li, Montaner, & Kerr, 2006).
Delivery of harm reduction / treatment services
Drug treatment engagement. The Australian heroin shortage saw decreased drop-out and increased re-enrolment in opioid agonist therapy (OAT), suggesting increasing demand for drug treatment up to a year after the shortage (Degenhardt, Conroy, et al., 2005; Smithson et al., 2004). Other heroin shortages, however, did not appear to affect treatment uptake. In the UK, a heroin shortage was followed by an increase in methadone usage outside of treatment settings, but not an increase in enrolment in methadone treatment (Harris et al., 2015). Similarly, during a heroin shortage in Kenya, where drug use is highly stigmatized and treatment is limited, participants reported riskier behaviors and withdrawal symptoms rather than treatment seeking (Mital et al., 2016). Changes observed during the Australian heroin shortage occurred in the context of widespread, publicly funded harm reduction initiatives, including substantial efforts to expand OAT coverage (Day et al., 2005). This may account for some of the difference in treatment outcomes observed in Australia as compared to the UK and Kenya. However, although many people who inject drugs reported increasing their use of stimulants during the Australian heroin shortage, service providers were not well equipped to deal with non-opiate drug-related harms (Topp et al., 2003).
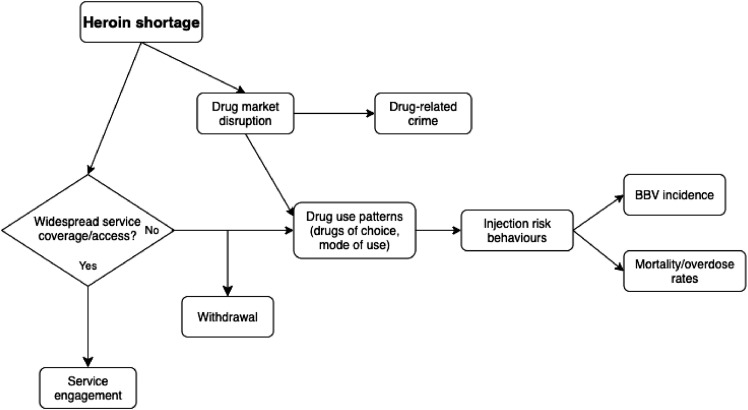
Risk pathways identified in studies of heroin shortages
Reviewed literature regarding heroin shortages was synthesized to create a risk pathway map in Figure 4 Key risk factors are drug market disruption and service coverage/access. Important outcomes are BBV incidence, mortality/overdose, drug-related crime, withdrawal, and service engagement. With the exception of drug-related crime, outcomes are strongly influenced by the presence or absence of widespread service coverage.
Fig. 4.
Risk pathway map for heroin shortages.
Note. Heroin shortages mainly disrupt the drug market, leading to a variety of possible outcomes. With the exception of drug-related crime, outcomes are strongly influenced by the presence or absence of widespread service coverage.
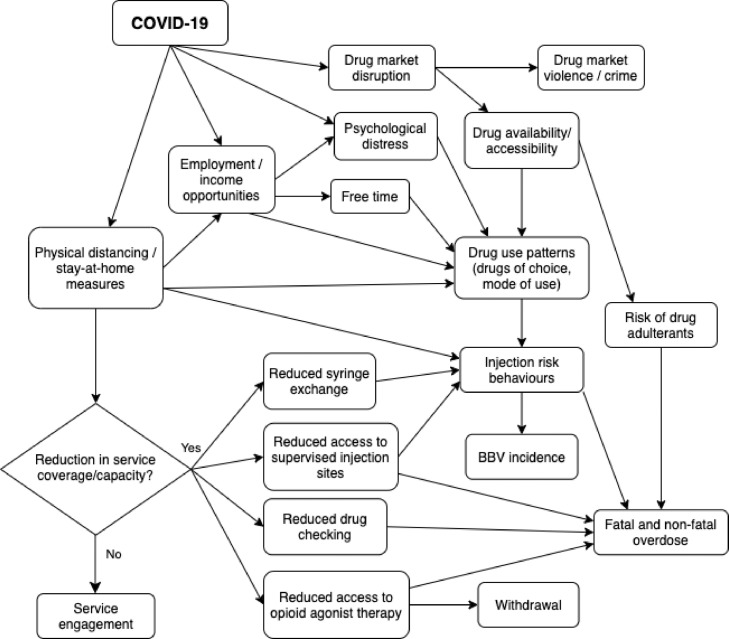
Proposed risk pathways for impacts of the COVID-19 pandemic on people who use drugs
Considering the reviewed literature on Big Events and the resultant risk pathway maps, we propose a risk pathway map specific to the COVID-19 pandemic (Fig. 5 ). Key antecedents, analogous to other Big Events, are drug market disruption, loss of employment and/or income opportunities, and increased psychological distress, along with a risk factor unique to the pandemic, the imposition of physical distancing and/or confinement measures. These risk factors directly or indirectly feed into changing drug use patterns and injection risk behaviors, such as injecting alone or re-using equipment. The multifaceted nature of harm reduction services are highlighted; the provision of these services is hypothesized to impact injection risk behaviors and the experience of withdrawal symptoms. Important outcomes to monitor are overdose rates, BBV incidence, withdrawal, and, potentially, engagement with harm reduction and treatment services.
