Significance
Rural people have been left out of the vast majority of research on the impacts of the COVID-19 pandemic. As such, our evidence-based understanding of the pandemic in the United States is incomplete, and rural recovery policies risk being informed by anecdotal or urban-centric information. We begin to complete this picture by measuring and assessing the impact of the COVID-19 pandemic on rural well-being in the North American West. Findings show there have been significant impacts on health-related and economic dimensions of well-being, and that these impacts are shared across sex, age, ethnicity, and education.
Keywords: COVID-19, rural America, well-being, health, economy
Abstract
Despite considerable social scientific attention to the impacts of the COVID-19 pandemic on urbanized areas, very little research has examined its impact on rural populations. Yet rural communities—which make up tens of millions of people from diverse backgrounds in the United States—are among the nation’s most vulnerable populations and may be less resilient to the effects of such a large-scale exogenous shock. We address this critical knowledge gap with data from a new survey designed to assess the impacts of the pandemic on health-related and economic dimensions of rural well-being in the North American West. Notably, we find that the effects of the COVID-19 pandemic on rural populations have been severe, with significant negative impacts on unemployment, overall life satisfaction, mental health, and economic outlook. Further, we find that these impacts have been generally consistent across age, ethnicity, education, and sex. We discuss how these findings constitute the beginning of a much larger interdisciplinary COVID-19 research effort that integrates rural areas and pushes beyond the predominant focus on cities and nation-states.
The COVID-19 pandemic has generated worldwide social and economic upheaval, with the United States experiencing disproportionately high levels of infection and economic fallout. While it has become increasingly clear that these impacts fall unevenly along lines of race, class, gender, and disability (1), research has focused much less attention on the role of rurality, despite it being a potentially critical axis along which the pandemic’s effects may vary (2). Thus, most research—and, by extension, national news coverage—has tended to highlight urban centers, resulting in limited information about how the COVID-19 pandemic is affecting rural regions.
As social scientists piece together empirical evidence to describe the COVID-19 pandemic’s macrolevel impacts across the entire country, the urban bias of data and research overlooks 46 million rural people (3–7). If left unaddressed, this gap in knowledge could result in the creation of ill-informed long-term recovery policies which are intended to serve the entire country but are ineffective for those living in rural areas.
These gaps in research are compounded by the fact that many rural communities may be uniquely vulnerable to the pandemic’s physical and economic impacts, and will require recovery plans which will look very different from those designed for urban areas. Rural regions tend to have higher levels of poverty (8), fewer job opportunities (9), and heightened vulnerability to labor market shocks (10) relative to urban areas. Further, they broadly lack access to healthcare (11), now see a heightened reliance on telehealth (12), tend to have older and health-compromised populations (13, 14), face serious barriers to enrollment in clinical trials (15), and have far more limited access to COVID-19 testing (16).
As such, scholars, policy makers, and practitioners cannot straightforwardly and uniformly apply prevailing urban-centric data and findings to rural populations. Not only does this limit a fuller understanding of the disaster itself, but it obscures the need for a more accurate and evidenced-based recovery process that is tailored to the social structural makeup of rural America.
The shortage of rural research on COVID-19 is due to a lack of publicly available, fine-grained data on rural regions. For example, although government statistics on unemployment are available for rural areas, standard errors can be quite large, and data are often suppressed for privacy, limiting the types of questions that can be reliably answered (17). When primary data collection does occur, it is often hindered by methodological difficulties stemming from the remoteness of rural areas (18).
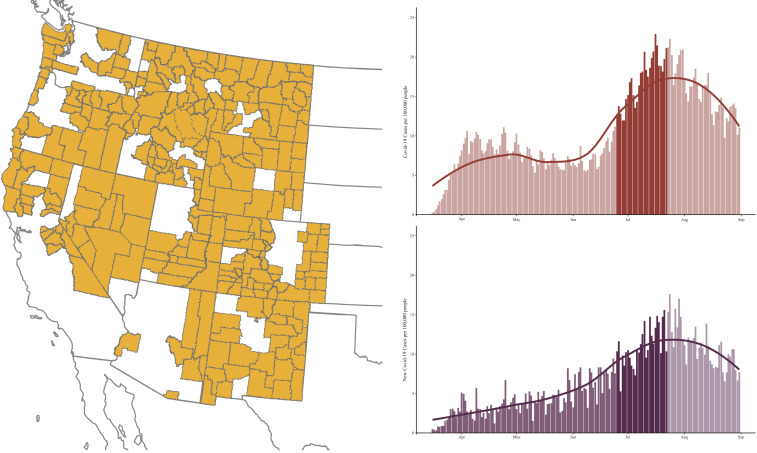
To overcome this difficulty, we launched an original data collection effort in June of 2020 in the most sparsely populated rural region of the United States—the North American West. Due to its unique social, political, and economic attributes (19), this large region is likely to have been heavily impacted by the pandemic, making it suitable for assessing how the pandemic has impacted rural well-being in the United States. Further, the geographical reach of this region makes up a substantial portion of the rural contiguous United States, inclusive of Arizona, California, Colorado, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming (Fig. 1).
