Abstract
Background
Face masks have become commonplace across the USA because of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic. Although evidence suggests that masks help to curb the spread of the disease, there is little empirical research at the population level. We investigate the association between self-reported mask-wearing, physical distancing, and SARS-CoV-2 transmission in the USA, along with the effect of statewide mandates on mask uptake.
Methods
Serial cross-sectional surveys were administered via a web platform to randomly surveyed US individuals aged 13 years and older, to query self-reports of face mask-wearing. Survey responses were combined with instantaneous reproductive number (Rt) estimates from two publicly available sources, the outcome of interest. Measures of physical distancing, community demographics, and other potential sources of confounding (from publicly available sources) were also assessed. We fitted multivariate logistic regression models to estimate the association between mask-wearing and community transmission control (Rt<1). Additionally, mask-wearing in 12 states was evaluated 2 weeks before and after statewide mandates.
Findings
378 207 individuals responded to the survey between June 3 and July 27, 2020, of which 4186 were excluded for missing data. We observed an increasing trend in reported mask usage across the USA, although uptake varied by geography. A logistic model controlling for physical distancing, population demographics, and other variables found that a 10% increase in self-reported mask-wearing was associated with an increased odds of transmission control (odds ratio 3·53, 95% CI 2·03–6·43). We found that communities with high reported mask-wearing and physical distancing had the highest predicted probability of transmission control. Segmented regression analysis of reported mask-wearing showed no statistically significant change in the slope after mandates were introduced; however, the upward trend in reported mask-wearing was preserved.
Interpretation
The widespread reported use of face masks combined with physical distancing increases the odds of SARS-CoV-2 transmission control. Self-reported mask-wearing increased separately from government mask mandates, suggesting that supplemental public health interventions are needed to maximise adoption and help to curb the ongoing epidemic.
Funding
Flu Lab, Google.org (via the Tides Foundation), National Institutes for Health, National Science Foundation, Morris-Singer Foundation, MOOD, Branco Weiss Fellowship, Ending Pandemics, Centers for Disease Control and Prevention (USA).
Introduction
In December, 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the resulting COVID-19 disease were first identified in Wuhan, China.1 The disease has spread globally since its identification, causing widespread mortality.2 Governments in the USA and worldwide have adopted many different approaches to curb the virus's continued transmission.3 Despite widespread implementation, the effectiveness of various non-pharmaceutical interventions has been debated,4 resulting in substantial heterogeneity in the acceptance of these interventions at the individual and community level,5 including the use of face masks and respirators.6
Evidence indicates that N95 respirators are an effective method to prevent respiratory virus transmission in some settings, but fit testing educational requirements and supply chain shortages necessitate their preferential allocation to front-line medical personnel who are at high risk of the disease.7 Consequently, cloth face coverings and surgical masks (collectively known as face masks) have been recommended as an alternative for the general public.8 Following the initial spread of the virus in the USA, many local and state jurisdictions have mandated the use of face masks in public settings.3 These masks are intended to serve as a mechanical barrier that prevents the spread of virus-laden droplets expelled by the user.9 Therefore, their purpose is to reduce transmission events by the individual, rather than to protect the individual from infection. Accordingly, face masks are advocated as a source of collective benefit that is most successful with high amounts of adoption.10
Research in context.
Evidence before this study
We searched PubMed and medRxiv for all articles posted between Jan 1 and Aug 24, 2020, with the terms: “mask”, “reproductive number”, “social distancing”, and “SARS-CoV-2”, or “COVID-19”. We combined this list with known publications that did not meet the specified search criteria. We excluded studies where the results were estimated from mathematical models or presented as hypotheticals, as well as those that did not directly estimate the association of face masks with transmission. We found two case reports and one non-peer reviewed observational study that met our criteria. Although each study made use of different endpoints, all found significantly lower disease measures with higher rates of mask-wearing. We also found a study that established mask mandates as a proxy for mask-wearing, but there was no statistical association between mandates and a lower rate of transmission. Despite little observational and experimental research on masks, physical distancing, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), evidence from other respiratory pathogens and bench science indicates the effectiveness of masks at reducing disease spread.
