Abstract
The mutual dependence of human and animal health is central to the One Health initiative as an integrated strategy for infectious disease control and management. A crucial element of the One Health includes preparation and response to influenza A virus (IAV) threats at the human-animal interface. The IAVs are characterized by extensive genetic variability, they circulate among different hosts and can establish host-specific lineages. The four main hosts are: avian, swine, human and equine, with occasional transmission to other mammalian species. The host diversity is mirrored in the range of the RT-qPCR assays for IAV detection. Different assays are recommended by the responsible health authorities for generic IAV detection in birds, swine or humans. In order to unify IAV monitoring in different hosts and apply the One Health approach, we developed a single RT-qPCR assay for universal detection of all IAVs of all subtypes, species origin and global distribution. The assay design was centred on a highly conserved region of the IAV matrix protein (MP)-segment identified by a comprehensive analysis of 99,353 sequences. The reaction parameters were effectively optimised with efficiency of 93–97% and LOD95% of approximately ten IAV templates per reaction. The assay showed high repeatability, reproducibility and robustness. The extensive in silico evaluation demonstrated high inclusivity, i.e. perfect sequence match in the primers and probe binding regions, established as 94.6% for swine, 98.2% for avian and 100% for human H3N2, pandemic H1N1, as well as other IAV strains, resulting in an overall predicted detection rate of 99% on the analysed dataset. The theoretical predictions were confirmed and extensively validated by collaboration between six veterinary or human diagnostic laboratories on a total of 1970 specimens, of which 1455 were clinical and included a diverse panel of IAV strains.
Introduction
In 2004 the World Health Organization (WHO), the World Organization for Animal Health (OIE), the United Nations’ Food and Agriculture Organization and the World Bank proposed a One Health Initiative as a holistic perspective on the management and control of influenza A virus (IAV) threats at the human-animal interface [1]. The One Health concept is based on the realization that human and animal health allied to environmental safeguarding are inextricably linked [2]. All IAVs originate from the wild bird reservoir across a very wide geographical range. They include many different genotype combinations of the eight genomic segments, but all IAVs are classically subdivided into subtypes defined by the hemagglutinin (HA) and neuraminidase (NA) glycoprotein combinations. A mechanism of variability includes drift which affects all eight genetic segments, with additional genetic diversity and scope for viral evolution provided by reassortment among the segments. In the case of HA and NA gene segments, their reassortment (genetic and associated antigenic shift) has featured in the emergence of novel human IAV pandemics [3, 4].
Along with the established human seasonal IAVs [5, 6], important animal IAVs include the avian influenza viruses (AIVs) [7–9] and swine influenza viruses (SwIVs) [10, 11]. AIVs in particular are recognized as a key potential threat to poultry and human health globally, with the notifiable H5 and H7 AIV subtypes having the potential to mutate from low pathogenicity (LP)AIV to the corresponding highly-pathogenic (HP)AIV with consequent virulent infections in farmed birds [7, 9]. Pigs are another important host which has been long known to serve as a “mixing vessel” for IAVs of different species origins, enabling genetic reassortment to generate new circulating SwIV strains in pigs which may potentially transmit zoonotically [12, 13]. Therefore, collaboration between human and animal health experts is prudent to respond to the threats posed by different IAV strains, particularly where a newly-evolved strain may threaten to cross or has crossed the species barrier, and harmonise the appropriate prevention and control steps [14]. The One Health approach prepared for the threat of goose/Guangdong H5N1 (GsGd) HPAIVs [9] to both poultry and public health, and also to the 2009 pandemic H1N1 (H1N1pdm09) IAVs which spread globally in humans [15] and also became established in pigs [11].
A key component of the One Health concept is to ensure our ability to sensitively, specifically and universally detect IAVs from different host species and sample matrices. The relatively conserved bicistronic genomic segment no. 7 (matrix protein (MP)-segment) of the viral genome is an attractive region for generic IAV detection by RT-qPCR. Primer and probe binding regions were previously selected within the most conserved regions of the AIV MP-segment, to guide the design and validation of an RT-qPCR for the global detection of AIVs belonging to all sixteen HA-subtypes [16]. Blind trials in a consortium of five European AI reference laboratories [17] led to international acceptance of this generic AIV detection protocol by the European Union and the OIE [18–20]. This assay has proven itself as a sensitive test in the initial diagnosis of suspect AIV outbreaks, prompting subsequent investigations of notifiable AIV by means of type-specific H5 and H7 RT-qPCRs [21, 22]. However, continuing genetic drift within the AIV MP-segment of newly-emerging clades of the GsGd lineage epizootic H5Nx HPAIVs compromised assay sensitivity due to nucleotide mismatches in the reverse primer binding region [23]. In addition, a more recently designed RT-qPCR which amplifies elsewhere within the MP-segment was validated [24] and featured successfully in subsequent AIV outbreaks and wild bird investigations [25–28], AIV in vivo studies [29, 30] and SwIV field investigations [31–34]. The importance of appropriate test validation has been emphasised in a veterinary context [35], with an MP-segment RT-qPCR for generic detection of contemporary H1N1, H1N2 and H3N2 SwIV subtypes in European pigs having been also validated [36].
In the case of human seasonal IAVs, a recent WHO protocol lists four different MP-segment RT-qPCR assays to encompass both seasonal and potential zoonotic strains [37]. Three MP RT-qPCRs continue to be listed by the OIE for IAV detection in swine, horses and birds [38–40]. Many of these assays were designed and validated in the context of IAV detection in a single species group. Although the MP-segment is relatively conserved in the IAV genome, certainly when compared to the subtype-determining HA and NA genes, continuing genetic drift has contributed to considerable nucleotide variability [41–43]. Therefore, there is an ongoing risk that the unpredictable emergence of new IAV strains with critical mismatches in the primer and/or probe binding sequences may compromise the sensitivity of the RT-qPCR assay, therefore requiring assay modifications or replacement [23, 36, 44, 45]. Such primer or probe complementarity problems may only be recognised retrospectively, when outbreaks, epizootics or epidemics are already ongoing. In addition, the history of human IAV pandemics has underlined the importance of retaining the ability to detect historical, re-emerging IAV strains [46, 47]. In the case of H1N1pdm09, its MP-segment had apparently circulated unrecognized in swine for roughly for a decade [15]. Given these challenges, consideration of a single generic approach for universal IAV detection of all subtypes remains highly desirable, particularly in the relevant One Health species groups. This study describes the careful modification of the MP-segment RT-qPCR [24] based on the analyses of 99,353 IAV MP-segment sequences available in public sequence databases, together with its comprehensive validation. Crucially, the modified assay design employed novel, more refined, in silico bioinformatics approaches [43].
Materials and methods
Clinical specimens, viral and bacterial taxa
Three specimen groups were included in the assay validation: i) 949 IAV negative field specimens collected from six mammalian and 68 avian species, ii) 409 non-IAV viruses, bacteria, and vaccine strains iii) 612 IAV positive specimens. The IAV positive pool was composed of 270 AIVs in 49 subtype combinations (both HPAIV and LPAIV, all HA and NA subtypes, collected from 1956 to 2020), 120 swine H1N1, H1N2 and H3N2 viruses (collected from 1946 to 2019), 108 human H3N2, 66 human H1N1pdm, 18 human pre-2009 and eight zoonotic strains (collected from 1934 to 2019) and 21 equine IAVs of H3N8 and H7N7 subtypes (collected from 1956 to 2009). The IAV positive pool included 369 IAV laboratory isolates and 243 characterised IAV positive field specimens. The field specimens encompassed various sample matrices like cloacal, tracheal and nasopharyngeal swabs, faeces, pooled organ suspensions and bronchoalveolar lavages. The list of specimens included in the study is provided in S1.
