Abstract
Introduction
As the Coronavirus Disease 2019 (COVID-19) cases in Kenya begin to rise, the number of severe and critical COVID-19 patients has the potential to quickly overload the local healthcare system beyond its capacity to treat people.
Objective
The purpose of this study was to gather information about the ability of hospitals in Kenya to provide emergency and critical care services and to identify priority actions for use by policymakers and other stakeholders as a roadmap toward strengthening the COVID-19 response in the country.
Methods
This was a comprehensive review of the published and grey literature on emergency and critical care services in Kenya published in the last three years through April 2020. Screening of articles was conducted independently by the authors and the final decision for inclusion was made collaboratively. A total of 15 papers and documents were included in the review.
Key recommendations
There is an urgent need to strengthen prehospital emergency care in Kenya by establishing a single toll-free ambulance access number and an integrated public Emergency Medical Services (EMS) system to respond to severe and critical COVID-19 patients in the community and other emergency cases. Functional 24-h emergency centres (ECs) need to be established in all the level 4, 5 and 6 hospitals in the country to ensure these patients receive immediate lifesaving emergency care when they arrive at the hospitals. The ECs should be equipped with pulse oximeters and functioning oxygen systems and have the necessary resources and skills to perform endotracheal intubation to manage COVID-19-induced respiratory distress and hypoxia. Additional intensive care unit (ICU) beds and ventilators are also needed to ensure continuity of care for the critically ill patients seen in the EC. Appropriate practical interventions should be instituted to limit the spread of COVID-19 to healthcare personnel and other patients within the healthcare system. Further research with individual facility levels of assessment around infrastructure and service provision is necessary to more narrowly define areas with significant shortfalls in emergency and critical care services as the number of COVID-19 cases in the country increase.
Keywords: Emergency treatment, Critical care, Prehospital emergency care, SARS coronavirus, Oxygen, Triage
African relevance
-
•
Key to managing COVID-19 patients in Africa is the ability of hospitals to provide emergency and critical care services
-
•
The gaps identified in this review could inform the strengthening of emergency and critical care systems in other countries
-
•
The recommendations can also improve emergency and critical care services to other non-pandemic patients
Introduction
In epidemiology, the idea of slowing a virus' spread so that fewer people need to seek treatment at any given time is known as “flattening the curve” [1]. The “curve” refers to the projected number of people who will contract the virus over a period of time. The faster the infection curve rises, the quicker the local health care system gets overloaded beyond its capacity to treat people. As the number of Coronavirus Disease 2019 (COVID-19) cases in Kenya begins to rise, the number of severe and critical COVID-19 patients has the potential to quickly overload the local healthcare system [2]. A baseline review of the system's ability to care for these patients is important to identify the priority actions for increasing surge capacity and the resources needed to care for the sickest patients with COVID-19.
In a cohort of COVID-19 patients in China, 15% of the cases were considered severe, and 5% were considered critical [3]. In Italy, 24.9% and 5.0% were considered severe and critical respectively [4]. While both countries are highly ranked as having well-developed public health care systems, the burden of these patients has been overwhelming due to the insufficiency in the provision of medical supplies and equipment leading to significant morbidity and mortality in both countries [5]. Some of the challenges in African health systems include poor coordination, management and leadership, inadequate human resources, and inadequate budget allocations for health [6]. A recent study conducted in 2018 evaluated the calibre of country pandemic preparedness plans within the WHO African region and revealed preparedness in South Africa was high at 79%, while Kenya managed about 60% [6]. Kenya reported its first case on the 13th of March 2020. Since then, the number of confirmed cases have been steadily increasing and modelling estimates predict that about 952,000 people in Kenya could end up being infected with COVID-19 and develop symptoms (symptomatic infected) [7].
The purpose of this study was thus to gather information about the ability of hospitals in Kenya to provide emergency and critical care services and to identify priority actions for use by policymakers and other stakeholders as a roadmap toward strengthening the COVID-19 response in the country.