Added value of this study
To understand the effectiveness of face masks as a non-pharmaceutical intervention, we directly examined mask-wearing instead of using mask mandates as a proxy. We supplemented case studies by using a large sample representative of the population across the USA, combined with community estimates of SARS-CoV-2 transmission. We showed that states with higher rates of mask-wearing had estimated instantaneous reproductive numbers that were lower than the crucial threshold needed to maintain disease transmission. We also showed that mask mandates alone might not be sufficient to increase mask-wearing rates and, therefore, highlight why studies analysing mask mandate interventions might not find a statistical effect, despite the positive effect of masks.
Implications of all the available evidence
In combination with previous research, this study shows that the community adoption of face masks might be an important non-pharmaceutical intervention for the reduction of SARS-CoV-2. Beyond mask mandates, innovative strategies to increase the use of face masks should be explored.
There is little empirical, population-level evidence on the effectiveness of face masks at preventing respiratory transmission of SARS-CoV-2, but it is growing.8, 11 Although studies on other respiratory infections12 and two recent case reports13, 14 suggest that wearing a mask might be effective, a recent global analysis (published as a preprint) found a small effect of mask mandates on reducing SARS-CoV-2 transmission in the presence of other interventions.15 In this Article, we use an ecological approach to assess mask compliance directly, irrespective of mandates. We combine survey data on self-reported mask-wearing habits across the USA with a time-varying measure of transmission control, as quantified by the instantaneous reproductive number (Rt) in each state. We then evaluate the association of a change in self-reported mask-wearing with the timing of mask mandates to better understand their effect on transmission of COVID-19.
Methods
Survey description
A web survey hosted on SurveyMonkey.com was used in conjunction with COVIDNearYou (a Boston Children's Hospital digital surveillance platform), as part of an effort to increase participatory syndromic surveillance for COVID-19.16 The survey data were collected through SurveyMonkey's so-called end-page river sampling. Briefly, the surveys were sent to people in the USA via the SurveyMonkey online survey platform.17 At the completion of these surveys, respondents in the USA were invited at random to participate in the COVIDNearYou web survey. Every user within a specified geography (the USA) had an equal probability of being selected. Data were not collected or processed on individuals that met the exclusion criteria (younger than 13 years old and older than 100 years old). The platform is primarily used for syndromic surveillance, and research is secondary; therefore the sample size was not optimised for research and was instead optimised to ensure a national coverage of the survey. The river sample is not a stochastic probability sample of the entire population; however, it reaches respondents with diverse geographical and demographic backgrounds to ensure broad representativeness. Responses to this questionnaire were collected between June 3 and July 27, 2020, in all 50 states and the District of Columbia. Respondents were not provided with incentives to complete the questionnaire and approximately 11% of those presented with the survey chose to participate. This study was approved by the Boston Children's Hospital Institutional Review Board and received a waiver of informed consent.
Survey responses were analysed as crude data (unweighted) and with survey weights that reflected the demographic composition of the USA. Survey weights accounted for age, race, sex, education, and geography by use of the Census Bureau's American Community Survey.18 Also included was a smoothing parameter for political party identification based on aggregates of SurveyMonkey research surveys, refreshed once per week with rolling 2-week aggregated data. There is no census parameter for partisan identification; however, attitudes towards face masks and COVID-19 differ along some partisan lines.5 This mechanism provides weights to ensure that the samples reflect the political composition of the USA. All weights are generated once a day for weekday surveys and once after weekend surveys.
Mask-wearing exposure
Survey respondents were asked a range of questions19 including how likely they were to wear a mask “while grocery shopping” or “while visiting with family or friends in their homes” on a four-point scale, from “very likely” to “not likely at all”. A composite exposure of consistent self-reported face mask-wearing was defined as the percentage of respondents who replied “very likely” to these two questions. The responses to other questions were not analysed, such as “while exercising outside”, which was dependent on weather and not thought to be as biologically relevant to transmission as the other two responses; and “while working at your office or workplace”, which was entirely confounded by and intertwined with work from home policies and did not make sense in the context that a large portion of Americans were not going to their workplace. Two sensitivity analyses of the exposure were included. One measured the percentage of respondents who replied “very likely” to each question separately. A second created a weighted variable where each Likert response was attributed to a percentage of time wearing a mask (appendix p 4). Surveys missing responses to either of the two questions we examined (n=4186) were excluded from sensitivity analyses and aggregate values.
