Abstract
Background:
Minimal change nephropathy (MCD) is a common pathological type of nephrotic syndrome and is often associated with acute kidney injury (AKI). This study aimed to investigate the clinical characteristics and related factors of AKI in patients with MCD and nephrotic syndrome.
Methods:
Patients from Chinese People's Liberation Army General Hospital who were diagnosed with pathological renal MCD with clinical manifestations of nephrotic syndrome were included from January 1, 2013 to December 31, 2017. Patients diagnosed with membranous nephropathy (MN) by renal biopsy from January 1, 2013 to December 31, 2017 are included as a control population. We retrospectively analyzed the clinical and pathological characteristics of patients as well as the percentages and clinical characteristics of AKI in different age groups. We assessed the correlation of pathological characteristics with serum creatinine using multivariate linear regression analysis.
Results:
A total of 367 patients with MCD were included in the analysis, with a sex ratio of 1.46: 1 (male: female) and an age range of 6 to 77 years. Among all the patients, 109 developed AKI (29.7%), and of these patients, 85 were male (78.0%). In the 586 patients with MN, 27 (4.6%) patients developed AKI. The percentage of AKI in MCD patients was significantly higher than that in MN patients (χ2 = 41.063, P < 0.001). The percentage of AKI increased with age in the MCD patients. The percentage of AKI in patients aged 50 years or older was 52.9% (46/87), which was significantly higher than that [22.5% (63/280)] in patients under 50 years (χ2 = 6.347, P = 0.013). We observed statistically significant differences in age (43 [27, 59] years vs. 28 [20, 44] years, Z = 5.487, P < 0.001), male (78.0% vs. 51.4%, χ2 = 22.470, P < 0.001), serum albumin (19.9 ± 6.1 g/L vs. 21.5 ± 5.7 g/L, t = 2.376, P = 0.018), serum creatinine (129.5 [105.7, 171.1] μmol/L vs. 69.7 [57.7, 81.9] μmol/L, Z = 14.190, P < 0.001), serum urea (10.1 [6.2, 15.8] mmol/L vs. 4.7 [3.6, 6.4] mmol/L, Z = 10.545, P < 0.001), IgE (266.0 [86.7, 963.0] IU/ml vs. 142.0 [35.3, 516.5] IU/ml, Z = 2.742, P = 0.007), history of diabetes (6.4% vs. 1.2%, P = 0.009), and history of hypertension (23.9% vs. 5.1%, χ2 = 28.238, P < 0.001) between the AKI group and the non-AKI group. According to multivariate linear regression analysis, among the renal pathological features analyzed, renal tubular epithelial cell damage (β = 178.010, 95% CI: 147.888−208.132, P < 0.001) and renal interstitial edema (β = 28.833, 95% CI: 11.966−45.700, P = 0.001) correlated with serum creatinine values.
Conclusions:
The percentage of AKI in MCD patients is significantly higher than that in MN patients. Patients over 50 years old are more likely to develop AKI. Renal tubular epithelial cell injury and renal interstitial edema may be the main pathological lesions that are associated with elevated serum creatinine in patients with MCD.
Keywords: Minimal change disease, Nephrotic syndrome, Acute kidney injury
Introduction
Minimal change disease (MCD) is a common pathology that leads to nephrotic syndrome. It has been reported that 70% to 90% of children with nephrotic syndrome present with pathological features of MCD,[1] and MCD accounts for approximately 10.9% to 38.5% of the cases of nephrotic syndrome in adults.[2,3] Although the incidence of MCD gradually decreases with age, it is still a common cause of nephrotic syndrome in elderly patients.[4] Acute kidney injury (AKI) is a common complication of nephrotic syndrome. AKI leads to prolonged remission of MCD.[5] Severe AKI would even render patients in need of renal replacement therapy, or lead to transformation into chronic renal insufficiency due to an incomplete recovery. The mechanism and risk factors for AKI in MCD are not completely clear. In this study, we aimed to analyze the clinical data of MCD, and summarize the clinical characteristics of MCD and AKI.
