Abstract
Introduction
The COVID-19 pandemic has led to closures of non-essential businesses and buildings. The impact of such closures on automated external defibrillator (AED) accessibility compared to changes in foot traffic levels is unknown.
Methods
We identified all publicly available online AED registries in Canada last updated May 1, 2019 or later. We mapped AED locations to location types and classified each location type as completely inaccessible, partially inaccessible, or unaffected based on government-issued closure orders as of May 1, 2020. Using location and mobility data from Google’s COVID-19 Community Mobility Reports, we identified the change in foot traffic levels between February 15–May 1, 2020 (excluding April 10–12) compared to the baseline of January 3–February 1, 2020, and determined the discrepancy between foot traffic levels and AED accessibility.
Results
We identified four provincial and two municipal AED registries containing a total of 5848 AEDs. Of those, we estimated that 69.9% were completely inaccessible, 18.8% were partially inaccessible, and 11.3% were unaffected. Parks, retail and recreation locations, and workplaces experienced the greatest reduction in AED accessibility. The greatest discrepancies between foot traffic levels and AED accessibility occurred in parks, retail and recreation locations, and transit stations.
Conclusion
A majority of AEDs became inaccessible during the COVID-19 pandemic due to government-mandated closures. In a substantial number of locations across Canada, the reduction in AED accessibility was far greater than the reduction in foot traffic.
Keywords: Public access defibrillator, COVID-19, Accessibility
Introduction
The COVID-19 pandemic led governments around the world to order mandatory closures of non-essential businesses and services in an effort to contain the spread of the disease. Such locations are often home to publicly available automated external defibrillators (AEDs), an effective intervention for out-of-hospital cardiac arrest (OHCA).1, 2, 3
The accessibility of AEDs is generally affected by the business hours of the AED’s host location, and previous literature has shown that many AEDs have been rendered inaccessible during evenings and weekends.4, 5, 6, 7 We sought to determine the impact that government-mandated closures had on AED accessibility in Canada, and the relative change in AED accessibility compared to changes in foot traffic levels after the first wave of closures were implemented early in the COVID-19 pandemic.
Methods
We identified all publicly available online automated external defibrillator (AED) registries in Canada that were updated May 1, 2019 or later. Each AED entry was manually screened by one of two authors and classified to a location type using address and text notes in the registry, as well as online information found from web searches. We used location type definitions based on those identified in existing literature,5, 6, 8 and adjusted the definitions to combine duplicate location types or to differentiate between similar location types with different closure status during the lockdown. For example, medical offices were separated into “Essential Medical” and “Non-Essential Medical” location types to differentiate between medical services that remained open during the closures (e.g., hospitals, walk-in clinics) and services that were closed (e.g., immunization clinics, dentist offices). All location information used in the study was available in the publicly available AED registries identified.
Once the regions included in the study were finalized, the authors searched for news releases published between January 1–May 1, 2020 by provincial and municipal governments of each region to determine the closure status of each location type. All news releases regarding COVID-19 or “novel coronavirus”, as well as all supplementary webpages referring to location closures and changes to civic services, were reviewed in full by authors KHBL and RA, and webpages containing relevant information were analyzed by both authors. Both authors cross-referenced the locations listed in each source of closure information with the location types determined from the AED registries to determine the closure status of each AED location type. If a location type was not listed as essential by any of the government news releases, those AEDs were deemed completely inaccessible. If a location type was listed as essential by some but not all of the government news releases, or if the location type had operating constraints such as capacity or opening hour limits, those AEDs were deemed partially inaccessible. AEDs in all other location types were deemed unaffected.
We obtained data on foot traffic levels from Google’s COVID-19 Community Mobility Reports.9 The reports were developed to aid understanding of movement trends during the COVID-19 pandemic and utilize aggregated and anonymized Google Maps user location data to determine changes in daily foot traffic levels, measured by the number of person-hours spent in each of six location categories: grocery and pharmacy, parks, residential, retail and recreation, transit stations, and workplaces. The changes in foot traffic provided by Google were computed relative to the same days of the week during a baseline period of January 3–February 1, 2020. We obtained the percent change in daily foot traffic for each location category relative to the median foot traffic level during the study period of February 15–May 1, 2020. We excluded April 10–12 because it was the Easter holiday weekend across Canada. Removal of holidays from foot traffic analysis was recommended in the Google documentation.10 We then computed the median change in foot traffic levels over the study period for each of the six Google locations categories. AED location types were mapped to these six categories.
To assess mismatch between AED accessibility and foot traffic levels, we compared the percent of AEDs that became completely inaccessible with the median percent change in foot traffic for each location category. This comparison considers the total decrease in AED accessibility against the change in foot traffic levels on a “typical day” during the study period.
