Abstract
Patient: Male, 65-year-old
Final Diagnosis: Heart failure • myocardial infarction • stroke
Symptoms: Right sided weakness
Medication:—
Clinical Procedure: CT scan • echocardiography
Specialty: Cardiology • Infectious Diseases • Medicine, General and Internal • Neurology
Objective:
Unusual clinical course
Background:
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily affects the lungs but can involve any organ. The medical community is struggling to cope with the critical illness associated with the disease. On top of that, patients who have recovered from COVID-19 have presented with complications such as thrombotic episodes in various organs both during and after being infected with SARS-CoV-2. A COVID-19-associated prothrombotic state has been mentioned in multiple recent research articles. The role of anticoagulants is debatable, because even after receiving them prophylactically, many patients have experienced thrombotic episodes. The situation, therefore, represents a challenge to the medical community.
Case Report:
We report on a COVID-19-associated prothrombotic state in a 65-year-old man with no history of comorbid illness. Initially, he presented with right-sided weakness and was found to have had an acute ischemic stroke. Urgent imaging after the stroke revealed changes on electrocardiography that were remarkable for left bundle branch block. The patient’s elevated cardiac enzyme levels correlated with a silent acute myocardial infarction (MI). His echocardiogram revealed a left ventricular (LV) thrombus. He was managed with a multidisciplinary approach involving Neurology, Cardiology, and Medicine.
Conclusions:
COVID-19-associated prothrombotic episodes involving arterial and venous systems have been reported in the literature. But concomitant stroke, acute MI, and LV thrombus rarely have been documented. The role of prophylactic or therapeutic anticoagulation is still unclear because even when patients are on these drugs, they continue to develop thrombotic episodes. Indeed, further studies are required to develop a standard management plan for what can be a fatal situation.
MeSH Keywords: COVID-19, Myocardial Infarction, Stroke, Thrombosis
Background
Since the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic in Wuhan, China in December 2019 as a cluster of unknown pneumonia cases, the infection has become widespread and a pandemic was declared on March 11, 2020 [1]. Currently, the world is striving to gain an understanding of the disease’s pathophysiology so as to achieve an optimal solution. SARS-CoV-2 primarily affects the pulmonary system. However, because of various mechanisms of underlying dysregulated immunity and systemic inflammation, some of which are not well understood, the virus tends to cause extrapulmonary complications, such as stroke, thromboembolic episodes, heart failure, acute kidney injury, and liver injury. [1]. The diagnosis is based on real-time reverse transcription polymerase chain reaction using GeneXpert technology [2]. We report a case of post-COVID-19-associated thrombotic complications in a previously healthy man. He presented with right-sided weakness and was later found to have experienced an acute ischemic stroke. Further investigation revealed an acute myocardial infarction (MI) and left ventricular (LV) thrombus.
Case Report
A healthy 65-year-old man with no previously diagnosed comorbidities or history of smoking, who was not an alcoholic, presented to the Emergency Department within 2 h of onset of right-sided weakness. There was no preceding trauma nor had the patient lost consciousness. On physical examination, he was conscious and oriented to time, place, and person. His initial vital signs revealed a blood pressure of 148/99 mmHg with mild tachypnea and tachycardia of 26/min and 102/min, respectively. His oxygen saturation was normal while breathing room air. The patient’s neurological examination was remarkable for global aphasia, left gaze deviation, right-sided hemiparesis with a decrease in power of 3/5 in both upper and lower limbs, and right hemispatial neglect. Chest auscultation revealed coarse crepitation bilaterally that was mild, diffuse, and scattered. The patient’s cardiovascular examination was unremarkable.
An immediate computed tomography (CT) perfusion scan of the head showed a matched perfusion defect in the left fronto-parieto-temporal region that gave the impression of an infarct with occlusion of the left middle cerebral artery (Figure 1). Because the patient had presented within 2 h of symptom onset, he was eligible for stroke thrombolysis. As per stroke protocol, 5 mg of intravenous alteplase, a tissue plasminogen activator (tPA), was administered, but it was discontinued after 8 minutes because of moderate bleeding from the patient’s oral mucosa.
Figure 1.
Computed tomography perfusion scan of the head. The red arrow points toward the ischemic stroke area and a matching perfusion defect is visible in the left fronto-parieto-temporal region.
