Abstract
Objectives
Multimorbidity, defined as the co-occurrence of at least two chronic diseases, is a common occurrence with ageing and a recognised public health concern, especially during the COVID-19 pandemic. The multimorbidity population is more susceptible to the virus, its complications, and death. The study aimed to explore the multimorbidity characteristics and their associations at a population level for the first time in Malta. Such data enables adequate priority and policy planning due to COVID-19’s predilection for this population.
Study and methods
Baseline data was collected from 3,947 adults recruited between 2014-2016 through a cross-sectional study. A single-stage sampling strategy was implemented and stratified by age (18 –70 years), sex and locality. Participants were invited to attend a health examination survey consisting of a questionnaire, anthropometric and biological measurements. Descriptive (chi-square) and analytic (regression modelling) statistics were used to determine the characteristics and associations of the multimorbidity population. The chronic diseases considered for multimorbidity were type 2 diabetes, obesity, hypertension, myocardial infraction, coronary heart disease and dyslipidaemia.
Results
Multimorbidity was present in 33% (95% confidence interval 31.54–34.47) of the study population, with a male predominance. Hypertension and myocardial infarction were the commonest multimorbidity combination from a young age group (20–30 years). Low socio-economic status and residing on the island of Gozo were positively associated with multimorbidity.
Conclusion
Multimorbidity in Malta was evident from a young age, with the highest occurrence among the low socio-economic status and residents of Gozo, bringing forward the need for preventive action. An adaptive healthcare system and policies are recommended to prevent, support, and manage multimorbidity non-communicable diseases while bracing for the current COVID-19 pandemic.
Keywords: Noncommunicable diseases, Multimorbidity, Coronavirus, Population health, Policies, Malta
The ageing population and prolonged life expectancy are global challenges with consequential impacts on the healthcare systems.1 Multimorbidity, defined as the co-occurrence of at least two chronic diseases, is a common occurrence in the current ageing era and a recognised serious public health concern.2 The understanding of multimorbidity is exceptionally more relevant during the COVID-19 pandemic. These individuals have been reported to experience poorer health outcomes if infected by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV2).3 Furthermore, a correlation has been reported between the burden of non-communicable diseases and COVID-19 deaths.4 Hence, a comprehensive understanding of the multimorbidity prevalence, characteristics, and determinants at a country level is paramount to enable adequate priority and policy planning, especially during the COVID-19 pandemic.
The Maltese archipelago is made up of two sister islands (Malta and Gozo), found in the middle of the Mediterranean Sea. This small European island state is a well-documented ageing country with 18.8% of the total population noted to be 65+ years in 2017. Life expectancy has been on the incline with an average life expectancy of 80.2 years for males and 84.6 years for females for the year 2017, both above the European average. Following the paradigm of ‘one patient – one disease,’ it has been reported that diabetes, obesity, and hypertension are highly prevalent within the adult Maltese population.5, 6, 7 However, to the best of our knowledge, multimorbidity at a population level has never been investigated among the Maltese Islands population. The aim of this study was to explore the multimorbidity characteristics and their associations at a population level (18–70 years) in view of the fact that COVID-19 has a predilection for this population.
Malta’s multimorbidity population characteristics
The total study population was 3,947 adults (18–70 years) with a male predominance (n = 1,998). Multimorbidity was present in 33% (95%: confidence interval [CI] 31.54–34.47; n = 1,302) of the study population, with a male predominance (58.53%, n = 762; P = <0.01). The multimorbidity population was composed of 56% having two chronic diseases, 27% with three chronic diseases, 8% with four chronic diseases, 9% with five chronic diseases, and 1% with six chronic diseases. On age stratification, as expected, the frequency of multimorbidity increased with increasing age (P = 0.01). Interestingly, multimorbidity was observed to be present from a young age (20–29 years) with the presence of two concurrent chronic diseases. On a population level, 50% of the 60–to 69-year-olds showed multimorbidity.
Malta is a well-known diabetogenic country,5 , 6 yet the commonest multimorbidity out of all the subpopulations, was the concurrent presence of hypertension and myocardial infarction (54.45% , 95%CI: 51.74–57.14; n = 709). In fact, only 1.61% (95%: CI 1.04–2.47; n = 21) had the concurrent presence of type 2 diabetes and obesity (two chronic diseases). Meanwhile, a total of 17.51% (95%: CI 15.54–19.67; n = 228) of the multimorbidity subpopulation had the presence of type 2 diabetes as part of their multimorbidity status.