Methods
The health care system in Kenya
The Republic of Kenya, located in eastern Africa, consists of 47 semiautonomous counties [8]. It has a population of 47.6 million people, with nearly 68.9% of the population living in rural areas [9]. Based on Ministry of Health data, there are 6608 (60.6%) public and 4293 (39.4%) private health care facilities in Kenya [10]. Of the public health care facilities, 5175 (78.3%) facilities are managed by county governments, 1004 (15.2%) by faith-based organisations (FBOs), 327 (5.0%) by non-governmental organisations (NGOs), and 100 (1.5%) are listed as other public institutions e.g. military hospitals.
Kenya's healthcare system is structured in a hierarchical manner beginning with primary healthcare, with the lowest unit being the community (level 1) and primary health care facilities (levels 2 and 3) consisting of dispensaries and health centres, graduating to primary referral facilities/hospitals (level 4) then secondary referral facilities (level 5) and finally tertiary referral facilities (level 6) [11].
Search strategy and selection criteria
This was a comprehensive review of the published literature on the emergency and critical care services within the Kenyan healthcare system. Controlled vocabulary terms and synonymous free text words and phrases that capture the concepts of emergency care (emergency medicine, acute care, emergency services, emergency department), and critical care (intensive care unit (ICU), high dependency unit (HDU)), were used. PubMed and other electronic resources that curate English-language medical literature (MEDLINE, Embase, Scopus, Web of Science Core Collections, Africa-Wide Information and CINAHL) were searched for articles on emergency and critical care services in Kenya published from April 2017 to April 2020. In addition, a search of the grey literature was performed of reports from both the Ministry of Health and other Non-Governmental Organisations, Google, Custom Search Engines, and Greylit.org. In the second phase, partial bibliographies compiled by earlier researchers were used and articles cited in the search results, that met the search criteria were included. Screening of articles was conducted independently by the authors and the final decision for inclusion was made collaboratively.
A summary of the papers and documents included in the review is shown in Table 1.
Table 1.
Summary of papers and documents included in the review.
| First author name/year | Document type | Reference | Main outcome/focus of paper | Data source |
|---|---|---|---|---|
| Sambala EZ, 2018 | Journal article | BMC Infect Dis 2018;18:567 | Healthcare systems | National survey |
| Brand SPC, 2020 | Journal article | medRxiv 2020.04.09.20059865 | Healthcare systems | National survey |
| Ministry of Health, 2020 | Public report | Kenya Master Health Facility List, Ministry of Health 2020. | Healthcare systems | National survey |
| Ministry of Health, 2020 | Public report | The Kenya Harmonized Health Facility Assessment (KHFA) 2018–2019. Ministry of Health 2020. | Healthcare systems | National survey |
| Otieno B, 2020 | Newspaper article | Man dies after refusing to board Covid-19 ambulance. The Star 2020. | Emergency care | Local news |
| Lampi M, 2018 | Journal article | BMC Emerg Med 2018;18(1):49 | Emergency care | Hospital data |
| Barasa E, 2020 | Journal article | PLoS ONE 15(7): e0236308 | Critical care | National survey |
| Nicholson B, 2017 | Jouranl article | Afr J Emerg Med. 2017 Dec;7(4):157–159 | Emergency care | National survey |
| Frasera MS, 2020 | Journal article | Afr J Emerg Med 2020;10(1):40–5 | Emergency care | Local survey |
| Fant CD, 2017 | Journal article | Front. Public Health 5:322 | Emergency care | Hospital data |
| Myers JG, 2020 | Journal article | BMJ Open 2017;7:e014974. | Emergency care | Hospital data |
| Kumar R, 2020 | Journal article | Pediatric Critical Care Medicine: 2019;20(12):e538-e545 | Critical care | Hospital data |
| Saleeby J, 2020 | Journal article | Afr J Emerg Med 2019;9(3):127–133 | Emergency care | Hospital data |
| Wangari W, 2020 | Journal article | J Crit Care. 2020;55:122–127 | Critical care | Review |
| Brotherton BJ, 2020 | Journal article | Crit Care 23, 244 (2019) | Critical care | Review |
A narrative synthesis was used in the analysis due to the different study designs used and the data presented was not amenable to meta-analysis.
