Abstract
Background.
Undifferentiated embryonal cell sarcoma (UESL) of the liver is the third most common malignant liver disease of childhood presenting as a rapidly enlarging intraabdominal mass. This systematic review explores the practicality of liver transplantation as a viable option in the treatment armamentarium for locally advanced undifferentiated embryonal cell sarcoma.
Methods.
A systematic review of the literature was performed using Medline and Embase, from inception of databases to December 31, 2018. Keywords and MeSH headings used were embryonal sarcoma, mesenchymal sarcoma, and liver transplant. Reviews and manuscripts with incomplete data were excluded.
Results.
Twenty-eight patients had orthotopic liver transplantation (OLT) as a curative treatment option. The median age at presentation was 8 and 27 years in the pediatric and adult population, respectively, with a similar male to female ratio. A majority of the patients presented with abdominal pain, palpable mass, and a normal alpha-feto-protein. The median tumor size was 15 cm mainly affecting the right lobe (62%) of the liver. Eighty-two percent of the patients underwent primary OLT and 5 patients had salvage OLT. One death (3.6%) was due to initial misdiagnosis and management for hepatoblastoma. Recurrence was noted in 7.1% of the population. The median follow-up was noted to be 28.5 months. The documented survival rate post-liver transplant for UESL was 96%.
Conclusions.
Based on available data and the very positive results therein, liver transplantation is a practical and justifiable use of a scarce resource as a treatment option for locally unresectable, undifferentiated embryonal cell sarcoma. The authors propose (accepting existence of different proposals) neoadjuvant therapy before curative resection, and if not achievable, then liver transplantation followed by adjuvant chemotherapy is an option for suitable candidates. For recurrent tumors after surgical resection, adjuvant therapy with salvage liver transplantation is an option.
INTRODUCTION
Undifferentiated embryonal cell sarcoma (UESL) of the liver is the third most common malignant liver disease of childhood accounting for 9%–13% of pediatric liver malignancies.1,2 Although commonly found in children, with a peak incidence between the age group of 6–10 years,3 there are reports of its presence in the adult population4 with no sex predilection.2
It presents as a rapidly growing palpable intraabdominal mass and abdominal pain,5 occasionally associated with fever and anorexia in the more advanced cases.6 First reported by Stocker and Ishak in 1978, these tumors arise from the malignant transformation of embryonal cells of the liver.7 Because of their internal myxoid nature with cystic and solid components, they are prone to rupture on biopsies.6
Historically, the prognosis of UESL was considered to be dismal.7 With the advent of curative surgical resection or a combination of liver resection and chemotherapy, improvement in the 5-year survival was noted.2 Shi et al felt that surgical resection with or without chemotherapy was associated with better outcomes and negative surgical margin was not associated with improved survival.8
In patients where a curative resection is not attainable, liver transplantation has been attempted as an option for a better prognosis. Donor scarcity has been one of the rate-limiting factors in this option.
This systematic review and our experience explore the practicality of liver transplantation, as a viable option in the treatment armamentarium for locally advanced undifferentiated embryonal cell sarcoma.
MATERIALS AND METHODS
Study Design and Search Strategies
The systematic review was structured on the methodology of the Cochrane systematic review protocol9 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for data reporting.10
A comprehensive and extensive computerized search of the English literature using the OVID search engine11 was performed.
The Medical Subject Headings (MeSH) headings used were “embryonal sarcoma,” “mesenchymal sarcoma,” and “liver transplant.” The headings were truncated to broaden the search and combined with Boolean operators to focus and connect the MeSH headings.
Eligibility Criteria
The PICO structure was used within the research question when the selection criteria were performed.12 All studies mentioning the use of liver transplant in the treatment of embryonal cell sarcoma were examined.
Observational reports, multicenter reports, single-center series, case reports, and case series were involved. No randomized control studies were found to have been performed on this topic.
Studies were limited to manuscripts in the English language and pertaining to human beings. Reviews and manuscripts containing incomplete data for the study were excluded
Information Sources
The bibliographic databases searched were Excerpta Medica database (EMBASE) and Ovid MEDLINE. The time frames for the respective bibliographic databases were from inception of the databases till December 31, 2018. The search string was first designed for PubMed and then translated to other databases (Figure 1).
