Abstract
Purpose
We aimed to evaluate utilization of inpatient hospital and critical care services among critically ill neurologic patients during the COVID-19 pandemic. We hypothesized, based on prior observations among ischemic stroke patients, that there would be significant decline in critically ill neurologic patients presenting to hospitals during the pandemic which may impact outcomes.
Methods
We used TriNetX, a large research network, collecting real-time electronic medical records data. We extracted data on utilization of critical care and hospital inpatient services among cohorts of patients with common neurocritical conditions between January–June 2020 and compared it to data from similar time-frames in previous years. We also compared clinical outcomes, comprising need for intubation and 30-day mortality, among these cohorts.
Results
We found a 28.1% reduction in intensive care unit (ICU) admissions with critical neurologic illnesses in 2020 when compared to 2019 (8568 vs. 11,917 patients, p < 0.0001) and a 34.4% reduction compared to 2018 (8568 vs. 13,064 patients, p < 0.0001). However, there was no statistically significant difference in mortality (2020: 12.2 vs. 2019: 12.4%; p = 0.7; vs. 2018: 12.6%; p = 0.62) or intubation rates across the years among patients using critical care services. There was 1% increase in mortality among non-ICU patients with similar diagnoses in 2020 compared to previous years (2020: 3.9% vs. 2019: 2.9% vs. 2018: 3.1%; p < 0.0001, p = 0.0001), but no difference in intubation rates.
Conclusion
There was a significant reduction in hospital and ICU admissions among patients with acute neurologic emergencies in 2020, after onset of COVID-19 pandemic, compared to previous years. While we did not find a significant difference in mortality among patients admitted to the ICU, there was slightly higher mortality among non-ICU patients with same diagnoses in 2020 compared to previous years. Prospective evaluation and further investigation into the reasons for these trends is needed.
Keywords: COVID-19, Critical illness, Neurologic, Neurocritical care
Highlights
-
•
There was a 30% reduction in hospitalizations among critically ill neurologic patients during the COVID-19 pandemic.
-
•
However, mortality was not significantly worse during the COVID-19 pandemic among critically ill neurologic patients.
-
•
Simultaneous COVID-19 infection was seen in 1.4% neurocritical patients with highest incidence in acute ischemic stroke.
1. Introduction
Reports from Italy (Carenzo et al., 2020) have demonstrated that the COVID-19 pandemic has imposed an overwhelming demand on healthcare systems leading to resource rationing (Emanuel et al., 2020). Critically ill neurologic patients are often perceived to have poor outcomes leading to premature limitation in care even prior to the pandemic (Becker et al., 2001). Therefore, during a COVID-19 surge, these patients may receive limited care leading to worse outcomes. Additionally, neurologic disease and COVID-19 infection may co-exist, either as a manifestation of COVID-19 infection (Nalleballe et al., 2020), a consequence of severe systemic illness such as hypoxia, or in the form of simultaneous COVID-19 infection in patients with primary neurologic illness. Each of these scenarios may impact outcomes in patients with neurologic disease during the COVID-19 pandemic. For example, COVID-19 patients with acute encephalopathy have been shown to have a significantly higher mortality (Shah et al., 2020). Finally, under-utilization of healthcare during the pandemic among ischemic stroke patients has been reported in several studies (Onteddu et al., 2020), (Kansagra et al., 2020), and this may apply to other critically ill neurologic patients as well, influencing their outcomes. Neuro-critical care (NCC) units across the country have been converted to COVID-19 units and neurointensivists have had to care for COVID-19 patients, diverting care from critically ill neurologic patients. Despite above, utilization of healthcare and outcomes in critically ill neurologic patients during the COVID-19 pandemic have not been studied. We hypothesized that there has been a significant reduction in admissions among critically ill neurologic patients during the COVID-19 pandemic and sought to compare mortality in these patients between 2020 and previous years.