Fig. 5.
Proposed risk pathway map for the COVID-19 pandemic.
Discussion
We completed a rapid systematic review of the impacts of Big Events on drug-related harms and service delivery for people who use drugs, with the overarching aim of informing responses to the COVID-19 pandemic. There are clear distinctions between the three Big Event types included in this review, none of which overlaps perfectly with the COVID-19 context. Natural disasters and heroin shortages are discrete events, occurring in a specific geographic area and time frame; the global financial crisis, in contrast, affected nations around the world, and its impact reverberated for years. Study designs reflected these differences in scale, with natural disaster publications tending to rely more on qualitative interviews and surveys able to capture abrupt changes in drug use risk environments relatively quickly, while studies of the global financial crisis were more likely to investigate epidemiological trends over several years. These methodological choices are suited to the respective Big Events, but mean that risk pathway maps derived from these groups of studies reflect different time scales and are not directly comparable. Big Events also differ in the proportion and segments of the population that experience their destabilizing effects; heroin shortages mostly affect people involved in the drug market, whereas natural disasters and financial crises disrupt society more broadly. Nevertheless, broad societal disruptions typically have a heightened impact on marginalized groups such as people who use drugs, and may trigger secondary events (e.g., drug market disruption) that also disproportionately affect those groups.
Though the reported impacts of Big Events differed across categories, some consistent themes were apparent. All reviewed Big Events caused major disruptions to drug markets, which were associated with increased risk across a range of harms. Psychological distress and economic instability generated by Big Events negatively impacted participants’ mental health, which may potentiate drug use risk behaviors and potentially necessitate more intensive treatment. Economic instability also affected the funding and coverage of harm reduction and treatment services, which further impact the risk of drug-related harms. Finally, flexibility in service provision was required to provide for adequate medication, transportation, and communication with clients on OAT. In some cases, this flexibility was facilitated by emergency preparedness plans.
Transferability of results to the COVID-19 context
While the nature and impacts of each Big Event differ, there are informative parallels between the Event types reviewed and the current pandemic context. Similar to major hurricanes in the United States, the COVID-19 pandemic has disrupted transportation networks and appears to have destabilized drug markets in some settings (Gomis, 2020; UNODC, 2020). In addition, the widespread imposition of physical distancing and stay-at-home measures in response to the pandemic reduces access to vital services and generates psychological distress, analogous to outcomes produced by natural disasters. Similarly, outcomes related to increased stress and decreased incomes and service access in the wake of the 2008 global financial crisis are highly relevant to the current context. As the effects of economic recession continued to emerge over many years following the 2008 crisis, vigilance to the ongoing impacts of the financial aspect of the COVID-19 pandemic may be necessary even after the immediate health crisis has abated. Finally, the literature on heroin shortages provides insight into the outcomes of of drug market disruption itself. Notably, only studies of the 2001 heroin shortage in Australia reported increases in drug treatment engagement, which may be attributable to the lack of service disruption caused by this Big Event. If local service providers are able to maintain their offerings and hours with little disruption, drug-related risks and harms associated with the COVID-19 pandemic might prove more similar to those of the Australian heroin shortage.
Not all of the effects of Big Events identified in the reviewed studies are directly relevant to COVID-19 responses. For example, physical infrastructure damage, population displacement, and acute trauma do not characterize the COVID-19 pandemic, limiting the relevance of natural disaster research to the current context. While both the 2008 global financial crisis and COVID-19 disrupted global productivity, the nature of the resulting economic recessions differ, and the recovery processes are likely to diverge as well, with emerging reports that the pandemic has served to increase income inequality (Alini, 2020). Finally, heroin shortages lack the society-wide impacts that characterize other reviewed Big Events and the COVID-19 context.
Implications for COVID-19 response
The results of this review cannot indicate how drug use rates will change as a result of the pandemic, but the overarching themes of drug market disruption, heightened risk of psychological distress and drug-related harms, and the importance of service adaptability, all have translatable implications not only for how governments and services can respond to COVID-19, but also how they can increase their preparedness for future Big Events of varying kinds.
Drug market and service disruptions may increase overdose and BBV rates
Big Events disrupt drug market dynamics, affecting drug availability, accessibility, price, and concentration. People may respond to market changes by switching to different drugs or changing their consumption habits, including engaging in riskier injection practices. These behavioral changes can increase the risk of overdose and BBV infection (Cepeda et al., 2010; Harris et al., 2015; Horyniak et al., 2015). In contrast with these risk factors, studies of the 2001 heroin shortage in Australia and Canada demonstrated a reduction in overdose mortality (Gilmour et al., 2006; Wood et al., 2006). However, the emergence of potent contaminants such as fentanyl differentiates the contemporary North American context from those of previous shortages (Belzak & Halverson, 2018). Several other factors contribute to heightened overdose risk in the current context. Border closures in response to the COVID-19 pandemic may compound the risk of drug contamination by limiting drug importation (Beletsky & Davis, 2017; RCCET, 2020). Additionally, physical distancing measures imposed as a result of the pandemic may reduce the capacity of spaces such as shelters and supervised injection sites, increasing the likelihood of someone using drugs in public or while alone (Schlosser & Harris, 2020). Using drugs in public settings is associated with a range of harms, including elevated risk of BBV infection and overdose (Trayner et al., 2020). People who use drugs in public are also more likely to experience arrest and incarceration (Ickowicz et al., 2017; Trayner et al., 2020), which could be exacerbated by increased policing of public spaces during stay-at-home mandates. Reduced access to supervised injection sites may also restrict access to naloxone, a potentially life-saving opioid antagonist (Chimbar & Moleta, 2018). Recent upticks in overdose mortality in many settings suggest that these are justified concerns ((Alter and Yeager, 2020); AMA, 2020; BCCDC, 2020; BCCS, 2020; Wan, 2020).
