Abstract
Objective
To assess the impact of the COVID-19 pandemic on the rate of same-day discharge (SDD) after robotic surgery
Methods
We reviewed our robotic surgeries during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020 and compared them with robotic procedures before COVID-19 and after restrictions were lifted. We followed our formerly described protocol in use since 2016 offering the option of SDD to all robotic urologic surgery patients, regardless of procedure type or patient-specific factors.
Results
During COVID-19 restrictions (COV), 89 robotic surgeries were performed and compared with 1667 of the same procedures performed previously (pre-COV) and 42 during the following month (post-COV). Among COV patients 98% (87/89 patients) opted for same-day discharge after surgery versus 52% in the historical pre-COV group (P < .00001). Post-COV, the higher rate of SDD was maintained at 98% (41/42 patients). There were no differences in 30-day complications or readmissions between SDD and overnight patients with only 2 COV (2%) and no post-COV 30-day readmissions.
Conclusion
SDD after robotic surgery was safely applied during the COVID-19 crisis without increasing complications or readmissions. SDD may allow continuation of robotic surgery despite limited hospital beds and when minimizing hospital stay is important to protect postoperative patients from infection. Our experience suggests that patient attitude is a major factor in SDD after robotic surgery since the proportion of patients opting for SDD was much higher during COV and continued post-COV. Consideration of SDD long-term may be warranted for cost savings even in the absence of a crisis.
The emergence of the COVID-19 pandemic has affected health care delivery worldwide. A massive reallocation of health care resources created major obstacles to routine medical care in addition to the need to limit nosocomial disease transmission as infected patients filled hospital beds.1
The care of surgical patients required adaptation to this novel situation at every phase of the surgical process (pre-, intra-, and postoperatively).2 , 3 Among the realities that was imposed by the COVID-19 crisis was a need to postpone elective surgeries and prioritize procedures by acuity of need in order to maintain hospital vacancies for infected patients as well as to preserve personal protective equipment (PPE) and other medical supplies. This unfortunately created a competing priority between managing the COVID-19 crisis and being able to surgically treat patients with cancers that might progress if indefinitely delayed.4
Effective from March 17, 2020, the Governor of Ohio ordered the suspension of all elective surgery,5 and while Ohio was one of the first states in the country to do so, many other states quickly followed. Among the resulting difficulties for surgeons treating urologic cancers was the uncertainty regarding how long this would last and the need to make difficult decisions regarding which cancer operations should be delayed or still performed and how to do so safely for the patients chosen to still have surgery.
One of the measures to potentially reduce the risk of nosocomial COVID-19 transmission as well as to conserve hospital resources is decreasing postoperative length of stay (LOS) among those still having surgery during the pandemic. We began integrating clinical-care pathways into robotic urologic surgical care with the aim of decreasing postoperative stays over a decade ago.6 Our recent report of same-day discharge (SDD) in the majority of robotic prostatectomy patients became very relevant once the COVID-19 crisis began.7 Additionally, while our work to limit LOS after robotic kidney surgery to one night was met with initial criticism,8, 9, 10, 11 it has since gained in acceptance,12 and we have since extended our robotic kidney surgery pathway to also allow for SDD.
When elective surgeries were banned in the State of Ohio and until May 1, 2020 when they were only allowed for elective surgeries not requiring an overnight stay,13 we applied our previous experience with SDD after robotic urologic surgery to allow patients with urologic cancers to still undergo surgical treatment while minimizing the risk of nosocomial transmission and maintaining hospital beds for a potential surge of COVID-19 patients. Because the burden of the COVID-19 crisis had been less than expected in Ohio, elective surgeries not needing overnight or longer stays were allowed first and later followed by the complete lifting of restrictions in June.14 We describe the impact of the COVID-19 pandemic during these several weeks of restriction on our SDD after robotic surgery initiative and the patient population we were able to continue to serve by intentionally intensifying our efforts to perform SDD robotic surgery as well as our experience with SDD since the lifting of restrictions. Our rate of success with SDD as well as impact on readmissions and complications were assessed and compared with our rate of SDD and outcomes before COVID-19.