Fig. 1.
(Left) Map of rural counties included in the survey sample frame highlighted in orange. (Top Right) COVID-19 daily case rate per 100,000 people in 2020 across the United States (20). The highlighted bars indicate the period of time when the survey was fielded. (Bottom Right) COVID-19 daily case rate per 100,000 people in 2020 in rural western counties (20). The highlighted bars indicate the period of time when the survey was fielded.
In this paper, we use newly collected rural data to examine how—and to what extent—the COVID-19 pandemic has impacted rural well-being. Importantly, we test this question through two essential dimensions of well-being: first, health-related well-being, measured by the level of direct experience with the virus and perceived impacts to overall life and physical and mental health; and second, economic well-being, including formal and informal work, perceived financial impacts, and perceptions of local economic health (21).
Finally, although often presumed a monolith, rural America is home to diverse populations. In addition to the epoch-spanning tenure of Indigenous communities and the long-established predominately Black communities in the rural South (22), rural America has grown increasingly racially and ethnically diverse in recent decades (23, 24), with particular population growth among Latino/Latinas (25, 26). Rural communities also fall along a broad spectrum of economic profiles, ranging from deeply impoverished to some of the wealthiest enclaves in the country (27), and are variously reliant upon natural resource extraction (28), manufacturing activities such as meatpacking (10), and natural amenity development (29). Because of this diversity, and the persistent, well-documented social and economic inequalities seen in the rural United States along the lines of gender, age, education, and ethnicity (30, 31), we not only examine well-being across the entire population but also compare results between male and female, ages, levels of education, and Latino/Latina and non-Latino/Latina in both a bivariate and multivariable context.
Results
The final analytic sample contained 1,009 respondents. As shown in Table 1, the weighted sample generally conformed to the population characteristics of the target population. In the main text, we report key findings of interest. Full statistics and confidence intervals of all variables and group comparisons, as well as multivariable models, are included in SI Appendix.
Table 1.
Demographic characteristics of sample and target population
| Population | |||||
| Variable | Levels | Sample | Nonmetro West | Nonmetro United States | |
| N | Weighted percent*,† | percent† | percent† | ||
| Sex | Male | 481 | 50.00 | 50.78 | 50.05 |
| Female | 507 | 48.00 | 49.22 | 49.94 | |
| Other | 4 | 0.70 | — | — | |
| Age, y | 18 to 29 | 46 | 10.39 | 15.21 | 15.13 |
| 30 to 39 | 95 | 23.29 | 11.97 | 11.49 | |
| 40 to 49 | 143 | 16.33 | 11.05 | 11.76 | |
| 50 to 64 | 281 | 28.58 | 20.61 | 20.94 | |
| 65+ | 409 | 20.41 | 18.60 | 18.52 | |
| Education‡ | Less than high school | 17 | 2.5 | 11.72 | 14.07 |
| High school or GED | 159 | 24.23 | 28.73 | 35.74 | |
| Some College | 251 | 38.54 | 26.18 | 21.50 | |
| Bachelors or Associates | 331 | 21.55 | 24.90 | 21.70 | |
| Graduate or professional degree | 239 | 12.94 | 8.47 | 6.99 | |
| Latino/Latina | Latino/Latina | 71 | 14.67 | 18.05 | 8.74 |
| Not Latino/Latina | 895 | 81.11 | 81.95 | 91.26 | |
| Race | White | 837 | 77.98 | 84.63 | 84.24 |
| Black | 2 | 0.09 | 1.02 | 8.26 | |
| Asian | 2 | 0.08 | 1.13 | 0.96 | |
| Native American | 23 | 4.00 | 6.17 | 2.17 | |
| Hawaiian or Pacific Islander | 2 | 0.18 | 0.15 | 0.13 | |
| Other | 48 | 6.65 | 3.81 | 1.84 | |
| Mixed race | 37 | 5.25 | 3.10 | 2.40 | |
| State | Arizona | 34 | 4.97 | 5.62 | — |
| California | 138 | 13.75 | 13.44 | — | |
| Colorado | 113 | 12.02 | 11.29 | — | |
| Idaho | 93 | 9.19 | 9.02 | — | |
| Montana | 134 | 11.04 | 10.89 | — | |
| Nevada | 105 | 3.85 | 4.40 | — | |
| New Mexico | 33 | 11.05 | 11.15 | — | |
| Oregon | 128 | 11.08 | 10.68 | — | |
| Utah | 55 | 5.03 | 5.20 | — | |
| Washington | 116 | 12.05 | 11.80 | — | |
| Wyoming | 60 | 5.98 | 6.51 | — | |
| Total N | 1,009 | — | 6,196,897 | 46,230,502 | |
Percent calculated using proportional weights by sex, age, education, Latino/Latina, Native American, and state.
Values may not equal 100%, due to rounding and/or refusals.
Census totals are for only those over the age of 25 y.
Impact on Health-Related Well-Being.
Direct experience with COVID-19.