2. Materials and methods
2.1. Data source
Appropriate approval was obtained from the Institutional Review Board (IRB). We performed our study using de-identified patient information extracted from the TriNetX database, a global collaborative clinical research platform collecting electronic medical record (EMR) data longitudinally in real-time from a network of health care organizations (HCO) in the U.S. and some U.S. territories. Since TriNetX extracts EMR data in real-time, there is no lag between patient hospitalization and entry into the database. However, given TriNetX is de-identified, it does not provide individual patient data, permit data downloads and does not provide hospital level information, such as hospital size. At University of Arkansas for Medical Sciences the data from TriNetX is managed by Arkansas Clinical Data Repository (AR-CDR) and maintained by the Department of Biomedical Informatics.
2.2. Analytic methods
We performed a retrospective cross-sectional cohort analysis in the form of independent queries by two physicians, using browser and real-time features of TriNetX. Patients hospitalized with the 5 most common neurocritical diagnoses (Table 1) and needing critical care services were identified between January 20 (the date the first COVID-19 case was reported in the U.S.) and June 15, 2020 using ICD-10 codes (Table 1). We restricted our time-frame to January to June 2020 to evaluate trends during the first wave of the pandemic. A comparison cohort was identified in an identical manner between January 20 to June 15, 2019. Baseline demographics, co-morbidities and clinical outcomes, including intubation rates and 30-day mortality were compared between the cohorts. Outcomes were compared after propensity-score matching for co-morbidities and baseline characteristics. To ensure that reduction in number of patients was restricted not only to the ICU, but also non-ICU hospitalizations, we additionally extracted data on patients with identical ICD-10 codes that used hospital inpatient services without using critical care service codes. Similarly, to ensure that there was a true decrease in 2020 and not an expected temporal variation, we also compared the 2020 cohort to a cohort comprising hospital and critical care admissions in 2018. Statistical analysis was performed through TriNetX analytics function. Co-morbidities were compared using independent samples t-test and outcomes were compared using z-test. P-values were obtained at a significance level of <0.05.
Table 1.
Baseline characteristics of critically ill neurologic patients in 2020 vs. 2019.
| Variable |
During COVID-19 Pandemic (01/20/20 to 06/15/20) |
Before Pandemic (01/20/19 to 06/15/19) |
% Decrease in 2020 vs. 2019 | p-value | |
|---|---|---|---|---|---|
| A. Disease: (ICD-10 Code) | No. of patients | No. of COVID-19 patients (%) | No. of patients | ||
| Subarachnoid Hemorrhage: (I60) | 1165 | ≤10 | 1598 | 27.1% | <0.0001 |
| Intracerebral Hemorrhage: (I61) | 1886 | 17 (0.9%) | 2529 | 25.4% | <0.0001 |
| Ischemic Stroke: (I63) | 4556 | 77 (1.7%) | 6440 | 29.6% | <0.0001 |
| Status epilepticus (G40.901) | 817 | ≤10 | 1204 | 32.1% | <0.0001 |
| Traumatic Brain Injury: (S06) | 2737 | 25 (0.9%) | 3621 | 24.4% | <0.0001 |
| Neuromuscular emergencies (MGa G70.01+ GBSb G61.0) | 106 | ≤10 | 205 | 48.3% | <0.0001 |
| All patients | 8568d | 118 (1.4%) | 11,917d | 28.1% | <0.0001 |
| B. Demographics | 01/20/20 to 06/15/20 | 01/20/19 to 06/15/19 | |
|---|---|---|---|
| Age (yrs) | 58.8 ± 21.2 | 58.5 ± 21.2 | |
| Female sex n (%) | 3741 (44%) | 5304 (45%) | |
| White n (%) | 5675 (66%) | 8116 (68%) | |
| Black n (%) | 2019 (24%) | 2602 (22%) | |
| Asian n (%) | 154 (2%) | 186 (2%) | |
| Hispanic ethnicity n (%) |
633 (7%) |
1072 (9%) |
|
|
C. Co-morbidities |
01/20/20 to 06/15/20 |
01/20/19 to 06/15/19 |
p-value |
| Hypertension n (%) | 4305 (50.3%) | 6038 (50.7%) | 0.55 |
| Ischemic heart disease n (%) | 2182 (25.5%) | 3177 (26.7%) | 0.06 |
| Diabetes Mellitus n (%) | 2127 (24.8%) | 2961 (24.9%) | 0.97 |
| Heart Failure n (%) | 1715 (20.0%) | 2440 (20.5%) | 0.42 |
| Chronic Kidney Disease n (%) | 1565 (18.3%) | 2110 (17.7%) | 0.30 |
| Nicotine dependence n (%) | 1460 (17.0%) | 2018 (16.9%) | 0.84 |
| Atrial Fibrillation n (%) | 1441 (16.8%) | 2094 (17.6%) | 0.16 |
| Obesity n (%) | 1367 (16.0%) | 1966 (16.5%) | 0.30 |
| COPDc n (%) | 1012 (11.8%) | 1437 (12.1%) | 0.59 |
| Asthma n (%) | 694 (8.1%) | 986 (8.3%) | 0.65 |
MG: Myasthenia gravis with crisis.