Results
We identified three provincial (British Columbia, Alberta, Nova Scotia) and two municipal (Mississauga and Toronto in Ontario) online AED registries. Links to the registries and closure announcements by each government are provided in Table 1 . These regions cover 13.1 million people (37.2% of national population). The registries listed 5848 AEDs in total, which we mapped to 21 location types (Table 2 ), and then to the six location categories from Google’s COVID-19 Community Mobility Reports. Workplaces consisted of ten location types such as schools, non-essential and essential medical facilities, banks, and government offices. Retail and recreational locations consisted of seven location types such as sports facilities and community centers. Parks, residences, transit stations, and grocery/pharmacy locations consisted of one location type each.
Table 1.
Data sources for AED locations and closure status information in each region.
| Region | AED registry | Source of closure status information | Closure information |
|---|---|---|---|
| Alberta | Alberta Public Access to Defibrillation Program20 | Province of Alberta | Government office closures21 |
| Province of Alberta | List of restricted and non-restricted services22 | ||
| British Columbia | BC Public Access to Defibrillation Program23 | Province of British Columbia | Government services affected by COVID-1924 |
| Province of British Columbia | List of COVID-19 essential services25 | ||
| Nova Scotia | EHS Provincial AED Registry26 | Province of Nova Scotia | Closures, cancellations and service changes27 |
| Province of Nova Scotia | COVID-19: what it means for Nova Scotians28 | ||
| Mississauga | Automated External Defibrillator – City Facilities – City of Mississauga29 | Province of Ontario | List of essential workplaces30 |
| Region of Peel | Services and facilities temporarily affected in Peel31 | ||
| City of Mississauga | Facility closures and reopenings32 | ||
| Toronto | Automatic External Defibrillators (AED) Locations – Open Data Toronto33 | Province of Ontario | List of essential workplaces30 |
| City of Toronto | COVID-19: changes to city services34 |
Table 2.
Mapping from specific locations to location types as well as location categories obtained from Google.
| Location category and type | Example Locations |
|---|---|
| Grocery and Pharmacy | Grocery stores, markets, convenience stores (including those at gas stations), pharmacies, drugstores |
| Parks | National parks, provincial parks, municipal parks, park amenities, park buildings |
| Residential | Homes, apartment complexes, condominiums |
| Retail and Recreation | |
| Arenas/Venues | Multi-purpose arenas, convention halls, concert venues |
| Attractions | Museums, art centers, science centers, casinos |
| Community Centers | Community centers, public libraries |
| Food and Beverage | Restaurants |
| Outdoor Recreational Facilities | Golf courses, marinas, beaches |
| Places of Worship | Churches, temples, mosques, synagogues |
| Recreation/Sports Facilities | Recreation centers, sports fields, fitness centers, ice rinks, aquatic centers |
| Transit Stations | Transit stations, transit maintenance yards |
| Workplaces | |
| Accommodation | Hotels, motels, bed & breakfasts |
| Associations/NGOs | Associations, union offices, non-profit organizations |
| Banks | Banks, credit unions |
| Educational Institutions | Elementary/secondary schools, colleges, universities, private schools |
| Essential Medical | Hospitals, healthcare centers, walk-in clinics |
| Government Offices | Federal/provincial/municipal offices, city/town halls |
| Municipal Services | Power/water/waste management sites, maintenance vehicle yards |
| Non-Essential Medical | Dental offices, physiotherapy offices, immunization clinics |
| Private Businesses | For-profit businesses, office towers, car dealerships |
| Social Services | Child services, food banks, homeless shelters |
Across all regions, we estimated that 69.9% of AEDs were completely inaccessible, 18.8% were partially inaccessible, and 11.3% were unaffected. Table 3 shows the breakdown of AEDs by location type and accessibility status. All AEDs in parks were estimated to be completely inaccessible. Within retail and recreational locations, we estimated that 99.0% of AEDs became completely inaccessible and 1.0% became partially inaccessible. Within workplaces, we estimated that 66.7% of AEDs became completely inaccessible, 25.0% became partially inaccessible, and 8.3% were unaffected. We estimated that all AEDs in grocery stores and pharmacies became partially inaccessible, and that all AEDs in transit stations and residences were unaffected in their accessibility.
Table 3.