Methods
We reviewed a prospective database of all robotic surgeries performed by a single surgeon (RA) between March 16 and June 5, 2020 (COV period) and compared them with historical controls prior to COVID-19 (pre-COV). During the initial period banning elective surgery (March 16-May 1), procedures were prioritized and scheduled in order based on cancer severity to treat the most time-sensitive cancers first (eg, Gleason 9 prostate cancer, >10 cm renal mass, etc.), and once elective surgery not requiring overnight stay was allowed (after May 1), the less severe cancers as well as selected noncancer cases that had been delayed were performed. During the period of March 30 to April 15, no robotic surgeries were performed as only 2 operating rooms were active, and only truly emergent surgery was allowed at our hospital during this time.
Of note, throughout the crisis period, no patient who was offered surgery based on the acuity of their cancer or condition refused to proceed. The expectation was set preoperatively that the procedure would be performed on an SDD basis unless complications mandated longer postoperative stay, but in no case were patients selected to undergo surgery or not during or after COV based on whether they were felt more or less likely to achieve SDD. All robotic procedures were included except that robotic radical cystectomy was excluded since SDD was not implemented for RRC pre-COV due to urinary diversion and need for return of bowel function, and no RRC procedures were performed during COV with only one performed post-COV with a 2-day stay.
Patients received our standard preoperative education otherwise and were informed about visitor restrictions policies, which included a ban on visitors on the hospital wards that persisted until June 15 although one visitor was permitted to accompany patients in the preoperative and postoperative area. All patients received a COVID-19 symptom and exposure questionnaire via telephone prior to hospital entry, and once testing availability in Ohio improved, an oropharyngeal swab for SARS-CoV-2 PCR test became mandated within 72 hours of surgery beginning on May 1. All surgeries were performed with PPE that included N-95 masks worn by the entire surgical team even in patients with a negative PCR until this N-95 requirement was lifted by hospital administration on July 7.
We followed our same previously described protocol in use since 2016 offering SDD to all of our robotic urologic surgery patients as an option, regardless of procedure type or patient-specific factors.7 Postoperative care includes ambulation within 2 hours, immediate diet, narcotic avoidance, and discharge from the recovery room or observation unit once ambulating, tolerating regular diet and pain control with oral medications. Patients are required to have a caregiver drive them home and stay with them for the first 24 hours after surgery in keeping with our institutional guidelines for any surgery with general anesthesia. Patients are instructed not to go to outside emergency departments or to be admitted to other facilities without notifying us to arrange transfer when needed, which allowed readmissions at any facility to be tracked in real-time in addition to during routine postoperative visits at approximately 1-2 weeks, at 1 month, and at 3-6 months depending on type of surgery.
The rate of SDD as well as complications and readmissions for the time period during pandemic restrictions on surgery (COV) were compared with patients who underwent the same robotic surgeries between 2016 and when the pandemic restrictions began (pre-COV) as well as the immediate 30-day period of time that followed lifting of all restrictions on surgery (post-COV). Immediate postoperative pain was assessed using a visual analog scale. Scores obtained during the first 6 hours were averaged for statistical analysis.
Student's t test or Mann-Whitney was applied as appropriate for continuous data, and Chi-square or Exact Fisher test for categorical variables. Normality was determined by the Shapiro-Wilk test, and Levene's test was used to assess the equality of variances. Statistical significance was considered at P < .05. Statistical analysis was performed using Statistical Analysis System software (v.9.4 SAS Institute, Cary, NC).
Results
A total of 89 robotic surgeries were performed during COV after the governor's ban was announced through June 5 with 1667 of the same procedures performed pre-COV. In the post-COV month that followed, 42 procedures were performed (Table 1 ). Our hospital procured the daVinci SP robot (single-port) in January 2019 with 125 (8%) of the 1667 pre-COV procedures performed on the SP robot and the remainder on the Xi robot. During the COV period, only 3 SP procedures were performed (3%), and post-COV 9 of 42 procedures were SP (21%).
Table 1.