GBS: Guillian Barre syndrome.
COPD: Chronic Obstructive Pulmonary Disease.
Total number of patients is lower than the sum of each individual diagnosis because there are some patients with two simultaneous diagnoses, e.g. status epilepticus in patients with intracerebral hemorrhage.
3. Results
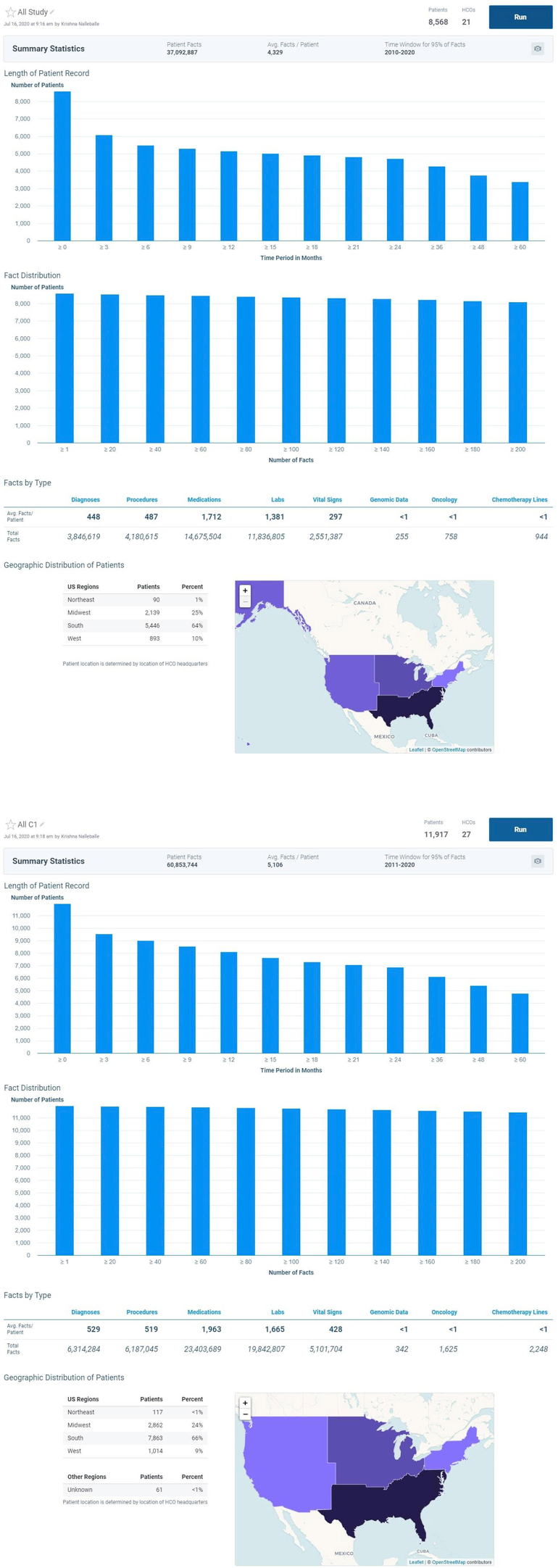
There were 8568 critically ill neurologic patients in 2020 and 11,917 in 2019 utilizing critical care services (Table 1). While the TriNetX database may contain data from outside U.S.A., majority of the HCOs in our cohorts were from the U.S. (99.7% from U.S., 0.3% outside U.S.A.) (Supplement Fig. S1). In both the cohorts, mean age was 58.5 years, 44–45% were female, 66–68% were Caucasian, 22–24% Black, 2% Asian and 7–9% Hispanic ethnicity. Demographics and comorbidities were not significantly different between 2020 and 2019 cohorts (Table 1).