AED accessibility and traffic level changes during the first wave of the COVID-19 pandemic in Canada.
| AEDs |
Change in Traffic Levels, % | ||||
|---|---|---|---|---|---|
| Location category and type | Total, No. | Unaffected, No. (%) | Partially Inaccessible, No. (%) | Completely Inaccessible, No. (%) | |
| Grocery and Pharmacy | 173 | 0 (0.0) | 173 (100.0) | 0 (0.0) | −18.0 |
| Parks | 141 | 0 (0.0) | 0 (0.0) | 141 (100.0) | −10.5 |
| Residential | 85 | 85 (100.0) | 0 (0.0) | 0 (0.0) | +20.0 |
| Retail and Recreation | 1539 | 0 (0.0) | 16 (1.0) | 1523 (99.0) | −48.0 |
| Arenas/Venues | 186 | 0 | 0 | 186 | |
| Attractions | 67 | 0 | 0 | 67 | |
| Community Centers | 424 | 0 | 0 | 424 | |
| Food and Beverage | 16 | 0 | 16 | 0 | |
| Places of Worship | 77 | 0 | 0 | 77 | |
| Outdoor Recreation Facilities | 62 | 0 | 0 | 62 | |
| Recreation/Sport Facilities | 707 | 0 | 0 | 707 | |
| Transit Stations | 277 | 277 (100.0) | 0 (0.0) | 0 (0.0) | −63.0 |
| Workplaces | 3633 | 300 (8.3) | 909 (25.0) | 2424 (66.7) | −52.5 |
| Accommodation | 27 | 0 | 27 | 0 | |
| Associations/ NGOs | 91 | 0 | 0 | 91 | |
| Banks | 78 | 0 | 78 | 0 | |
| Educational Institutions | 1258 | 0 | 0 | 1258 | |
| Essential Medical Facilities | 300 | 300 | 0 | 0 | |
| Government Offices | 488 | 0 | 0 | 488 | |
| Municipal Services | 618 | 0 | 618 | 0 | |
| Non-Essential Medical Facilities | 81 | 0 | 81 | 0 | |
| Private Businesses | 587 | 0 | 0 | 587 | |
| Social Services | 105 | 0 | 105 | 0 | |
| Total | 5848 | 662 (11.3) | 1098 (18.8) | 4088 (69.9) | N/A |
Mobility data from the four provinces indicated that the largest decrease in foot traffic occurred in transit stations (−63.0%), followed by workplaces (−52.5%), retail and recreation locations (−48.0%), grocery and pharmacy locations (−18.0%), and parks (−10.5%). Residential areas were the only category to experience an increase (+20.0%) in foot traffic.
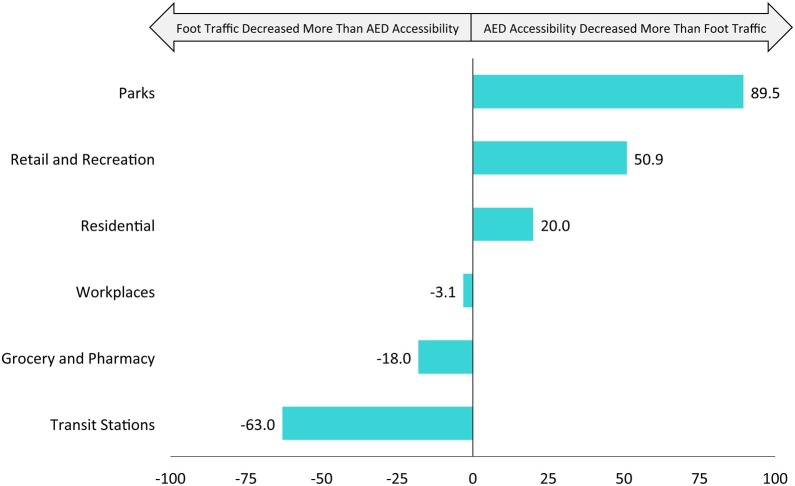
The largest discrepancies between estimated AED accessibility and foot traffic (Fig. 1 ) occurred in parks (100% completely inaccessible vs. 10.5% traffic decrease), retail and recreation locations (99.0% completely inaccessible vs. 48.0% traffic decrease), and transit stations (100% unaffected vs. 63.0% traffic decrease).
Fig. 1.
Proportion of completely inaccessible AEDs vs. percent decrease in foot traffic for each location category.
Discussion
While AEDs are effective in increasing survival from out-of-hospital cardiac arrest (OHCA), our findings suggest that they were largely inaccessible during the first wave of the pandemic. During non-pandemic times, most AEDs are hidden from public view or are not accessible to the public outside of a building’s hours of operation, which may contribute to low rates of bystander AED usage.4, 5, 6, 7, 8, 11, 12 Coupled with the fact that studies reported increased OHCA incidence during COVID-19,13, 14 pandemic-driven closures likely exacerbated the gap between the need for AEDs and their availability for resuscitative efforts. Consideration must be given to the effect of building closures on AED accessibility for subsequent pandemic waves, especially in areas with high risk of OHCA.