Descriptive statistics, stratified by self-reported mask-wearing, were evaluated with two-tailed χ2 tests at a p<0·05 significance threshold (with software gmisc version 1.9.2). Surveys missing responses to individual questions were still used in aggregate values for available measures. To produce visual maps of reported mask-wearing in the USA, the three-digit prefix of each zip code reported in the survey results was fuzzy matched to a three-digit ZIP Code Tabulation Area prefix.
For validation with an alternative instrument to assess self-reported mask-wearing, survey results were compared against cross-sectional New York Times and Dynata interviews on mask-wearing.6 Survey responses and validation interviews were aggregated by county (restricted to counties with ten or more observations, n=1055) between July 2 and July 14, 2020, and Spearman's non-parametric correlation coefficient was used to assess the relationship between results from the two different sources.
Physical distancing exposure
Population-level physical distancing by state and by week was quantified as the duration of time spent at home compared with a baseline period defined by Google (Jan 3–Feb 6, 2020). The baseline period represented a recent period before widespread mobility changes because of COVID-19.20 Duration of time spent at home was estimated with the Google community mobility measure on residential time, which was estimated by use of anonymised and aggregated data from individual Google users who opted into location history on their mobile devices.20 A measure of physical distancing from Carnegie Mellon University's Delphi Research Group COVID-19 symptom survey21 was included in a sensitivity analysis. Individuals were asked, in a survey delivered on the Facebook web platform, “in the past 24 hours, with how many people have you had direct contact, outside of your household”, in various settings. The number of self-reported contacts at social gatherings (with censored outlier responses) was aggregated over each week and state by use of the Delphi Research Group weighted sampling scheme.21
Community transmission control outcome
The daily estimated Rt—the number of secondary cases arising from a single case for a given day—was used to measure state-specific community transmission control. Rt was aggregated to the week and dichotomised as epidemic slowing (1 if Rt<1) or epidemic at maintenance or growing (0 if Rt≥1). Rt was dichotomised to reduce noise (non-biologically relevant changes in Rt) from small fluctuations in the underlying data, reduce autocorrelation (ie, the relationship between the model's residuals at time t and lagged residuals at time t minus n), and allow for the use of a regression framework less prone to bias than the non-normally distributed continuous Rt. Rt estimates were downloaded from the rt.live publicly available database, which were fitted to case data from The COVID Tracking Project and the open COVID-19 data working group (methods and adaptation previously described).2 Sensitivity analyses were done with Rt values downloaded from epiforecasts.io22 (available up to July 19, 2020) and with Rt dichotomised at values sequentially from 0·975 to 1·150 with intervals of 0·005 (eg, 0·975, 0·980, 0·985, and so on until 1·150) instead of the critical value of 1. Both approaches accounted for reporting delays by use of a subset of cases that described both the date of disease onset and the date of notification.2, 22
Modelling mask effectiveness on transmission control
We fitted multivariate logistic regression models with R (version 3.6.2) and the stats package (version 3.6.2) to predict the community transmission control outcome (binary Rt) by use of state-specific and week-specific estimates of self-reported mask-wearing (crude and survey-weighted) and physical distancing measures (relative residential time). Our models defined a single percentage point as the unit of measurement for mask-wearing; however, we also assessed a 10% change, because this value represented approximately a single standard deviation of observed data, suggesting that it is a realistic goal for a public health intervention. State population density was included as a potential confounder, given the association between the population structure and SARS-CoV-2 transmission,23 and the association between urban versus rural regions and face mask usage.6 The percentage of non-White individuals included in the study was included as a confounder because of the relationship of race with epidemiological indicators of SARS-CoV-224 and uptake of non-pharmaceutical interventions.25 A linear weekly time trend was also modelled.
To address the potential of reverse causation, where high previous transmission rates induced increased rates of mask-wearing and a lower potential Rt (because of reduced effective contact availability), we included each state's peak Rt from March to May, 2020 (as estimated by rt.live), as a confounder in a sensitivity analysis. We also evaluated an interaction between the exposures of self-reported mask-wearing and physical distancing.