The prevalence of simultaneous COVID-19 infection among critically ill neurologic patients was 1.4%, with the highest proportion in patients with AIS (1.7%), followed by TBI (0.9%) and ICH (0.9%). The number of patients with SAH, SE, NME and simultaneous COVID-19 infection was ≤10 per group, a threshold below which TriNetX cannot extract a specific number.
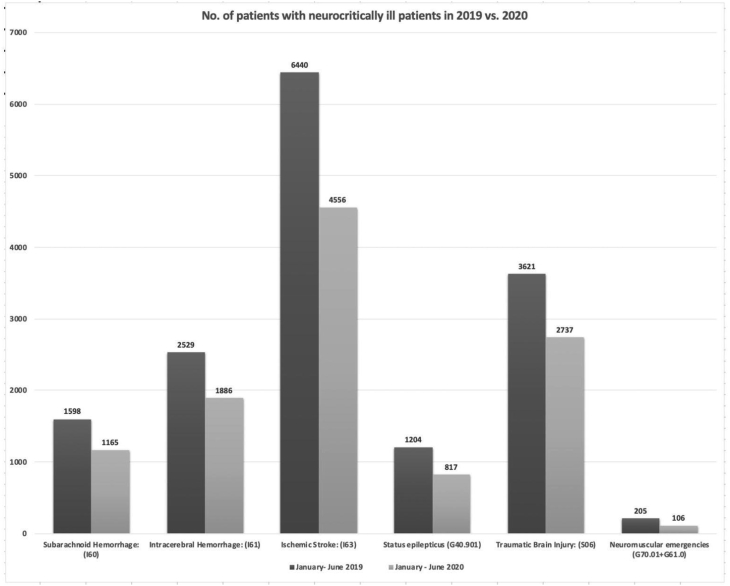
Among critically neurologic patients utilizing ICU services, there was a 28.1% reduction in 2020 when compared to 2019 (2020: 8568 vs. 2019: 11,917; p < 0.0001). There was a 27.1% reduction in admissions with subarachnoid hemorrhage (SAH), 25.4% with intracerebral hemorrhage (ICH), 29.6% with acute ischemic stroke (AIS), 32.1% with status epilepticus (SE), 24.4% with traumatic brain injury (TBI) and 48.3% with neuromuscular emergencies (NME) (Guillian-Barré syndrome and myasthenia gravis exacerbation) (p < 0.0001 for all) (Table 1, Fig. 1). When compared to 2018, there was a 34.4% reduction in 2020 among critically neurologic patients utilizing ICU services (2020: 8568 vs. 2018: 13,064; p < 0.0001).
Fig. 1.
Number of neurocritically ill patients in 2019 versus 2020
This figure shows the number of admissions with each neurocritical care diagnosis during 2019 versus 2020.
Among patients with neurocritical diagnoses admitted to the hospital but not utilizing ICU services, there was 26.6% decrease in 2020 compared to 2019 and a 24.7% decrease compared to 2018 (2020: 31,665 vs. 2019: 43,151 vs. 2018: 42,037; p < 0.0001).
With respect to outcomes, there was no significant difference in 30-day mortality (12.2 vs. 12.4%, p = 0.7). or intubation rates (7.8% vs. 8.4%, p = 0.14) among critically ill neurologic patients utilizing ICU services in 2020 versus 2019. There was no statistically significant difference in mortality across individual diagnoses as well (Table 2). Similarly, there was no difference in overall mortality when compared to 2018 (12.2% vs. 12.6%, p = 0.62). However, among hospitalized patients not receiving ICU care, there was a 1% increase in mortality in 2020 compared to 2019 and a 0.8% increase compared to 2018 and while numerically small, this difference was statistically significant (2020: 3.9% vs. 2019: 2.9% vs. 2018: 3.1%; p ≤ 0.0001).
Table 2.