While the COVID-19 virus initially spread through urban coastal regions within the United States, by late spring of 2020, it began quickly shifting into rural regions (Fig. 1) (32). Our survey—conducted in June and July of 2020, during this rural expansion of the virus—captures this increasing prevalence of the COVID-19 virus among rural communities. We found that, in total, 28.35% [24.73, 32.26] of respondents had at least one form of direct experience with the COVID-19 virus. Broken down by type of direct experience, 2.26%, CI [1.46, 3.48], of respondents had personally confirmed or suspected an infection themselves, 8.52%, CI [6.43, 11.20], reported that a family member contracted the virus, and 19.35%, CI [16.22, 22.90], reported that either a friend or acquaintance had a confirmed or suspected case.
COVID-19 experience varied slightly along educational lines; respondents with only a high school diploma were statistically less likely to report that a friend or acquaintance had a confirmed or suspected case than higher education groups. Perhaps notably, there was no other statistically significant variation by sex, age, education, or ethnicity in bivariate or multivariable analyses.
Self-reported impact of the COVID-19 pandemic.
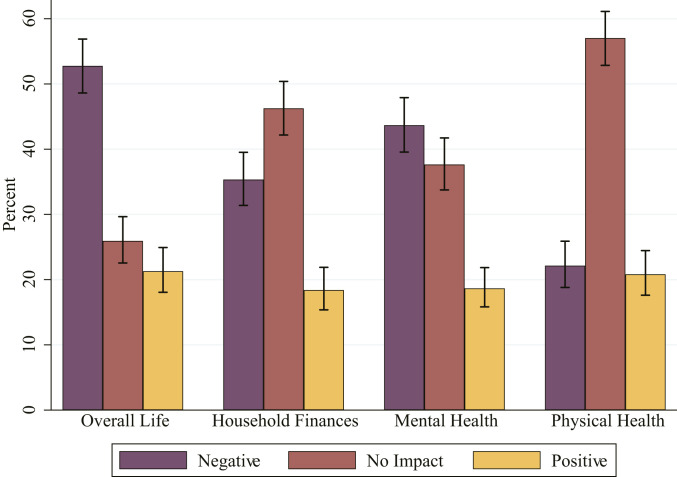
While 28.35% of rural Westerners had direct contact with the virus themselves or indirectly through their social networks, far more reported broader impacts from the pandemic and its associated economic and social effects. Respondents were asked to rate, from 1—Extremely Negative—to 10—Extremely Positive—the impact of the COVID-19 pandemic on their overall life, as well as three aspects of their lives: household finances, mental health, and physical health. All items averaged near the midpoint—with residents of the rural West reporting minor negative impacts to overall life (mean = 4.56, CI = 4.36, 4.76), household finances (mean = 4.67, CI = 4.47, 4.86), and mental health (mean = 4.64, CI = 4.46, 4.83). Impacts to physical health, although still near the midpoint, averaged on the positive side of the scale (mean = 5.22, CI = 5.02, 5.41).
When this measure is broken down into three groups, negative impact (1 to 4), no impact at all (5), and positive impact (6 to 10), we found 52.77%, CI [48.61, 56.88], of respondents reported some level of negative impact to overall life (Fig. 2). The next largest negative impact was to mental health, with 43.68%, CI [39.56, 47.90], reporting some level of negative impact. This resonates with national statistics, where 37.8% and 40.9% reported symptoms of depression or anxiety during the same period (33).
Fig. 2.
Perceived impact of the COVID-19 pandemic. Error bars represent 95% CIs.
These reported negative impacts are much higher than rates of experience with the virus, and they indicate that the broader effects of the COVID-19 pandemic are wide-reaching in rural regions. When comparing across groups, we find older adults reported significantly less negative impact from the pandemic relative to other age groups. However, there was no trend in statistically significant variation for perceived impacts by sex, education, or ethnicity. These results were consistent across bivariate and multivariable models.
Impact on Economic Well-Being.
Prior to the pandemic, rural households already struggled economically compared to their metropolitan counterparts. For instance, while rural areas were less severely impacted by the 2008 financial crisis, they have been slower to recover in the long term (34), and working poverty is much more prevalent among rural workers than urban workers (35). Combined with a heavy reliance on industries that are highly susceptible to pandemic-related closures, such as outdoor recreation, tourism, and factory work, this economic profile suggests that rural regions may be particularly vulnerable to COVID-19−related economic shocks. We investigated the pandemic’s impact on economic well-being through impacts to formal and informal work, as well as use of unemployment insurance.
Formal work.
Formal work includes work performed either independently or for a business where hours and income are reported to the government and taxes are paid. To assess the pandemic’s impacts on formal work, we asked respondents whether they were employed during 2019 before the COVID-19 pandemic, and whether that employment was full- or part-time. We found the pandemic had a significant negative impact on formal employment among rural Westerners. While 3.00%, CI [1.86, 4.81], of rural Westerners were temporarily unemployed in the year prior to the pandemic, 12.74%, CI [9.95, 16.17], were temporarily unemployed in the past month, marking a 9.74 percentage point increase. This is a slightly higher rate than comparable changes in national unemployment rates, which increased by 7.40 percentage points between June of 2019 and June of 2020 (36).