For each model, influential observations (up to n=24) with a Cook's distance over 4/N were excluded.26 The influential observations removed varied between models, except for observations from New Jersey (characterised by high reported mask-wearing rates, notably high physical distancing rates, and high community transmission control), which were repeatedly excluded for influence. Autocorrelation was visually assessed in the base model (model 1) with white noise critical value cutoffs (R stats version 3.6.2). Although the base model (model 1) showed autocorrelation at a 1-week lag, dichotomisation and once a week aggregation removed other significant correlations.
Two additional modelling frameworks were used in sensitivity analyses. Although each survey consisted of an independent sample of respondents, a mixed model (produced using R lme4 version 1.1) with a random intercept for state and the same fixed effects as reported in the crude logistic model (model 1) was fitted to account for the potential hierarchical structure of the observations. Additionally, Rt was converted to a six-level categorical variable (the category boundaries are detailed in appendix pp 3 and 5) and an ordinal logistic regression (done with R MASS software version 7.3) was fitted to measure the association of reported mask-wearing with levels of Rt. Detailed formulations of each model can be found in the appendix (p 5)).
Mask mandates
The date for each statewide mask mandate was extracted from the masks4all database. To assess the effect of mask mandates on self-reported mask-wearing, segmented regression was run comparing the 2 weeks before and 2 weeks after each state's intervention. All 12 states that issued a statewide mandate between June 17 and July 13, 2020 (2 weeks after the survey start and 2 weeks before survey completion), were included in this analysis.
Role of the funding source
The funding bodies had no role in study design, data collection, analysis, interpretation, writing of the manuscript, or the decision to publish. All authors had full access to all the data in the study and the corresponding author had final responsibility for the decision to submit for publication.
Results
Self-reported mask-wearing was evaluated in 378 207 survey responses recorded between June 3 and July 27, 2020. Most individuals (319 980, 84·6%) reported that they were very likely to wear a face mask to the grocery store, whereas just under half (152 158, 40·2%) reported that they did so to visit friends and family. A similar proportion (150 323, 39·8%) reported they were very likely to wear a mask to the grocery store and with family or friends. Few (17 903, 4·7%) reported they were “not likely at all” to wear a mask in either setting. The percentage of individuals in each county who reported always wearing a mask in the New York Times interviews was correlated with the proportion of those who reported that they were “very likely” to wear a mask to the grocery store (Spearman's ρ=0·74, p<0·0001), with the proportion of those who were “very likely” to wear a mask with family or friends (Spearman's ρ=0·52, p<0·0001), and with the composite score (Spearman's ρ=0·53, p<0·0001).
Self-reported mask-wearing was higher among women, Black, Hispanic, and race groups other than White, respondents with lower income, and increased in a linear manner with age (table 1 ). There was substantial geographical heterogeneity in survey responses (figure 1A ), with the highest percentage of reported mask wearers along the coasts and southern border, and in large urban areas. When aggregating self-reported mask-wearing across US census divisions to assess time trends, there was a general increase in reported use (figure 1B). The west north central census division reported the lowest mask usage across the entire period surveyed.
Table 1.