Robotic Urologic Procedures Performed During COVID-19 Restrictions on Surgery and the Same Procedures Performed Before This Since 2016 and in the Month iImmediately Following Lifting of Restrictions
| Pre-COV, N (%) | COV, N (%) | Post-COV, N (%) | |
|---|---|---|---|
| Prostatectomy | 1230 (73.8) | 67 (75.3) | 33 (78.6) |
| Partial nephrectomy | 235 (14.1) | 12 (13.5) | 3 (7.1) |
| Nephrectomy | 115 (6.9) | 7 (7.9) | 1 (2.4) |
| Adrenalectomy | 18 (1.1) | 0 | 1 (2.4) |
| Nephroureterectomy | 12 (0.7) | 2 (2.2) | 0 |
| Partial cystectomy | 6 (0.3) | 1 (1.1) | 0 |
| Pyeloplasty | 48 (2.9) | 0 | 3 (7.1) |
| Ureteral reconstruction | 3 (0.2) | 0 | 1 (2.4) |
| Total | 1667 | 89 | 42 |
Mean age in the pre-COV and COV groups were 61.5 years (range, 19-88 years) and 62.6 years (range, 32-81 years), respectively (P = .31). Mean body mass index was 30.1 kg/m2 (range, 16-54 kg/m2) in the pre-COV group and 29.3 kg/m2 (range, 21-50 kg/m2) in the COV group (P = .18). COV patients had lower mean blood loss and shorter operative time on average (90 vs 105 mL, P = .002 and 141 vs 149 minutes, P < .001) potentially due to less teaching during COV surgeries. There was no statistically significant difference in mean postoperative pain scores (4.4 in pre-COV vs 4.2 in COV, P = .51).
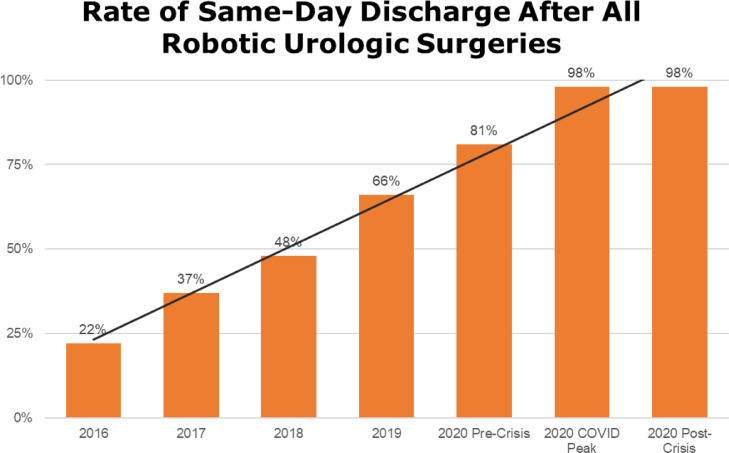
In the pre-COV group 861 (52%) were discharged on the same day as surgery with an increasing proportion of SDD over time.(Fig 1 ) During the COV period, the rate of SDD rose to 87 of 89 patients or a 98% rate of SDD (P < .0001). The remaining 2 patients during COV were discharged on postoperative day 1, and included one prostatectomy patient with vasovagal syncope, that was likely anesthesia related but precluded discharge, and one partial nephrectomy patient who was unable to void until 11 pm and was admitted overnight due to lack of transportation at this late time.
Figure 1.
Proportion of patients discharged on the same day as robotic urologic surgery since same-day program initiated in 2016, including during COVID outbreak and in the month after resumption of normal elective surgery (postcrisis period). (Color version available online.)
All patients were discharged to their own homes and not nursing facilities or other accommodations. The mean distance traveled by patients to our hospital for surgery during COV was 61.8 miles (range, 9-142 miles) such that this was not a limitation to SDD. Also, ASA score among COV patients was 2 in 42 patients (47%) and 3 in the rest, and SDD was not withheld in any patients due to age or comorbidities. Mean postoperative LOS was 5.7 hours (range, 2.1-9 hours). Pathology data are shown in Table 2 .
Table 2.
