This editorial refers to ‘Novel antisense therapy targeting microRNA-132 in patients with heart failure: results of a first-in-human Phase 1b randomized, double-blind, placebo-controlled study’†, by T. Thum et al., on page 178.
Heart failure (HF) is frequent, lethal, and expensive.1 In spite of remarkable progress in clinical management of patients and use of devices, the prognosis of this condition remains poor, with mortality rates estimated at 6–7% at 1 year in patients with chronic HF and at ≥25% in those hospitalized with acute HF.2 HF is also tremendously expensive, representing 2–3% of national health expenditures in high-income countries3 and a projection to more than double in the next 20 years as a result of the population ageing.4 Current drug treatment for HF has not evolved significantly recently. Standard of care includes drugs [angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, mineralocorticoid receptor antagonists, ivabradin, and, more recently, combined ARB–neprilysin inhibitors5] that have been developed based on patho-physiological discoveries dated decades ago. Most notably, all the available drugs are small molecules. At this present time, not a single biological drug (recombinant protein, peptide, nucleic acid, or monoclonal antibody) is available for a disease as prevalent as HF.
It is in this setting that the recent development of novel nucleic acid therapeutics is most welcome news. In this issue of the European Heart Journal, Thum and collaborators report the first-in-human data for an antisense locked nucleic acid (LNA) oligonucleotide (CDR132L) targeting microRNA (miR)-132-3p for HF patients.6 That non-coding nucleic acids, and miRNAs in particular, play a fundamental role in the pathophysiology of HF is a notion that has gained progressive ground over the last decade. Several miRNAs are known to be expressed in a dysregulated manner during disease progression, hence the therapeutic opportunity of manipulating their levels through the design of antisense molecules. An attractive mechanistic consideration for miRNA targeting is the ability of a single intervention targeting one miRNA to influence the expression of multiple genes both within and between important pathways relevant to the disease. This is mediated through the well-known mechanism of action of miRNAs, by which an individual molecule can target multiple mRNAs, inducing their degradation or blocking their translation.
While the original proposal of creating an ‘antisense’ oligonucleotide-based drug to inhibit RNA dates back three decades,7 the field of RNA-targeted therapeutics has now matured significantly, with several RNA-targeting drugs already approved for commercial use and several others in the final phases of the clinical trial pipeline.8,9 This progress was rendered possible by significant improvements in the chemical modification of antisense nucleic acids to increase their pharmacological properties while maintaining Watson–Crick base pairing. In particular, the inclusion of LNA nucleotides in the antisense oligonucleotide increases both stability and thermodynamic strength of duplex formation with complementary target RNAs.10 The efficacy of this approach in the cardiovascular field is also highlighted by recent evidence in humans injected with an LNA antagonist to miR-92a-3p, an agent that is being developed for intervention in cardiovascular disease and wound healing. At doses up to 1.5 mg/kg, this LNA molecule showed dose-dependent decreases in circulating miR-92a levels and target derepression in the peripheral blood compartment. This encouraging study has provided early evidence of target-specific activity following injection of miRNA antagonists into humans.11
The work by Thum and collaborators on miR-132-3p inhibition in HF has progressively built momentum from pre-clinical studies to the first-in-human trial reported in this issue.6 First, the miR-132 stem–loop is part of a cluster (the miR-212/132 family). This stem–loop cluster is responsive to HF cues and its expression is activated in cells and experimental models mimicking HF conditions. Second, two miRNAs from this cluster (i.e. miR-212 and miR-132) both independently regulate similar target genes in the heart, in particular a member of the FoxO gene family (both miRNAs directly target FoxO312), which contributes antihypertrophic signals by regulating calcineurin signalling in cardiomyocytes as well as autophagy.12–14 Third, and the most important finding from a translational context, inhibition of miR-132-3p alone (i.e independent of miR-212) via an antisense oligonucleotide approach is sufficient to block the development of cardiac hypertrophy and transition to heart failure in multiple mouse models.12 With this is at hand, a subsequent expansive large animal study has provided definitive pre-clinical evidence of dosing regimens, safety, and efficacy.12 In this randomized study, which assessed both intravenous and intracoronary delivery, medium and high doses of the miR-132-3p LNA inhibitor (5 mg/kg and 10 mg/kg, respectively) were effective at improving cardiac function and reducing brain natriuretic peptide (BNP) levels, while not affecting evolution of the fibrotic scar or cardiac revascularization. It was previously shown that deletion of the same axis in mice positively affects angiogenesis in vivo,15 thus it is important to note that this mechanism of action is not obviously relevant in the context of revascularization in the heart post-injury.