All specimens were obtained from the repositories of the collaborating institutions. All of the sensitive data were treated anonymously according to the international standard EN ISO/IEC 17025: 2018 and the entire data management is compliant with General Data Protection Regulation of the European Union.
Quantified standard (QS)
Total nucleic acid extracts of A/mallard/Czech Republic/13579-84K/2010 (H4N6) and A/goose/Czech Republic/1848-T14/2009 (H7N9) AIVs (further referred as QS-1 and QS-2 respectively; GenBank accession numbers JF789621 and HQ244418) were quantified by comparison to a dilution series of a known quantity of synthetic SVIP-MP (State Veterinary Institute Prague) assay version 1 amplicon (4nM DNA ultramer, Integrated DNA Technologies) tested by the SVIP-MPv1 assay [24]. The ultramer dilution series spanned a concentration range from 1e7 to 1e2 copies/μl in triplicate. The standards were aliquoted and stored at -80°C.
Nucleic acid extraction
Nucleic acid extraction was performed by accredited means within the collaborating laboratories: i) MagNA Pure Compact (Total Nucleic Acid Extraction Kit, input volume of 200μl or 400μl and an elution volume of 50μl) and MagNA Pure 96 (DNA and Viral NA Small Volume Kit, input volume of 200μl and an elution volume of 50μl) extractors (all from Roche), ii) Nucleomag Vet kit (Macherey-Nagel) or MagAttract 96 cador Pathogen Kit (Qiagen) on King Fisher Flex 96 (Thermo Fisher Scientific): Input volume 200μl and elution volume 100μl, and iii) manual and robotic extraction depending on the origin of the specimen, as described by Slomka et al. [48].
Primers and probe selection
The primers and the probe (Table 1) were selected upon a comprehensive in-silico analysis of 99,353 AIV MP sequences which represented the entire collection of the Influenza Virus Database (IVD) (https://www.ncbi.nlm.nih.gov/genomes/FLU/Database/nph-select.cgi?go=database) [49] and Global Initiative on Sharing All Influenza Data’s EpiFlu (https://www.gisaid.org/) database collection as of February 2018 [43]. Briefly, the sequences were downloaded in five data pools (Table 2) and aligned with the MAFFT (Multiple Alignment using Fast Fourier Transform) tool [50]. Alignment processing was performed with the AliView program [51]. Positional nucleotide numerical summary (PNNS) and entropy were calculated by the PNNS calculator and Entropy Calculator modules of the Alignment Explorer web application [52].
Table 1. The primer and probe details.
| Name | Sequence 5’→ 3’ | Position | Label |
|---|---|---|---|
| SVIP-MP-F | GGCCCCCTCAAAGCCGA | 77–93 | --- |
| SVIP-MP-R | CGTCTACGYTGCAGTCC | 258–242 | --- |
| SVIP-MP_P2-MGB | TCACTKGGCACGGTGAGCGT | 237–218 | 5’FAM-3’MGB-NFQ(EQ)* |
* The quencher type is supplier dependent; the probe is in reverse direction.
Table 2. The MP-segment data groups, database origin and SVIP-MPv2 assay theoretical inclusivity values.
| Data groups | Database source | Downloaded MP-sequences | Number of informative sequences# | Assay inclusivity | |
|---|---|---|---|---|---|
| Human H3N2 | GISAID | 37,406 | 35,876 | 35,876 (100%) | |
| Human H1N1pdm | GISAID | 16,948 | 16,311 | 16,311 (100%) | |
| Avian | GISAID | 21,530 | 20,652 | 20,287 (98.2%) | |
| Swine | IVD | 9,337 | 9,088 | 8,596 (94.6%) | |
| Others | Others subtotal | 7,064 | 5,927 | 5,927 (100%) | |
| Human H1N1 seasonal | IVD | 3,140 | |||
| Human H7Nx | GISAID | 1,249 | |||
| Human H5Nx | GISAID | 428 | |||
| Human H2N2 | IVD | 129 | |||
| Human H1N2 | GISAID | 71 | |||
| Human H9N2 | GISAID | 22 | |||
| Human H10N8 | IVD | 6 | |||
| Environment | GISAID | 1,368 | |||
| Canine | IVD | 303 | |||
| Equine | GISAID | 238 | |||
| Feline | GISAID | 44 | |||
| Other mammals | GISAID | 70 | |||
| TOTAL | 99,353 | 87,854 | 86,997 (99.0%) | ||
# MP-segment submissions containing the primer and probe sequences.
Inclusivity assessment in-silico
The aligned MP-segment data pools were trimmed and concatenated (joining only the primer-probe-primer binding motifs into a continuous sequence; further referred as region of interest, ROI) with the AliView program [51]. Alignment stratification and sequence sorting was performed by the SequenceTracer module of the Alignment Explorer web application. The sequence variants in the alignment were considered at above the 0.5% threshold level. For a detailed analysis pipeline please refer to [43]. For additional sequence sorting according to isolate names the Fasta headers were extracted with FaBox 1.42 http://users-birc.au.dk/palle/php/fabox/ [53].
SVIP-MPv2 RT-qPCR assay
The SVIP-MP assay version 2 consists of the original SVIP-MP-F and SVIP-MP-R primer pair [24] (Integrated DNA Technologies), and a newly designed 5’ FAM-labelled and 3’-minor groove binder (MGB)-modified probe SVIP-MP_P2-MGB (Table 1; ThermoFisher Scientific, Eurofins Genomics). The primers encompass a 182 nucleotides-long amplicon. The probe is synthesised in the reverse complement orientation, i.e. its 5’-end is digested downstream from the reverse primer. The SVIP-MPv2 assay was developed and validated as a one-step procedure using the QuantiNova Probe RT-PCR Kit (Qiagen) with final concentrations of primers (1.4μM each) and probe (0.4μM) in a final volume of 25μl (20μl reaction mix and 5μl of total nucleic acid extract).
The reactions were run on the CFX 96 (BioRad) thermal cycler with the following thermoprofile: 45°C 10min, 95°C 5min followed by 45 cycles of 95°C for 10s and 64°C for 30s and 72°C 10s, with signal acquisition in the FAM channel at the end of the 64°C annealing step. The Cq (quantification cycle) values were estimated by using the automatic baseline threshold option of the CFX Manager software v3.1 or CFX Maestro software v1.1.
The diagnostic test criteria of the SVIP-MPv2 assay were evaluated as described previously [54–56] with general performance criteria defined according to [55].
MeltMan [57] SVIP-MPv2 RT-qPCR reactions were performed by adding the SYTO82 dye (Thermo Fisher Scientific) in a final concentration of 0.8μM, without changing other reaction components, and the thermoprofile was extended with melting analysis from 50°C to 95°C and continuous signal gathering in the VIC channel of the CFX96 instrument.
Efficiency
Calibration and standard curves were constructed by 10-log dilution of the QS-1 and QS-2 in a concentration from 1e6 to 1e2 (QS1) or from 1e7 to 1e2 (QS-2) copies/μl in triplicates. The dilutions were prepared in a total background nucleic acid of swine origin (at least 7ng/μl) and analysed on the CFX96 instrument. In addition, the efficiency was inferred by using linear regression analysis in the LinReg v. 2017.1 program [58].