Methods
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of Chinese People's Liberation Army General Hospital (No. S2020-364-01) and the requirement for informed consent was waived.
Study population
A retrospective, cross-sectional study was performed on 407 patients with clinical manifestations of nephrotic syndrome, who were diagnosed with MCD by renal biopsy from January 1, 2013 to December 31, 2017 at Chinese People's Liberation Army General Hospital. A total of 367 patients were included in the analysis. Seventeen patients were excluded for not meeting the diagnostic criteria for nephrotic syndrome, or because they had reached remission at admission, and 23 patients were excluded for incomplete clinical data [Figure 1]. The inclusion criteria were as follows: (1) clinical manifestations of nephrotic syndrome, which is diagnosed if the 24-hour urine protein quantification is >3.5 g/d, and the plasma albumin is <30 g/L; (2) no obvious or slight changes in glomeruli under light microscopy, no specific immune complex deposition in immunofluorescence, and pathologically diagnosed as MCD. The exclusion criteria were as follows: (1) failure to meet the diagnostic criteria for nephrotic syndrome or remission of nephrotic syndrome at admission, (2) concomitant with other diseases that may damage the kidney, such as tumors, connective tissue disease, and hematological diseases, and (3) incomplete clinical data.
Figure 1.
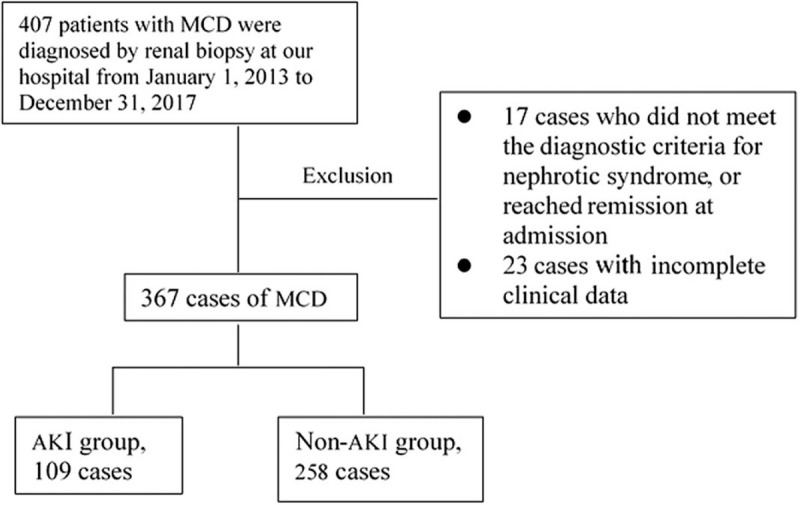
Selection of patients for AKI occurrence analysis from the MCD patients. AKI: Acute kidney injury; MCD: Minimal change disease.
In addition, we included 586 patients diagnosed with membranous nephropathy (MN) by renal biopsy and meeting the diagnostic criteria for nephrotic syndrome from January 1, 2013 to December 31, 2017 as a control population. The inclusion criteria were as follows: (1) clinical manifestations of nephrotic syndrome, which is diagnosed if the 24-hour urine protein quantification is >3.5 g/d, and the plasma albumin is <30 g/L; (2) diffuse thickening of glomerular basement membrane, fine grainy deposition of immunoglobulin G (IgG) and C3 along the glomerular capillary wall under immunofluorescent staining, pathologically diagnosed as MN.
AKI was defined according to the Kidney Disease Improving Global Outcomes (KDIGO) criteria.[6] In this study, AKI can be diagnosed as follows: (1) serum creatinine increased to ≥1.5 times baseline; (2) serum creatinine increase >0.3 mg/dL (26.5 μmol/L) within 48 h; (3) urinary output <0.5 ml·kg−1·h−1 during a 6-h block.