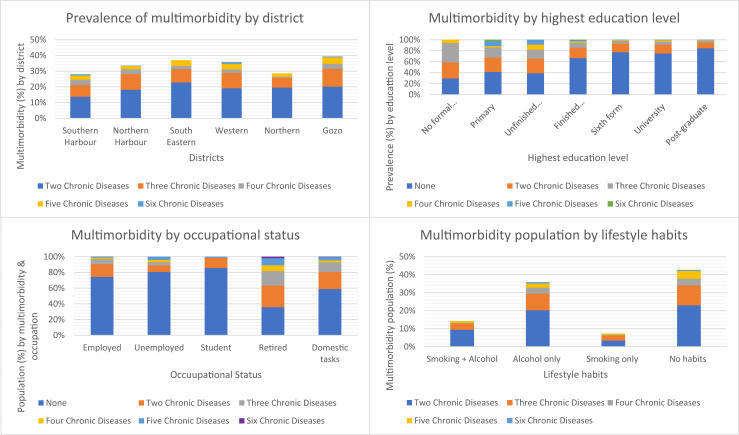
The small sister island of Gozo (one district) was observed to have the highest multimorbidity occurrence out of the six districts (P = <0.01), as shown in Fig. 1 . An inverse relationship was observed between multimorbidity and education level (Fig. 1), while those that reported as having retired (typically 61+ years) exhibited the highest frequency of multimorbidity, as shown in Fig. 1. While a higher tendency (42.66%, 95%CI: 40.00–45.36) of following a non-smoking and none alcohol consumption lifestyle habits was noted (Fig. 1), followed by 35.82% (95%CI:33.26–38.46) reporting to have an alcohol consumption habit.
Fig. 1.
Distribution of multimorbidity by socio-economic and lifestyle status.
Relationships between different socio-economic and lifestyle habits were evident. Indeed, low education level (no formal education odds ratio [OR]:7.95 P = <0.01; primary education OR:6.98, P = <0.01; unfinished secondary education OR:7.68, P = <0.01 and finished secondary odds ratio [OR]:2.37, P = <0.01) was synergistically associated with the presence of multimorbidity when compared to postgraduate education. On adjusting for age and sex (OR:2.07, P = 0.02) and then further adjusting for socio-economic status (for occupation and locality: OR:2.06, P = 0.02), only unfinished secondary level (up to 9 years of compulsory education) was observed to be associated with the presence of multimorbidity. Meanwhile, an inverse relationship with multimorbidity was observed for those employed (OR: 0.45, P = <0.01) and for students (OR: 0.05, P = <0.01) when compared to domestic tasks as a full-time job. Conversely, those reporting to be retired were associated with the presence of multimorbidity (OR:2.62 ,P = 0.01). However, significance was lost after adjusting for age, sex and socio-economic status. The sister island of Gozo was significantly independently associated with multimorbidity even after adjusting for age, sex, and socio-economic status (OR:1.69, P = <0.01). A non-smoking (OR:1.35, P = 0.01) and none alcohol consumption (OR:1.31, P = <0.01) habits both exhibited an association with multimorbidity following univariant logistic regression analyses. However, on adjusting for potential confounders, only none alcohol consumption habit remained associated with the presence of multimorbidity (OR:1.24, P = 0.03).
Discussion
The prevalence of multimorbidity is on the rise, with a meta-analysis study reporting an average frequency of 33.1% at a global level,8 similar to this current study’s finding. Ageing is the usual contributing risk factor for the development of multimorbidity as a consequence of chronic multiorgan system dysregulation. Hence, the presence of multimorbidity from the young age of 20 years, as shown in this study, brings forward the need for immediate action, including consideration of early onset of population screening for signs of common non-communicable diseases (NCDs), apart from further research. Additionally, the presence of cardiometabolic multimorbidity as the dominating chronic disease from a young age within this study population predisposes this population further to COVID-19 infectious disease risk. Indeed, individuals with multiple conditions have a higher susceptibility to infectious diseases and less resistance to withstand acute health threats. Notwithstanding the higher burden imposed on the healthcare systems due to the dual communicable and non-communicable diseases.