Review of some of the upper chest images from the patient’s neck CT scan revealed incidental bilateral peripheral pulmonary consolidations. A chest X-ray was performed, which showed bilateral patchy infiltrates and scattered reticulations (Figure 2). An electrocardiogram showed a left bundle branch block with sinus tachycardia and elevated troponin-T levels suggestive of MI (Figure 3). An echocardiogram was remarkable for compromised left LV function and LV thrombus with severely reduced systolic LV function (26% ejection fraction [EF]) and mild mitral valve regurgitation (Figure 4).
Figure 2.
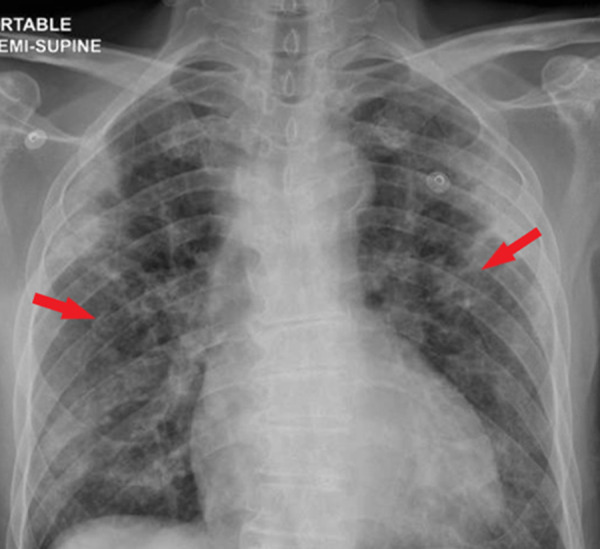
Chest X-ray. Red arrows point to bilateral patchy infiltrates.
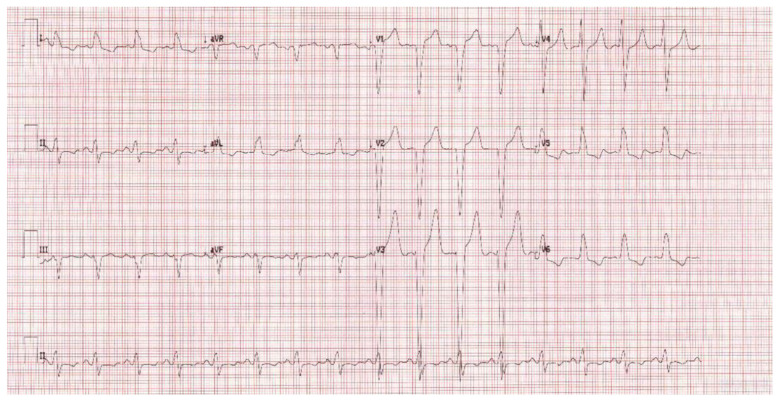
Figure 3.
Electrocardiogram. An electrocardiogram reveals left bundle branch block, broad QRS, and a notched (“M”-shaped) R wave in the lateral leads (v5–v6).
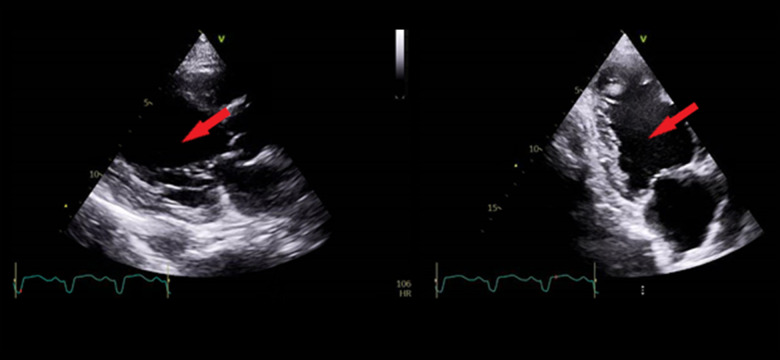
Figure 4.
Transthoracic echocardiography. The red arrows point to a thrombus in the left ventricle.
Given the chest X-ray findings, the patient was isolated and tested for COVID-19 infection. Two COVID-19 reverse transcription polymerase chain reaction (PCR) tests returned negative results. A CT scan of the patient’s chest showed bilateral consolidations with diffuse ground-glass opacities (Figure 5).
Figure 5.