Limit of Detection (LOD)
The LOD was estimated according to the modified Two LOD procedure [55] and expressed as influenza A virions/μl of nucleic acid extract. First, the LOD6 was determined by preparing a serial dilution of the QS in a range of 100, 50, 20, 10, 5, 2, 1 and 0.1 copies/μl in six replicates and two independent runs resulting in a total of 12 replicates per each dilution point. All dilutions series were prepared in a total swine genomic nucleic acid background with a concentration at least 7ng/μl under repeatability conditions (i.e. prepared separately before each run). The highest QC dilution with all replicates positive was considered as the LOD6 of the assay. The accuracy of the dilution series was verified at the 0.1 dilution level where a maximum of one positive result per six replicates was accepted. The LOD of the assay with 95% confidence level (LOD95%) was determined by 60 replicates of the QS dilution corresponding to the LOD6 on the condition that all 60 replicates must have shown specific positive amplification. Finally, the LOD95% was calculated by constructing the Probability of Detection (POD) curve [56].
Precision
The precision is related to the random error of measurement and characterizes the closeness of the measured values obtained by replicate measurements under specified conditions. The precision is multicomponential. We considered the repeatability (intra-assay variation) and reproducibility (inter-assay variation). The repeatability and reproducibility of the SVIP-MPv2 assay was estimated from three measurements of 12 replicates of the QS-1 in the concentration of 10x LOD95% prepared in a total swine genomic nucleic acid background (at least 7ng/μl). Each measurement was performed on different days using different CFX96 instruments where the reaction mixes were prepared by three different operators using different pipette sets. The repeatability was calculated for each run and was expressed as standard deviation (SD) and repeatability relative standard deviation as a percentage (%RSDr). The reproducibility was investigated from all three runs and the results were expressed as reproducibility relative standard deviation as a percentage %RSDR [55].
Robustness
The robustness assesses the capacity of the assay to tolerate small deviations during the experiment preparation and measurement [56]. It can also reveal instrument or qPCR kit dependence. The assay robustness was determined by implementing the fractional factorial experimental design [55, 56]. A six-parameter orthogonal combination matrix was designed to follow multiple parameters at any given time (S2 Table 1 in S3 File). We included two RT-qPCR kits QuantiNova and AgPath-ID One-Step RT-qPCR (ThermoFisher Scientific), two different platforms (CFX96 and LC480 I, (Roche)) and deviating primer (optimised and -33,3% (i.e. 0.7μM)) and probe (optimised and -50% (i.e. 0.2μM)) concentrations, erroneous reaction volumes (19μl or 21μl (+5μl of template)) and annealing temperatures of ±1°C (i.e. 63 and 65°C). In each combination the assay was tested using 10xLOD95% of QS-1 in triplicates in a single run.
Electrophoresis and sequencing
Electrophoretic analyses were performed on the TapeStation 4500 (D1000 Screen Tape and D1000 Reagents kits; all from Agilent Technologies) or by horizontal electrophoresis using a 2% (w/v) agarose gel (TAE buffer, and 10V/cm). Sequencing reactions were run using the Big Dye Terminator Cycle Sequencing Kit v3.1 and analysed on 3130 or 3500 Genetic Analysers (all from Life Technologies).
Validation
The assay was validated through a combined effort of six veterinary or human diagnostic laboratories by using the following qPCR platform and chemistry combinations: i) CFX 96 (BioRad) and LC480 I (Roche)-QuantiNova Probe RT-PCR Kit (Qiagen); ii) LightCycler 480 II (Roche) and RotorGene Q (Qiagen)-OneStep RT-PCR (Qiagen) or QuantiNova Probe RT-PCR kits; and iii) Mx3000/5P thermocylers series (Agilent)-QuantiFast Probe RT-PCR+ROXvial Kit (Qiagen).
Results
Development of the SVIP-MPv2 assay
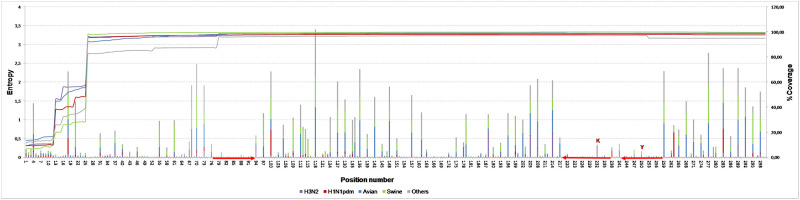
Re-assessment of the original SVIP-MP assay [24], based on in silico analysis of 99,353 downloaded IAV MP-sequences [43] confirmed the high sequence stability of the primers, guided the need for a new fluorescent probe design. Based on a highly conserved stretch at nucleotide positions 218–237, a novel FAM-labelled and MGB-modified probe SVIP-MP_P2-MGB, was selected (Table 1, Fig 1). This longer probe encompasses the original UPL104 probe motif with a K degenerate nucleotide at position 232, which improved assay inclusivity for contemporary human H3N2 strains (S2 Fig 1 in S2 File).
Fig 1. The entropy plot.
The nucleotide variation of the IAV MP-segment within positions 1–300. The variability was calculated as entropy and was visualised separately for the five data pools: Human (H3N2 and H1N1pdm), avian, swine, and others, along the primary y-axis. The column heights are proportional to the amount of nucleotide variation/position observed. The line chart shows the coverage of the selected region in a given data pool, along the secondary y-axis. The primers and probe regions of the SVIP-MPv2 assay are highlighted by red arrows. The PNNS of the primers and probe sequences are provided in S2 Fig 1 in S2 File.
Qualitative parameters of the SVIP-MPv2 assay
Efficiency
The calibration curve repeatedly showed strong linearity with a correlation coefficient R2≥0.996 and RT-qPCR efficiency ranged from 93–97% (S2 Fig 2 in S2 File). Linear regression analysis inferred from raw fluorescent signals revealed mean efficiency of 1.94±0.06.
Limit of detection
The sensitivity of the assay was expressed as LOD95% i.e. the number of IAV genome equivalents detected with 95% confidence. The LOD95% was estimated in two independent experiments by using dilution series of the QS-1 and QS-2 in a total genomic nucleic acid. The POD curve (S2 Fig 3 in S2 File) demonstrated consistent detection of approximately ten IAV genomes per 25μl reaction.
Precision
The repeatability of the SVIP-MPv2 assay revealed SD of 0.33–0.40 and %RSDr of 0.98–1.13% indicating absence of inherent random effects, even at highly diluted template quantities. The reproducibility showed SD of 1.04 and %RSDR of 2.99% suggesting that the described SVIP-MPv2 protocol may be readily transferred to other laboratories.
Robustness
The six-parameter orthogonal combination matrix showed expected results with mean Cq of 35.76±1.18 and %RSDR of 1.18% suggesting an acceptable standard of robustness. However, clear chemistry dependence was observed where the QuantiNova kit consistently showed lower Cq values in comparison with the AgPath kit. This was further confirmed by evaluating the SVIP-MPv2 assay with QuantiTect Probe RT-qPCR, OneStep RT-PCR (both from Qiagen) and AgPath RT-qPCR kits. Finally, the robustness suggested independence from the qPCR thermal cycler model.
Validation of the SVIP-MPv2 assay
The SVIP-MPv2 assay validation included the specificity and inclusivity parameters.
Specificity
The specificity demonstrated the ability of the assay to selectively detect the desired template without any false positive signal. Two components of this parameter are recognized: i) cross reaction with a host genomic nucleic acid background, or ii) with other microbial taxa present in a clinical specimen. The genomic interference was investigated on a total of 1358 IAV negative specimens of multiple matrices (S1, AIV negative specimens and others). Potential cross reaction with other viral or bacterial genomes was investigated on a total of 409 specimens composed of 15 avian, five swine, three equine and 12 human viruses and 10 bacterial taxa. The human virus collection included also 35 SARS_CoV2 positive nasopharyngeal swabs. In addition, human origin field specimens positive for two non-IAV respiratory viruses in five different combinations were analysed. Finally, assay specificity was investigated on 12 different vaccines and 10 compound feed specimens for fattening poultry (S1, others). In order to resolve weak positive FAM signals (high Cq values) and monitor the generation of nonspecific amplicons including primer dimers, the SVIP-MPv2 assay was run in MeltMan format [57]. The reactions with weak FAM curves (Cq>35) or melting peaks overlapping with the positive control were resolved by electrophoresis and if possible by amplicon sequencing. Positive FAM curves were always associated with the specific amplicon. We did not observe any non-specific, false positive FAM signal generation regardless of the host, virus or bacterial species and specimen matrix investigated including the taxonomically most closely related Influenza B (both Yamagata and Victoria lineages) and Influenza C Virus strains. This sufficiently proved the high specificity of the SVIP-MPv2 assay.