The injection risk behaviors that result from drug market and service disruptions may also promote the spread of blood-borne viruses (BBV). In the drug market, a reduced supply may promote equipment sharing, as was reported during a heroin shortage in Kenya (Mital et al., 2016). Additionally, disruptions to the operation of harm reduction services were associated with reduced access to and use of sterile needles and syringes, potentially increasing the risk of HCV and HIV incidence among people who inject drugs (Harris et al., 2015; Tarjan et al., 2015). If services are operating under reduced hours or capacity due to the COVID-19 pandemic, it may prove difficult to provide adequate service coverage. For example, the UK government implemented stay-at-home restrictions in mid-March 2020. By the following month, the number of clients and visits received at needle and syringe programs (NSPs) had dropped by more than a third, and the number of needles distributed decreased by 29% (Whitfield, Reed, Webster, & Hope, 2020).
Psychological and financial instability increase drug-related risk
Big Events disrupt not only drug markets and service accessibility but also people's sense of safety and security. Studies of Hurricane Katrina identified a need for services to be responsive to trauma caused by natural disasters and displacement (Maxwell et al., 2009; Toriello et al., 2007). During the 2008 global financial crisis, people who use drugs reported that increased social and financial stress contributed to increased drug use (Bruguera et al., 2018). The COVID-19 pandemic represents both a health and an economic crisis, and may engender psychological distress, anxiety, and grief, as well as potential increases in drug use as people cope with these negative feelings (Panchal et al., 2020). Physical distancing measures may hinder access to supports such as group therapy and disrupt social solidarity among people who use drugs, exacerbating any negative psychological consequences of the pandemic (Schlosser & Harris, 2020). Social and psychological support services may need to consider provisions to provide access to the appropriate technology for therapy by telephone or videoconference.
The COVID-19 pandemic has dramatically impacted the world economy, with high levels of job loss seen in countries around the globe (ILO, 2020). During the 2008 global financial crisis, a reviewed study in Greece indicated that as the GDP growth rate declined, rates of homelessness and unemployment increased among people who inject drugs in Athens (Paraskevis et al., 2013). For people who use drugs, the COVID-19 pandemic may also potentiate the loss of employment or the loss of opportunities to generate income, such as panhandling or shoplifting, that depend on high-density public spaces. Any loss of income may increase psychological distress and exacerbate the issue of rising prices as drug supply dwindles (Nagelhout et al., 2017). As stress has also been associated with initiating drug use, there is not only a concern for people currently using drugs, but also a risk that the number of PWUD might increase as economic opportunities decline (Dom et al., 2016). Conversely, financial assistance programs implemented by governments in response to COVID-19 may protect against these harms, provided that people are able to access them. A report regarding the CARES Act in the United States indicates that vulnerable people experience more barriers to accessing benefits (Roll & Grinstein-Weiss, 2020).
Supporting harm reduction to reduce drug-related risk
The provision of both harm reduction and drug treatment services depends upon adequate funding. In the context of Big Events, the lack of specific attention to people who use drugs has concretized in the form of reduced funding for harm reduction programs (Tarjan et al., 2015), lack of access to opioid agonist treatment (Mital et al., 2016), and funding distinctions between mental health treatment and substance use treatment (Maxwell et al., 2009). Securing funding is imperative in order to ensure that these essential services are not interrupted by the COVID-19 pandemic.
Reviewed publications of the response to Hurricane Sandy largely focused on the provisioning of opioid agonist therapy (OAT), emphasizing the need for flexibility during a crisis (Gupta et al., 2017; Matusow et al., 2018; McClure et al., 2014; Tofighi, 2014). In response to the COVID-19 pandemic, clinical guidance has been issued to support OAT via telemedicine in the United States (SAMHSA, 2020) and Canada (Bruneau et al., 2020). Longer prescription durations and increased allowance for take-home doses for people on OAT have also been announced in nations such as Australia (DHHS, 2020), Ireland (EMCDDA, 2020), and Iran (Deilamizade & Moghanibashi-Mansourieh, 2020). The UK government has called for an increase to harm reduction service provision and reach wherever possible, despite staffing limitations (PHE, 2020). Currently, however, OAT guidance is highly variable by jurisdiction, and there is a lack of data on the implementation and scaling up of these policies.