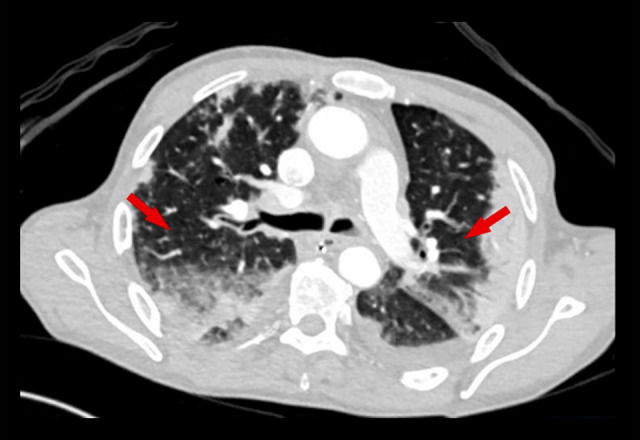
Computed tomography scan of the chest. The red arrows point to bilateral consolidations with diffuse ground-glass opacities.
Further bloodwork showed high levels of C-reactive protein (CRP) and ferritin, elevated levels of interleukins (ILs) and D-dimer, and lymphopenia (Table 1). A multidisciplinary team, including representatives from Neurology, Cardiology, and Internal Medicine, was involved in managing the patient for an acute stroke, MI, and LV thrombus. He was started on aspirin 100 mg, clopidogrel 75 mg, and atorvastatin 40 mg.
Table 1.
Patient laboratory findings.
| Laboratory test | Normal range | Results | Interpretation |
|---|---|---|---|
| Lymphocytes | 1 to 3×103/µL | 0.9×103/µL | Low |
| D-dimer | 0 to 0.44 mg/L | 3.37 mg/L | High |
| CRP | 0 to 5 mg/L | 170.4 mg/L | High |
| Troponin | 3 to 15 ng/L | 189 ng/L | High |
| Interleukin-6 | ≤7 pg/mL | 172 pg/mL | high |
CRP – C-reactive protein.
On the second day of the patient’s admission, he became short of breath, requiring 4L/min of oxygen to maintain saturation. COVID-19 serology was immunoglobulin (Ig) M-negative and IgG-positive, which correlated with his previous infection. Workup for sepsis, including testing for Mycobacterium tuberculosis (sputum smear, PCR, and culture for acid-fast bacillus), PCR for respiratory viruses, and bacterial cultures, were negative. The patient was diagnosed and managed as having post-COVID-19 pneumonia with thrombotic complications. He was started on therapeutic anticoagulation with low-molecular-weight heparin (LMWH) and had no further thrombotic complications.
The patient’s condition gradually improved and he continued physical and occupational therapy in the hospital. A repeat transthoracic echocardiogram done on an inpatient basis 1 month after admission showed resolution of the thrombus but the persistence of the reduced EF (22%). The patient did not deteriorate further during his hospital stay and began to maintain normal oxygen saturation. However, because he was critically ill with myopathy, he is receiving physiotherapy and rehabilitation therapy. He also is being rigorously followed by a consultant cardiologist, and once his condition has been stabilized with the rehabilitation therapy, he is scheduled to undergo coronary angiography on an outpatient basis.
Discussion
Various underlying pathophysiological mechanisms are associated with COVID-19. The SARS-CoV-2 virus manifests as systemic inflammation and immune cell overactivation with the release of cytokines and IL production [3]. Recent evidence also supports an association between COVID-19 and thrombotic events, and the literature has documented cases of both arterial and venous thrombotic events [4]. Thrombotic complications, such as pulmonary embolism, acute aortic thrombosis, cerebral vein thrombosis, coronary artery thrombosis, stroke, and acute superior mesenteric artery thrombosis, are associated with severe COVID-19 illness [5–9]. Although the exact mechanism of a COVID-19 hypercoagulable state remains unclear, Haimei proposed that the increased risk of thrombosis in patients with COVID-19 is related to SARS- CoV-2-mediated enhanced angiotensin-converting enzyme 2 (ACE2) activation, which is an essential component of the renin-angiotensin system expressed by vascular endothelial cells. ACE2 converts angiotensin (Ang) 2 into Ang-(1–7) and Ang 1 into Ang-(1–9), respectively [10]. Ang-(1–9) causes an imbalance between the plasma concentration of tPA and plasminogen activator inhibitor-1 (PAI-1), resulting in an increased risk of thrombosis [10]. Another suggested mechanism involves elevation of D-dimer levels and presence of antiphospholipid antibodies, which are frequently reported in patients with COVID-19 who have vascular thrombotic complications and can lead to thrombotic events [11].