Results
Prehospital emergency care
Our literature search did not identify any single toll-free ambulance access number or an integrated public emergency medical services (EMS) system in Kenya [12]. The Kenya Harmonized Health Facility Assessment (KHFA) 2018/2019 report identified only 18% (n = 2927) of the facilities had an ambulance on site [12,13]. Delays in ambulance transportation resulted in patients having to wait for hours for an ambulance [14].
Emergency centres
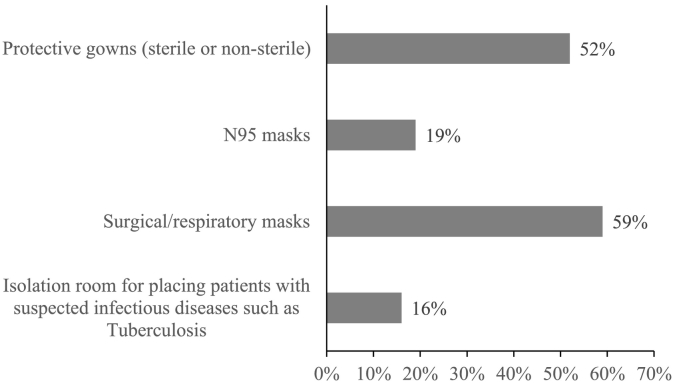
The World Health Assembly (WHA) Resolution 72.16 in May 2019 urged member states to establish a dedicated area or unit for emergency services and care in all first-level hospitals and above with appropriate equipment and capacity for management and diagnosis [15]. First-level hospitals are the lowest level of health care facilities that can provide major surgery [16]. In the Kenya healthcare system, these would be level 4 facilities [11]. Only 20% (n = 411) of level 4, 5 and 6 hospitals in Kenya had a dedicated 24-h emergency centre [13]. There was no nationally accepted emergency centre triage system [17,18]. Fig. 1 below shows the proportion of facilities in Kenya from the KHFA 2018/2019 report that had infection prevention items for general emergency services among facilities that provided this service in a designated emergency area [13].
Fig. 1.
Proportion of facilities in Kenya in 2018 that had infection prevention items for general emergency services among facilities that provided this service in a designated emergency area. (N = 114).
The availability of pulse oximetry and oxygen therapy was 58% and 78% (n = 411) respectively [13]. Only 39% (n = 411) of the facilities could perform endotracheal intubation necessary for invasive mechanical ventilation.
Critical care
A recent national survey identified 537 ICU beds and 256 ventilators in Kenya [19]. The survey did not assess the ability of the facilities to effectively care for critically ill patients.
Discussion
Our findings identified significant gaps in the ability of hospitals in Kenya to provide emergency and critical care services for severe and critical COVID-19 patients.
Prehospital emergency care
Due to the lack of an integrated EMS system, most acutely ill and injured patients self-present to the hospitals in Kenya using private cars and taxis [20,21]. Restrictions in movement in Kenya that followed the COVID-19 pandemic meant that most patients were unable to access emergency medical care in time and this led to incidences of patients succumbing to their illnesses and injuries [12,22]. The current WHO operational considerations for case management of COVID-19 in health facility and community recommends that severely ill patients with concerns about having COVID-19 should call the prehospital care service and a basic COVID-19 ambulance sent to transport the patient to the appropriate level of emergency care [23]. The recommended ratio of one ambulance unit for every 50,000 people has previously been suggested which would result in response times as low as four to seven minutes [24,25]. This ratio does not distinguish between basic and advanced life-support capabilities. Traffic congestion, poor maps, and poor road signs which may all increase the response time in cities with poor infrastructure. With a country population size of 47.6 million, Kenya would need at least 952 ambulances [9]. Organizing simple low-cost prehospital systems has been associated with a dramatic decrease in patients' risk of death by up to 25% [26,27]. As the cases of COVID-19 in Kenya increase, there is an urgent need to strengthen the prehospital emergency care system by establishing a single national toll-free emergency access number and developing an integrated EMS system to respond to severe and critical COVID-19 cases in the community and other emergency cases, especially with the imposed travel restrictions.