The new realities of the COVID-19 pandemic provide opportunities for the field of harm reduction to adapt and progress. Harm reduction services, including needle and syringe exchange (Turner, Hutchinson, & Vickerman, 2011), drug analysis (Kerr & Tupper, 2017), take-home naloxone provision (Chimbar & Moleta, 2018), supervised injection sites (Potier, Laprevote, Dubois-Arber, Cottencin, & Rolland, 2015), and safe supply provision (Chang et al., 2020), may need to supplement in-person access with strategies such as mobile operations, home delivery, peer distribution, mail, and vending machines in order to extend their coverage (Brar et al., 2020; Whitfield et al., 2020). Legislative and financial support from governmental authorities is paramount for these services to continue their operations.
Planning for Big Events
Several of the publications reporting on natural disasters noted the importance of emergency preparedness planning for harm reduction and drug treatment services (Gupta et al., 2017; Matusow et al., 2018; Maxwell et al., 2009). Research on preparations made by service providers for unhoused people in response to the 2003 SARS outbreak similarly noted the importance of including vulnerable populations in emergency preparedness planning (Leung et al., 2008). Services should ideally publish any preparedness plans that are already in place, along with the process of their development, to support other services in planning for the broad range of emergencies that may occur and to which they must be able to flexibly and rapidly respond. Given the importance of communicating with clients to maintain continuity of care as identified by several studies, preparedness plans should include measures to ensure that up-to-date contact details are maintained, or alternative strategies are in place to maintain contact (e.g., obtaining client permission to pass on messages to known contacts).
Higher-level preparedness plans (e.g., as developed by provincial governments) should include people who use drugs and other marginalized groups, such as people experiencing homelessness, as priority populations. The way in which governments respond to the current crisis will impact harm reduction services and the people they serve (Chang et al., 2020). By responding quickly, flexibly, and with respect for people's intersecting identities, governmental agencies and services are in the position to reduce harms associated with the Big Event of COVID-19.
Limitations
The quality of included studies varied; however, expectations regarding methodological rigour must be balanced against the realities of conducting research in the aftermath of Big Events. We do not consider that methodological weaknesses invalidate the findings of this review; rather, they highlight aspects of study design and analysis for researchers to consider in studying the COVID-19 pandemic and future Big Events.
Our rapid review did not yield any research on outcomes for people who use drugs during recent respiratory infection outbreaks, the Big Event type that would have been most directly comparable to the COVID-19 pandemic. There has been some work in this area in relation to other marginalized populations. Research in response to the 2003 SARS outbreak and its impact on people who are homeless identified challenges in communicating public health messages with marginalized populations and in providing space for screening or quarantining (Leung, 2008). Another report identified low incidence of H1N1 among marginalized populations such as sex workers; its authors suggested that social marginalization may have had a protective effect against infection (Rodwell et al., 2010).
Few studies considered the impact of Big Events on particularly marginalized subpopulations of people who use drugs, including women, gender diverse people, Indigenous peoples, and visible minorities, thus limiting the evidence base that could be used to inform intersectional COVID-19 responses for marginalized groups. Validating the findings of our review with people who use drugs, including those from various subpopulations, is an important next step in this work. We also note that most studies were conducted in high-income countries, with very little representation of middle- or low-income countries in the results. There is a need for more data to understand the experiences of people who use drugs in low- and middle-income countries during and after Big Events.
Conclusion
We have undertaken a comprehensive and inclusive review of literature concerning drug-related risk, harms, and service provision in the aftermath of Big Events. Potential risk pathways to monitor have been suggested; however, no assumptions regarding the epidemiology of drug use can be drawn from this study. Only future work will be able to indicate which factors play a role in heightening or reducing drug-related risks and harms for the specific circumstances of a global pandemic. We have offered suggestions for services to consider as they adapt to rapidly changing drug use risk environments, and provided risk pathway maps that may prove useful as analytical tools for future studies of Big Events.
Declarations of Interest
None.
Funding sources
This work was supported by the Canadian Institutes of Health Research (grant #442632).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.drugpo.2021.103127.
Appendix. Supplementary materials
References
- Ahsan S. The coronavirus pandemic is putting addiction recovery at risk. Now Toronto. 2020 13 April 2020. Retrieved from https://nowtoronto.com/lifestyle/health/addiction-recovery-coronavirus-pandemic/ [Google Scholar]
- Alini E. Canada's ‘K-shaped’ recovery spans jobs, debt and housing. Global News. 2020 17 October 2020. [Google Scholar]
- Alter A., Yeager C. 2020. COVID-19 Impact on US National Overdose Crisis. [Google Scholar]; Retrieved from http://www.odmap.org/Content/docs/news/2020/ODMAP-Report-June-2020.pdf.
- AMA . American Medical Association; 2020. Issue brief: Reports of increases in opioid related overdose and other concerns during COVID pandemic. [Google Scholar]; Retrieved from https://www.ama-assn.org/system/files/2020-08/issue-brief-increases-in-opioid-related-overdose.pdf.
- BCCDC . 2020. Overdose response indicator report. [Google Scholar]; Retrieved from http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/Overdose/Overdose%20Response%20Indicator%20Report.pdf.
- BCCS . British Columbia Coroners Service; 2020. Illicit Drug Toxicity Deaths in BC: January 1, 2010 – July 31, 2020. [Google Scholar]; Retrieved from https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/illicit-drug.pdf.