Of those reporting they were employed full-time in the year prior to the pandemic, 21.36%, CI [16.60, 27.03], were no longer employed full-time at the time of the survey. Of this 21.36%, a total of 49.90%, CI [36.35, 63.45], were temporarily unemployed, and 27.60% CI [16.47, 42.42], had shifted to part-time employment.
We see more dramatic effects of the COVID-19 pandemic for part-time employment. Of those who were employed part-time in the year prior to the pandemic, 41.07%, CI [29.29, 53.98], were not employed part-time by the time of the survey. Of those who were no longer employed part-time, 2.83%, CI [0.07, 11.12], had become full-time employees and 72.77%, CI [51.52, 87.05], were temporarily unemployed. We do not observe significant trends in variation in unemployment either prepandemic or in the month leading up to the survey across age, sex, education, or ethnicity in either the bivariate or multivariable context.
Informal work.
Informal work is labor performed for cash or the trade of goods or services which is not reported to the government, such as home repair, landscaping, or babysitting (37). Prior research suggests that rural residents are more likely than metropolitan residents to engage in informal work, especially in response to poor economic conditions (37). We found that, although many rural Westerners lost work due to the pandemic, it does not appear that they were replacing that work with informal work.
A total of 16.35%, CI [13.32, 19.92], of respondents reported at least one household member engaging in informal work in the year prior to the pandemic, while only 14.39%, CI [11.66, 17.63], reported a household member engaging in informal work in the month prior to the survey. Respondents who were 18 y to 29 y old were significantly more likely than respondents over the age of 65 y to report that someone in their household performed informal work before and during the pandemic. Further, those with no high school education were significantly more likely than any other education group to report that members of their household performed informal work during the pandemic, but not prepandemic. There were no other significant differences by sex, age, education, or ethnicity, and these results were similar across bivariate and multivariable analyses.
Use of unemployment insurance.
Unemployment benefits have proven to be a critical lifeline for affected households as COVID-19−related economic shutdowns continue and businesses begin to close permanently (38). We asked survey respondents whether they or anyone in their household used unemployment insurance in the year prior to the pandemic or whether they were on unemployment insurance at the time of the survey, and found that use of unemployment insurance rose dramatically. Just 3.00%, CI [1.86, 4.81], of respondents reported household use of unemployment insurance in the year prior to the pandemic; at the time of the survey, that number had risen to 12.31%, CI [9.71, 15.49], marking a fourfold increase in benefit use. Although not an exact comparison, this statistic is similar to the change in the national Unemployment Insurance rate over the same time period, which the Federal Reserve Bank of St. Louis reported as increasing from 1.5% in 2019 to 11.5% for the survey window (39). Further, we found these increases were felt widely across the rural West, with no significant trend in differences of unemployment insurance usage prepandemic or in the month leading up to the survey by sex, age, education, or ethnicity. Results were consistent in bivariate and multivariable analyses.
Perceptions of local economic health.
A key component of long-term economic recovery from the pandemic will be the extent to which individuals begin participating in the economy—through both work and consumption. This propensity to spend will be influenced by confidence and optimism regarding their economic situation. Understanding consumer confidence can help predict to what extent individuals will begin participating in the economy, and is a metric frequently used as an indicator for the presence or likelihood of a recession (40).
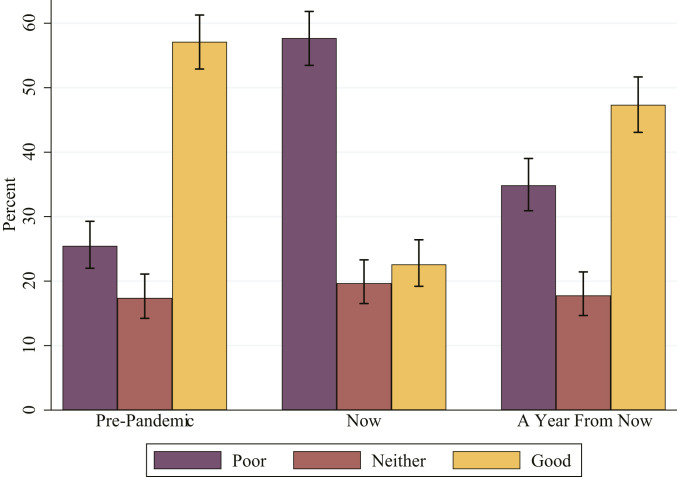
Although national measures of consumer sentiment are frequently reported (41, 42), rural specific indicators are sparse. To assess economic sentiment among residents of the rural American West, we asked respondents to indicate how healthy they think their county’s economy was in the year prior to the pandemic, at the time of the survey, and how healthy they expect it to be 1 y after the survey. Respondents rated economic health from 1—Extremely Poor—to 7—Extremely Good.
Similar to the reported national trends in consumer sentiment (41, 42), we see a statistically significant self-reported shock to economic health perceptions as a result of the pandemic, suggesting rural people felt a loss of economic confidence similar to the broader, national population. On average, survey respondents viewed their county to be in good economic health in the year before the pandemic (mean = 4.69, CI = 4.52, 4.86) and in poor economic health at the time of survey (mean = 3.34, CI = 3.19, 3.49). But, despite this near-term decline in perceptions of economic health, respondents expected to see an economic rebound a year into the future, although at a level of economic health significantly lower than in the year prior to the pandemic (mean = 4.25, CI = 4.08, 4.41).