Pathologic Data on Prostatectomy and Partial Nephrectomy Procedures During Study
| Pre-COV | COV | Post-COV | |
|---|---|---|---|
| RALP (n) | 1230 | 67 | 33 |
| Pathologic stage, n (%) | |||
| Tx | 1 (0.08) | - | 2 (6.1) |
| T2 | 615 (49.9) | 47 (70.1) | 12 (36.4) |
| T3a | 478 (38.8) | 14 (20.9) | 13 (39.4) |
| T3b | 132 (10.7) | 6 (9.0) | 6 (18.1) |
| T4 | 4 (0.3) | - | |
| Mean lymph node yield (range) | 8.1 (0-25) | 8.2 (2-20) | 7.6 (2-29) |
| Node positive patients, n (%) | 91 (7.4) | 3 (4.1) | 4 (12.1) |
| RAPN (n) | 235 | 12 | 3 |
| Nephrometry score (SD, range) | 7.2 (±0.1, 4-11) | 7.5 (±0.4, 5-10) | 7.3 (±2.8,4-9) |
| Pathologic stage, n (%) | |||
| Benign | 33 (14) | - | - |
| T1a | 139 (59) | 9 (75) | 3 (100) |
| T1b | 44 (19) | 3 (25) | - |
| T2a | 3 (1.2) | - | - |
| T3a | 16 (6.8) | - | - |
Among the 1667 pre-COV patients, 4.0% (67/1,667) experienced a significant complication (Clavien III-V) within 30 days of surgery, and the 30-day all-cause readmission rate was 1.2% (20/1,667). Specifically, among the 861 of 1667 pre-COV patients who were discharged the same day as surgery, the 30-day complication rate and readmission rate were 3.0% (26/861) and 1.1% (10/861), respectively, such that SDD did not increase the risk of complications or readmissions (P = .246 and P = .999, respectively).
Among the 89 COV patients, there were 2 patients readmitted within 30 days postoperatively, including one prostatectomy patient admitted on POD#27 for 4 days of intravenous antibiotics due to a Methicilliin-Resistant Staph Aureus (MRSA) urinary tract infection. The other readmission was a patient who underwent partial nephrectomy for a 7 cm tumor with an On-Q pain pump (Avanos Medical, Inc., Alpharetta, GA) left in place due to the size of the extraction incision. The patient presented to the emergency department on POD#2 complaining that it was leaking and was (unnecessarily) admitted that night to the hospitalist team without our knowledge and discharged as soon as we evaluated him the next morning.
Following the COV period, of 42 surgeries performed, 41 were successfully discharged on the same day (98%). Mean postoperative LOS was 5.5 hours, mean Operative time (OT) was 140 minutes and Mean Estimated blood loss (EBL) 86 mL. Mean pain score was 4.5. There were no Clavien-Dindo III-V complications in post-COV group. The one post-COV patient who was not discharged on the same day was a prostatectomy patient with postoperative dizziness that resolved by the following morning but precluded discharge.
Discussion
We began offering but not mandating SDD to our robotic surgery patients as a routine beginning in 2016.7 Since then with growing experience, the proportion of patients opting for SDD has increased without an increase in complications or readmissions such that when COVID-19 crisis began, we were comfortable increasing our efforts to achieve SDD in order to allow us to continue to surgically treat urologic cancer patients. Since we had routinely been offering all patients SDD regardless of comorbidities or complexity of their surgery (eg, complex partial nephrectomy versus routine prostatectomy, etc), we did not change our protocol but found patients more willing to opt for SDD during COVID-19 likely out of anxiety of contracting the disease nosocomially.15 Among the competing anxieties of leaving their cancer untreated, being admitted after surgery to a hospital treating COVID-19 patients, and the potential fear of going home too early, the combination of proceeding with their surgery during COV but with SDD was apparently the optimal combination since no patients who were offered surgery during COV refused, and the vast majority of patients opted for SDD.
During COV, 98% of our patients were discharged the same day of surgery with no increase in readmissions compared to historical controls and no COVID-19 infections within 30 days. Demographic factors, pain score, OT and EBL were not determinants of SDD, and neither extreme age, body mass index, nor comorbidities (ie, ASA class) were limitations to SDD in our experience. Certainly, not all surgeons will be comfortable initiating an SDD protocol during a crisis if not already implementing it. We capitalized on our care pathway of SDD that began in 2016 in an attempt to safely shorten as much as possible the LOS during COV in line with CDC and American College of Surgeons guidelines.16 , 17 This allowed us to continue to perform more pressing cancer surgery during COV without taking up patients beds being reserved for an anticipated surge and also allowed more elective robotic procedures once surgeries not requiring an overnight stay were permitted.