Inclusivity
This property is also known as the diagnostic sensitivity of the assay to detect as many subtypes, strains and phylogenetic lineages among all IAVs as possible. We distinguished two components of this parameter: Theoretical and experimental.
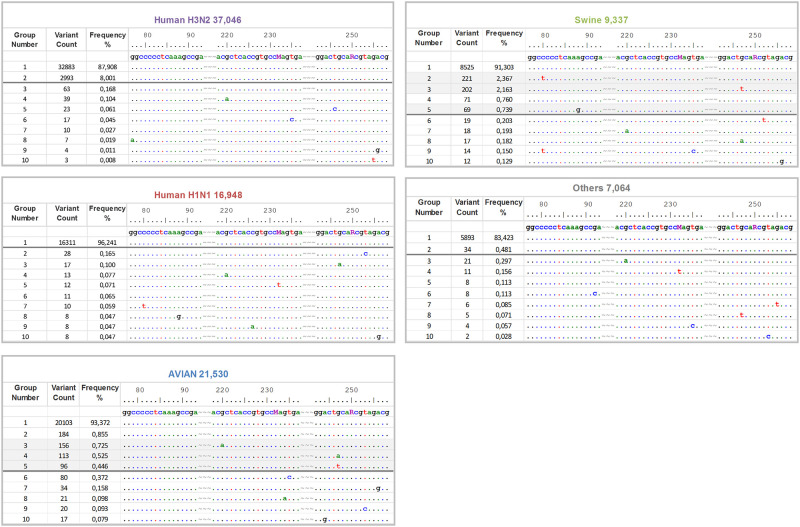
The theoretical inclusivity was calculated in-silico as the proportion of the analysed MP-sequences which has 100% identity to the primers and probe. To this end the sequence alignments were concatenated to include only the ROI and subsequently stratified. As seen, the concatenated human H3N2 data was decomposed to 39, the human H1N1pdm to 34, the avian to 112, the swine to 64 and the others to 40 ROI groups with highly asymmetrical frequency distributions (Table 2, S2 Fig 4 in S2 File). Only the ROI groups situated above the empirical threshold of 0.5% were used for the theoretical inclusivity estimation. As a result, 100% of human (both H3N2 and H1N1pdm), 98.2% of avian, 94.6% of swine and 100% of other IAV strains exhibited perfect sequence identity to the primers and probe sequences. Overall, this resulted in a 99% detection rate at the defined threshold level. The concatenated alignments are available as a Supporting dataset, enabling all of the primers or probe sequence variants to be identified by the SequenceTracer web tool [43].
The experimental inclusivity demonstrated the real ability of the assay to universally detect various IAV strains, subtypes and pathotypes in a spectrum of specimen matrices collected from different host species. The inclusivity of the SVIP-MPv2 assay was evaluated on a total of 612 IAV positive specimens of 50 subtype combinations. The list of all IAV strains, subtypes and pathotypes as well as collection dates and specimen matrices are listed in S1. All of the IAVs were successfully detected at the participating laboratories, which was in full agreement with the predicted expectations and proved the high inclusivity of the SVIP-MPv2 assay.
Experimental validation at APHA (UK) of the SVIP-MPv2 assay included parallel testing of a wide range of AIV isolates (n = 77) by the earlier SVIP-MPv1 [24] and the MP-gene RT-qPCR [16] assays (S3). Similar parallel testing of SwIV isolates (n = 54) and seven porcine respiratory tissues involved substitution of the MP-gene “perfect match” RT-qPCR [36] for the Spackman assay [16]. The APHA (UK) validation also included the testing of 79 swabs obtained from AIV outbreaks and experimentally-infected birds, assessed by both the SVIP-MPv1 and v2 RT-qPCRs. Overall, the SVIP-MPv2 assay demonstrated similar Cq values to those registered by the other MP-gene RT-qPCRs (S3).
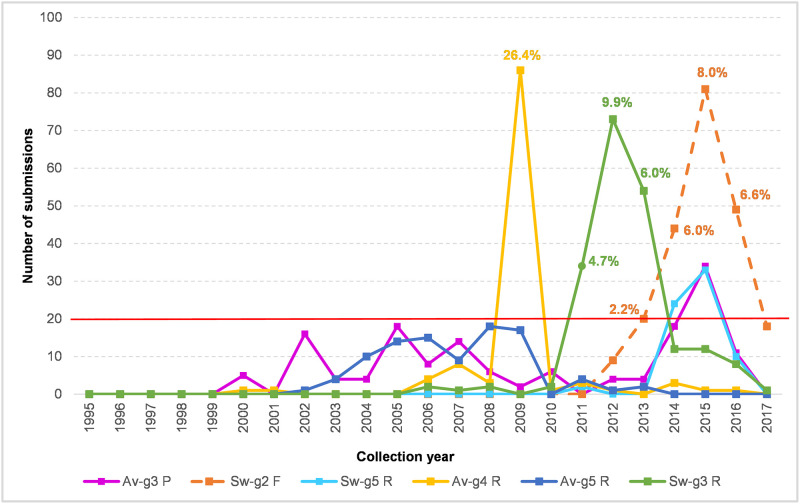
Identification of potentially critical IAV variants
The inclusivity assessment revealed three potentially critical ROI variants in the avian (Fig 2, groups 3–5) and three in the swine MP-sequence data (Fig 2, groups 2, 3 and 5). Especially, the avian-groups_3–5 and swine-groups_3 and 5 are of concern due to potential interference with probe annealing or 3′-priming. For a detailed investigation the Fasta headers were extracted from the corresponding MP-sequence groups and the spacio-temporal characteristics were further investigated. Temporal distribution chart (Fig 3) revealed three sharp peaks corresponding with avian-group_4-reverse, swine-group_2-forward and swine-group_5-reverse primers. The avian-group_4-reverse consists mainly of A/mallard/northern_pintail/(H3N8, H4N6, H10N7) strains from Alaska from a single sampling period in 2009. The swine-group_2-forward and swine-group_3-reverse were both among the US swine strains (all subtypes, i. e. H1N1, H1N2, H3N2) obtained between 2012–2017 and 2011–2016 respectively. The remaining groups were distributed at a low frequency since 2000–2003 with a slight peak of the avian-group_3-probe in 2015 (mainly A/duck/chicken/goose/Hunan/2015(H5N6)-like strains) and the swine-group_5 in 2014–2015 (predominantly A/swine/US/2014 and 2015 strains of all three subtypes). However, all of these variants occurred within the background population of the prevailing perfect match strains which dominated at the same time in a given sampling locality (Fig 3) as determined from the submitted sequence data.
Fig 2. Alignment stratification of the data pools.
Fig 3. Temporal distribution chart of the critical ROI variants.
The concatenated (forward-probe-reverse) alignments of the human H3N2 and H1N1pdm, avian, swine, and other IAVs prepared by the SequenceTracer web tool. The alignment shows the first ten MP-sequence groups in a descending order aligned to the SVIP-MPv2 primers and probe sequences (5’→3’). Note that the probe and the reverse primer sequences are shown in the forward (positive stranded) orientations. The alignment was drawn in the Graphic View mode of the BioEdit program. For clarity, the primers and probe sequences were separated by tildes and numbered according to their MP-segment positions. The dots indicate nucleotide identity and the horizontal grey bars designate the threshold (≥0.5%). The shaded groups designate potentially critical MP-segment variants. For full alignment stratifications please refer to S2 Fig 4 in S2 File.