Fig. 3 visually shows these results by breaking economic health perceptions into poor (1 to 3), neither (4), and good (5 to 7). From this, we see that 57.13%, CI [52.89, 61.27], reported their county as in good economic health before the pandemic, 22.60%, CI [19.20, 26.41], reported good economic health at the time of survey, and 47.35%, CI [43.07, 51.67], reported they expect their county to be in good economic health a year from the survey.
Fig. 3.
Reported local economic health perceptions. Error bars represent 95% CIs.
Perceptions of economic health varied significantly by level of education. Although still following the same general pattern, for all three time periods, those with graduate degrees were significantly more pessimistic than at least one group with a lower level of educational attainment. The most pronounced difference was when respondents were asked to look toward the future. Those with graduate degrees were notably more pessimistic (mean = 4.00, CI = 3.70, 4.29) than those with either no high school diploma (mean = 5.78, CI = 5.04, 6.52) or only a high school diploma (mean = 4.69, CI = 4.36, 5.03). Finally, there was no clear trend in significant differences for sex, age, or ethnicity, and these results were consistent in the multivariable models.
Discussion
We find that the COVID-19 pandemic has had wide-reaching impacts on rural well-being. Since the year prior to the pandemic, one in five full-time employed adults were no longer full-time, corresponding to a 9.74 percentage point increase in unemployment—an increase greater than the 7.40 percentage point increase seen nationally (36). As a result, reliance upon unemployment insurance has risen considerably. Furthermore, our results show that half of rural respondents perceive some level of negative impact on their overall lives and perception of local economic health has dropped dramatically.
These results provide policy-relevant evidence that continued support for healthcare (physical and mental), employment, social insurance, and public confidence in the economy are necessary for rural people in the United States. Although our findings are premised on a sample of residents living across the expansive rural western United States, these results may provide insight into rural life across the United States, especially those with similar socioeconomic conditions. That said, there are important differences across regions—such as the larger proportion of Black residents in the American South compared to larger populations of Latino/Latinas in the American West—that sustain the need for continued research on rural areas.
Although we do find some significant differences by age and education, we find that the most notable trends are similarities—rather than differences—across groups. Both direct experience with and impacts from the COVID-19 pandemic are widely shared across the population. This lack of variation is somewhat surprising given what is known about social stratification and social determinants of health in the United States (31). It will be essential that future work continues to track this variation, or lack thereof, to determine whether the impact of the COVID-19 pandemic really represents a shared experience, or whether we are simply picking up on truncated variation due to the survey occurring during the initial spike of the pandemic in many of these counties (Fig. 1).
We see major declines in perceptions of local economic health at the time of survey among all groups. However, alongside these current negative perceptions of economic health, we also see broad optimism that an economic rebound will take place within a year from the study—a belief that is held across sexes, education levels, age groups, and ethnicities. This broad optimism bodes well for increased economic activity among rural Americans, should their immediate material conditions begin to recover.
The results presented here begin the difficult work of completing the picture of the impact of the COVID-19 pandemic across all populations, communities, and geographic regions in the United States—not just the more densely populated metropolitan areas that have received the bulk of research attention. With that said, the impacts of the COVID-19 pandemic on well-being still remain poorly understood at all levels, and there remains a lack of social scientific data beyond virus case numbers and overall economic health indicators for rural areas, urban areas, and the nation as a whole.
By profiling the impacts felt by those living in the rural American West—an area representing over 6 million people—we have shown that many of the dramatic impacts documented in urban locales and on the national stage are just as prominent as, and in some cases even more pronounced, in the most geographically sparse region of the United States. As these rural regions have poorer hospital access (11), more vulnerable labor markets (10, 29), and heightened levels of material hardship compared to urban areas (8, 40, 43), these dramatic impacts likely indicate an even more difficult road to recovery. These vulnerabilities of rural areas are reflected in our findings of significant increases in unemployment, heightened use of unemployment insurance, negative impacts to mental health, and currently poor perceptions of local economic health.
This study represents the beginning of a broader, and much needed, body of work on the impacts of the COVID-19 pandemic in the rural United States. The academic and journalistic discussion of the pandemic remains dominated by an emphasis on urban areas and national trends. A broad, interdisciplinary body of work examining rural people and places within the broader context of COVID-19 is essential for understanding the full impacts of the disaster and ensuring a successful recovery. Key to this new research initiative is the continued generation of robust and timely primary data on rural people and the impacts they are experiencing. Without these data, we will be unable to create the type of evidence-based policies needed to address the needs of Americans from all parts of the country.