Patient education has been essential to our SDD process from inception, and as our experience has increased, our ability to instill confidence in patients in SDD has increased given hundreds of patients who have safely been discharged the same day as their robotic surgery. We believe that the additional measures such as utilizing low-pressure pneumoperitoneum,18 reasonable operative times, narcotic avoidance, and immediate diet and ambulation are also critical in facilitating SDD and also rely on surgeon comfort and experience over time. Surgeons who have already embarked upon SDD protocols can be encouraged by our experience to extend this further during crises like COVID-19.
In addition, the avoidance of leaving abdominal drains likely contributes to SDD since no patients then are required to manage a drain at home, and lack of a drain may also have a psychosomatic effect on patient willingness for SDD. Among the 1667 pre-COV patients, a Jackson-Pratt or Blake drain was placed in only 5 (0.3%) patients with no drains left in any of the COV or post-COV patients.
It is less clear and more controversial what implications our findings will have on LOS after robotic surgery following the resolution of the COVID-19 pandemic. If indeed nearly all patients can be safely discharged on the day of robotic surgery in experienced hands, this may suggest that we should consider continuing near total SDD even after the crisis. While the expected level of COVID infections in our state did not surge as much as expected, we still achieved nearly complete SDD after the need to preserve hospital beds had passed (post-COV). Of course, this did rely on patient attitudes since we offered but did not force SDD, and it is possible that patient preferences will shift after the risk of nosocomial COVID-19 has passed with some no longer preferring the safety of home over an overnight stay.
Nevertheless, since we found no medical necessity for overnight hospitalization in the vast majority of our patients, whether this will cause us to more strongly encourage discharge once COVID-19 has passed is uncertain. For the time being, we intend to use our experience to reassure patients that SDD is extremely safe without forcing it on any patients, but just as our previous experience since 2016 allowed for an increasing rate of SDD, we believe that our experience during COV will make us more adept at SDD in the long run. Whether our experience is reproducible and will be accepted by other surgeons and institutions will require time to determine, but the natural evolution with minimally invasive surgery has always been to reduce LOS over time with ours and others’ previous work in this regard increasingly being adopted.
Certainly, not all surgeons performing robotic surgery will adopt SDD, and it may not be as safe for less experienced or lower volume surgeons unfamiliar with their outcomes or what to expect if they attempt it. Even during a crisis like COVID-19, forcing SDD when not safe could have a worse, unintended effect since readmissions and complications would create more of a strain and use of resources than an overnight stay or delaying surgery to a more opportune time. Our study is limited by the experience of one surgeon who has performed over 5000 robotic operations, although such extensive experience may not be necessary. As we have shared our experience with colleagues, we have seen SDD adopted in a variety of settings including academic and private hospitals by surgeons with diverse backgrounds in terms of training and experience. While SDD may not be appropriate for all, further study (and open minds) will be needed to identify optimal implementation and timing since even procedures such as laparoscopic cholecystectomy, now performed predominantly as an outpatient procedure, did not reach this reality overnight.
For those able to safely adopt SDD based on knowledge of their outcomes and complications, SDD has the potential to allow patients to be treated despite the limitations imposed by such a crisis and may warrant consideration by high-quality and highly experienced surgeons even when resources are not stretched as thin. The unique situation imposed by COVID-19 advanced us in SDD beyond what we expected otherwise, but even before COVID-19, the financial pressures on modern health care suggest a need to explore SDD protocols and likely now post-COVID will make the potential savings more important than ever.
Conclusion
SDD was feasible and safe after robotic urological surgery during restrictions imposed by the COVID-19 crisis. An increase in patient acceptance for SDD during and after the initial COV period was seen with nearly all patients able to go home the day of surgery without any increase in complications or readmissions. During crises like the COVID-19 pandemic, adopting a protocol of SDD after robotic surgery may allow more surgeries to be performed while preserving hospital beds and reducing postoperative patient exposure to infection and may allow for cost savings in the absence of such a crisis.
Acknowledgments
The authors would like to acknowledge Deborah Chervin for database maintenance and the OhioHealth Research Institute.