FIGURE 1.
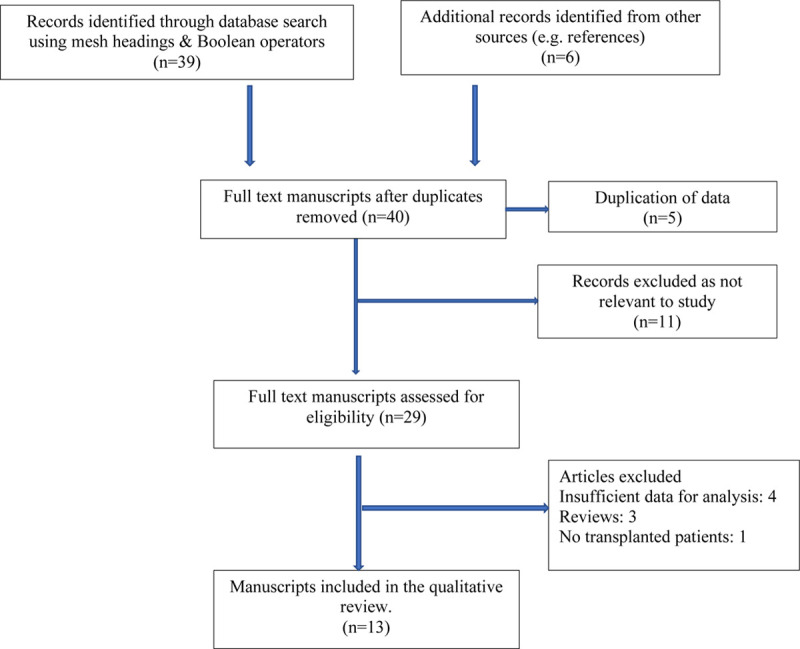
Flow chart of search strategy and exclusion criteria.
Study Selection
The bibliographic reference manager software EndNote X9.1.1 was used to manage the references emerging from the database searches.
Titles and abstracts of references were screened, and the potentially relevant references were assessed for eligibility. The full manuscripts were obtained and screened against the inclusion and exclusion criteria. Reference lists of eligible manuscripts were screened to pick missed relevant articles. If similar or follow-up results were reported in different papers especially by the same institution, the manuscript containing the complete and latest dataset was selected
Data Extraction and Analysis
A code-book was created on Microsoft Excel database. The data extracted were based on the following sections: (a) general information on the manuscript (eg, y of publication, country of origin, type of study, and time period); (b) demographics of the dataset (eg, study design, sample size and characteristics, age, and gender); (c) morphology and staging of tumor; (d) type and cycles of chemotherapy used; (d) follow-up period; and (e) retransplant and recurrence.
Data are presented as median (range) and nonparametric tests are used for comparisons unless otherwise specified.
Case Report
A retrospective review of the charts of 2 patients treated for UESL at the University of Alberta Hospital, Edmonton, Alberta, Canada, was carried out (Figure 2). The data extraction and analysis were carried out as mentioned in the previous paragraph (Table 1). This was with the approval of the Local Health Research Ethics Board and in compliance with the appropriate Health Information Act (Pro00097398). For the purpose of this review, our data has been combined with data gleaned from the manuscripts.
FIGURE 2.
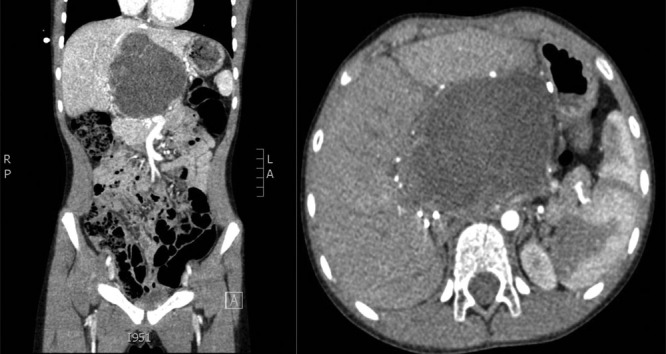
Cross-sectional imaging of UESL tumor treated at University of Alberta Hospital, Edmonton, Canada.