Although government-mandated closures rendered certain services unavailable, it should be noted that they do not necessarily close off the location type from pedestrian traffic entirely. The clearest example of this is phenomenon is parks. During the lockdown, people could still walk around in parks. However, park buildings and community centers in the park would have been closed, preventing the public from accessing AEDs located there. At the other end of the spectrum, transit stations remained open, but foot traffic decreased substantially, since fewer people were travelling to work or for other purposes, so the mismatch is opposite from the parks mismatch.
Static AED placement is generally not robust to large-scale disruptions, since those AEDs are reliant on accessibility of the host location. Mitigating the impact of accessibility disruptions can be achieved by systematically placing AEDs in 24/7-accessible locations or employing innovative methods to facilitate AED delivery, such as smartphone-enabled lay responders or drones.6, 15, 16, 17, 18, 19
This study has several limitations. We used foot traffic as a proxy for OHCA risk. All locations of a location type were assumed to have identical AED accessibility. It is believed that most AEDs are unregistered, so true accessibility during COVID-19 is unknown. Finally, Google’s mobility data likely underestimates traffic decreases since foot traffic levels in winter, which is their baseline, are likely lower than in spring.
Conclusion
We estimated that a majority of AEDs became inaccessible during the first wave of the COVID-19 pandemic due to government-mandated closures. In a substantial number of locations across Canada, the reduction in AED accessibility was far greater than the reduction in foot traffic.
Sources of funding
None.
Conflict of interest statement
The authors declare no conflicts of interest.
CRediT authorship contribution statement
K.H. Benjamin Leung: Methodology, Data curation, Investigation, Writing - original draft. Rejuana Alam: Data curation, Investigation, Visualization, Validation. Steven C. Brooks: Conceptualization, Writing - review & editing. Timothy C.Y. Chan: Conceptualization, Methodology, Writing - review & editing, Supervision.
Acknowledgements
None.
References
- 1.The Public Access Defibrillation Trial Investigators Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 2.Weisfeldt M.L., Sitlani C.M., Ornato J.P., et al. Survival after application of automatic external defibrillators before arrival of the emergency medical system. Evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blom M.T., Beesems S.G., Homma P.C.M., et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. doi: 10.1161/CIRCULATIONAHA.114.010905. [DOI] [PubMed] [Google Scholar]
- 4.Hansen C.M., Wissenberg M., Weeke P., et al. Automated external defibrillators inaccessible to more than half of nearby cardiac arrests in public locations during evening, nighttime, and weekends. Circulation. 2013;128:2224–2231. doi: 10.1161/CIRCULATIONAHA.113.003066. [DOI] [PubMed] [Google Scholar]
- 5.Sun C.L.F., Demirtas D., Brooks S.C., Morrison L.J., Chan T.C.Y. Overcoming spatial and temporal barriers to public access defibrillators via optimization. J Am Coll Cardiol. 2016;68:836–845. doi: 10.1016/j.jacc.2016.03.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun C.L.F., Brooks S.C., Morrison L.J., Chan T.C.Y. Ranking businesses and municipal locations by spatiotemporal cardiac arrest risk to guide public defibrillator placement. Circulation. 2017;135:1104–1119. doi: 10.1161/CIRCULATIONAHA.116.025349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deakin C.D., Anfield S., Hodgetts G.A. Underutilisation of public access defibrillation is related to retrieval distance and time-dependent availability. Heart. 2018;104:1339–1343. doi: 10.1136/heartjnl-2018-312998. [DOI] [PubMed] [Google Scholar]
- 8.Karlsson L., Malta Hansen C., Wissenberg M., et al. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: a registry-based study. Resuscitation. 2019;136:30–37. doi: 10.1016/j.resuscitation.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Google . 2020. COVID-19 community mobility reports.https://www.google.com/covid19/mobility/ [Cited 2020 May 2]; Available from: [Google Scholar]
- 10.Google . 2020. Community mobility reports help: understand the data.https://support.google.com/covid19-mobility/answer/9825414?hl=en&ref_topic=9822927 [Cited 2020 October 28]; Available from: [Google Scholar]