The Fasta headers were extracted from the avian-groups_3–5 and swine-groups_3 and 5 (Fig 2; shaded) by the FaBox web tool and the submission counts per year were visualised as a line chart. The proportion of the particular group in the submissions available from the same year and geographic area were shown at key nodes as percentages.
Discussion
The study successfully exploited thorough bioinformatics analyses of the IAV MP-segment to modify an earlier RT-qPCR design by simply altering the probe sequence. Our aim was to provide a new version of the assay, SVIP-MPv2, which compensated the deficiency observed for the original version [43] and now meets the requirement for multi-species origin IAV detection in accord with the One Health initiative. In addition, the new version is independent of the proprietary commercial UPL104 probe employed in the first version, where the position, number and character of the LNA modified nucleotides have not been disclosed. There have also recently emerged difficulties in the future procurement of the UPL104 probe, so without open knowledge of its full sequence details there is presently little or no possibility of an alternative supplier.
Despite the challenges posed by the aims of this study, the SVIP-MPv2 assay was effectively optimised with a LOD95% of approximately ten IAV genome templates per reaction with high repeatability, reproducibility and robustness. The assay is compliant with the MIQE (Minimum Information for publication of Quantitative real-time PCR Experiments) guidelines [54] and the parameters fulfil the crucial diagnostic RT-qPCR criteria and validation guidelines [55]. Although these guidelines were intended for detection of genetically modified organisms, several approaches such as LOD and robustness were also adopted in our study to underline the importance of method performance and criteria for acceptance. However, the main advantage of the SVIP-MPv2 assay is its high inclusivity in detecting a range of diverse-origin IAVs. The in-silico analysis predicted 99% IAV detection rate in the analysed collection of MP sequences (n = 99,353), which included all known IAV subtypes from various host species and geographical origins obtained since 1902 [43]. The IAV-like subtypes H17N10 and H18N11, described exclusively in bats [59, 60], were excluded from the analysis because they do not pose any threats to human or livestock health. The zoonotic potential of these IAV-like viruses is unknown and they are genetically highly distinct from other IAV subtypes.
The theoretical inclusivity predictions were confirmed experimentally by six veterinary or human public health diagnostic laboratories which independently tested diverse panels of human, avian, swine and equine IAV strains obtained in a range of specimen matrices. Testing of IAV negative specimens demonstrated the high specificity of the SVIP-MPv2 assay, and included other avian viral pathogens of note. Validation included testing AIVs of diverse origins which included all 16 HA and nine NA subtypes. The AIVs included isolates and clinical specimens obtained from the most recent incursion of the important GsGd lineage into Europe, namely the H5N8 HPAIV (clade 2.3.4.4b), during early 2020 [61]. Seventy-seven AIV isolates were tested by the SVIP-MPv2 assay alongside the earlier validated SVIP-MPv1 [24] and Spackman et al. [16] MP-gene RT-qPCRs with an overall close concordance evident among the recorded Cq values, which was also observed between the first two of these assays when applied to the testing of 79 swabs obtained from AIV outbreaks or from experimentally-infected birds (S3). The choice of well-characterised IAV positive and negative specimens, both laboratory isolates and those of clinical origin, reflected the OIE guidelines for validation which underlined the need to include such reference samples [35]. The SVIP-MPv2 test also detected all IAV strains in the proficiency test organised by the European Union Reference Laboratory for AIV (Instituto Zooprofilacttico delle Venezie, Italy) in 2019 and 2020.
Replacing the probe clearly improved the in silico inclusivity of the SVIP-MP assay for the human H3N2 IAVs to 100% relative to the original 91.7% [43]. Sensitive H3N2 detection is important not only for public health, but also because this human subtype can transmit into swine leading to the establishment of new reassorted lineages [11, 62, 63]. Importantly, the assay sensitively detected the SwIV genotypes which contain the internal gene cassette of H1N1pdm origin which have become increasingly more prevalent during the past decade, regardless of the subtype determined by the glycoprotein (external) genes [11, 64]. As in the case of validation of the SVIP-MPv2 assay with well-characterised AIV isolates and clinical specimens, parallel testing of SwIVs was carried-out alongside the earlier validated MP-gene RT-qPCRs, namely the SVIP-MPv1 [24] and ‘perfect-match’ assays [36]. Again, an overall close concordance was observed among the recorded Cq values for the SwIV isolates (n = 54) and clinical specimens (n = 10).
Returning to the importance of the new SVIP-MPv2 probe design based on bioinformatics analysis the new probe retained unchanged inclusivity for the various data pools, i.e. 100% for human H1N1pdm, 98.2% for avian, 94.6% for swine and 100% for others assessed at the 0.5% threshold level. Consequently, the overall inclusivity rate increased to 99.0% from the original 95.8%. On the other hand, the slight decrease in the inclusivity for the swine IAVs (94.6%) was mainly due to the variations in the reverse primer binding positions of the US SwIVs, albeit at a low background frequency. Therefore, despite being extremely conserved, the reverse primer represents potentially vulnerable component of the assay among the US swine IAV MP-sequences. Unfortunately, the SwIVs included in the experimental validation did not include the corresponding MP-segment variants, therefore the SVIP-MPv2’s ability to detect these variants was not investigated. This small concern warrants the ongoing assessment of primers and probe sequences in silico in order to monitor for any sustained mutational trends in this region. Nevertheless, the assay’s high inclusivity for various species combined with high sensitivity predestines the SVIP-MPv2 as a universal IAV screening tool, not only for the One Health species, but also for minor or occasional mammalian hosts which merit investigation as a risk for zoonotic infection [65, 66]. The careful design of the SVIP-MPv2 assay has taken into account the long term evolutionary trends which continue within conserved genes such as MP1, so reducing the need for future modifications or adjustments which were required for the assay of Spackman et al., [16] to provide detection of pandemic H1N1 viruses in swine [36] or H5 HPAI viruses in wild and domestic birds [23, 67, 68]. Similarly, it can also reduce the number of different generic RT-qPCR techniques recommended for IAV surveillance in the human population [37].
Large-scale multiple sequence alignments (LS-MSA) represent an invaluable information source for a universal diagnostic PCR design or reassessment [69–71]. A comprehensive analysis of sequence variability based on LS-MSAs was also critical to the presented study. Nevertheless, sequence databases may be vulnerable to errors and biases which are important to consider. Although errors such as single nucleotide insertions, redundant stretches of primers or cloning vectors, sequence submissions in incorrect directions etc. can be recognized relatively easily [52, 72] and correctable during alignment, others may be more difficult to identify, e.g. stock contamination or sequencing errors [73]. In addition, it is important to consider the compositional bias which addresses significant under- or over-representation of certain sequence variants. For instance, 55% of the avian primer-probe-primer groups included only a single MP-sequence variant. How many of these may be a sequencing error, thereby representing a degree of misleading data? Conversely, how many of these are true variants, reflecting hidden evolutional plasticity even of the ultra-conserved regions of the MP-segment and potential for future emergence as a new MP variant escaping detection? While some compositional bias of the data is unavoidable the variants with the lowest frequency were discarded by setting a threshold of 0.5%.