Table 1.
Patients with UESL treated at University of Alberta Hospital, Edmonton, Canada
| Name | sLTx | Age | Sex | Symptoms | Site | Solid/cystic component | AFP | Size (mean) | Curative resection before OLT | Postsurgery chemo | Chemo after liver surgery | Post sLTx chemo | Major complications | Follow-up period in remission (mo) | Death |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 120 | F | Distension, pain and mass | Right → left | Y | N | 15 × 7 cm | Rt trisegmentectomy | ARST 0332 protocol | VAC chemo (1 dose) | Cyclophosphamide and vinorelbine | 12 | 0 | |
| 2 | 1 | 372 | F | Recurrence after surgery | Seg: 2, 3, 4 | Y | N | 10.3 × 8.5 × 7.7 cm | Resected twice: (left lobe, segment 6) | Cyclophosphamide and vincristine | Rejection due to noncompliance | 120 | 0 |
ARST (0332 protocol), ifosfamide and doxorubicin; F, female, age in mo; N, normal; OLT, orthotopic liver transplantation; Rt, right; sLTx, salvage liver transplant; UESL, undifferentiated embryonal cell sarcoma; VAC chemo, temozolomide and irineotecan; Y, yes.
RESULTS
Demographics of Study Population
A total of 28 patients have undergone orthotopic liver transplant (OLT) for undifferentiated embryonal cell sarcoma reported in 13 articles and including our unreported experience. The manuscripts were all retrospective in nature. The time frame of the selected manuscripts was from 1981 to 2016.
The median age of pediatric patients who were transplanted for UESL was 8 years (range: 4 mo–15 y). The median age for adults (>18 y) who required liver transplant for UESL was 27 years (range: 21–54 y).
The male to female ratio of the patients undergoing OLT was similar.
Presenting Symptoms
Presenting symptoms were described in 12 patients who underwent liver transplant. The most common presenting symptoms were epigastric and right upper quadrant pain with a palpable mass.2,3,13,14 Two patients described abdominal distention as part of their presenting symptom.4 One patient presented with jaundice before transplant.15
Investigations Used
A majority of patients had a computerized tomography and MRI for diagnosis and staging. Tumor staging using the PRE-TEXT classification16 was reported in 2 patients. The tumor marker, alpha-feto-protein (AFP) was reported in 10 patients, 90% had normal or negative results. Only 1 patient was found to have a raised AFP, and this patient was initially misdiagnosed as hepatoblastoma.17
Tumor Morphology
The median diameter of the tumor on imaging was 15 cm (range: 8–25 cm).
Thirteen patients had descriptions about the site of their tumor in the liver. Eight (62%) of those patients predominantly had tumors involving the right lobe of the liver, some of which were extending in to the left lobe. Three patients had tumors originating in the left lobe. One of the patients had tumors in the hilar region of the liver and another had tumor involving the entire liver.
Characterization of the tumor was mentioned in 8 patients and all of them had a solid and cystic component. One of those patients had hemorrhaged in to the tumor. Two patients were initially diagnosed to have undifferentiated mesenchymal hamartomas but were found to have UESL in the resected specimen.18
Only 1 patient had a distant lung metastasis; this was resected before liver transplant.3
Chemotherapy
Preoperative and Postoperative Chemotherapy With Curative Resection in Patients Undergoing Salvage OLT
Four of the 6 patients who underwent curative resection had preoperative chemotherapy. This involved alkylating agents (ifosfamide, cisplatin) and anthracyclines. The median number of cycles was 9 (range: 5–10).
Similar chemotherapeutic agents were used postoperatively, and the median number of cycles was 4 (range: 2–10) (Table 2).
Table 2.