Clinical data collection
Clinical data were collected from patients with MCD at the time of renal biopsy, including age, sex, previous medical history (diabetes and hypertension history), 24-hour urine protein quantification, hemoglobin, C-reactive protein (CRP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ-glutamyl transpeptidase (γ-GT), serum total protein, serum albumin, serum creatinine, serum urea, and immunoglobulin E (IgE). Pathological data from the renal biopsies of all patients were collected: (1) renal tubular lesions: renal tubular epithelial granules or vacuole-like degeneration, cell shedding, epithelial cell regeneration and rearrangement, tubular atrophy, protein casts; (2) renal interstitial lesion: inflammatory cell infiltration, interstitial fibrosis, and renal interstitial edema; and (3) renal arteriolar lesions: renal intimal thickening and vitreous degeneration. Indexes of renal tubular lesions and renal interstitial lesions are divided into four levels according to the proportion of the area of the cortex occupied by the lesions: none (0%), mild (1%–25%), moderate (26%–50%), and severe (>50%), with scores of 0, 1, 2, and 3, respectively. Renal arteriolar lesions: intimal thickening of the renal arterioles is indicated if the thickness of the intima is greater than the thickness of the media, and hyaline degeneration is defined as the uniform pinkish deposit of the intima of the vessel wall under periodic acid-Schiff (PAS) staining. Renal arteriolar intimal thickening and hyaline degeneration were scored as 0 and 1 according to absence and presence, respectively. And then these scores were added up to obtain the total pathological score. The cross-sectional data of patients were retrospectively analyzed, and patients were divided into an AKI group and a non-AKI group for comparison. Clinical data of MN group including age, gender, and AKI percentage were collected.
Statistical analysis
In this study, SPSS Statistics v22.0 (IBM Corporation, Armonk, NY, USA) was used for statistical analysis. Continuous variables with normal distribution were expressed as mean ± standard deviation and analyzed using Student's t-test. The nonnormally distributed continuous variables were expressed as median (Q1, Q3) and analyzed using Wilcoxon rank-sum test. Categorical variables were presented as numbers of cases (%), and Chi-squared test or Fisher exact test was used for analysis. The correlations between renal pathological changes and elevated serum creatinine were analyzed with Spearman's correlation and multivariate linear regression analysis. P < 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 367 patients with MCD and 586 patients with MN were included in the analysis. Among the patients with MCD included, 218 were male and 149 were female. The male-to-female ratio was 1.46:1, and the age range was 6 to 77 years old. AKI occurred in 109 (29.7%) out of 367 patients, among whom 85 were male (78.0%) and 24 were female (22.0%). The characteristics of the 586 patients with MN were as follows: gender ratio 1.82:1 (male 378, female 208), age 15 to 83 years old, and AKI accounting for 4.6% (27/586). The percentage of AKI in MCD patients was significantly higher than that in MN patients (χ2 = 41.063, P < 0.001) [Table 1].
Table 1.
Demographic characteristics and percentages of AKI in MCD and MN patients.
| Characteristics | MCD (n = 367) | MN (n = 586) | Statistical values | P |
| Age (years), median (Q1, Q3) | 33 (21, 48) | 51 (31, 69) | 7.674∗ | 0.056 |
| Male, n (%) | 218 (59.4) | 378 (64.5) | 0.157† | 0.876 |
| AKI, n (%) | 109 (29.7) | 27 (4.6) | 41.063† | < 0.001 |
Z values.
χ2 values.
AKI: Acute kidney injury; MCD: Minimal change disease; MN: Membranous nephropathy.
There were 39 patients (10.6%) with hypertension and 10 patients (2.7%) with diabetes in patients with MCD. In addition, we noticed that elevated liver enzymes were recorded in MCD patients, with an increased ALT of >40 U/L in 65 patients (17.7%), increased AST of >40 U/L in 38 patients (10.4%), and increased γ-GT of >50 U/L in 70 patients (19.1%). We also observed an increased serum IgE of over 100 IU/mL in 212 patients (57.8%) in our study.