Generally, a RT-qPCR design for universal IAV detection represents a difficult challenge. The predefined lengths and sequence motifs of the conserved regions greatly limit the freedom for oligonucleotide selection [69]. Other than perfect fit to the conserved regions, the selected primer and probe candidates may not exhibit ideal thermodynamic parameters such as sufficient lengths, melting temperature values or GC content. In addition, oligonucleotides may be vulnerable to a degree of homo- or hetero-dimerization, or hairpin formation. To overcome these undesired properties, the SVIP-MPv2 assay had to be rigorously optimised, which included adjustment of the annealing temperature to 64°C together with increased primers and probe concentrations to achieve optimal reaction parameters.
The history of IAV outbreaks suggests that novel epizootic or pandemic strains can emerge suddenly from a previously unrecognized virus population. Therefore, bioinformatics monitoring of any such novel but epidemiologically important strains remains important as regards potential sensitivity consequences for any IAV RT-qPCR. If the new IAV variant were to include novel mutations in the primer or probe binding sites, its emergence could compromise diagnostic issues especially during the early stages of the outbreak when prompt responses based on accurate epidemiological or field information are critical for the implementation of appropriate control measures. Therefore, sensitive and specific detection of the broadest range of different IAV strains and subtypes, irrespective of the host source, is of utmost importance. This study has provided a holistic approach to the development and evaluation of a RT-qPCR assay for universal IAV detection. The primers and probe, selected on the evolutionarily ultra-conserved regions in the MP-segment, were a crucial consideration to ensure the assay’s broad inclusivity for detection of the diverse IAV range. In conclusion, the modified MP-segment RT-qPCR should be used as a frontline screening tool to detect diverse IAV strains, particularly when considering the One Health perspective.
Supporting information
(XLSX)
(DOCX)
(DOCX)
(ZIP)
Acknowledgments
This work was dedicated to Dr. Martina Havlíčková, head of the National Reference Laboratory for Influenza, National Institute of Public Health, Czech Republic, our friend and colleague, who passed away in December 2019. We thank all contributors to the EpiFlu (Global Initiative on Sharing All Influenza Data) and IVD (National Centre for Biotechnology Informations) databases. Further, Drs Kristien Van Reeth (Univerity of Gent, Gent, Belgium) and Gustavo del Real (Instituto Nacional de Investigación y Tecnología Agraria (INIA) Madrid, Spain) are gratefully acknowledged for their permission to include testing of SwIV isolates from their respective countries.
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
State Veterinary Institute Prague, Czech Republic and Veterinary Institute Zvolen, Slovak Republic: The work was performed in connection with the activities of the National Reference Laboratory for Avian Influenza Viruses and was not funded by additional financial sources. Animal and Plant Health Agency, United Kingdom: The work was funded by the Department of Environment, Food and Rural Affairs (Defra, UK) and the Devolved Administrations of Scotland and Wales through the Programmes of Work (i) “FLUFUTURES - Reducing Influenza A Virus (avian and mammalian) hazards in the UK” (SE2211) and (ii) “FLUFUTURES 2.0 - Understanding the diverse spectrum of influenza virus based threats to the UK” (SE2213); plus two Defra Contract C programmes, namely (iii) the National Reference Laboratory for Statutory and Exotic Virus Diseases of Avian Species and Relevant Hosts (SV3400), and (iv) the International Reference Laboratory for Avian Influenza and Swine Influenza (SV3006). Danam.Vet.Molbiol, Budapest, Hungary; SCG Diagnosztika Ltd., Délegyháza, Hungary; Prophyl Animal Health Ltd., Mohács, Hungary: The companies own budgets were used. The funders provided support in the form of salaries for authors [ÁD, TV, MM] but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section. No funding by any additional financial sources. National Institute of Public Health, Czech Republic: The work was supported by Ministry of Health, Czech Republic - conceptual development of research organization („The National Institute of Public Health – NIPH, 75010330“).
References
- 1.Gibbs EP. The evolution of One Health: a decade of progress and challenges for the future. Vet Rec. 2014;174: 85–91. 10.1136/vr.g143 [DOI] [PubMed] [Google Scholar]
- 2.Powdrill TF, Nipp TL, Rinderknecht JL. One health approach to influenza: assessment of critical issues and options. Emerg Infect Dis. 2010;16: e1. [DOI] [PubMed] [Google Scholar]
- 3.Webster RG, Laver WG, Air GM, Schild GC. Molecular mechanisms of variation in influenza viruses. Nature. 1982;296: 115–21. 10.1038/296115a0 [DOI] [PubMed] [Google Scholar]
- 4.Lowen AC. Constraints, drivers, and implications of influenza a virus reassortment. Annu Rev Virol. 2017; 4: 105–121. 10.1146/annurev-virology-101416-041726 [DOI] [PubMed] [Google Scholar]
- 5.Bailey ES, Choi JY, Fieldhouse JK, Borkenhagen LK, Zemke J, Zhang D, et al. The continual threat of influenza virus infections at the human-animal interface: What is new from a one health perspective? Evol Med Public Health. 2018;2018: 192–198. 10.1093/emph/eoy013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krammer F, Smith GJD, Fouchier RAM, Peiris M, Kedzierska K, Doherty PC, et al. Influenza. Nat Rev Dis Primers. 2018;4: 3 10.1038/s41572-018-0002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexander DJ, Brown IH. History of highly pathogenic avian influenza. Rev Sci Tech. 2009;28: 19–38. 10.20506/rst.28.1.1856 [DOI] [PubMed] [Google Scholar]
- 8.Capua I, Alexander DJ. Avian influenza infections in birds-a moving target. Influenza Other Respir Viruses. 2007;1: 11–18. 10.1111/j.1750-2659.2006.00004.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lycett SJ, Duchatel F, Digard P. A brief history of bird flu. Philos Trans R Soc Lond B Biol Sci. 2019;374: 20180257 10.1098/rstb.2018.0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown IH. History and epidemiology of Swine influenza in Europe. Curr Top Microbiol Immunol. 2013; 370: 133–146. 10.1007/82_2011_194 [DOI] [PubMed] [Google Scholar]
- 11.Vincent A, Awada L, Brown I, Chen H, Claes F, Dauphin G, et al. Review of influenza A virus in swine worldwide: a call for increased surveillance and research. Zoonoses Public Health. 2014; 61: 4–17. 10.1111/zph.12049 [DOI] [PubMed] [Google Scholar]
- 12.Bourret V. Avian influenza viruses in pigs: An overview. Vet J. 2018; 239: 7–14. 10.1016/j.tvjl.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 13.Harris KA, Freidl GS, Munoz OS, von Dobschuetz S, De Nardi M, Wieland B, et al. Epidemiological Risk Factors for Animal Influenza A Viruses Overcoming Species Barriers. Ecohealth. 2017;14: 342–360. 10.1007/s10393-017-1244-y [DOI] [PubMed] [Google Scholar]
- 14.Dwyer DE, Kirkland PD. Influenza: One Health in action. N S W Public Health Bull. 2011;22: 123–6. 10.1071/NB11005 [DOI] [PubMed] [Google Scholar]
- 15.Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459: 1122–5. 10.1038/nature08182 [DOI] [PubMed] [Google Scholar]
- 16.Spackman E, Senne DA, Myers TJ, Bulaga LL, Garber LP, Perdue ML, et al. Development of a real-time reverse transcriptase PCR assay for type A influenza virus and the avian H5 and H7 hemagglutinin subtypes. J Clin Microbiol. 2002;40: 3256–3260. 10.1128/jcm.40.9.3256-3260.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slomka MJ, Coward VJ, Banks J, Londt BZ, Brown IH, Voermans J, et al. Identification of sensitive and specific avian influenza polymerase chain reaction methods through blind ring trials organized in the European Union. Avian Dis. 2007;51: 227–234. 10.1637/7674-063006R1.1 [DOI] [PubMed] [Google Scholar]
- 18.EU, E.U. Commission Decision of 4 August 2006 approving a Diagnostic Manual for avian influenza as provided for in Council Directive 2005/94/EC.