On a population level, the second wave of COVID-19 in Malta saw a drastic increase in COVID-19 cases and hospitalization among the young with a spill off to the elderly.9 Consequentially, a drastic spike in COVID-19 mortality was reported among the elderly (average age 84 years; males 56.10%), all of whom suffered from multimorbidity.9 The male COVID-19 mortality predominance coincides not only with global COVID-19 mortality gender distribution but with this current study’s findings. In Malta, it has already been reported that the male population, as well as the Gozo district, have a worse metabolic profile when compared to their female counterparts. One of the potential reasons was noted to be the higher frequency of overweight and obese status and increase in sedentary work and lifestyle among the men.5 , 6
Despite the small geographical area, the metabolic discrepancies between the districts have never been investigated before, and this merits further research. However, it appears that the short 20 min ferry ride between the main island of Malta and the small island of Gozo might have a social, cultural, and physical effect on health. The relationship between low socio-economic status and risk of multimorbidity was revalidated by this study. While the relationship between none alcohol habits and risk of multimorbidity is not the typically reported relationship, a possible reason for this is that it is customary for patients with chronic diseases to be advised to stop all bad habits, including alcohol consumption.
Implications for policy and practice
Policymakers should comprehend that multimorbidity is a common occurrence and not the exception, even among the younger generations and that the main action goal should be to prevent the occurrence of multimorbidity. Country-specific characteristics of the multimorbidity population act as the foundations for such preventive policies, especially during the pandemic, following the fact that COVID-19 has a predilection for this population. Indeed, a syndemic strategy is required to fight the pandemic while preventing and managing non-communicable diseases (NCDs). Preventing COVID-19 spread will inevitably reduce NCDs progression and prevent complications. Such syndemic strategies include disease surveillance of both COVID-19 and NCDs, robust containment and preventive public health strategies and policies with clear communication to the public, strong civil society, and a resilient universal healthcare system. The healthcare system in Malta is very accessible, with multiple primary healthcare hubs and an acute hospital all free of charge for the tax-paying population, with comprehensive access and health care coverage. Yet, multimorbidity is evident despite the universal healthcare system, implying that other factors are contributing to these comorbidities. It is evident from this study that tackling social determinants of health while considering demographic characteristics need to be considered in Malta. This requires a multisectoral and multistakeholder approach to establish a whole of the society action plan. Considering that the Maltese Islands are obesogenic, tackling the obesogenic environment is a requisite, even more importantly during COVID-19 restrictions. Increasing accessibility to green and open spaces to encourage physical activity will have a positive preventive effect on a number of common NCDs comorbidities, as well as on the population’s mental health status. Indeed, the reduction in social activities and isolation brought about by COVID-19 further increased the population’s susceptibility to mental health problems. Such problems are known to be requisites for the development of other NCDs and the presence of multimorbidity. Hence, the accessibility to helplines, psychological and social support within the communities would aid in preventing the development of comorbidities within the population. Food insecurity is another important aspect that needs to be tackled. In light of the pandemic, providing subsidies on nutritional value food is a way to encourage adequate nutritional food intake and aid in the prevention of comorbidities, including obesity and cardiovascular disease.
It is acknowledged that policymakers face a common debacle as to how to assign adequate resources and healthcare services to meet the demands of the growing burden of non-communicable diseases and multimorbidity.10 However, healthcare planning and preventive care are an investment and not an expense. In fact, it is recommended that preventive care through early screening is to be considered in dealing with the growing multimorbidity occurrence in Malta. Clinical guidelines considering multimorbidity are rare due to the complex interactions of different chronic diseases and polypharmacy; however, in this multimorbidity era, such guidelines are recommended based on clinical trials, as well as multimorbidity studies, similar to this current study. The importance of such action is even more highlighted in the current pandemic unprecedented times, where the multimorbidity subpopulation is more at risk of acquiring the viral infection, as well as for complications and mortality. At the onset of the pandemic, most of the healthcare services were disrupted. Essential services, screening programs, as well as planned consultation appointments were reduced or cancelled as part of the COVID-19 mitigation measures. Although such actions were taken to curb the viral spread, the care of the multimorbidity population, also considered as vulnerable population during the pandemic, was invariably affected. It is anticipated that these measures will have a long-term devastating consequence to individuals, including those asymptomatic, as well as those with multimorbidity. Hence, an adaptive healthcare system to deal with both COVID-19 and NCDs is required. Tools to facilitate communication between the public and the healthcare professionals should be implemented through the use of telehealth and telemedicine, as well as increasing the access to local and social support. Institution of policies is recommended to prevent, support, and manage non-communicable diseases while bracing for the current COVID-19 pandemic.