Outcomes in critically ill neurologic patients during COVID-19 pandemic in 2020 versus the same time frame in 2019.
| Disease (ICD-10 code) | COVID-19 Pandemic (1/20/2020-6/15/2020) | Before Pandemic (01/20/19-06/15/19) | P-Value |
|---|---|---|---|
| A. Intubation and mechanical ventilation | |||
| Subarachnoid Hemorrhage: (I60) | 103 (8.8%) | 156 (9.8%) | 0.40 |
| Intracerebral Hemorrhage: (I61) | 171 (9.1%) | 272 (10.8%) | 0.07 |
| Ischemic Stroke: (I63) | 342 (7.5%) | 549 (8.5%) | 0.05 |
| Status epilepticus: (G40.901) | 74 (9.1%) | 140 (11.6%) | 0.07 |
| Traumatic Brain Injury: (S06) | 202 (7.4%) | 253 (7.0%) | 0.55 |
| Neuromuscular emergencies (MGa G70.01+ GBSb G61.0) | 13 (12.3%) | 30 (14.6%) | 0.60 |
| All patients | 668 (7.8%) | 998 (8.4%) | 0.14 |
| B. 30-day Mortality | |||
| Subarachnoid Hemorrhage: (I60) | 185 (15.9%) | 235 (14.7%) | 0.40 |
| Intracerebral Hemorrhage: (I61) | 356 (18.9%) | 473 (18.7%) | 0.90 |
| Ischemic Stroke: (I63) | 556 (12.2%) | 819 (12.7%) | 0.42 |
| Status epilepticus (G40.901) | 95 (11.6%) | 155 (12.9%) | 0.40 |
| Traumatic Brain Injury: (S06) | 330 (12.1%) | 403 (11.1%) | 0.25 |
| Neuromuscular emergencies (MGa G70.01+ GBSb G61.0) | 10 (9.4%) | 12 (5.9%) | 0.24 |
| All patients | 1048 (12.2%) | 1479 (12.4%) | 0.70 |
MG: Myasthenia Gravis; bGBS: Guillian Barre syndrome.
4. Discussion
Reduction in hospitalizations among AIS patients during the COVID-19 pandemic has been reported previously (Onteddu et al., 2020), (Zhao et al., 2020). We suspected a similar pattern among other critically ill neurologic and neurosurgical patients, however, this has not been studied previously. Our study showed a 28 to 35% reduction in utilization of critical care services among patients with acute neurologic/neurosurgical emergencies in U.S. hospitals in 2020 compared to previous years (2019 and 2018). Similarly, there was a 25–27% reduction in non-ICU hospitalizations among patient with neurologic/neurosurgical emergencies. The reason for this reduction remains unclear, but could be multifactorial. There may have been apprehension among patients due to fear of contracting COVID-19 infection in the hospitals, even though there are no reports of in-hospital provider-to-patient transmission so far. This hypothesis needs to be confirmed and corroborated with first responder data, which was not available in TriNetX. Additionally, there may be limited ICU bed availability with diversion of patients to non-ICU floors, an expected outcome of a pandemic. However, we found a reduction across all hospitalizations among patients with these diagnoses.
While several studies have described neurologic manifestations in COVID-19 infection (Nalleballe et al., 2020), the prevalence of simultaneous COVID-19 in neurologic/neurosurgical patients has not been described. We found that simultaneous COVID-19 infection in critically ill neurologic/neurosurgical patients was low (1.4%). This low prevalence could be due to due to under-reporting, given that testing may not have been performed in these patients as they did not meet traditional COVID-19 testing criteria. Additionally, lower prevalence may be due to significant regional heterogeneity across the U.S., given our cohort of patients was not balanced across all U.S. regions (Supplement Fig. S1).