- 19.Hoffmann B, Beer M, Reid SM, Mertens P, Oura CA, van Rijn PA, et al. A review of RT-PCR technologies used in veterinary virology and disease control: sensitive and specific diagnosis of five livestock diseases notifiable to the World Organisation for Animal Health. Vet Microbiol. 2009;139: 1–23. 10.1016/j.vetmic.2009.04.034 [DOI] [PubMed] [Google Scholar]
- 20.OIE, World Oganization of Animal Health, Avian Influenza (infection with avian influenza viruses), Chapter 3.3.4 "Manual of Diagnostic tests and Vaccinesdfor Terrestrial Animals".2015.
- 21.Seekings AH, Slomka MJ, Russell C, Howard WA, Choudhury B, Nunez A, et al. Direct evidence of H7N7 avian influenza virus mutation from low to high virulence on a single poultry premises during an outbreak in free range chickens in the UK, 2008. Infect Genet Evol. 2018;64: 13–31. 10.1016/j.meegid.2018.06.005 [DOI] [PubMed] [Google Scholar]
- 22.Slomka MJ, Irvine RM, Pavlidis T, Banks J, Brown IH. Role of real-time RT-PCR platform technology in the diagnosis and management of notifiable avian influenza outbreaks: experiences in Great Britain. Avian Dis. 2010;54: 591–596. 10.1637/8947-052909-Reg.1 [DOI] [PubMed] [Google Scholar]
- 23.Slomka MJ, To TL, Tong HH, Coward VJ, Hanna A, Shell W, et al. Challenges for accurate and prompt molecular diagnosis of clades of highly pathogenic avian influenza H5N1 viruses emerging in Vietnam. Avian Pathol. 2012;41: 177–193. 10.1080/03079457.2012.656578 [DOI] [PubMed] [Google Scholar]
- 24.Nagy A, Vostinakova V, Pirchanova Z, Cernikova L, Dirbakova Z, Mojzis M, et al. Development and evaluation of a one-step real-time RT-PCR assay for universal detection of influenza A viruses from avian and mammal species. Arch Virol. 2010;155: 665–73. 10.1007/s00705-010-0636-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagy A, Černíková L, Jiřincová H, Havlíčková M, Horníčková J. Local-scale diversity and between-year "frozen evolution" of avian influenza A viruses in nature. PLoS One. 2014;9: e103053 10.1371/journal.pone.0103053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hill SC, Hansen R, Watson S, Coward V, Russell C, Cooper J, et al. Comparative micro-epidemiology of pathogenic avian influenza virus outbreaks in a wild bird population. Philos Trans R Soc Lond B Biol Sci. 2019;374: 20180259 10.1098/rstb.2018.0259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reid SM, Brookes SM, Nunez A, Banks J, Parker CD, Ceeraz V, et al. Detection of non-notifiable H4N6 avian influenza virus in poultry in Great Britain. Vet Microbiol. 2018;224: 107–115. 10.1016/j.vetmic.2018.08.026 [DOI] [PubMed] [Google Scholar]
- 28.Reid SM, Nunez A, Seekings AH, Thomas SS, Slomka MJ, Mahmood S, et al. Two Single Incursions of H7N7 and H5N1 Low Pathogenicity Avian Influenza in U.K. Broiler Breeders During 2015 and 2016. Avian Dis. 2019; 63: 181–192. 10.1637/11898-051418-Reg.1 [DOI] [PubMed] [Google Scholar]
- 29.Slomka MJ, Seekings AH, Mahmood S, Thomas S, Puranik A, Watson S, et al. Unexpected infection outcomes of China-origin H7N9 low pathogenicity avian influenza virus in turkeys. Sci Rep. 2018;8: 7322 10.1038/s41598-018-25062-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puranik A, Slomka MJ, Warren CJ, Thomas SS, Mahmood S, Byrne AMP, et al. Transmission dynamics between infected waterfowl and terrestrial poultry: Differences between the transmission and tropism of H5N8 highly pathogenic avian influenza virus (clade 2.3.4.4a) among ducks, chickens and turkeys. Virology. 2020;541: 113–123. 10.1016/j.virol.2019.10.014 [DOI] [PubMed] [Google Scholar]
- 31.Ryt-Hansen P, Larsen I, Kristensen CS, Krog JS, Wacheck S, Larsen LE. Longitudinal field studies reveal early infection and persistence of influenza A virus in piglets despite the presence of maternally derived antibodies. Vet Res. 2019;50: 36 10.1186/s13567-019-0655-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ryt-Hansen P, Pedersen AG, Larsen I, Krog JS, Kristensen CS, Larsen LE. Acute Influenza A virus outbreak in an enzootic infected sow herd: Impact on viral dynamics, genetic and antigenic variability and effect of maternally derived antibodies and vaccination. PLoS One. 2019;14: e0224854 10.1371/journal.pone.0224854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ryt-Hansen P, Larsen I, Kristensen CS, Krog JS, Larsen LE. Limited impact of influenza A virus vaccination of piglets in an enzootic infected sow herd. Res Vet Sci. 2019;127: 47–56. 10.1016/j.rvsc.2019.10.015 [DOI] [PubMed] [Google Scholar]
- 34.Ryt-Hansen P, Pedersen AG, Larsen I, Kristensen CS, Krog JS, Wacheck S, et al. Substantial Antigenic Drift in the Hemagglutinin Protein of Swine Influenza A Viruses. Viruses. 2020;12: pii E248 10.3390/v12020248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.OIE, World Organisation for Animal Health. Principles and methods of validation of diagnostic assays for infectious diseases, chapter 1.1.1. 2018.
- 36.Slomka MJ, Densham AL, Coward VJ, Essen S, Brookes SM, Irvine RM, et al. Real time reverse transcription (RRT)-polymerase chain reaction (PCR) methods for detection of pandemic (H1N1) 2009 influenza virus and European swine influenza A virus infections in pigs. Influenza Other Respir Viruses. 2010;4: 277–293. 10.1111/j.1750-2659.2010.00149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO, World Health Organisation information for the molecular detection of influenza viruses. November 2018. https://www.who.int/influenza/gisrs_laboratory/molecular_diagnosis/en/
- 38.OIE, World Organisation for Animal Health. Terrestrial Manual 2018b. Avian influenza. Chapter 3.3.4.
- 39.OIE, World Organisation for Animal Health. Terrestrial Manual 2018c. Influenza A virus of swine. Chapter 3.8.7.
- 40.OIE, World Organisation for Animal Health. Terrestrial Manual 2018d. Equine influenza. Chapter 3.5.7.