Author statements
Acknowledgements
The authors are extremely grateful for the strong support forthcoming from the University of Malta (through the Medical School and Research Innovative Development Trust department) and from the Alfred Mizzi Foundation as major sponsors, as well as that of a host of others, including Atlas Health Insurance (Malta). The in-kind support and encouragement of the Parliamentary Secretariat for Health of the Government of Malta is also gratefully acknowledged. Furthermore, a note of appreciation and acknowledgement is forwarded to Professor Julian Mamo, Professor Josanne Vassallo, and Professor Neville Calleja for their continuous support and advice during the academic progression.
Ethical approval
The Research Ethics Committee of the Faculty of Medicine and Surgery at the University of Malta granted approval.
Funding
Funding was obtained from the University of Malta, Alfred Mizzi Foundation, and Atlas Insurance (Malta). Funding had no role in the design of the study, analysis, and interpretation of data and in writing the manuscript.
Competing interests
The authors declare no conflict of interest.
References
- 1.Garin N., Koyanagi A., Chatterji S., Tyrovolas S., Olaya B., Leonardi M. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016 Feb;71(2):205–214. doi: 10.1093/gerona/glv128. http://www.ncbi.nlm.nih.gov/pubmed/26419978 [Internet]. [cited 2020 Sep 14] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li J., Green M., Kearns B., Holding E., Smith C., Haywood A. Patterns of multimorbidity and their association with health outcomes within Yorkshire, England: baseline results from the Yorkshire Health Study. BMC Publ Health. 2016;16:649. doi: 10.1186/s12889-016-3335-z. http://www.ncbi.nlm.nih.gov/pubmed/27464646 [Internet]. [cited 2020 Sep 14] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. http://www.ncbi.nlm.nih.gov/pubmed/31986264 (London, England) [Internet]. [cited 2020 Apr 22] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azarpazhooh M.R., Morovatdar N., Avan A., Phan T.G., Divani A.A., Yassi N. COVID-19 pandemic and burden of non-communicable diseases: an ecological study on data of 185 countries. J Stroke Cerebrovasc Dis. 2020 Sep;29(9):105089. doi: 10.1016/j.jstrokecerebrovasdis.2020.105089. http://www.ncbi.nlm.nih.gov/pubmed/32807484 [Internet]. [cited 2020 Sep 10] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuschieri S. The diabetes epidemic in Malta. South East Eur J Public Heal. 2020 Feb 19;8 [Google Scholar]
- 6.Cuschieri S., Vassallo J., Calleja N., Camilleri R., Borg A., Bonnici G. vol. 2. Wiley-Blackwell; 2016. Prevalence of obesity in Malta [Internet] pp. 466–470.http://www.ncbi.nlm.nih.gov/pubmed/28090352 (Obesity science and practice). [cited 2017 Oct 7] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuschieri S., Vassallo J., Calleja N., Pace N., Mamo J. The effects of socioeconomic determinants on hypertension in a cardiometabolic at-risk European country. Int J Hypertens. 2017;2017 doi: 10.1155/2017/7107385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen H., Manolova G., Daskalopoulou C., Vitoratou S., Prince M., Prina A.M. Prevalence of multimorbidity in community settings: a systematic review and meta-analysis of observational studies. J Comorbidity. 2019;9 doi: 10.1177/2235042X19870934. http://www.ncbi.nlm.nih.gov/pubmed/31489279 [Internet].[cited 2020 Sep 10] 2235042X19870934. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuschieri S., Balzan M., Gauci C., Aguis S., Grech V. Mass events trigger Malta's second peak after initial successful pandemic suppression. J Community Health. 2020 Sep 16:1–8. doi: 10.1007/s10900-020-00925-6. http://link.springer.com/10.1007/s10900-020-00925-6 [Internet]. [cited 2020 Sep 17] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corrao G., Rea F., Carle F., Di Martino M., De Palma R., Francesconi P. Measuring multimorbidity inequality across Italy through the multisource comorbidity score: a nationwide study. Eur J Public Health. 2020 Oct 1;30(5):916–921. doi: 10.1093/eurpub/ckaa063. https://academic.oup.com/eurpub/article/30/5/916/5841175 [Internet]. [cited 2020 Oct 10] Available from: [DOI] [PubMed] [Google Scholar]