- 11.Huig I.C., Boonstra L., Gerritsen P.C., Hoeks S.E. The availability, condition and employability of automated external defibrillators in large city centres in the Netherlands. Resuscitation. 2014;85:1324–1329. doi: 10.1016/j.resuscitation.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 12.Daya M.R., Schmicker R.H., Zive D.M., et al. Out-of-hospital cardiac arrest survival improving over time: results from the resuscitation outcomes consortium (ROC) Resuscitation. 2015;91:108–115. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ringh M., Rosenqvist M., Hollenberg J., et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 16.Berglund E., Claesson A., Nordberg P., et al. A smartphone application for dispatch of lay responders to out-of-hospital cardiac arrests. Resuscitation. 2018;126:160–165. doi: 10.1016/j.resuscitation.2018.01.039. [DOI] [PubMed] [Google Scholar]
- 17.Boutilier J.J., Brooks S.C., Janmohamed A., et al. Optimizing a drone network to deliver automated external defibrillators. Circulation. 2017;135:2454–2465. doi: 10.1161/CIRCULATIONAHA.116.026318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Claesson A., Bäckman A., Ringh R.N.M., et al. Time to delivery of an automated external defibrillator using a drone for simulated out-of-hospital cardiac arrests vs emergency medical services. J Am Med Assoc. 2017;317:2332–2334. doi: 10.1001/jama.2017.3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheskes S., McLeod S.L., Nolan M., et al. Improving access to automated external defibrillators in rural and remote settings: a drone delivery feasibility Study. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.016687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alberta Health Services . 2020. AED map & site listing.https://secure.heart-safe.ca/theme/common/page.cfm?i=11440 [Cited 2020 May 2]; Available from: [Google Scholar]
- 21.Government of Alberta . 2020. COVID-19: temporary office closures.https://www.alberta.ca/covid-19-temporary-office-closures.aspx [Cited 2020 May 10]; Available from: [Google Scholar]
- 22.Government of Alberta . 2020. Restricted and Non-Restricted Services. [Cited 2020 May 10]; Available from: https://www.alberta.ca/restricted-and-non-restricted-services.aspx. [Google Scholar]
- 23.British Columbia Emergency Health Services . 2020. BC — public access to defibrillation — find an AED.https://www.bcpadprogram.ca/admin/contentx/default.cfm?PageId=11521 [Cited 2020 May 2]; Available from: [Google Scholar]
- 24.Government of British Columbia . 2020. Government services affected by COVID-19.https://www2.gov.bc.ca/gov/content/safety/emergency-preparedness-response-recovery/covid-19-provincial-support/covid-19-services-changes [Cited 2020 May 7]; Available from: [Google Scholar]
- 25.Government of British Columbia . 2020. List of COVID-19 essential services.https://www2.gov.bc.ca/gov/content/safety/emergency-preparedness-response-recovery/covid-19-provincial-support/essential-services-covid-19 [Cited 2020 May 8]; Available from: [Google Scholar]
- 26.Province of Nova Scotia . 2020. EHS Nova Scotia volunteer AED map.https://nsgi.novascotia.ca/EHS-NS-Volunteer-AED-Map/ [Cited 2020 May 2]; Available from: [Google Scholar]
- 27.Province of Nova Scotia . 2020. Closures, cancellations and service changes.https://novascotia.ca/closures-cancellations-and-service-changes/ [Cited 2020 May 9]; Available from: [Google Scholar]
- 28.Province of Nova Scotia . 2020. COVID-19: what it means for Nova Scotians.https://novascotia.ca/coronavirus/what-it-means-for-nova-scotians/ [Cited 2020 May 9]; Available from: [Google Scholar]
- 29.City of Mississauga . 2019. Automated external defibrillator — city facilities. Mississauga Data.https://data.mississauga.ca/datasets/caa78d0c6c63459abf294df84542f817_0 [Cited 2020 May 2]; Available from: [Google Scholar]
- 30.Government of Ontario . 2020. List of essential workplaces.https://www.ontario.ca/page/list-essential-workplaces [Cited 2020 May 8]; Available from: [Google Scholar]
- 31.Region of Peel . 2020. Services and facilities temporarily affected in Peel.https://www.peelregion.ca/coronavirus/affected-services.asp [Cited 2020 May 8]; Available from: [Google Scholar]
- 32.City of Mississauga . 2020. Facility closures and reopenings.https://web.mississauga.ca/city-of-mississauga-news/covid-19/facility-closures-and-reopenings/ [Cited 2020 May 6]; Available from: [Google Scholar]
- 33.City of Toronto . 2020. Automatic external defibrillators (AED) locations. City Toronto Open Data Portal.https://open.toronto.ca/dataset/automatic-external-defibrillators-aed-locations/ [Cited 2020 May 2]; Available from: [Google Scholar]
- 34.City of Toronto . 2020. COVID-19: changes to city services.https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/affected-city-services/ [Cited 2020 May 6]; Available from: [Google Scholar]