- 41.Ito T, Gorman OT, Kawaoka Y, Bean WJ, Webster RG. Evolutionary analysis of the influenza A virus M gene with comparison of the M1 and M2 proteins. J Virol. 1991;65: 5491–8. 10.1128/JVI.65.10.5491-5498.1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Widjaja L, Krauss SL, Webby RJ, Xie T, Webster RG. Matrix gene of influenza A viruses isolated from wild aquatic birds: ecology and emergence of influenza A viruses. J Virol. 2004;78: 8771–9. 10.1128/JVI.78.16.8771-8779.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nagy A, Jiřinec T, Jiřincová H, Černíková L, Havlíčková M. In silico re-assessment of a diagnostic RT-qPCR assay for universal detection of Influenza A viruses. Sci Rep. 2019;9: 1630 10.1038/s41598-018-37869-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Melzl H, Wenzel JJ, Kochanowski B, Feierabend K, Kreuzpaintner B, Kreuzpaintner E, et al. First sequence-confirmed case of infection with the new influenza A(H1N1) strain in Germany. Euro Surveill. 2009;14: pii: 19203 10.2807/ese.14.18.19203-en [DOI] [PubMed] [Google Scholar]
- 45.Surveillance Group for New Influenza A(H1N1) Virus Investigation and Control in Spain. New influenza A(H1N1) virus infections in Spain, April-May 2009. Euro Surveill. 2009;14: pii: 19209 10.2807/ese.14.19.19209-en [DOI] [PubMed] [Google Scholar]
- 46.Nakajima K, Desselberger U, Palese P. Recent human influenza A (H1N1) viruses are closely related genetically to strains isolated in 1950. Nature. 1978;274: 334–9. 10.1038/274334a0 [DOI] [PubMed] [Google Scholar]
- 47.Scholtissek C, von Hoyningen V, Rott R. Genetic relatedness between the new 1977 epidemic strains (H1N1) of influenza and human influenza strains isolated between 1947 and 1957 (H1N1). Virology. 1978;89: 613–7. 10.1016/0042-6822(78)90203-9 [DOI] [PubMed] [Google Scholar]
- 48.Slomka MJ, Pavlidis T, Coward VJ, Voermans J, Koch G, Hanna A, et al. Validated RealTime reverse transcriptase PCR methods for the diagnosis and pathotyping of Eurasian H7 avian influenza viruses. Influenza and Other Respiratory Viruses. 2009;3: 151–164. 10.1111/j.1750-2659.2009.00083.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bao Y, Bolotov P, Dernovoy D, Kiryutin B, Zaslavsky L, Tatusova T, et al. The influenza virus resource at the National Center for Biotechnology Information. J Virol. 2008;82: 596–601. 10.1128/JVI.02005-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Katoh K, Misawa K, Kuma K, Miyata T. MAFFT: a novel method for rapid multiple sequence alignment based on fast Fourier transform. Nucleic Acids Res. 2002;30: 3059–66. 10.1093/nar/gkf436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Larsson A. AliView: a fast and lightweight alignment viewer and editor for large datasets. Bioinformatics. 2014;30: 3276–8. 10.1093/bioinformatics/btu531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nagy A, Jiřinec T, Černíková L, Jiřincová H, Havlíčková M. Large-scale nucleotide sequence alignment and sequence variability assessment to identify the evolutionarily highly conserved regions for universal screening PCR assay design: an example of influenza A virus. Methods Mol Biol. 2015;1275: 57–72 10.1007/978-1-4939-2365-6_4 [DOI] [PubMed] [Google Scholar]
- 53.Villesen P. FaBox: an online toolbox for fasta sequences. Mol Ecol Resources. 2007;7:965–968. [Google Scholar]
- 54.Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem. 2009;55: 611–22. 10.1373/clinchem.2008.112797 [DOI] [PubMed] [Google Scholar]
- 55.Broeders S, Huber I, Grohmann L, Berben G, Taverniers I, M. Mazzara M, et al. Guidelines for validation of qualitative real-time PCR methods. Trends Food Sci Technol. 2014;37: 115–126. [Google Scholar]
- 56.BVL, Guidelines for the single-laboratory validation of qualitative real-time PCR methods. Bundesamt für Verbraucherschutz und Lebensmittelsicherheit. BVL3; 2016.
- 57.Nagy A, Černíková L, Vitásková E, Křivda V, Dán Á, Dirbáková Z, et al. MeltMan: Optimization, Evaluation, and Universal Application of a qPCR System Integrating the TaqMan qPCR and Melting Analysis into a Single Assay. PLoS One. 2016;11: e0151204 10.1371/journal.pone.0151204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ruijter JM, Ramakers C, Hoogaars WM, Karlen Y, Bakker O, van den Hoff MJ, et al. Amplification efficiency: linking baseline and bias in the analysis of quantitative PCR data. Nucleic Acids Res. 2009;37: e45 10.1093/nar/gkp045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tong S, Li Y, Rivailler P, Conrardy C, Castillo DA, Chen LM, Recuenco S, et al. A distinct lineage of influenza A virus from bats. Proc Natl Acad Sci U S A. 2012;109: 4269–74. 10.1073/pnas.1116200109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tong S, Zhu X, Li Y, Shi M, Zhang J, Bourgeois M, et al. New world bats harbor diverse influenza A viruses. PLoS Pathog. 2013;9: e1003657 10.1371/journal.ppat.1003657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.King J, Schulze Ch, Engelhardt A, Hlinak A, Lennermann S, Rigbers R, et al. Novel HPAIV H5N8 reassortant (clade 2.3.4.4b) detected in Germany. Viruses. 2020;12:281 10.3390/v12030281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Loubet P, Enouf V, Launay O. The risk of a swine influenza pandemic: Still a concern? Expert Review of Respiratory Medicine. 2019;13: 803–805. 10.1080/17476348.2019.1645011 [DOI] [PubMed] [Google Scholar]
- 63.Van Reeth K. and Vincent AL. Influenza Viruses In: Zimmerman JJ, Karriker LA, Ramirez A, Schwartz KJ, Stevenson GW, editors. Diseases of Swine. John Wiley and Sons Inc; 2019, pp 576–593. [Google Scholar]
- 64.Watson SJ, Langat P, Reid SM, Lam TT, Cotten M, Kelly M, et al. Molecular epidemiology and evolution of influenza viruses circulating within European swine between 2009 and 2013. J Virol. 2015; 89: 9920–31. 10.1128/JVI.00840-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Borland S, Gracieux P, Jones M, Mallet F, Yugueros-Marcos J. Influenza A virus infection in cats and dogs: A literature review in the light of the "One Health" concept. Front Public Health. 2020; 8 10.3389/fpubh.2020.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Venkatesh D, Bianco C, Nunez A, Collins R, Thorpe D, Reid SM, et al. Detection of H3N8 influenza A virus with multiple mammalian-adaptive mutations in a rescued grey seal (Halichoerus grypus) pup. Virus Evol. 2020; 6: veaa016 10.1093/ve/veaa016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Heine HG, Foord AJ Wang J, Valdeter S, Walker S, Morrissy Ch. et al. Detection of highly pathogenic zoonotic influenza virus H5N6 by reverse-transcriptase quantitative polymerase chain reaction. Virol J. 2015;12: 18 10.1186/s12985-015-0250-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoffmann B, Hoffmann D, Henritzi D, Beer M, Harder TC. Riems influenza a typing array (RITA): An RT-qPCR-based low density array for subtyping avian and mammalian influenza a viruses. Sci Rep. 2016;6: 27211 10.1038/srep27211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alm E, Lesko B, Lindegren G, Ahlm C, Söderholm S, Falk KI, et al. Universal single-probe RT-PCR assay for diagnosis of dengue virus infections. PLoS Negl Trop Dis. 2014;8: e3416 10.1371/journal.pntd.0003416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Černíková L, Vitásková E, Nagy A. Development and evaluation of TaqMan real-time PCR assay for detection of beak and feather disease virus. J Virol Methods. 2017;244: 55–60. 10.1016/j.jviromet.2017.02.017 [DOI] [PubMed] [Google Scholar]
- 71.Khan KA, Cheung P. Presence of mismatches between diagnostic PCR assays and coronavirus SARS-CoV-2 genome. R. Soc. Open Sci. 2020;7: 200636 10.1098/rsos.200636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Suarez DL, Chester N, Hatfield J. Sequencing artifacts in the type A influenza databases and attempts to correct them. Influenza Other Respir Viruses 2014;8: 499–505. 10.1111/irv.12239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krasnitz M, Levine AJ, Rabadan R. Anomalies in the influenza virus genome database: New biology or laboratory errors? J Virol. 2008;82: 8947–50. 10.1128/JVI.00101-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(DOCX)
(DOCX)
(ZIP)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.