Patients undergoing salvage LTx with chemotherapy
| Author, y | Age (mo) | Preresection chemo | Preresection chemo cycles | Postresection chemo | Postsurgery chemo cycles | Presalvage liver Tx chemo | Post-LTx chemo cycles | Post-LTx chemo |
|---|---|---|---|---|---|---|---|---|
| Walther, 2014 | 84 | Vincristine, actinomycin D, ifosfamide doxorubicin | 9 | Vincristine, actinomycin, ifosfamide doxorubicin | 10 | Etoposide, carboplatinum | None | None |
| Plant A., 2013 | 156 | Cisplatin, doxorubicin | 5 | None | None | Ifosfamide, etoposide, carboplatin | 2 | Ifosfamide, carboplatin, paclitaxel |
| Castrillon GA, 2009 | 30 | NA | NA | NA | NA | NA | NA | NA |
| AHS PT 1, 2018 | 120 | Ifosfamide, doxorubicin | 10 | Ifosfamide, doxorubicin | 4 | VAC chemo temozolomide irineotecan | Cyclophosphamide vinorelbine | |
| AHS PT 2, 2005 | 372 | None | None | Cyclophosphamide, vincristine | NA | None | None | None |
LTx, liver transplant; NA, data not available; none, did not have chemotherapy.
Preoperative and Postoperative Chemotherapy in Patients Undergoing Primary OLT
The main chemotherapeutic agents are similar to the ones used in patients for salvage OLT, which include alkylating agents and anthracyclines with a median number of 4 cycles (range: 1–6) (Table 3).
Table 3.
Patients undergoing primary LTx with chemotherapy
| Author, y | Primary LTx | Age (mo) | Pre-LTx chemo | Pre-LTx chemo cycles | Post-LTx chemo cycles | Post-LTx chemo |
|---|---|---|---|---|---|---|
| Schluckebier D, 2016 | 1 | 120 | Ifosfamide, vincristine, dactinomycin | 4 | 9 | Ifosfamide, vincristine, dactinomycin |
| Shi Y, 2017 | 10 | 108 | NA | NA | NA | NA |
| Techavichit P, 2016 | 1 | 264 | Ifosfamide doxorubicin | 5 | None | None |
| Walther, 2014 | 1 | 156 | Ifosfamide doxorubicin | 6 | 4 | Vincristine, actinomycin D, cyclophosphamide |
| Walther, 2014 | 1 | 132 | Ifosfamide doxorubicin. | 5 | 1 | Ifosfamide |
| Ismail, 2013 | 1 | 4 | Cislplatin doxorubicin | 2 | NA | Cyclophosphamide, doxorubicin vincristine |
| Rohan V, 2014 | 2 | 32 | NA | NA | NA | NA |
| Chen LE, 2006 | 1 | 73 | Cisplatin, adriamycin, vincristine, Ifosfamide | 4 | None | None |
| Chen LE, 2006 | 1 | 60 | Cisplatin, adriamycin, vincristine | 1 | None | None |
| Okajima H, 2009 | 1 | 180 | Vincristine, actinomycin cyclophosphamide | Stopped early: side effects | NA | Vincristine, actinomycin, cyclophosphamide |
| Dower NA, 2000 | 1 | 72 | Ifosfamide, carboplatin, etopiside | 2 | None | None |
| Khan Z, 2017 | 1 | 252 | Ifosfamide doxorubicin | 5 | None | None |
| Dhanasekaran R, 2012 | 1 | 648 | Adriamycin ifosfamide dacarbacine | 10 mo | None | None |
LTx, liver transplant; NA, data not available; none, did not have chemotherapy.
Surgical Resection With Curative Intent, Before Liver Transplant
Five patients had surgical resection with curative intent before liver transplantation. Of the patients who underwent surgery before their OLT, 2 (including 1 of our patients) had a right trisegmentectomy.3 One patient had a right lobe resection. Another patient underwent an exploratory laparotomy and cyst drainage of a multiloculated cystic tumor.13
One of our patients had a left lobe resection. She developed recurrence 4 years later and underwent segment 4 resection. The patient developed a second recurrence in the remnant liver a further 6 years later and required a salvage OLT.
Orthotopic Liver Transplantation
Two modalities of a surgical approach have been used for patients who presented with UESL tumors. Depending on the initial presentation, primary OLT (Table 4) and salvage OLT (Table 5) have been the available options. Primary OLT was performed in patients in which the tumor was contained in the liver, but a curative resection was not a practical option because of either insufficient remnant volume or involvement/proximity to major vascular structures.1,18 Salvage liver transplant was resorted to in cases wherein the tumor was treated with chemotherapy and curative resection was achieved, but the tumor recurred.