Emergency departments (EDs)
Majority of the primary (level 4), secondary (level 5) and tertiary (level 6) hospitals in Kenya lack a dedicated 24-h emergency centre as prescribed by the WHA Resolution 72.16. Emergency centres serve as the first point of contact for many people around the world especially in low- and middle-income countries (LMICs) where there are logistical or financial barriers to healthcare access and people present for care only when symptomatic with acute illness or injury [28,29]. They are specifically designed to provide timely recognition of time-sensitive conditions, resuscitation and referral for severely ill patients, and the delivery of definitive care for many others. Due to the large number of COVID-19 cases expected to present to hospitals across Kenya within the next couple of months, there is a need to establish 24-h EDs in all the level 4, 5 and 6 hospitals. This will ensure patients presenting to these hospitals receive immediate lifesaving emergency care, especially the severe and critically ill patients.
Lack of national triage guidelines in Kenya could lead to the healthcare facilities in Kenya being overwhelmed by COVID-19 patients. Based on current estimates, 80% of confirmed cases of COVID-19 can be treated as outpatients, up to 20% require hospitalization and 5% need intensive care [3,4,30]. Efficient triage of patients with COVID-19 at the ED will help hospitals in the country cope with the patient influx, direct necessary medical resources to efficiently support the critically ill and protect the safety of health-care workers. The WHO algorithm for COVID-19 triage and referral for resource-limited settings during community transmission is a useful guide that should be adopted to categorise patients into those that can be isolated in the community, those needing admission to the hospital and those needing ICU care [30].
Lack of infection prevention items in emergency care facilities in Kenya could lead to an increased exposure to healthcare workers and patients. Since the identification of COVID-19 in December 2019, there have been many reports of infections in healthcare workers and hospitalised patients in both the UK and other countries across the world [[31], [32], 33., [34]]. Without the appropriate infection prevention and control measures in the EDs in Kenya, acutely ill COVID-19 patients seeking evaluation and treatment in the EDs will not only have the potential to spread the disease to the healthcare personnel but also other patients across the hospitals. Practical interventions that can be instituted to improve COVID-19 infection prevention in the ED are shown in Table 2.
Table 2.
Practical interventions to improve COVID-19 infection prevention in the ED.
| Interventions |
||
|---|---|---|
| Hand hygiene [35,36] | Improve access to necessary supplies (e.g., alcohol-based hand sanitizer, personal protective equipment (PPE)) | Empower patients to ask if the healthcare workers have performed hand hygiene |
| Standard precautions [37] | Promote PPE use through pre-notification | |
| Transmission-based precautions [37] | Redesign work processes to incorporate hand hygiene and PPE use | Employ COVID-19 screening tools in triage to identify patients requiring precautions |
| Designate clinician champions | Ask patients with respiratory complaints (i.e., cough) to wear a mask | |
| Audit practices through formal monitoring programs and provide feedback to the healthcare workers | Implement a respiratory hygiene program | |
| Post visual reminders (e.g., signs) | Ensure adequate access to airborne infection isolation rooms | |
Though most facilities in Kenya had pulse oximetry and oxygen therapy, many could not perform endotracheal intubation needed for those severe COVID-19 patients needing invasive mechanical ventilation. Most patients with severe COVID-19 disease require oxygen therapy and the most critically ill patients require mechanical ventilation [3,4]. Oxygen therapy is recommended by the World Health Organization (WHO) as the first-line therapy for treating COVID-19-induced respiratory distress and hypoxia [38]. For these reasons, there is a need to ensure all EDs within COVID-19 treatment health care facilities in Kenya are equipped with pulse oximeters and functioning oxygen systems including single-use oxygen delivery interfaces. Similarly, they need to have the necessary resources and skills to perform endotracheal intubation to ensure that those who need respiratory care support due to COVID-19, or beyond, receive it.