Now, the same team of investigators report the first-in-human data from this antisense oligonucleotide strategy for HF patients with New York Heart Association (NYHA) class I–III and left ventricular ejection fraction (LVEF) >30% (Take home figure).6 The study design was a prospective, randomized, and placebo-controlled phase 1b dose-escalation study. The dosing regimen involving 28 patients at four dose cohorts and placebo (5:2 design) up to a maximum of 10 mg/kg intravenously 4 weeks apart. The dosing regimen, in general, appeared to be safe and well tolerated. The study drug was readily detected in the plasma of all dosed patients in the absence of drug accumulation. Critically, plasma levels of miR-132-3p were dose-dependently reduced in patients receiving the drug. Based on predictive pharmacokinetic modelling, the team pooled the placebo and low dose groups and three higher dose groups into two pools [non-pharmacodynamic (PD)-active and PD-active, respectively; 27 patients in total]. Using this strategy, a number of efficacy measures were assessed, including NT-proBNP, LVEF and NT-proBNP combined, biomarkers of HF, and cardiac fibrosis, as well as QRS complex narrowing. Although some trends and significance were noted, the study design at this phase 1b stage was clearly underpowered for efficacy measures. What is striking, however, is the encouraging safety, tolerability, and dose-dependent target reduction in the plasma observed, supported by valuable prediction modelling of dosing from porcine efficacy and safety studies. There is indeed great encouragement embedded within this important dataset.
Graphical abstract .
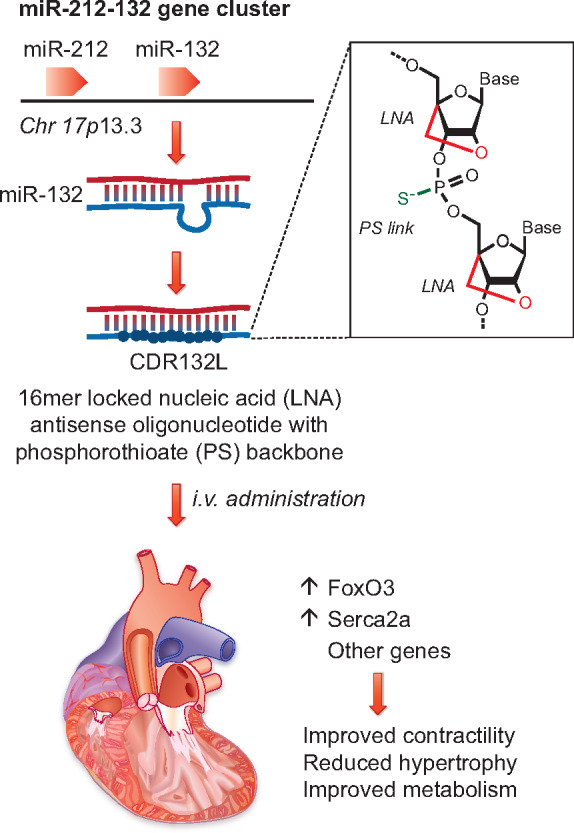
Thum and co-workers6 show that inhibition of miR-132, which is expressed from the miR-212-132 locus on human chromosome 17, results in increased levels of FoxO3 and Serca2a and improved cardiac function. Inhibition is achieved by administering a chemically modified oligonucleotide (CDR132L), which contains locked nucleic acid (LNA) nucleotides and phosphonothioate (PS) linkages to increase in vivo stability.
More broadly, this study is also important to the field to guide additional investigations targeting miRNAs and other RNA species using oligonucleotide approaches in cardiovascular patients. The 4-weekly dosing regimen, the chemistry, and the pharmacokinetics all show encouraging signs for use in humans. In summary, this first-in-human study targeting miR-132-3p described here represents a considerable advance in the field of miRNA therapeutics in cardiovascular disease. While it is too early to indicate whether the strategy will be efficacious in human, the safety and feasibility herein described, when combined with the detailed evidencing of efficacy in small and large animal models, provides tremendous encouragement for progression of further studies in patients with HF. The results of the next phase in this exciting journey will be eagerly awaited by the field.
Acknowledgements
A.H.B. is supported by the British Heart Foundation programme grant RG/14/3/30706 and Chair of Translational Cardiovascular Sciences CH/11/2/28733, European Research Council Advanced Grant 338991 VASCMIR, and from the European Union’s Horizon 2020 Programme for Research and Innovation (Cardioregenix: 825670). M.G. is supported by the European Research Council (ERC) Advanced Grant 787971 ‘CuRE’, by the British Heart Foundation (BHF) Programme Grant RG/19/11/34633, and the King’s College London BHF Centre of Research Excellence grant RE/18/2/34213; and by grants 825670 ‘CardioReGenix’ and 874764 ‘REANIMA’ from the European Commission Horizon 2020 programme.