Table 4.
Patients undergoing primary OLT
| Name, y | Age | Sex | Symptoms | Tumor site | Solid/cystic | Size of tumor | Preop chemo | P-OLT chemo | Remission period | Recurrence after OLT | Re-OLT | Death |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schluckebier D, 2016 | 120 | M | Abdominal pain | Entire | Y | NA | Y | Y | No | No | 0 | |
| Shi Y, 2017 | 108 (m) | NA | 13.7 (m) | N | N | 60 9 (m) | No | No | 0 | |||
| Techavichit P, 2016 | 264 | RUQ mass and pain | NA | Y+He | 23 | Y | N | 28 | No | No | 0 | |
| Walther 1, 2014 | 156 | F | RUQ mass and pain | Rt | NA | NA | Y | Y | 24 | No | No | 0 |
| Walther 2, 2014 | 132 | M | Pain, weight loss | Rt | Y | 17×, 12×, 14 | Y | Y | 24 | No | No | 0 |
| Ismail, 2013 | 4 | F | Abdominal pain | Rt→Lt | NA | NA | Y | Y | 8 | Yes | No | 1 |
| Rohan V | 32 | NA | NA | NA | NA | N | NA | NA | No | No | 0 | |
| Chen LE, 2006 | 73 | F | NA | NA | NA | NA | Y | N | 45 | No | No | 0 |
| Chen LE, 2006 | 60 | F | NA | NA | NA | NA | Y | N | 29 | No | No | 0 |
| Okajima H, 2009 | 180 | M | Jaundice | Hilar | NA | 15 | Y | Y | 24 | Yes | 0 | |
| Dower NA, 2000 | 72 | M | RUQ pain, anemia | Rt→ Lt | Y | 12 × 11 × 14 | Y | N | 79 | No | Yes | 0 |
| Khan Z, 2017 | 252 | M | RUQ mass and pain | Rt lobe | Y | 14 × 10 × 10 | Y | None | 18 | No | No | 0 |
| Dhanasekaran R, 2012 | 648 | M | Distension | Lt lobe | NA | 25 | Y | None | 123 | No | Yes | 0 |
Period of remission and age in mo, size of tumor in centimeter.
F, female; He, hemorrhage; Lt, left; (m), mean; M, male; N, no; NA, not available; OLT, orthotopic liver transplantation; P-OLT chemo, post-OLT chemo; Rt, right; Y, yes.
Table 5.
Patients undergoing salvage OLT
| Name | Age | Sex | Symptoms | Tumor site | Solid/cystic component | Size of tumor (mean) | Preop chemo | Curative resection before LTx | Postsurgery chemo | Donor type | Post-LTx chemo | Period in remission | Recurrence after-LTx | Death |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Walther, 2014 | 84 | M | Shoulder tip pain | Right → left | Y | 8 cm | Y | RT trisegmentectomy | Y | Cadaveric whole liver | 168 | 0 | 0 | |
| Plant A, 2013 | 156 | Right | NA | N | Y | Resection | N | NA | Y | 37 | 37 | 0 | ||
| Castrillon GA, 2009 | 30 | M | Large nontender mass | Left → rt | Y | 18 × 15 × 20 cm | None | Exploratory laparotomy and cyst drainage | N | Cadaveric whole liver | N | 12 | 0 | 0 |
| UAH 1 2018 | 120 | F | Abdo distension, pain, and mass | Rt → left | Y | 15 × 7 cm | Y | Rt trisegmentectomy | Y | Live unrelated left lateral seg | Y | 3 | 0 | 0 |
| UAH 2 2005 | 372 | F | Recurrence after surgery | Left and seg4 | Y | 10.3 × 8.5 × 7.7 cm | Left lobe → seg6 resect | Y | NA | NA | 120 | 0 | 0 |
Age, period in remission, recurrence in mo.
F, female; LTx, liver transplant; M, male; N, no; NA, not available; OLT, orthotopic liver transplant; rt, right; Y, yes.