Methods
Data for this study were collected via dual mode phone and internet survey of residents of the rural counties in the western United States. We defined rural counties as those counties defined by the United States Office of Management and Budget (OMB) as nonmetropolitan (44). The OMB defines a county as metropolitan either if they have an urban core of at least 50,000 residents or if they are connected to a core metropolitan county by at least 25% of either rural to urban, or urban to rural commuting (44). Nonmetropolitan counties are any county not classified as metropolitan. We define the US West as the 11 states of Arizona, California, Colorado, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming. The 278 sample counties are shown in Fig. 1.
Data were collected from June 25 to July 22, 2020—a period of significant increase in the COVID-19 pandemic across the United States and within this region (Fig. 1)—and a total of 1,009 surveys were collected. The survey was administered by drawing a random sample of households from the United States Postal Service Delivery Sequence file. Addresses were then matched against publicly available databases to discern contact information for those residing at sampled addresses. Potential respondents were contacted by phone, email, and postcard, and sampling continued until a sample of at least 1,000 responses was reached. The survey was offered in English and Spanish. Yale University’s Human Research Protection Program reviewed and approved the procedures of this study under exemption determination ID#2000027941. All participants gave informed consent prior to data collection.
The sample was designed to be representative of the population at a sampling error of ±3.1% at the 95% confidence level. To accomplish this, soft quotas and oversampling were implemented for less accessible groups of young adults, Native Americans, and Latino/Latinas. To further ensure generalizability, we implemented rake weights when estimating statistics (45). Results were weighted by age, sex, Latino/Latina status, Native American status, education level, and state. This approach—although not a simple random sample, due to the stratified nature of the sampling design, the large oversample drawn to ensure timely results, and the termination of the survey at a desired N—was adopted to ensure cost-effective and timely survey administration while still providing robust and reliable results.
Due to the study design and sampling approach outlined above, a response rate is somewhat less interpretable than it would be in a simple random sample. For example, it is important to remember that, due to the halting of the survey at 1,000 responses and the blasted nature of the sampling, there is likely right censoring, where those who may have responded eventually were not given the opportunity. Relying on the most conservative formulas provided by the American Association for Public Opinion Research (AAPOR) (46), our contact rate, which represents the proportion of all cases in which a responsible member of the housing unit was reached, was 3.0% using AAPOR Contact Rate 1. This corresponds with a response rate—complete interviews relative to entire sample—calculated using the AAPOR Response Rate 1 formula of 1.1%. This low rate is unsurprising given our correspondingly low contact rate. However, our cooperation rate, which captures the proportion of all cases interviewed relative to cases contacted, was much stronger, at 37.7%, as determined by the AAPOR Cooperation Rate 1. Although our total response rate is lower than historically desirable in survey research, it is in line with nationally declining response rates (47), as well as recent surveys in pandemic contexts such as this (48). Further, our use of soft quotas for hard to reach groups and poststratification via rake weighting reduce the issues of generalizability this lower response rate may imply (49).
Data were analyzed using the survey package within Stata 15. Although the results presented in this study are generally descriptive, we estimate 95% CIs around all point estimates, to facilitate a more robust comparison of results between groups. We adopt a conservative approach and assess 95% CIs for overlap, to determine significant differences. Although this approach is stricter than a conventional P < 0.05 test via a t test or χ2 (50), we feel it is the appropriate method given the large volume of comparisons and results being presented. As such, all indications of bivariate statistical significance discussed in the results are at the P < 0.01 level (50). Further, to assess the stability of our findings when groupings are considered in tandem, we estimate exploratory multivariable models for each outcome. In the case of dichotomous outcomes, the models are linear probability models, and, in the case of continuous outcomes, they are linear ordinary least squares regressions. To ensure consistent interpretation across bivariate and multivariable analyses, we also evaluate significance of the multivariable models at the P < 0.01 level. Although we focus on a narrative and visual presentation of results for the sake of brevity, full tables are provided in SI Appendix.
Survey measures were developed through a thorough review of relevant literature and existing instruments. When possible, questions from previously published studies were adopted. Although a full description of each survey question is not included here, a detailed description of all questions reported in this paper is included in SI Appendix. The raw data and code to facilitate replication of this analysis is available on the Open Science Framework (OSF) project for this study located at DOI:10.17605/OSF.IO/64EZG.
Supplementary Material
Acknowledgments
This material is based upon work supported by the NSF under Grant 2029990: RAPID: Impacts of COVID-19 Pandemic on Rural Attitudes about Federal Aid and Recovery. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2019378118/-/DCSupplemental.
Data Availability.
Anonymized primary survey data have been deposited in OSF (DOI:10.17605/OSF.IO/64EZG). Data used to generate Covid-19 trends in Figure 1 is publicly available and was extracted from the New York Times (20). Population data from the 2014–2018 5-y American Community Survey estimates in Table 1 is publicly available as was extracted from the National Historic Geographic Information System hosted by IPUMS (51).