Percentage of AKI by age in the MCD patients
To determine whether age affects the complications of AKI in MCD patients, we divided patients with MCD into eight subgroups by age. The proportional distribution of AKI complications within each subgroup was presented in Table 2. The percentage of AKI was 22.5% (63/280) in MCD patients under 50 years of age, and 52.9% (46/87) in MCD patients aged 50 years and older. The percentage of AKI in patients aged 50 years and older was significantly higher than that in patients under 50 years old (χ2 = 6.347, P = 0.013). These results suggested that the percentage of AKI increased with age in the MCD patients and was especially high in patients aged 50 years and older.
Table 2.
Percentages of AKI complications within each age subgroup of patients with nephrotic syndrome and minimal change disease (n = 367).
| Age (years) | MCD | MCD+AKI | Percentage (%) |
| 1–9 | 5 | 0 | 0 |
| 10–19 | 66 | 8 | 12.1 |
| 20–29 | 92 | 22 | 23.9 |
| 30–39 | 54 | 15 | 27.8 |
| 40–49 | 63 | 18 | 28.6 |
| 50–59 | 46 | 24 | 52.2 |
| 60–69 | 32 | 16 | 50.0 |
| 70–79 | 9 | 6 | 66.7 |
AKI: Acute kidney injury; MCD: Minimal change disease.
Clinical data of AKI and non-AKI groups in the MCD patients
There were no significant differences in ALT, AST, γ-GT, total protein, 24-h urine protein, chronic renal interstitial injury and intrarenal arteriosclerosis between patients complicated with AKI (AKI group) and patients who were not complicated with AKI (non-AKI group) (all P > 0.05). Patients in the AKI group were significantly older (43 [27, 59] years vs. 28 [20, 44] years, Z = 5.487, P < 0.001), had significantly lower serum albumin (19.9 ± 6.1 g/L vs. 21.5 ± 5.7 g/L, t = 2.376, P = 0.018), and higher serum creatinine (129.5 [105.7, 171.1] μmol/L vs. 69.7 [57.7, 81.9] μmol/L, Z = 14.190, P < 0.001), serum urea (10.1 [6.2, 15.8] mmol/L vs. 4.7 [3.6, 6.4] mmol/L, Z = 10.545, P < 0.001), and IgE (266.0 [86.7, 963.0] IU/mL vs. 142.0 [35.3, 516.5] IU/mL, Z = 2.742, P = 0.007), and were more likely to be male (78.0% vs. 51.4%, χ2 = 22.470, P < 0.001) and have a history of diabetes (6.4% vs. 1.2%, P = 0.009) and hypertension (23.9% vs. 5.1%, χ2 = 28.238, P < 0.001) as compared with non-AKI group [Table 3].
Table 3.
Clinical data of non-AKI and AKI subgroups in the MCD patients.