- Beletsky L., Davis C.S. Today's fentanyl crisis: Prohibition's Iron Law, revisited. International Journal of Drug Policy. 2017;46:156–159. doi: 10.1016/j.drugpo.2017.05.050. [DOI] [PubMed] [Google Scholar]
- Belzak L., Halverson J. The opioid crisis in Canada: a national perspective. Health Promotion and Chronic Disease Prevention in Canada. 2018;38(6):224–233. doi: 10.24095/hpcdp.38.6.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett A.S., Golub A., Dunlap E. Drug Market Reconstitution after Hurricane Katrina: Lessons for Local Drug Abuse Control Initiatives. Justice Research and Policy. 2011;13(1):23–44. doi: 10.3818/JRP.13.1.2011.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brar R., Bruneau J., Butt P., Goyer M., Lim R., Poulin G.…Wood E. In: i. S. M. (CRISM) C.R.I., editor. Vancouver; British Columbia: 2020. [Google Scholar]
- Bruguera P.R., J., Gilvarry E., Braddick F., Veettil M., Anderson P., Mielecka-Kubien Z., Kaner E., Gaul A. How does Economic Recession Affect Substance Use? A Reality Check with Clients of Drug Treatment Centres. Journal of Mental Health Policy and Economics. 2018;21:11–16. [PubMed] [Google Scholar]
- Bruneau J., Rehm J., Wild T.C., Wood E., Sako A., Swansburg J., Lam A. 2020. Telemedicine support for addiction services: national rapid guidance document (version 1) [Google Scholar]; Retrieved from https://crism.ca/wp-content/uploads/2020/05/CRISM-National-Rapid-Guidance-Telemedicine-V1.pdf.
- Cepeda A., Valdez A., Kaplan C., Hill L.E. Patterns of substance use among hurricane Katrina evacuees in Houston, Texas. Disasters. 2010;34(2):426–446. doi: 10.1111/j.1467-7717.2009.01136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J., Agliata J., Guarinieri M. COVID-19 - Enacting a ‘new normal’ for people who use drugs. International Journal of Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimbar L., Moleta Y. Naloxone effectiveness: a systematic review. Journal of Addictions Nursing. 2018;29(3):167–171. doi: 10.1097/JAN.0000000000000230. [DOI] [PubMed] [Google Scholar]
- Collins A.B., Boyd J., Czechaczek S., Hayashi K., McNeil R. (Re)shaping the self: An ethnographic study of the embodied and spatial practices of women who use drugs. Health and Place. 2020:63. doi: 10.1016/j.healthplace.2020.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day C., Degenhardt L., Gilmour S., Hall W. The impact of changes to heroin supply on blood-borne virus notifications and injecting related harms in New South Wales, Australia. BMC Public Health. 2005;5:84. doi: 10.1186/1471-2458-5-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day C., Degenhardt L., Hall W. Documenting the heroin shortage in New South Wales. Drug and Alcohol Review. 2006;25(4):297–305. doi: 10.1080/09595230600741024. [DOI] [PubMed] [Google Scholar]
- Day C., Topp L., Rouen D., Darke S., Hall W., Dolan K. Decreased heroin availability in Sydney in early 2001. Addiction. 2003;98:93–95. doi: 10.1046/j.1360-0443.2003.00266.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Conroy E., Day C., Gilmour S., Hall W. The impact of a reduction in drug supply on demand for and compliance with treatment for drug dependence. Drug and Alcohol Dependence. 2005;79(2):129–135. doi: 10.1016/j.drugalcdep.2005.01.018. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Day C., Conroy E., Gilmour S., Hall W. Age differentials in the impacts of reduced heroin: effects of a “heroin shortage” in NSW, Australia. Drug and Alcohol Dependence. 2005;79(3):397–404. doi: 10.1016/j.drugalcdep.2005.03.028. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Day C., Dietze P., Pointer S., Conroy E., Collins L., Hall W. Effects of a sustained heroin shortage in three Australian States. Addiction. 2005;100(7):908–920. doi: 10.1111/j.1360-0443.2005.01094.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Day C., Hall W., Conroy E., Gilmour S. Was an increase in cocaine use among injecting drug users in New South Wales, Australia, accompanied by an increase in violent crime? BMC Public Health. 2005;5:40. doi: 10.1186/1471-2458-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Peacock A., Colledge S., Leung J., Grebely J., Vickerman P., Larney S. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Global Health. 2017;5(12):e1192–e1207. doi: 10.1016/s2214-109x(17)30375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deilamizade A., Moghanibashi-Mansourieh A. Challenges of providing COVID-19 prevention services to homeless people who use drugs in Iran. International Journal of Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS . 2020. COVID-19 Response: Pharmacotherapy services: information for prescribers and dispensers. Retrieved from https://de4e0707-9881-41c5-b4b5-79de5c5c6366.filesusr.com/ugd/ebb8bf_8710dc68993b4d839509ebd8115389f9.pdf?index=true. [Google Scholar]
- Dom G., Samochowiec J., Evans-Lacko S., Wahlbeck K., Van Hal G., McDaid D. The Impact of the 2008 Economic Crisis on Substance Use Patterns in the Countries of the European Union. International Journal of Environmental Research and Public Health. 2016;(1):13. doi: 10.3390/ijerph13010122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlap E., Graves J., Benoit E. Stages of drug market change during disaster: Hurricane Katrina and reformulation of the New Orleans drug market. International Journal of Drug Policy. 2012;23(6):473–480. doi: 10.1016/j.drugpo.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMCDDA . 2020. Impact of COVID-19 on drug services and help-seeking in Europe. [Google Scholar]; Retrieved from https://www.emcdda.europa.eu/system/files/publications/13073/EMCDDA-Trendspotter-Covid-19_Wave-1-2.pdf.