Twenty-three patients (82%) underwent primary OLT, and five patients (18%) had salvage OLT. The type of donor liver was documented in 8 patients. Six patients received deceased donor livers, and 2 patients received live related15 and unrelated donors.
Three patients (11%) were documented to have rejection after OLT.4,19 One patient had cardiac dysfunction.18 One patient has a bile duct anastomotic leak3 and another had developed a diaphragmatic hernia.18 The majority of the patients had tacrolimus as 1 of their immunosuppressive medications.
Two patients (7.1%) required retransplant because of rejection.4,19
Pathology
All the explanted pathology was suggestive of UESL. Patients, who had description of the histology of their explanted liver, had between 90% and 100% necrosis of their tumor. These patients had undergone chemotherapy before liver transplantation.
Survival and Recurrence
The median survival was 28.5 months (range: 8–123 mo). This is influenced by the bias in the timeline of reporting. Eleven patients were documented to have survived the 5-year period.
One patient (3.6%) died after OLT.17 This particular patient was misdiagnosed as hepatoblastoma initially and had preoperative chemotherapy but did not respond and underwent an OLT.
Only 2 (7.1%) of the 28 patients had recurrence after liver transplant.1,15,17 One of the patients had recurrent hilar tumor in the transplanted liver, which was resected and treated with chemotherapy.15 The patient was disease free 18 months after resection. The other patient had a misdiagnosis of primary tumor, had an OLT, and relapsed.17
Two (7.1%) patients had to undergo retransplant for rejection.4,19
DISCUSSION
Management strategies have evolved in the treatment of locally unresectable UESL. This systematic review has examined the available literature on the use of liver transplantation as a potential treatment option in both the pediatric and adult population, wherein the tumor is unresectable and as salvage therapy in patients with recurrence.
Our systematic review along with our clinical experience has analyzed the data presently available on the utilization of OLT for the treatment of UESL. The data have been pooled based on the demographics, presenting symptoms, investigation used, tumor morphology, chemotherapy, and outcomes on liver transplantation.
Interpretation of data for the purpose of this systematic review must accept that data pooling has inherent limitations in sensitivity, clinical heterogeneity, and publication bias. Nevertheless, this is the largest reported series of patients treated with OLT for this rare tumor.
A total of 28 patients had liver transplantation as a curative treatment option. The median age at presentation of the tumor was 8 and 27 years in the pediatric and the adult population, respectively, with a similar male to female ratio. The majority of the patients presented with upper abdominal pain and a palpable mass. A majority of the patients had a normal AFP, and the median tumor size was 15 cm mainly affecting the right lobe of the liver (62%).
Eighty-two percent (23) of the patients underwent primary OLT, and 5 patients (18%) had salvage OLT.
One death (3.6%) was noted because of an initial misdiagnosis and management for hepatoblastoma. Recurrence was noted in 7.1% of the population, and retransplantation was required for 2 patients with rejection. All the patients were alive till the point of publication of the respective articles except for 1 patient, and the median recorded survival was noted to be 28.5 months. The documented survival rate postliver transplant for UESL was 96%.
From our review, a standardized chemotherapeutic regimen was not used universally for UESL.
In conclusion, based on the available data, and the very positive results therein, liver transplantation is a practical and justifiable use of a scarce resource as a treatment option for locally unresectable, undifferentiated embryonal cell sarcoma. The authors propose (accepting existence of different proposals) neoadjuvant therapy before curative resection, and if not achievable, then liver transplantation followed by adjuvant chemotherapy is an option for suitable candidates.” For recurrent tumors after surgical resection, adjuvant therapy with salvage liver transplantation is an option.
Footnotes
Published online 15 January, 2021.
The authors declare no funding and conflicts of interest.
B.I.B. and N.M.K. participated in review design. B.I.B., N.M.K., D.L.B., A.M.J.S., K.Z.D., and S.M.G. participated in the writing of the article. B.I.B. participated in the performance of the review. B.I.B. participated in data analysis.