| Items | Non-AKI(n = 257) | AKI(n = 109) | Statistical values | P |
| Age (years), median (Q1, Q3) | 28 (20, 44) | 43 (27, 59) | 5.487∗ | <0.001 |
| Male, n (%) | 132 (51.4) | 85 (78.0) | 22.470† | <0.001 |
| Alanine aminotransferase (U/L), median (Q1, Q3) | 19.0 (13.2, 34.0) | 18.7 (12.3, 32.6) | 0.380∗ | 0.704 |
| Aspartate aminotransferase (U/L), median (Q1, Q3) | 19.2 (15.0, 26.0) | 19.3 (14.7, 31.5) | 1.058∗ | 0.290 |
| γ-glutamyl transpeptidase (U/L), median (Q1, Q3) | 25.5 (16.2, 39.1) | 29.2 (18.7, 52.5) | 1.294∗ | 0.122 |
| Serum creatinine (μmol/L), median (Q1, Q3) | 69.7 (57.7, 81.9) | 129.5 (105.7, 171.1) | 14.190∗ | <0.001 |
| Serum urea (mmol/L), median (Q1, Q3) | 4.7 (3.6, 6.4) | 10.1 (6.2, 15.8) | 10.545∗ | <0.001 |
| Total protein (g/L), mean ± SD | 46.2 ± 4.7 | 43.6 ± 8.7 | 0.848‡ | 0.397 |
| Serum albumin (g/L), mean ± SD | 21.5 ± 5.7 | 19.9 ± 6.1 | 2.376‡ | 0.018 |
| 24 h urine protein (g/d), mean ± SD | 5.6 (4.4, 8.1) | 5.9 (4.6, 8.4) | 1.236‡ | 0.216 |
| Immunoglobulin E (IU/mL), median (Q1, Q3) | 142.0 (35.3, 516.5) | 266.0 (86.7, 963.0) | 2.742∗ | 0.007 |
| History of diabetes, n (%) | 3 (1.2) | 7 (6.4) | – | 0.009 |
| History of hypertension, n (%) | 13 (5.1) | 26 (23.9) | 28.238† | <0.001 |
| Chronic renal interstitial lesion, n (%) | 7 (2.7) | 5 (4.6) | – | 0.268 |
| Intrarenal arteriosclerosis, n (%) | 4 (1.6) | 3 (2.8) | – | 0.347 |
Z values.
χ2 values.
t values.
AKI: Acute kidney injury; MCD: Minimal change disease; SD: Standard deviation; -: Not available.
Renal pathological characteristics and correlation with AKI complications in the MCD patients
To determine the key renal pathological features and their correlations with AKI complications in the MCD patients, we obtained the renal pathological results and analyzed their correlations with AKI complications that occurred in the patients. The key pathological features and their proportional distribution were as follows: renal tubular atrophy (139/367, 37.9%), protein casts (187/367, 51.0%), renal tubular epithelial cell damage (including granules or vacuole-like degeneration and shedding) (334/367, 91.0%), interstitial edema (133/367, 36.2%), renal interstitial inflammatory cell infiltration (158/367, 43.1%), renal interstitial fibrosis (163/367, 44.4%), renal intimal thickening (97/367, 26.4%), and hyalinization (34/367, 9.3%).
Among all MCD patients, 12 were identified with chronic renal tubular interstitial damage by renal pathological examination. To avoid the impact of chronic tubulointerstitial fibrosis on the results of the analysis, these 12 patients were excluded. The renal pathological features of the remaining 355 patients were scored according to the pathological scoring method described in the Methods section. Spearman correlation analysis results showed that each pathological injury score and the total pathological score were significantly correlated with the serum creatinine values except renal arteriolar intimal thickening [Table 4].
Table 4.
Spearman correlation analysis of pathological changes and serum creatinine.
| Pathological injury | Correlation coefficient | P |
| Tubular atrophy | 0.210 | 0.038 |
| Protein casts | 0.248 | 0.005 |
| Tubular epithelial cell injury | 0.319 | <0.001 |
| Interstitial edema | 0.300 | <0.001 |
| Inflammatory cell infiltration | 0.310 | <0.001 |
| Interstitial fibrosis | 0.309 | <0.001 |
| Renal arteriolar intimal thickening | 0.158 | 0.178 |
| Renal arteriolar hyalinization | 0.319 | <0.001 |
| Pathological score | 0.289 | <0.001 |
Next, we performed multivariate linear regression analysis of the characterized key pathological injury features with their corresponding serum creatinine values. The results demonstrated that renal tubular epithelial cell damage (β = 178.010, 95% CI: 147.888−208.132, P < 0.001) and interstitial edema (β = 28.833, 95% CI: 11.966−45.700, P = 0.001) were significantly associated with the serum creatinine values, and were the main pathological injuries leading to decreased renal function.