- Friedman S.R., Rossi D., Braine N. Theorizing “Big Events” as a potential risk environment for drug use, drug-related harm and HIV epidemic outbreaks. International Journal of Drug Policy. 2009;20(3):283–291. doi: 10.1016/j.drugpo.2008.10.006. [DOI] [PubMed] [Google Scholar]
- Gilmour S., Degenhardt L., Hall W., Day C. Using intervention time series analyses to assess the effects of imperfectly identifiable natural events: a general method and example. BMC Medical Research Methodology. 2006;6:16. doi: 10.1186/1471-2288-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick S.N., Prohaska S.M., LaKosky P.A., Juarez A.M., Corcorran M.A., Des Jarlais D.C. The Impact of COVID-19 on Syringe Services Programs in the United States. AIDS and Behavior. 2020 doi: 10.1007/s10461-020-02886-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomis B. How the illicit drug trade is adapting to the coronavirus pandemic. World Politics Review. 2020 [Google Scholar]; Retrieved from https://www.worldpoliticsreview.com/articles/28696/how-the-illicit-drug-trade-is-adapting-to-the-coronavirus-pandemic.
- Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A.…Ziebuhr J. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta V.K., Hansen H., Mendoza S., Chen X.L., Swift R.G. Merging Outpatient Addiction and Opioid-Maintenance Programs During A Disaster: Lessons From Hurricane Sandy. Disaster Medicine and Public Health Preparedness. 2017;11(5):531–537. doi: 10.1017/dmp.2016.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M., Forseth K., Rhodes T. It's Russian roulette: adulteration, adverse effects and drug use transitions during the 2010/2011 United Kingdom heroin shortage. International Journal of Drug Policy. 2015;26(1):51–58. doi: 10.1016/j.drugpo.2014.09.009. [DOI] [PubMed] [Google Scholar]
- Hong Q.N., Pluye P., Bujold M., Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic review of qualitative and quantitative evidence. Systematic Reviews. 2017;6:61. doi: 10.1186/s13643-017-0454-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5364694/pdf/13643_2017_Article_454.pdf.
- Hong Q.N., Pluye P., Fàregues S., Bartlett G., Boardman F., Cargo M.…Vedel I. VERSION 2018 User guide; 2018. MIXED METHODS APPRAISAL TOOL (MMAT) [Google Scholar]
- Horyniak D., Stoove M., Degenhardt L., Aitken C., Kerr T., Dietze P. How do drug market changes affect characteristics of injecting initiation and subsequent patterns of drug use? Findings from a cohort of regular heroin and methamphetamine injectors in Melbourne, Australia. International Journal of Drug Policy. 2015;26(1):43–50. doi: 10.1016/j.drugpo.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Ickowicz S., Wood E., Dong H., Nguyen P., Small W., Kerr T.…Milloy M.J. Association between public injecting and drug-related harm among HIV-positive people who use injection drugs in a Canadian setting: A longitudinal analysis. Drug and Alcohol Dependence. 2017;180:33–38. doi: 10.1016/j.drugalcdep.2017.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILO . International Labor Organization; 2020. Almost 25 million jobs could be lost worldwide as a result of COVID-19, says ILO. [Google Scholar]; Retrieved from https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_738742/lang-en/index.html.
- Jacka B.P., Phipps E., Marshall B.D.L. Drug use during a pandemic: Convergent risk of novel coronavirus and invasive bacterial and viral infections among people who use drugs. International Journal of Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffords S. CBC News; 2020. Two crises': Ontario's opioid problem worsens during COVID-19 as services for drug users scale back. [Google Scholar]
- Kerr T., Tupper K. 2017. Drug checking as a harm reduction intervention. [Google Scholar]
- Kotarba J.A., Fackler J., Johnson B.D., Dunlap E. The melding of drug markets in Houston after Katrina: dealer and user perspectives. Substance Use & Misuse. 2010;45(9):1390–1405. doi: 10.3109/10826081003682917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhdar C.B., Bastianic T. Economic constraint and modes of consumption of addictive goods. International Journal of Drug Policy. 2011;22(5):360–365. doi: 10.1016/j.drugpo.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Lam V., Sankey C., Wyman J., Zhang M. 2020. COVID-19 Opioid Agonist Treatment Guidance. [Google Scholar]; 22 March 2020. Retrieved from https://www.camh.ca/-/media/files/covid-19-modifications-to-opioid-agonist-treatment-delivery-pdf.pdf?la=en&hash=261C3637119447097629A014996C3C422AD5DB05.