Despite a reduction in hospitalizations and utilization of critical care services, we did not find a significant increase in mortality after onset of COVID-19 pandemic among critically ill neurologic patients that needed ICU care. This may indicate that ICU care has likely not been impacted in most centers. However, among patients hospitalized with these diagnoses but not receiving critical care, there was small increase in mortality during the pandemic compared to previous years. The reasons for this trend need further exploration but may due to reduced ICU bed availability leading to patients, that would ordinarily have been cared for in the ICU, being managed in non-critical care settings and by providers that lack specific expertise. Critically ill neurologic patients have been shown to have better outcomes when managed by specially trained neurocritical care personnel in dedicated neurocritical care units (Moheet et al., 2020) and during the pandemic this care may not have been available or patients may have been admitted to medical ICUs due to simultaneous COVID-19 infections. These hypotheses need further study as this data was not available in TriNetX. Additionally, patients with underlying chronic neurologic disorders such as myasthenia gravis, epilepsy, may have been more compliant with medications and outpatient follow-up due to fear of needing inpatient services during the pandemic which may have had led to reduced hospitalizations. Similarly, prevalence of trauma may have declined due to lockdown during the first wave of the pandemic. These hypotheses need further evaluation as we were not able to delineate this information through TriNetX. In addition, the true mortality could be significantly higher as we could not capture pre-hospital deaths, which may have occurred prior to presentation. This needs to be corroborated with first-responder data. Finally, as the pandemic continues to evolve, there may be a delayed collateral impact on critically ill neurologic patients. Guidelines to ensure adequate care for NCC patients during the pandemic (Moheet et al., 2020) should be adopted widely.
There are several limitations in our study, including its retrospective nature, reporting bias associated with using ICD-10 codes and inability to balance the severity of illness in both the cohorts. Additionally our cohorts do not account for regional heterogeneity in the COVID-19 pandemic and heterogeneity in care based on hospital size and level of care. As described above, we could not confirm several of our hypotheses for reduction in hospitalizations and critical care utilization among this patient population, due to limitations in the database. Finally, with the pandemic still ongoing, the true collateral impact on outcomes may not be evident till the pandemic has concluded. Lastly, we were unable delineate functional outcomes which are important outcome measures in neurologic patients.
5. Conclusion
There has been a significant reduction in hospitalizations and utilization of critical care services among critically ill neurologic/neurosurgical patients during onset the COVID-19 pandemic in the U.S., without significant increase in mortality. Prospective studies are needed to confirm our findings, determine the true extent of collateral impact of COVID-19 on care of critically ill neurologic/neurosurgical patients and to determine factors contributing to reduction in healthcare utilization by this patient population.
Financial disclosures
Vishank Arun Shah: None; Krishna Nalleballe: None; Sanjeeva Reddy Onteddu: None.
Details page
-
1.
I confirm that the manuscript complies with instructions to authors.
-
2.
I confirm that authorship requirements have been met and the final manuscript was approved by all authors.
-
3.
I confirm that this manuscript has not been published elsewhere and is not under consideration by another journal.
-
4.
I confirm adherence to ethical guidelines. Appropriate IRB approval was obtained prior to study and given data was de-identified study was provided an exempt status by local IRB.
-
5.
The study required no funding.
Credit author statement
Vishank Arun Shah: Conceptualization, Methodology, Data curation, Writing-Original draft preparation. Krishna Nalleballe: Methodology, Data curation, Statistical analysis, Software, Writing- Reviewing and Editing. Sanjeeva Onteddu: Data curation, Statistical analysis, Software, Writing- Reviewing and Editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbih.2021.100207.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
figs1.
References
- Becker K.J., Baxter A.B., Cohen W.A. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–772. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M., Bui R., Zanella A., Grasselli G., Lagioia M., Protti A., Cecconi M. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of covid-19. N. Engl. J. Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of covid-19 on stroke evaluation in the United States. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moheet A.M., Shapshak A.H., Brissie M.A. Neurocritical care resource utilization in pandemics: a statement by the neurocritical care society. Neurocritical Care. 2020 doi: 10.1007/s12028-020-01001-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalleballe K., Reddy Onteddu S., Sharma R. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.06.020. S0889-1591(20)31008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onteddu S.R., Nalleballe K.A., Department of Neurology, University of Arkansas for Medical Sciences, Sharma R., Brown A.T. Underutilization of health care for strokes during the COVID-19 outbreak. Int. J. Stroke. 2020 doi: 10.1177/1747493020934362. 1747493020934362. [DOI] [PubMed] [Google Scholar]
- Shah V.A., Nalleballe K., Zaghlouleh E., Onteddu S. Acute encephalopathy is associated with worse outcomes in COVID-19 patients. Brain Behav Immun Health. 2020:100136. doi: 10.1016/j.bbih.2020.100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Li H., Kung D., Fisher M., Shen Y., Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]