Discussion
MCD, a common pathological type of nephrotic syndrome, is generally sensitive to glucocorticoids. However, there remains some patients who are under the great risk of developing AKI.[1] Although the majority of these patients could recover and regain normal renal function after AKI, some patients develop chronic renal insufficiency or even turn to long-term renal replacement therapy. Besides, AKI delays the remission of nephrotic syndrome of MCD.[5,7,8] The mechanism and risk factors for AKI in MCD are currently uncertain, and the results in previous reports are inconsistent. Some studies have shown that AKI with MCD nephrotic syndrome may be associated with excessive leakage of urinary protein, decreased serum albumin, increased age and hypertension.[9–12] And other studies have suggested that factors including sepsis, deep vein thrombosis, nonsteroidal anti-inflammatory drugs (NSAIDs) or contrast agents were also related.[13] To our surprise, there were still some patients who would develop AKI even without these risk factors in clinical practice. Therefore, we performed this retrospective study to analyze patients who were diagnosed with MCD by renal biopsy in our hospital. Meanwhile, patients diagnosed with MN by renal biopsy were also included as a control group.
The results showed that the percentage of AKI was significantly higher in MCD patients than that in MN patients, which indicates a higher possibility of MCD patients to develop AKI. In addition, the results showed that the percentage of male was higher in MCD patients and the percentage of AKI was also significantly higher in men than in women. Maas et al[14] also found that males with MCD are more prone to AKI, and the reason is unclear. Our study found that the incidence of AKI gradually increased with age, which is consistent with the previous study.[14] Particularly, the percentage of AKI in patients aged 50 or older was significantly higher than that in patients under 50 years old. These results suggested that the patients aged 50 or older are more predisposed to AKI. Aging can result in the macro- and microstructure changes of kidney, causing glomerular filtration rate (GFR) decrease and rendering kidney more vulnerable to acute stressors.[15] This may be an underlying reason why AKI is more likely to occur in patients aged 50 years or older.
What's more, we also found that some patients with MCD had elevated AST, ALT, and γ-GT, but there was no significant difference between the AKI group and the non-AKI group, indicating that the elevation in transaminase might not be correlated with the occurrence of AKI. To our knowledge, elevated transaminase has not been reported in MCD patients. In this study, these patients with MCD who had elevated transaminase levels had no previous history of hepatitis or fatty liver. The cause of the elevated transaminase was unclear. The transaminase levels in these patients were often observed to return to normal level with the remission of nephrotic syndrome. Additionally, elevated IgE in the serum of MCD patients was also reported in this study (57.8%), which is similar to a previous study,[16] and there was a significant difference between the AKI group and the non-AKI group. Elevated IgE levels in MCD may reflect the activation of B cells and T cells. Studies have shown that MCD patients experience a major persistent T helper cell type 2 (Th2) immune response. Thus, MCD may be a representation of Th2-dependent glomerular disease. During nephrotic syndrome relapse, this disease is often associated with elevated IgE levels, allergies, elevated levels of interleukin 4 (IL-4) in peripheral T cells, and secretion of interleukin 13 (IL-13). IL-13 regulates immunoglobulin isotype switching towards IgE.[17]
This study collected the renal pathological data from 367 MCD patients. 91.0% of these patients demonstrated renal tubular epithelial cell damage (including granular or vacuolar degeneration and shedding). Renal tubular atrophy, protein casts, renal interstitial edema, renal interstitial inflammatory cell infiltration, renal interstitial fibrosis, renal intimal thickening and hyaline degeneration were also observed. The multiple linear regression analysis indicated that renal tubular epithelial cell injury and renal interstitial edema were found to be closely related to the serum creatinine values, suggesting that renal tubular epithelial cell injury and renal interstitial edema may be the main pathological lesions leading to AKI. Some studies suggested that the renal ischemia is present in most cases of severe AKI, especially in aged and/or hypertensive patients with nephrosclerosis or microvascular lesions that reduce the afferent arteriolar blood supply to the glomerular tuft.[18] Renal ischemia may result from renal tubular epithelial cell injury, but the mechanism of ischemia remains elusive.