Conflicts of interest: none declared.
Footnotes
† doi:10.1093/eurheartj/ehaa898.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Arnlov J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Barnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castaneda-Orjuela CA, Castillo-Rivas J, Catala-Lopez F, Choi JY, Christensen H, Cirillo M, Cooper L Jr, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, El Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, El Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabares-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C.. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, Ferrari R, Piepoli MF, Delgado Jimenez JF, Metra M, Fonseca C, Hradec J, Amir O, Logeart D, Dahlstrom U, Merkely B, Drozdz J, Goncalvesova E, Hassanein M, Chioncel O, Lainscak M, Seferovic PM, Tousoulis D, Kavoliuniene A, Fruhwald F, Fazlibegovic E, Temizhan A, Gatzov P, Erglis A, Laroche C, Mebazaa A, Heart Failure Association of the European Society of Cardiology. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail 2016;18:613–625. [DOI] [PubMed] [Google Scholar]
- 3. Cook C, Cole G, Asaria P, Jabbour R, Francis DP.. The annual global economic burden of heart failure. Int J Cardiol 2014;171:368–376. [DOI] [PubMed] [Google Scholar]
- 4. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 6. Täubel J, Hauke W, Rump S, Viereck J, Batkai S, Poetzsch J, Rode L, Weigt H, Genschel C, Lorch U, Theek C, Levin AA, Bauersachs J, Solomon SD, Thum T. Novel antisense therapy targeting microRNA-132 in patients with heart failure: results of a first-in-human Phase 1b randomized, double-blind, placebo-controlled study. Eur Heart J 2021;42:178–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stephenson ML, Zamecnik PC.. Inhibition of Rous sarcoma viral RNA translation by a specific oligodeoxyribonucleotide. Proc Natl Acad Sci USA 1978;75:285–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crooke ST, Witztum JL, Bennett CF, Baker BF.. RNA-targeted therapeutics. Cell Metab 2018;27:714–739. [DOI] [PubMed] [Google Scholar]
- 9. Setten RL, Rossi JJ, Han SP.. The current state and future directions of RNAi-based therapeutics. Nat Rev Drug Discov 2019;18:421–446. [DOI] [PubMed] [Google Scholar]
- 10. Elmen J, Lindow M, Schutz S, Lawrence M, Petri A, Obad S, Lindholm M, Hedtjarn M, Hansen HF, Berger U, Gullans S, Kearney P, Sarnow P, Straarup EM, Kauppinen S.. LNA-mediated microRNA silencing in non-human primates. Nature 2008;452:896–899. [DOI] [PubMed] [Google Scholar]
- 11. Abplanalp WT, Fischer A, John D, Zeiher AM, Gosgnach W, Darville H, Montgomery R, Pestano L, Allee G, Paty I, Fougerousse F, Dimmeler S.. Efficiency and target derepression of anti-miR-92a: results of a first in human study. Nucleic Acid Ther 2020;doi: 10.1089/nat.2020.0871. [DOI] [PubMed] [Google Scholar]
- 12. Foinquinos A, Batkai S, Genschel C, Viereck J, Rump S, Gyongyosi M, Traxler D, Riesenhuber M, Spannbauer A, Lukovic D, Weber N, Zlabinger K, Hasimbegovic E, Winkler J, Fiedler J, Dangwal S, Fischer M, de la Roche J, Wojciechowski D, Kraft T, Garamvolgyi R, Neitzel S, Chatterjee S, Yin X, Bar C, Mayr M, Xiao K, Thum T.. Preclinical development of a miR-132 inhibitor for heart failure treatment. Nat Commun 2020;11:633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ronnebaum SM, Patterson C.. The FoxO family in cardiac function and dysfunction. Annu Rev Physiol 2010;72:81–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ni YG, Berenji K, Wang N, Oh M, Sachan N, Dey A, Cheng J, Lu G, Morris DJ, Castrillon DH, Gerard RD, Rothermel BA, Hill JA.. Foxo transcription factors blunt cardiac hypertrophy by inhibiting calcineurin signaling. Circulation 2006;114:1159–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kumarswamy R, Volkmann I, Beermann J, Napp LC, Jabs O, Bhayadia R, Melk A, Ucar A, Chowdhury K, Lorenzen JM, Gupta SK, Batkai S, Thum T.. Vascular importance of the miR-212/132 cluster. Eur Heart J 2014;35:3224–3231. [DOI] [PubMed] [Google Scholar]