References
- 1.Dorn A. V., Cooney R. E., Sabin M. L., COVID-19 exacerbating inequalities in the US. Lancet 395, 1243–1244 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lakhani H. V., Pillai S. S., Zehra M., Sharma I., Sodhi K., Systematic review of clinical insights into novel coronavirus (CoVID-19) pandemic: Persisting challenges in U.S. rural population. Int. J. Environ. Res. Public Health 17, 4279 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks M. M., Voltaire S. T., “Rural families in the U.S.: Theory, research, and policy” in Rural Families and Communities in the United States: Facing Challenges and Leveraging Opportunities, Glick J. E., McHale S. M., King V., Eds. (Springer, Cham, Switzerland, 2020), pp. 253–268. [Google Scholar]
- 4.Tickamyer A. R., Sex, lies, and statistics: Can rural sociology survive restructuring? (or) what is right with rural sociology and how can we fix it. Rural Sociol. 61, 5–24 (1996). [Google Scholar]
- 5.Lobao L., Continuity and change in place stratification: Spatial inequality and middle‐range territorial units. Rural Sociol. 69, 1–30 (2004). [Google Scholar]
- 6.Bennett K. J., Rural population estimates: An analysis of a large secondary data set. J. Rural Health 29, 233–238 (2013). [DOI] [PubMed] [Google Scholar]
- 7.Puma J. E., et al. , A community‐engaged approach to collecting rural health surveillance data. J. Rural Health 33, 257–265 (2017). [DOI] [PubMed] [Google Scholar]
- 8.Weber B., Miller K., “Poverty in rural America then and now” in Rural Poverty in the United States, Tickamyer A. R., Sherman J., Warlick J., Eds. (Columbia University Press, New York, NY, 2017), pp. 28–64. [Google Scholar]
- 9.Green G., “The opportunities and limits of economic growth” in Rural Poverty in the United States, Tickamyer A. R., Sherman J., Warlick J., Eds. (Columbia University Press, New York, NY, 2017), pp. 416–438. [Google Scholar]
- 10.Thiede B., Slack T., “The old versus the new economies and their impacts” in Rural Poverty in the United States, Tickamyer A. R., Sherman J., Warlick J., Eds. (Columbia University Press, New York, NY, 2017), pp. 231–256. [Google Scholar]
- 11.Berry E., “Thinking about rural health” in Rural America in a Globalizing World: Problems and Prospects for the 2010s, Bailey C., Jensen L., Ransom E., Eds. (West Virginia University Press, Morgantown, WV, 2014), pp. 661–676. [Google Scholar]
- 12.Hirko K. A., et al. , Telehealth in response to the Covid-19 pandemic: Implications for rural health disparities. J. Am. Med. Inform. Assoc. 27, 1816–1818 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henning-Smith C., The unique impact of COVID-19 on older adults in rural areas. J. Aging Soc. Policy 32, 396–402 (2020). [DOI] [PubMed] [Google Scholar]
- 14.Peters D. J., Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. J. Rural Health 36, 446–456 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dandachi D., et al. , Treating COVID-19 in rural America. J. Rural Health (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Souch J. M., Cossman J. S., A commentary on rural-urban disparities in COVID-19 testing rates per 100,000 and risk factors. J. Rural Health (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Isserman A. M., Westervelt J., 1.5 million missing numbers: Overcoming employment suppression in County Business Patterns data. Int. Reg. Sci. Rev. 29, 311–335 (2006). [Google Scholar]
- 18.Dillman D. A., Moving survey methodology forward in our rapidly changing world: A commentary. J. Rural Soc. Sci. 31, 8 (2016). [Google Scholar]
- 19.Burow P. B., McConnell K., Farrell J., Social scientific research on the American west: Current debates, novel methods, and new directions. Environ. Res. Lett. 14, 125012 (2019). [Google Scholar]
- 20.New York Times , Data from “Coronavirus (Covid-19) data in the United States.” GitHub. https://github.com/nytimes/covid-19-data. Accessed 26 October 2020.
- 21.Linton M. J., Dieppe P., Medina-Lara A., Review of 99 self-report measures for assessing well-being in adults: Exploring dimensions of well-being and developments over time. BMJ Open 6, e010641 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thorton R., American Indian Holocaust and Survival: A Population History Since 1492 (University of Oklahoma Press, Norman, OK, 1987). [Google Scholar]
- 23.Lichter D. T., Immigration and the new racial diversity in rural America. Rural Sociol. 77, 3–35 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lichter D. T., Brown D. L., Rural America in an urban society: Changing spatial and social boundaries. Annu. Rev. Sociol. 37, 565–592 (2011). [Google Scholar]
- 25.Nelson P. B., Lee A. W., Nelson L., Linking baby boomer and Hispanic migration streams into rural America—A multi-scaled approach. Popul. Space Place 15, 277–293 (2009). [Google Scholar]
- 26.Lichter D. T., Johnson K. M., A demographic lifeline? Immigration and Hispanic population growth in rural America. Popul. Res. Policy Rev., 1–19 (2020). [Google Scholar]
- 27.Farrell J., Billionaire Wilderness: The Ultra-Wealthy and the Remaking of the American West (Princeton University Press, Princeton, NJ, 2020). [Google Scholar]
- 28.Krannich R. S., Gentry B., Luloff A., Robertson P., “Resource dependency in rural America: Continuities and change” in Rural America in a Globalizing World, Bailey C., Jensen L., Ransom E., Eds. (West Virginia University Press, Morgantown, WV, 2014), pp. 208–225. [Google Scholar]
- 29.Mueller J. T., Definining Dependence: The Natural Resource Community Typology. Rural Sociol., 10.1111/ruso.12357 (2020). [DOI] [Google Scholar]
- 30.Tickamyer A. R., Sherman J., Warlick J., Rural Poverty in the United States (Columbia University Press, New York, NY, 2017). [Google Scholar]
- 31.Cheng K. J. G., Sun Y., Monnat S. M., COVID-19 death rates are higher in rural counties with larger shares of Blacks and Hispanics. J. Rural Health 36, 602–608 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paul R., Arif A. A., Adeyemi O., Ghosh S., Han D., Progression of COVID-19 from urban to rural areas in the United States: A spatiotemporal analysis of prevalence rates. J. Rural Health 36, 591−601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Disease Control , Anxiety and Depresion Household Pulse Survey. https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm. Accessed 18 November 2020.