Critical care
The current number of ICU beds and ventilators in the country is significantly lower than the current prediction models have estimated which is an additional 1511 ICU beds and 1609 ventilators if all the expected number of COVID-19 symptomatic infections will occur within a six months period resulting in a higher peak, compared to when the same number of symptomatic infections are spread out over a longer period of time [19]. It is important to note here that the mere presence of an ICU bed does not imply the ability to effectively care for critically ill patients. In addition to the beds, an ICU must meet certain minimum standards relating to work practice, caseload, staffing and operational requirements, design, equipment and patient monitoring. The continuity of care for critically ill COVID-19 patients seen in the ED is dependent on the availability of these critical care services. Given the high burden of critical illness in COVID-19 patients, the high mortality for these patients, and the availability of strategies for their management, there is a rationale for immediately increasing the number of ICU beds and ventilators in the country as a response to the COVID-19 pandemic.
Limitations
The primary limitation of this study is the data was mainly from published secondary data. Most of the data was from national surveys that included all secondary and tertiary hospitals and all public primary hospitals. Based on this, the data is potentially representative of all the public hospitals able to provide emergency and critical care services in Kenya. The study was further limited by the fact that we could not access the raw data and did not do any physical assessments of the healthcare facilities to verify the information. Data on the availability of the specialised human resources required to provide emergency and critical care services was not available. Further research with individual facility levels of assessment around infrastructure and service provision is necessary to more narrowly define areas with significant shortfalls in emergency and critical care services as the number of COVID-19 cases in the country increase.
Conclusion
This review highlights significant gaps in the ability of hospitals in Kenya to provide emergency and critical care services for severe and critical COVID-19 patients. With no organised prehospital emergency care system, insufficient emergency centres, ICU beds and ventilators, many of these patients will be at risk of significant morbidity and mortality. In addition, the limitations in the availability of infection prevention items e.g. isolation rooms, N95 masks etc. will potentially lead to the spread of the disease to the healthcare personnel and other patients across the healthcare system. Immediate action is required by the national and county governments and all stakeholders involved in the healthcare system in Kenya to address the gaps identified in this review to enable the country to safely deal with the projected large numbers of severe and critical COVID-19 patients.
Dissemination of results
Results from this review were shared with the Ministry of Health through an informal presentation.
CRediT authorship contribution statement
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content:
BW contributed 65% and MM 35%.
All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declared no conflicts of interest.
Contributor Information
Benjamin W. Wachira, Email: benjamin.wachira@aku.edu.
Margarita Mwai, Email: margarita.mwai@aku.edu.
References
- 1.Hethcote H.W. The mathematics of infectious diseases. SIAM Rev. 2000;42(4):599–653. doi: 10.1137/S0036144500371907. Available from. [DOI] [Google Scholar]
- 2.World Health Organisation (WHO) WHO coronavirus disease (COVID-19) dashboard. World Health Organ. 2020. https://covid19.who.int/ Available from: [accessed 19 May 2020]
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323(13):1239–42. Available from: doi: 10.1001/jama.2020.2648. [DOI] [PubMed]
- 4.Livingston E., Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;323(14):1335. doi: 10.1001/jama.2020.4344. Available from. [DOI] [PubMed] [Google Scholar]
- 5.Radu S. Countries with the most well-developed public health care systems. US News World Rep. 2020 https://www.usnews.com/news/best-countries/slideshows/countries-with-the-most-well-developed-public-health-care-system/ Available from: accessed 19 May 2020. [Google Scholar]
- 6.Sambala E.Z., Kanyenda T., Iwu C.J., Iwu C.D., Jaca A., Wiysonge C.S. Pandemic influenza preparedness in the WHO African region: are we ready yet? BMC Infect Dis. 2018;18:567. doi: 10.1186/s12879-018-3466-1. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brand SPC, Aziza R, Kombe IK, Agoti CN, Hilton J, Rock KS et al. Forecasting the scale of the COVID-19 epidemic in Kenya. medRxiv. Available from: 10.1101/2020.04.09.20059865 [accessed 24 May 2020]. [DOI]
- 8.National Council for Law Reporting . National Council for Law Reporting; 2010. The constitution of Kenya, 2010. [Google Scholar]
- 9.Kenya National Bureau of Statistics (KNBS) KNBS; 2020. 2019 Kenya population and housing census volume I: population by county and sub-county.https://www.knbs.or.ke/?wpdmpro=2019-kenya-population-and-housing-census-volume-i-population-by-county-and-sub-county Available from: accessed 17 May 2020. [Google Scholar]
- 10.Ministry of Health. Kenya Master Health Facility List Ministry of Health. 2020. http://kmhfl.health.go.ke/#/home Available from: accessed 8 May 2020.