The results of this study showed that patients with AKI had significantly lower albumin than those without AKI, while there was no significant difference in 24-hour urinary protein between these two groups. Previous studies have reported that AKI is associated with lower serum albumin, which can lead to fluid retention in the third interstitial space, insufficient effective circulating blood volume, and AKI.[19] Elevated serum albumin levels may reduce the occurrence of AKI by both increasing plasma osmotic pressure and effective circulating blood volume. However, there are also reports pointing out that there are no decrease in circulating blood volume and renal plasma flow of most patients with MCD. The patients demonstrated variant responses to albumin infusion, and some patients have unchanged or even reduced GFR.[20] These conflicting results suggest that further research is needed to determine whether lower serum albumin is associated with AKI. Lower serum albumin in MCD patients is mainly due to a large amount of proteinuria leakage. In addition to proteinuria leakage, serum albumin levels are also related to patients’ nutritional intake and protein synthesis in liver. In this study, there was no significant difference in 24-h urine protein quantification between the AKI group and the non-AKI group, but the serum albumin level was lower in AKI group, suggesting that there may be other factors affecting the serum albumin level.
However, there are also some limitations in our study. This study is a retrospective study and only based on cross-sectional data. Patients were included according to predefined clinical and histological criteria. Furthermore, patients were all from a single center. Therefore, a prospective multi-center study is certainly required to further validate our conclusion.
In summary, patients with MCD have a greater possibility to develop AKI than patients with MN. Male or older patients are more prone to AKI. Renal tubular epithelial cell damage and renal interstitial edema may be the major pathological injuries that lead to AKI.
Funding
This work was supported by the grants from the National Key Research and Development Program of China (No. 2016YFC0906202), the Natural Science Foundation of Hainan Province (No. 20158332), and Sanya Technology Innovation Fund (No. 2014YW33).
Conflicts of interest
None.
Footnotes
How to cite this article: Lin SP, Zhu FG, Meng JL, Sun XW, Cui J, Liang S, Yin Z, Sun XF, Cai GY. Clinical features of acute kidney injury in patients with nephrotic syndrome and minimal change disease: a retrospective, cross-sectional study. Chin Med J 2021;134:206–211. doi: 10.1097/CM9.0000000000001218
References
- 1.Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal change disease. Clin J Am Soc Nephrol 2017; 12:332–345. doi: 10.2215/CJN.05000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imtiaz S, Drohlia MF, Nasir K, Salman B, Ahmad A. Analysis of renal diseases detected in renal biopsies of adult patients: a single-center experience. Saudi J Kidney Dis Transpl 2017; 28:368–378. doi: 10.4103/1319-2442.202788. [DOI] [PubMed] [Google Scholar]
- 3.Chang JH, Kim DK, Kim HW, Park SY, Yoo TH, Kim BS, et al. Changing prevalence of glomerular diseases in Korean adults: a review of 20 years of experience. Nephrol Dial Transplant 2009; 24:2406–2410. doi: 10.1093/ndt/gfp091. [DOI] [PubMed] [Google Scholar]
- 4.Haas M, Spargo BH, Wit EJ, Meehan SM. Etiologies and outcome of acute renal insufficiency in older adults: a renal biopsy study of 259 cases. Am J Kidney Dis 2000; 35:433–447. doi: 10.1016/s0272-6386(00)70196-x. [DOI] [PubMed] [Google Scholar]