REFERENCES
- 1.Plant AS, Busuttil RW, Rana A, et al. A single-institution retrospective cases series of childhood undifferentiated embryonal liver sarcoma (UELS): success of combined therapy and the use of orthotopic liver transplant. J Pediatr Hematol Oncol. 2013; 35:451–455 [DOI] [PubMed] [Google Scholar]
- 2.Techavichit P, Masand PM, Himes RW, et al. Undifferentiated embryonal sarcoma of the liver (UESL): a single-center experience and review of the literature. J Pediatr Hematol Oncol. 2016; 38:261–268 [DOI] [PubMed] [Google Scholar]
- 3.Walther A, Geller J, Coots A, et al. Multimodal therapy including liver transplantation for hepatic undifferentiated embryonal sarcoma. Liver Transpl. 2014; 20:191–199 [DOI] [PubMed] [Google Scholar]
- 4.Dhanasekaran R, Hemming A, Salazar E, et al. Rare case of adult undifferentiated (embryonal) sarcoma of the liver treated with liver transplantation: excellent long-term survival. Case Reports Hepatol. 2012; 2012:519741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walterhouse DO, Cohn SL. Diagnostic and Therapeutic Advances in Pediatric Oncology. 1997, Kluwer Academic Publishers [Google Scholar]
- 6.Aronson DC, Meyers RL. Malignant tumors of the liver in children. Semin Pediatr Surg. 2016; 25:265–275 [DOI] [PubMed] [Google Scholar]
- 7.Stocker JT, Ishak KG. Undifferentiated (embryonal) sarcoma of the liver: report of 31 cases. Cancer. 1978; 42:336–348 [DOI] [PubMed] [Google Scholar]
- 8.Shi Y, Rojas Y, Zhang W, et al. Characteristics and outcomes in children with undifferentiated embryonal sarcoma of the liver: a report from the National Cancer Database. Pediatr Blood Cancer. 2017; 64:e26272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Briscoe S. A review of the reporting of web searching to identify studies for cochrane systematic reviews. Res Synth Methods. 2018; 9:89–99 [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gall C, Brahmi FA. Retrieval comparison of EndNote to search MEDLINE (Ovid and PubMed) versus searching them directly. Med Ref Serv Q. 2004; 23:25–32 [DOI] [PubMed] [Google Scholar]
- 12.Wallace BC, Kuiper J, Sharma A, et al. Extracting PICO sentences from clinical trial reports using supervised distant supervision. J Mach Learn Res. 2016; 17:132. [PMC free article] [PubMed] [Google Scholar]
- 13.Castrillon GA, Sepúlveda E, Yepez NL, et al. Hepatic transplantation in a child with giant multicystic tumor: pathological and imaging findings. Pediatr Transplant. 2010; 14:e58–e61 [DOI] [PubMed] [Google Scholar]
- 14.Khan ZH, Ilyas K, Khan HH, et al. Unresectable undifferentiated embryonal sarcoma of the liver in an adult male treated with chemotherapy and orthotopic liver transplantation. Cureus. 2017; 9:e1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okajima H, Ohya Y, Lee KJ, et al. Management of undifferentiated sarcoma of the liver including living donor liver transplantation as a backup procedure. J Pediatr Surg. 2009; 44:e33–e38 [DOI] [PubMed] [Google Scholar]
- 16.MacKinlay GA, Pritchard J. A common language for childhood liver tumors. Pediatr Surg Int. 1992; 7:325–326 [Google Scholar]
- 17.Ismail H, Dembowska-Bagińska B, Broniszczak D, et al. Treatment of undifferentiated embryonal sarcoma of the liver in children–single center experience. J Pediatr Surg. 2013; 48:2202–2206 [DOI] [PubMed] [Google Scholar]
- 18.Chen LE, Shepherd RW, Nadler ML, et al. Liver transplantation and chemotherapy in children with unresectable primary hepatic malignancies: development of a management algorithm. J Pediatr Gastroenterol Nutr. 2006; 43:487–493 [DOI] [PubMed] [Google Scholar]
- 19.Dower NA, Smith LJ, Lees G, et al. Experience with aggressive therapy in three children with unresectable malignant liver tumors. Med Pediatr Oncol. 2000; 34:132–135 [DOI] [PubMed] [Google Scholar]