- 11.Ministry of Health . Ministry of Health; 2007. Reversing the trends: the second national health sector strategic plan of Kenya – NHSSP II 2005–2010.http://www.healthyfutures.eu/images/healthy/deliverables/D5.1/Kenya/kenya%20second%20national%20health%20sector%20strategic%20plan%202005%20-%202010.pdf Available from: accessed 19 May 2020. [Google Scholar]
- 12.Matiang'i F. Order; 2020. The Public Order Act (Cap. 56), The Public Order (State Curfew)http://kenyalaw.org/kl/fileadmin/pdfdownloads/LegalNotices/2020/LN36_2020.pdf Available from: accessed 20 May 2020. [Google Scholar]
- 13.Ministry of Health . Ministry of Health; 2020. The Kenya Harmonized Health Facility Assessment (KHFA) 2018–2019.https://www.health.go.ke/wp-content/uploads/2020/01/KHFA-2018-19-Popular-version-report-Final-.pdf Available from: accessed 8 May 2020. [Google Scholar]
- 14.Otieno B. Man dies after refusing to board covid-19 ambulance. The Star. 2020 https://www.the-star.co.ke/news/2020-05-10-man-dies-after-refusing-to-board-covid-19-ambulance/ Available from: accessed 20 May 2020. [Google Scholar]
- 15.World Health Organisation (WHO) World Health Organ; 2020. World Health assembly resolution 72.16.https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf?ua=1 Available from: accessed 20 May 2020. [Google Scholar]
- 16.Jamison D.T., Breman J.G., Measham A.R., Alleyne G., Claeson M., Evans D.B. 2nd ed. World Bank; Washington, DC: 2006. Disease control priorities in developing countries. [PubMed] [Google Scholar]
- 17.Wachira B.W., Wallis L.A., Geduld H. An analysis of the clinical practice of emergency medicine in public emergency departments in Kenya. Emerg Med J. 2012;29(6):473–476. doi: 10.1136/emj.2011.113753. Available from. [DOI] [PubMed] [Google Scholar]
- 18.Lampi M., Junker J.P.E., Tabu J.S., Berggren P., Jonson C.-O., Wladis A. Potential benefits of triage for the trauma patient in a Kenyan emergency department. BMC Emerg Med. 2018;18(1):49. doi: 10.1186/s12873-018-0200-7. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barasa E, Ouma PO, Okiro EA. Assessing the hospital surge capacity of the Kenyan health system in the face of the COVID-19 pandemic. PLoS ONE 15(7): e0236308. Available from: doi: 10.1371/journal.pone.0236308. [DOI] [PMC free article] [PubMed]
- 20.Wachira B.W., Smith W. Major incidents in Kenya: the case for emergency services development and training. Prehospital Disaster Med. 2013;28(2):170–173. doi: 10.1017/S1049023X13000010. Available from. [DOI] [PubMed] [Google Scholar]
- 21.Broccoli M.C., Calvello E.J., Skog A.P., Wachira B., Wallis L.A. Perceptions of emergency care in Kenyan communities lacking access to formalised emergency medical systems: a qualitative study. BMJ Open. 2015;5(11) doi: 10.1136/bmjopen-2015-009208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korir W. Petition 120 of 2020 (Covid 025) Kenya Law. 2020 http://kenyalaw.org/caselaw/cases/view/193192/ Available from: accessed 19 May 2020. [Google Scholar]
- 23.World Health Organization (WHO). Operational considerations for case management of COVID-19 in health facility and community: interim guidance 19 March 2020. World Health Organ.2020. Available from: https://www.who.int/publications-detail/operational-considerations-for-case-management-of-covid-19-in-health-facility-and-community [accessed 20 May 2020].