Characteristics of unweighted survey respondents by status of likelihood to wear a mask
| Very likely (n=152 158) | Somewhat likely (n=81 596) | Not so likely (n=73 723) | Not likely at all (n=67 832) | Total (n=375 309) | |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 103 624 (42%) | 54 314 (22%) | 47 825 (19%) | 40 908 (17%) | 246 671 (66%) |
| Male | 46 543 (38%) | 26 374 (21%) | 25 226 (20%) | 25 910 (21%) | 124 053 (33%) |
| Missing | 1991 (43%) | 908 (20%) | 672 (15%) | 1014 (22%) | 4585 (1%) |
| p value | .. | .. | .. | .. | <0·0001 |
| Age (years) | |||||
| 13–17 | 7 (33%) | 4 (19%) | 5 (24%) | 5 (24%) | 21 (0%) |
| 18–24 | 6328 (33%) | 4626 (24%) | 4564 (24%) | 3895 (20%) | 19 413 (5%) |
| 25–34 | 15 943 (35%) | 9790 (22%) | 9955 (22%) | 9629 (21%) | 45 317 (12%) |
| 35–44 | 25 679 (36%) | 14 938 (21%) | 14 339 (20%) | 15 503 (22%) | 70 459 (19%) |
| 45–54 | 32 138 (40%) | 17 505 (22%) | 15 778 (19%) | 15 755 (19%) | 81 176 (22%) |
| 55–64 | 35 005 (44%) | 17 697 (22%) | 14 915 (19%) | 12 772 (16%) | 80 389 (21%) |
| 65+ | 35 763 (48%) | 15 874 (21%) | 13 114 (18%) | 9372 (13%) | 74 123 (20%) |
| Missing | 1295 (29%) | 1162 (26%) | 1053 (24%) | 901 (20%) | 4411 (1%) |
| p value | .. | .. | .. | .. | <0·0001 |
| Race | |||||
| White | 91 105 (35%) | 58 395 (22%) | 58 303 (22%) | 55 380 (21%) | 263 183 (70%) |
| Black | 26 904 (62%) | 8638 (20%) | 4579 (11%) | 2955 (7%) | 43 076 (11%) |
| Hispanic | 8858 (57%) | 3237 (21%) | 2166 (14%) | 1309 (8%) | 15 570 (4%) |
| Other | 16 510 (49%) | 7314 (22%) | 5513 (16%) | 4202 (13%) | 33 539 (9%) |
| Missing | 8781 (44%) | 4012 (20%) | 3162 (16%) | 3986 (20%) | 19 941 (5%) |
| p value | .. | .. | .. | .. | <0·0001 |
| Household income | |||||
| <US$50 000 | 47 847 (44%) | 23 025 (21%) | 19 373 (18%) | 17 927 (17%) | 108 172 (29%) |
| US$50 000–99 000 | 43 380 (39%) | 24 601 (22%) | 22 285 (20%) | 20 707 (19%) | 110 973 (30%) |
| >US$100 000 | 51 010 (38%) | 29 095 (22%) | 27 951 (21%) | 25 954 (19%) | 134 010 (36%) |
| Missing | 9921 (45%) | 4875 (22%) | 4114 (19%) | 3244 (15%) | 22 154 (6%) |
| p value | .. | .. | .. | .. | <0·0001 |
| Census division | |||||
| New England | 10 747 (48%) | 5421 (24%) | 3838 (17%) | 2518 (11%) | 22 524 (6%) |
| Middle Atlantic | 20 939 (45%) | 10 336 (22%) | 8407 (18%) | 6826 (15%) | 46 508 (12%) |
| East north central | 17 206 (35%) | 11 205 (23%) | 10 723 (22%) | 10 117 (21%) | 49 251 (13%) |
| West north central | 7692 (28%) | 6168 (23%) | 6557 (24%) | 6762 (25%) | 27 179 (7%) |
| East south central | 7508 (35%) | 4484 (21%) | 4530 (21%) | 4838 (23%) | 21 360 (6%) |
| West south central | 15 332 (40%) | 7883 (21%) | 7490 (20%) | 7417 (19%) | 38 122 (10%) |
| South Atlantic | 34 688 (42%) | 17 453 (21%) | 15 610 (19%) | 14 218 (17%) | 81 969 (22%) |
| Pacific | 27 244 (48%) | 11 989 (21%) | 9878 (17%) | 8028 (14%) | 57 139 (15%) |
| Mountain | 10 802 (35%) | 6657 (21%) | 6690 (21%) | 7108 (23%) | 31 257 (8%) |
| p value | .. | .. | .. | .. | <0·0001 |
| Health status | |||||
| Excellent | 42 791 (41%) | 19 453 (19%) | 18 125 (18%) | 23 046 (22%) | 103 415 (28%) |
| Very good | 61 462 (39%) | 36 537 (23%) | 33 015 (21%) | 27 374 (17%) | 158 388 (42%) |
| Good | 9971 (46%) | 4573 (21%) | 3870 (18%) | 3150 (15%) | 21 564 (6%) |
| Fair | 36 256 (41%) | 20 487 (23%) | 18 240 (21%) | 13 638 (15%) | 88 621 (24%) |
| Poor | 1445 (51%) | 450 (16%) | 392 (14%) | 540 (19%) | 2827 (1%) |
| Missing | 233 (47%) | 96 (19%) | 81 (16%) | 84 (17%) | 494 (0%) |
| p value | .. | .. | .. | .. | <0·0001 |
Characteristics of unweighted survey respondents by their likelihood to wear a protective mask “while visiting with friends or family in their homes.” For each response, the number of respondents (and percentage of the row total) and the p value on the association between the characteristic and degree of mask-wearing from a χ2 test are presented.