Our patient initially presented with stroke. Further investigation revealed acute MI and an LV thrombus was seen on echo-cardiography, which might have been the cause of his stroke. The reason for the LV thrombus could be related to a low EF after a silent MI. On the other hand, the possible rationale for silent MI can be attributed to SARS- CoV-2-related coronary artery thrombosis; however, it can only be confirmed after coronary angiography. The cardiologist suggested that our patient not undergo that test because of his history of acute stroke. The patient does not have any of the traditional risk factors for development of thrombosis, such as a hypercoagulable state, nor previously known thrombophilia or a family history of thrombosis. Hence, because he had positive IgG antibodies against the SARS-CoV-2 virus, the likely explanation is a post-COVID-19-associated prothrombotic state that led to a MI, stroke, and LV thrombus.
There may be several approaches to management of hyper-coagulability associated with COVID-19. In a narrative review, Carfora et al. suggested using anti-inflammatory drugs (corticosteroids and human monoclonal antibodies) or statins and ACE-I, which reduce endothelial dysfunction in keeping with their proposed mechanisms of action. LMWH usually also is used to prevent thrombosis [12]. In an observational cross-sectional prospective study by Ionescu et al., therapeutic anticoagulation was found to have better efficacy in preventing thrombotic episodes in severe COVID-19, leading to a decrease in mortality [13]. Similarly, Nadkarni and Lala, in a retrospective observational study of 4389 elderly individuals confirmed to be COVID-19-positive, evaluated the role of anticoagulation in decreasing mortality and intubation in hospitalized patients [14]. In a multicenter, prospective cohort study, Helms et al. reported an increased risk of thrombosis associated with severe COVID-19 disease despite the fact that the patients were kept on prophylactic or therapeutic anticoagulation [15]. Overall, the results of research in this area show a lower risk of thrombosis in patients receiving preventive and therapeutic doses of anticoagulants. However, optimal types and regimens are yet to be explored.
Conclusions
Published reports indicate that some patients with COVID-19 infection have received anticoagulants as prophylaxis and also for therapy, with beneficial results in terms of reduction in associated thrombotic episodes. Currently, there are no guidelines or recommendations for prevention of COVID-19-associated thrombosis, raising a critical concern about the need for further studies of ways to avoid this life-threatening situation.
References:
- 1.Zaim S, Chong JH, Sankaranarayanan V, et al. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45(8):100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Axell-House DB, Lavingia R, Rafferty M, et al. The estimation of diagnostic accuracy of tests for COVID-19: A scoping review. J Infect. 2020;81(5):681–97. doi: 10.1016/j.jinf.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McFadyen JD, Stevens H, Karlheinz P. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res. 2020;127(4):571–87. doi: 10.1161/CIRCRESAHA.120.317447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Berre A, Marteau V, Emmerich J, et al. Concomitant acute aortic thrombosis and pulmonary embolism complicating COVID-19 pneumonia. Diagn Interv Imaging. 2020;101(5):321–22. doi: 10.1016/j.diii.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavalcanti DD, Raz E, Shapiro M, et al. Cerebral venous thrombosis associated with COVID-19. Am J Neuroradiol. 2020;41(8):1370–76. doi: 10.3174/ajnr.A6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shams A, Ata F, Mushtaq K, et al. Coronary thrombosis in a young male with COVID-19. IDCases. 2020;21:e00923. doi: 10.1016/j.idcr.2020.e00923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung S, Quiwa JC, Pillai A, et al. Superior mesenteric artery thrombosis and acute intestinal ischemia as a consequence of COVID-19 infection. Am J Case Rep. 2020;21:e925753-1–3. doi: 10.12659/AJCR.925753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haimei M. Pathogenesis and treatment strategies of COVID-19-related hypercoagulant and thrombotic complications. Clin Appl Thromb. 2020;26:1076029620944497. doi: 10.1177/1076029620944497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID-19. N Engl J Med. 2020;382(17):e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carfora V, Spiniello G, Ricciolino R, et al. Anticoagulant treatment in COVID-19: A narrative review. J Thromb Thrombolysis. 2020 doi: 10.1007/s11239-020-02242-0. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ionescu F, Grasso-Knight G, Castillo E, et al. Therapeutic anticoagulation delays death in COVID-19 patients: Cross-sectional analysis of a prospective cohort. TH Open. 2020;4(3):e263–70. doi: 10.1055/s-0040-1716721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadkarni GN, Lala A, Bagiella E, et al. A single health system study. J Am Coll Cardiol. 2020;76(16):1815–26. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–98. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]