- 24.McSwain N. Trauma. Appleton and Lange; Norwalk, CT: 1991. Prehospital emergency medical systems and cardiopulmonary resuscitation; pp. 99–107. [Google Scholar]
- 25.Braun O., McCallion R., Fazackerley J. Characteristics of midsized urban EMS systems. Ann Emerg Med. 1990;19(5):536–546. doi: 10.1016/S0196-0644(05)82186-9. Available from. [DOI] [PubMed] [Google Scholar]
- 26.Husum H., Gilbert M., Wisborg T., Van Heng Y., Murad M. Rural prehospital trauma systems improve trauma outcome in low-income countries: a prospective study from North Iraq and Cambodia. J Trauma Inj Infect Crit Care. 2003;54(6):1188–1196. doi: 10.1097/01.TA.0000073609.12530.19. Available from. [DOI] [PubMed] [Google Scholar]
- 27.Henry J., Reingold A. Prehospital trauma systems reduce mortality in developing countries: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2012;73(1):261–268. doi: 10.1097/TA.0b013e31824bde1e. Available from. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organisation (WHO) World Health Organ; 2020. Emergency care.https://www.who.int/health-topics/emergency-care#tab=tab_2 Available from. accessed 20 May 2020. [Google Scholar]
- 29.Cannoodt L., Mock C., Bucagu M. Identifying barriers to emergency care services. Int J Health Plann Manage. 2012;27(2):e104–e120. doi: 10.1002/hpm.1098. Available from. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organisation (WHO) World Health Organ; 2020. Algorithm for COVID-19 triage and referral. Patient triage and referral for resource-limited settings during community transmission - 22 March 2020.https://iris.wpro.who.int/bitstream/handle/10665.1/14502/COVID-19-algorithm-referral-triage-eng.pdf Available from: accessed 23 May 2020. [Google Scholar]
- 31.Hunter J.C., Nguyen D., Aden B., Al Bandar Z., Al Dhaheri W., Abu Elkheir K. Transmission of Middle East respiratory syndrome coronavirus infections in healthcare settings. Abu Dhabi. Emerg Infect Dis. 2016;22(4):647–656. doi: 10.3201/eid2204.151615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keeley A.J., Evans C., Colton H., Ankcorn M., Cope A., State A. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020;25(14):2000433. doi: 10.2807/1560-7917.ES.2020.25.14.2000433. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7160437/ Available from: accessed 23 May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.SARS-CoV-2 infection in 86 healthcare workers in two Dutch hospitals in March 2020. medRxiv. Available from: https://www.medrxiv.org/content/10.1101/2020.03.23.20041913v3 [accessed 23 May 2020].
- 34.Wang X., Pan Z., Cheng Z. Association between 2019-nCoV transmission and N95 respirator use. J Hosp Infect. 2020;105(1):104–105. doi: 10.1016/j.jhin.2020.02.021. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boyce J.M., Pittet D. Healthcare Infection Control Practices Advisory Committee, HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep. 2002;51(RR-16):1–45. quiz CE1-4. [PubMed] [Google Scholar]
- 36.World Health Organisation (WHO). WHO guidelines on hand hygiene in health care: first global patient safety challenge: clean care is safer care. World Health Organ.2020. Available from: https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf. [PubMed]
- 37.Siegel J.D., Rhinehart E., Jackson M., Chiarello L. Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10 Suppl 2):S65–S164. doi: 10.1016/j.ajic.2007.10.007. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organisation (WHO) World Health Organ; 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected.https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf Available from. [Google Scholar]