- Leung C.S., Ho M.M., Kiss A., Gundlapalli A.V., Hwang S.W. Homelessness and the response to emerging infectious disease outbreaks: lessons from SARS. Journal of Urban Health. 2008;85(3):402–410. doi: 10.1007/s11524-008-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malinowska-Sempruch K. What interventions are needed for women and girls who use drugs? A global perspective. Journal of Acquired Immune Deficiency Syndromes. 2015;69:S96–S97. doi: 10.1097/QAI.0000000000000621. [DOI] [PubMed] [Google Scholar]
- Matusow H., Benoit E., Elliott L., Dunlap E., Rosenblum A. Challenges to Opioid Treatment Programs After Hurricane Sandy: Patient and Provider Perspectives on Preparation, Impact, and Recovery. Substance Use & Misuse. 2018;53(2):206–219. doi: 10.1080/10826084.2016.1267225. [DOI] [PubMed] [Google Scholar]
- Maxwell J.C., Podus D., Walsh D. Lessons learned from the deadly sisters: drug and alcohol treatment disruption, and consequences from Hurricanes Katrina and Rita. Substance Use & Misuse. 2009;44(12):1681–1694. doi: 10.3109/10826080902962011. [DOI] [PubMed] [Google Scholar]
- McClure B., Mendoza S., Duncan L., Rotrosen J., Hansen H. Effects of regulation on methadone and buprenorphine provision in the wake of Hurricane Sandy. Journal of Urban Health. 2014;91(5):999–1008. doi: 10.1007/s11524-014-9904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbin W., Fernando R. In: Economics in the Time of COVID-19. Baldwin R., Weder di Mauro B., editors. CEPR Press; London: 2020. The economic impact of COVID-19; pp. 45–51. [Google Scholar]
- Mital S., Miles G., McLellan-Lemal E., Muthui M., Needle R. Heroin shortage in Coastal Kenya: A rapid assessment and qualitative analysis of heroin users' experiences. International Journal of Drug Policy. 2016;30:91–98. doi: 10.1016/j.drugpo.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelhout G.E., Hummel K., de Goeij M.C.M., de Vries H., Kaner E., Lemmens P. How economic recessions and unemployment affect illegal drug use: A systematic realist literature review. International Journal of Drug Policy. 2017;44:69–83. doi: 10.1016/j.drugpo.2017.03.013. [DOI] [PubMed] [Google Scholar]
- Panchal N., Kamal R., Orgera K., Cox C., Garfield R., Hamel L.…Chidambaram P. Kaiser Family Foundation; 2020. The Implications of COVID-19 for Mental Health and Substance Use. [Google Scholar]; Retrieved from https://www.rcorp-ta.org/sites/default/files/2020-07/The%20Implications%20of%20COVID-19%20for%20Mental%20Health%20and%20Substance%20Use%20_%20KFF.pdf.
- Pandor A., Kaltenthaler E., Martyn-St James M., Wong R., Cooper K., Dimairo M.…Booth A. Delphi consensus reached to produce a decision tool for SelecTing Approaches for Rapid Reviews (STARR) Journal of Clinical Epidemiology. 2019;114:22–29. doi: 10.1016/j.jclinepi.2019.06.005. [DOI] [PubMed] [Google Scholar]
- Paraskevis D., Nikolopoulos G., Fotiou A., Tsiara C., Paraskeva D., Sypsa V.…Hatzakis A. Economic recession and emergence of an HIV-1 outbreak among drug injectors in Athens metropolitan area: a longitudinal study. PLoS One. 2013;8(11):e78941. doi: 10.1371/journal.pone.0078941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavarin R.M., Sanchini S., Marani S., Turino E., Tadonio L., Cantarelli B. Mortality Risk among Cocaine Users before and after the Economic Recession: Results of a Longitudinal Study. European Addiction Research. 2020;26(1):10–19. doi: 10.1159/000503343. [DOI] [PubMed] [Google Scholar]
- PHE . 2020. COVID-19: guidance for commissioners and providers of services for people who use drugs or alcohol. Retrieved from https://www.gov.uk/government/publications/covid-19-guidance-for-commissioners-and-providers-of-services-for-people-who-use-drugs-or-alcohol/covid-19-guidance-for-commissioners-and-providers-of-services-for-people-who-use-drugs-or-alcohol#contents. [Google Scholar]
- Pong K.M., Abdel-Latif M.E., Lui K., Wodak A.D., Feller J.M., Campbell T., Oei J. The temporal influence of a heroin shortage on pregnant drug users and their newborn infants in Sydney, Australia. Australian & New Zealand Journal of Obstetrics & Gynaecology. 2010;50(3):230–236. doi: 10.1111/j.1479-828X.2010.01146.x. [DOI] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N. 2006. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. Retrieved from. [Google Scholar]
- Potier C., Laprevote V., Dubois-Arber F., Cottencin O., Rolland B. Supervised injection services: what has been demonstrated? A systematic literature review. Drug and Alcohol Dependence. 2015;145:48–68. doi: 10.1016/j.drugalcdep.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Pouget E.R., Sandoval M., Nikolopoulos G.K., Friedman S.R. Immediate Impact of Hurricane Sandy on People Who Inject Drugs in New York City. Substance Use & Misuse. 2015;50(7):878–884. doi: 10.3109/10826084.2015.978675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RCCET Changements à l'offre de drogues illicites et à l'accès aux services dans le contexte de la COVID-19, et méfaits pour la santé associés. Alerte du Réseau communautaire canadien d’épidémiologie des toxicomanies. 2020 [Google Scholar]
- Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. doi: 10.1016/S0955-3959(02)00007-5. [DOI] [Google Scholar]
- Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Rodwell T.C., Robertson A.M., Aguirre N., Vera A., Anderson C.M., Lozada R.…Strathdee S.A. Pandemic (H1N1) 2009 Surveillance in Marginalized Populations Tijuana, Mexico. Emerging Infectious Diseases. 2010;16(8):1292–1295. doi: 10.3201/eid1608.100196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll S., Grinstein-Weiss M. Did CARES Act benefits reach vulnerable Americans? Evidence from a national survey. Brookings. 2020 [Google Scholar]; Retrieved from https://www.brookings.edu/research/did-cares-act-benefits-reach-vulnerable-americans-evidence-from-a-national-survey/.