- 5.Komukai D, Hasegawa T, Kaneshima N, Takayasu M, Sato Y, Hirose M, et al. Influence of acute kidney injury on the time to complete remission in adult minimal change nephrotic syndrome: a single-centre study. Nephrology (Carlton) 2016; 21:887–892. doi: 10.1111/nep.12678. [DOI] [PubMed] [Google Scholar]
- 6.Fliser D, Laville M, Covic A, Fouque D, Vanholder R, et al. Ad-hoc working group of ERBP. A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol Dial Transplant 2012; 27:4263–4272. doi: 10.1093/ndt/gfs375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen T, Lv Y, Lin F, Zhu J. Acute kidney injury in adult idiopathic nephrotic syndrome. Ren Fail 2011; 33:144–149. doi: 10.3109/0886022X.2011.553301. [DOI] [PubMed] [Google Scholar]
- 8.Fujigaki Y, Tamura Y, Nagura M, Arai S, Ota T, Shibata S, et al. Unique proximal tubular cell injury and the development of acute kidney injury in adult patients with minimal change nephrotic syndrome. BMC Nephrol 2017; 18:339.doi: 10.1186/s12882-017-07∗56-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waldman M, Crew RJ, Valeri A, Busch J, Stokes B, Markowitz G, et al. Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol 2007; 2:445–453. doi: 10.2215/CJN.03531006. [DOI] [PubMed] [Google Scholar]
- 10.Jennette JC, Falk RJ. Adult minimal change glomerulopathy with acute renal failure. Am J Kidney Dis 1990; 16:432–437. doi: 10.1016/s0272-6386(12)80055-2. [DOI] [PubMed] [Google Scholar]
- 11.Stellato T, Cappelleri A, Farina M, Pisano L, Scanziani R, Meroni M, et al. Severe reversible acute renal failure in idiopathic nephrotic syndrome. J Nephrol 2010; 23:717–724. [PubMed] [Google Scholar]
- 12.Smith JD, Hayslett JP. Reversible renal failure in the nephrotic syndrome. Am J Kidney Dis 1992; 19:201–213. doi: 10.1016/s0272-6386(13)80001-7. [DOI] [PubMed] [Google Scholar]
- 13.Cameron JS. The nephrotic syndrome and its complications. Am J Kidney Dis 1987; 10:157–171. doi: 10.1016/s0272-6386(87)80170-1. [DOI] [PubMed] [Google Scholar]
- 14.Maas RJ, Deegens JK, Beukhof JR, Reichert LJ, Ten Dam MA, Beutler JJ, et al. The clinical course of minimal change nephrotic syndrome with onset in adulthood or late adolescence: a case series. Am J Kidney Dis 2017; 69:637–646. doi: 10.1053/j.ajkd.2016.10.032. [DOI] [PubMed] [Google Scholar]
- 15.Coca SG. Acute kidney injury in elderly persons. Am J Kidney Dis 2010; 56:122–131. doi: 10.1053/j.ajkd.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shu KH, Lian JD, Yang YF, Lu YS, Wang JY. Serum IgE in primary glomerular diseases and its clinical significance. Nephron 1988; 49:24–28. doi: 10.1159/000184981. [DOI] [PubMed] [Google Scholar]
- 17.Tan Y, Yang D, Fan J, Chen Y. Elevated levels of immunoglobulin E may indicate steroid resistance or relapse in adult primary nephrotic syndrome, especially in minimal change nephrotic syndrome. J Int Med Res 2011; 39:2307–2313. doi: 10.1177/147323001103900629. [DOI] [PubMed] [Google Scholar]
- 18.Meyrier A. Nephrosclerosis: update on a centenarian. Nephrol Dial Transplant 2015; 30:1833–1841. doi: 10.1093/ndt/gfu366. [DOI] [PubMed] [Google Scholar]
- 19.Lowenstein J, Schacht RG, Baldwin DS. Renal failure in minimal change nephrotic syndrome. Am J Med 1981; 70:227–233. doi: 10.1016/0002-9343(81)90754-3. [DOI] [PubMed] [Google Scholar]
- 20.Vande Walle J, Mauel R, Raes A, Vandekerckhove K, Donckerwolcke R. ARF in children with minimal change nephrotic syndrome may be related to functional changes of the glomerular basal membrane. Am J Kidney Dis 2004; 43:399–404. doi: 10.1053/j.ajkd.2003.10.039. [DOI] [PubMed] [Google Scholar]