Figure 1.
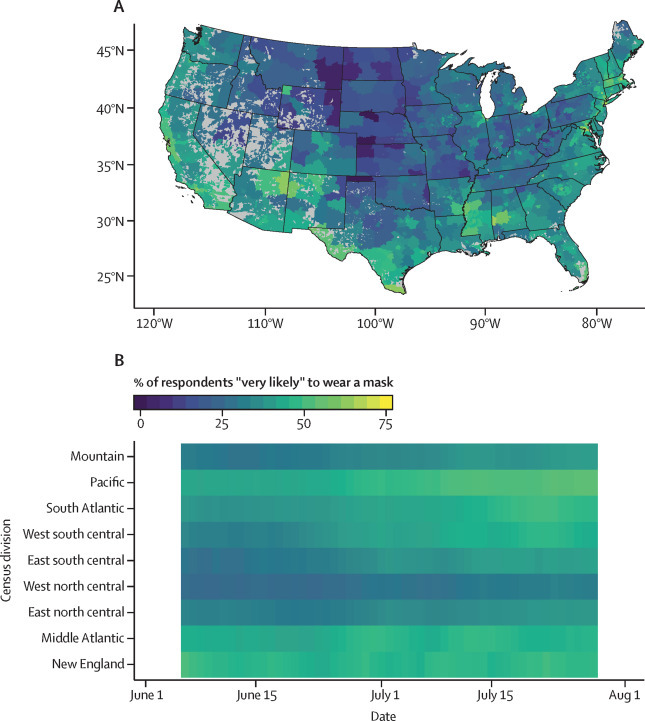
Mask-wearing across three-digit zip code areas and over time
(A) The percentage of individuals who responded they were “very likely” to wear a mask to the grocery store and with family or friends was averaged across the entire study period and each three-digit ZIP Code Tabulation Area prefix (fuzzy matched with reported zip code) in the USA. ZIP Code Tabulation Area clusters with less than 50 responses are shown in grey. (B) Observations of mask-wearing were also aggregated at the daily level across each census division for the study period.
We found a negative relationship between the mean percentage of people who reported wearing a mask and the Rt (figure 2 ). In a multivariate logistic regression model adjusting for confounders, physical distancing, and a time trend, there was a significant association between percentage of reported mask-wearing and community transmission control (ie, Rt<1; table 2 , model 1). A 10% increase in reported mask-wearing was associated with an increase of more than three-fold in odds of transmission control (model 1 with a 10-point extrapolation, odds ratio [OR] 3·53, 95% CI 2·03–6·43). The association between self-reported mask-wearing and community transmission control was not substantially affected by survey-weight standardisation, use of an Rt estimated from epiforecasts.io, use of an alternative definition of mask-wearing, and controlling for peak Rt (table 2, models 2–6). The association between the weighted Likert scale variable of self-reported mask-wearing and community transmission control was similar to the unweighted mask-wearing variable (OR 1·20, 95% CI 1·10–1·30).
Figure 2.
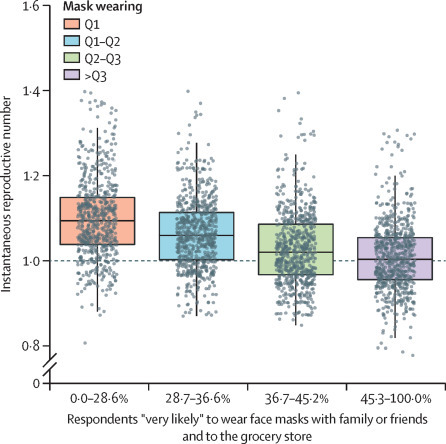
Mask wearing and the instantaneous reproductive number
Box (median and IQR) and whisker (minimum and maximum, excluding outliers) plots of Rt estimates for each week within the study period and state (grey circles). Plot is stratified by quartiles (Q1: 0–28·6%, Q2: 28·7–36·6%, Q3: 36·7–45·2%, Q4: 45·3–100·0%) of the percentage of individuals who reported that they were “very likely” to wear a mask with family or friends and to the grocery store.