- SAMHSA . 2020. FAQs: Provision of methadone and buprenorphine for the treatment of Opioid Use Disorder in the COVID-19 emergency. [Google Scholar]; Retrieved from https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf.
- Schlosser A., Harris S. Care during COVID-19: Drug use, harm reduction, and intimacy during a global pandemic. International Journal of Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smithson M., McFadden M., Mwesigye S.E., Casey T. The impact of illicit drug supply reduction on health and social outcomes: the heroin shortage in the Australian Capital Territory. Addiction. 2004;99(3):340–348. doi: 10.1046/j.1360-0443.2003.00603.x. [DOI] [PubMed] [Google Scholar]
- Tarjan A., Dudas M., Gyarmathy V.A., Rusvai E., Treso B., Csohan A. Emerging Risks Due to New Injecting Patterns in Hungary During Austerity Times. Substance Use & Misuse. 2015;50(7):848–858. doi: 10.3109/10826084.2015.978672. [DOI] [PubMed] [Google Scholar]
- Tofighi B.G., Williams A.R., Biary R., Rotrosen J., Lee J.D. Outcomes among buprenorphine-naloxone primary care patients after Hurricane Sandy. Addiction Science & Clinical Practice. 2014;9(3) doi: 10.1186/1940-0640-9-3. E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp L., Day C., Degenhardt L. Changes in patterns of drug injection concurrent with a sustained reduction in the availability of heroin in Australia. Drug and Alcohol Dependence. 2003;70(3):275–286. doi: 10.1016/s0376-8716(03)00013-9. [DOI] [PubMed] [Google Scholar]
- Toriello P.J., Morse P.A., Morse E.V., Kissinger P., Pedersen-Wasson E. The resuscitation of a New Orleans substance abuse treatment agency after Hurricane Katrina. Journal of Health Care for the Poor and Underserved. 2007;18(2):482–486. doi: 10.1353/hpu.2007.0050. [DOI] [PubMed] [Google Scholar]
- Trayner K.M.A., McAuley A., Palmateer N.E., Goldberg D.J., Shepherd S.J., Gunson R.N.…Hutchinson S.J. Increased risk of HIV and other drug-related harms associated with injecting in public places: national bio-behavioural survey of people who inject drugs. International Journal of Drug Policy. 2020;77 doi: 10.1016/j.drugpo.2020.102663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner K., Hutchinson S., Vickerman P. The impact of needle and syringe provision and opiate substitution therapy on the incidence of hepatitis C virus in injecting drug users: pooling of UK evidence. Addiction. 2011;106(11):1978–1988. doi: 10.1111/j.1360-0443.2011.03515.x. [DOI] [PubMed] [Google Scholar]
- UNODC . 2020. COVID-19 and the drug supply chain: from production and trafficking to use. [Google Scholar]; Retrieved from https://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf.
- Valdez A., Cepeda A., Negi N.J., Kaplan C. Fumando la piedra: emerging patterns of crack use among Latino immigrant day laborers in New Orleans. Journal of Immigrant and Minority Health. 2010;12(5):737–742. doi: 10.1007/s10903-009-9300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veritas Health Innovation. Covidence systematic review software. Melbourne.
- Wan W.L., H. Cries for help’: Drug overdoses are soaring during the coronavirus pandemic. Washington Post. 2020 [Google Scholar]; Retrieved from https://www.washingtonpost.com/health/2020/07/01/coronavirus-drug-overdose/.
- Weatherburn D., Jones C., Freeman K., Makkai T. Supply control and harm reduction: lessons from the Australian heroin ‘drought’. Addiction. 2003;98:83–91. doi: 10.1046/j.1360-0443.2003.00248.x. [DOI] [PubMed] [Google Scholar]
- Whitfield M., Reed H., Webster J., Hope V. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. International Journal of Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2020). WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Retrieved from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid- 19—11-march-2020
- Wood E., Stoltz J.A., Li K., Montaner J.S., Kerr T. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction. 2006;101(5):689–695. doi: 10.1111/j.1360-0443.2006.01385.x. [DOI] [PubMed] [Google Scholar]
- Xu D. Physical mobility under stay-at-home orders: A comparative analysis of movement restrictions between the U.S. and Europe. Economics and Human Biology. 2020;40 doi: 10.1016/j.ehb.2020.100936. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.