- 34.Bennett K. J., Yuen M., Blanco-Silva F., Geographic differences in recovery after the great recession. J. Rural Stud. 59, 111–117 (2018). [Google Scholar]
- 35.Thiede B. C., Lichter D. T., Slack T., Working, but poor: The good life in rural America? J. Rural Stud. 59, 183–193 (2018). [Google Scholar]
- 36.National Conference of State Legislatures , National unemployment monthly update. https://www.ncsl.org/research/labor-and-employment/national-employment-monthly-update.aspx. Accessed 18 November 2020.
- 37.Jensen L., Tickamyer A. R., Slack T., Rural-urban variation in informal work activities in the United States. J. Rural Stud. 68, 276–284 (2019). [Google Scholar]
- 38.Bartik A. W., et al. , The impact of COVID-19 on small business outcomes and expectations. Proc. Natl. Acad. Sci. U.S.A. 117, 17656–17666 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Federal Reserve Bank of St. Louis , Insured Unemployment Rate [IURNSA]. https://fred.stlouisfed.org/graph/?g=x6r3. Accessed 18 November 2020.
- 40.Fuhrer J. C., What role does consumer sentiment play in the US macroeconomy? N. Engl. Econ. Rev., 32–44 (1993). [Google Scholar]
- 41.Curtin R., July 2020. survey results. Survey of Consumers: University of Michigan. https://data.sca.isr.umich.edu/fetchdoc.php?docid=65773. Accessed 18 November 2020.
- 42.Organisation for Economic Cooperation and Development, Main Economic Indicators 2020, Issue 8 (2020) 10.1787/ab8aaf4f-en. [DOI] [Google Scholar]
- 43.Brown D. L., Schafft K. A., Rural People and Communities in the 21st Century: Resilience and Transformation (Polity Press, Medford, MA, ed. 2, 2019). [Google Scholar]
- 44.Office of Management and Budget , 2010 Standard for Delineating Metropolitan and Micropolitan Statistical Areas; Notice (Tech. Rep. Number 123, Executive Office of the President of the United States, 2010).
- 45.Vehovar V., Toepoel V., Steinmetz S., “Non-probability sampling” in The Sage Handbook of Survey Methods, Wolf C., Joye D., Smith T., Fo Y., Eds. (Sage, Thousand Oaks, CA, 2016), pp. 329–345. [Google Scholar]
- 46.The American Association for Public Opinion Research , Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. American Association for Public Opinion Research (American Association for Pulbic Opinion Research, ed. 9, 2016). [Google Scholar]
- 47.Stedman R. C., Connelly N. A., Heberlein T. A., Decker D. J., Allred S. B., The end of the (research) world as we know it? Understanding and coping with declining response rates to mail surveys. Soc. Nat. Resour. 32, 1139–1154 (2019). [Google Scholar]
- 48.Piltch-Loeb R., Merdjanoff A. A., Bhanja A., Abramson D. M., Support for vector control strategies in the United States during the Zika outbreak in 2016: The role of risk perception, knowledge, and confidence in government. Prev. Med. 119, 52–57 (2019). [DOI] [PubMed] [Google Scholar]
- 49.Kulas J. T., Robinson D. H., Smith J. A., Kellar D. Z., Post‐stratification weighting in organizational surveys: A cross‐disciplinary tutorial. Hum. Resour. Manage. 57, 419–436 (2018). [Google Scholar]
- 50.Cumming G., Inference by eye: Reading the overlap of independent confidence intervals. Stat. Med. 28, 205–220 (2009). [DOI] [PubMed] [Google Scholar]
- 51.Manson S., Schroeder J., Riper D. V., Kugler T., Ruggles S. IPUMS national historical geographic information system: Version 15.0 [dataset]. 10.18128/D050.V15.0. Deposited 17 August 2020. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized primary survey data have been deposited in OSF (DOI:10.17605/OSF.IO/64EZG). Data used to generate Covid-19 trends in Figure 1 is publicly available and was extracted from the New York Times (20). Population data from the 2014–2018 5-y American Community Survey estimates in Table 1 is publicly available as was extracted from the National Historic Geographic Information System hosted by IPUMS (51).