Footnotes
Financial Disclosure:The authors declare that they have no relevant financial interests.
References
- 1.Dietz L, Horve PF, Coil DA, Fretz M, Eisen JA, Van Den Wymelenberg K. 2019 novel coronavirus (COVID-19) pandemic: built environment considerations to reduce transmission. mSystems. 2020;5(2):1–15. doi: 10.1128/mSystems.00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steward J, Kitley WR, Schmidt CM, et al. Urologic surgery and COVID-19: How the pandemic is changing the way we operate. J Endourol. 2020 doi: 10.1089/end.2020.0342. [DOI] [PubMed] [Google Scholar]
- 3.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020 doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moujaess Elissar, Raphael Kourie Hampig, Ghosn Marwan. Cancer patients and research during COVID-19 pandemic: a systematic review of current evidence. Crit Rev Oncol Hematol. 2020 doi: 10.1016/j.critrevonc.2020.102972. doi: 10.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Director's Order for the management of non-essential surgeries as and procedures throughout Ohio. 2020. Available at: https://governor.ohio.gov/wps/portal/gov/governor/media/news-and-media/elective%20surgeries-postponed-in-ohio-hospitals. Accessed July 2, 2020.
- 6.Shah AD, Abaza R. Clinical pathway for 3-day stay after robot-assisted cystectomy. J Endourol. 2011;25:1253–1258. doi: 10.1089/end.2011.0035. [DOI] [PubMed] [Google Scholar]
- 7.Abaza R, Martinez O, Ferroni MC, et al. Same Day Discharge after Robotic Radical Prostatectomy. J Urol. 2019;202:959–963. doi: 10.1097/JU.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 8.Abaza R, Shah K. A single overnight stay is possible for most patients undergoing robotic partial nephrectomy. Urology. 2013;81:301–306. doi: 10.1016/j.urology.2012.08.067. [DOI] [PubMed] [Google Scholar]
- 9.Gorin MA, Allaf ME. Editorial comment on: A single overnight stay is possible for most patients undergoing robotic partial nephrectomy. Urology. 2013;81:306–307. doi: 10.1016/j.urology.2012.08.088. [DOI] [PubMed] [Google Scholar]
- 10.Khemees TA, Nasser SM, Abaza R. Clinical pathway after robotic nephroureterectomy: omission of pelvic drain with next-day catheter removal and discharge. Urology. 2014;83:818–823. doi: 10.1016/j.urology.2013.10.078. [DOI] [PubMed] [Google Scholar]
- 11.Petros FG, Angell JE, Abaza R. Outcomes of robotic nephrectomy including highest-complexity cases: largest series to date and literature review. Urology. 2015;85:1352–1358. doi: 10.1016/j.urology.2014.11.063. [DOI] [PubMed] [Google Scholar]
- 12.Sentell KT, Badani KK, Paulucci DJ, et al. A single overnight stay after robotic partial nephrectomy does not increase complications. J Endourol. 2019;33:1003–1008. doi: 10.1089/end.2019.0218. [DOI] [PubMed] [Google Scholar]
- 13.Saker, Anne: Coronavirus in Ohio: Hospitals resumed elective surgeries. Here's what you need to know. Cincinnati Enquirer Available at:https://www.cincinnati.com/story/news/2020/05/04/coronavirus-ohio-hospitals-reopen-elective-surgery-what-you-need-know/3078316001/ Accessed July 17, 2020
- 14.Director's Order for the management of non-essential surgeries as and procedures throughout Ohio., 2020. Available at:https://content.govdelivery.com/attachments/OHOOD/2020/06/02/file_attachments/1465220/0758_001.pdf. Accessed July 2, 2020.
- 15.Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention: framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. Available at:https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Accessed July 1, 2020
- 17.American College of Surgeons: COVID-19: recommendations for management of elective surgical procedures. Available at:https://www.facs.org/covid-19/clinical-guidance/elective-surgery. Accessed July 1, 2020.
- 18.Puliatti S, Eissa A, Eissa R, et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int. 2020;125:E7–E14. doi: 10.1111/bju.15071. [DOI] [PubMed] [Google Scholar]