Table 2.
Results of multivariable logistic regression analysis for seven different models on mask-wearing and Rt values accounting for various factors
| Model 1: association with Rt, OR (95% CI) | Model 2: weighted sample, OR (95% CI) | Model 3: association with Rt, OR (95% CI) | Model 4: alternative mask definition 1, OR (95% CI) | Model 5: alternative mask definition 2, OR (95% CI) | Model 6: accounting for transmission before the start of the study, OR (95% CI) | Model 7: with interaction term, OR (95% CI) | |
|---|---|---|---|---|---|---|---|
| Composite percentage of respondents “very likely” to wear a mask | 1·14* (1·07–1·20) | 1·13* (1·07–1·20) | 1·10* (1·04–1·15) | .. | .. | 1·14* (1·08–1·21) | 1·17† (1·05–1·32) |
| Time trend (measured by week) | 1·36* (1·17–1·58) | 1·35* (1·16–1·57) | 1·27* (1·11–1·45) | 1·37* (1·18–1·59) | 1·40* (1·20–1·63) | 1·38* (1·18–1·60) | 1·35* (1·17–1·56) |
| Physical distancing (measured by proxy) | 1·42* (1·16–1·74) | 1·43* (1·17–1·75) | 1·37† (1·13–1·66) | 1·41* (1·15–1·72) | 1·52* (1·24–1·86) | 1·39† (1·13–1·72) | 1·77 (0·99–3·15) |
| Race other than White | 0·94* (0·91–0·96) | 0·94* (0·91–0·97) | 0·94* (0·92–0·97) | 0·94* (0·91–0·96) | 0·96* (0·93–0·98) | 0·93* (0·90–0·96) | 0·95* (0·92–0·97) |
| Density (measured by 1000 people per square mile) | 0·09† (0·02–0·39) | 0·08* (0·02–0·31) | 0·30‡ (0·10–0·88) | 0·09† (0·02–0·39) | 0·08* (0·02–0·32) | 0·03* (0·01–0·15) | 0·10† (0·03–0·41) |
| Percentage of respondents “very likely” to wear a mask with family or friends | .. | .. | .. | 1·14* (1·08–1·21) | .. | .. | .. |
| Percentage of respondents “very likely” to wear a mask when grocery shopping | .. | .. | .. | .. | 1·07† (1·02–1·12) | .. | .. |
| State peak Rt (March–May) | .. | .. | .. | .. | .. | 2·60* (1·49–4·56) | .. |
| Mask wearing and physical distancing | .. | .. | .. | .. | .. | .. | 0·99 (0·98–1·01) |
| Total number of observations (week × state) | 376 | 379 | 378 | 376 | 382 | 381 | 382 |
| Akaike information criterion | 347·78 | 352·83 | 383·84 | 347·10 | 366·59 | 346·94 | 363·63 |
| Pseudo R2 | 0·39 | 0·38 | 0·31 | 0·40 | 0·35 | 0·41 | 0·37 |
Each N represents one observation of one state on a single week. Model 1 reports the association of the outcome of community transmission control (Rt<1) with the percentage of survey respondents stating that they were “very likely” to wear a face mask to the grocery store and to visit family and friends, aggregated by state and week. Model 1 controls for a weekly time trend, physical distancing (measured by relative Google mobility residential time), percentage non-White, and population density. We evaluated the association using survey weights (model 2), alternative estimators of Rt (model 3), and alternative definitions of mask usage (models 4 and 5). Model 6 accounts for each states' peak Rt before the start of the study, and model 7 includes an interaction of mask wearing with physical distancing. OR=odds ratio. Rt=instantaneous reproductive number.
p<0·001.
p<0·01.
p<0·05.
When adjusting for community self-reported contacts instead of mobility, the association between a 1% change in reported mask-wearing and community transmission control was attenuated compared with the base model (model 1; OR 1·09, 95% CI 1·02–1·16), but was still significant (appendix p 1). Self-reported mask-wearing was also significantly associated with reduced transmission across multiple Rt dichotomisation thresholds (appendix p 2) and when categorised as an ordinal variable (appendix p 3). A mixed model with a random intercept for state found a stronger association of reported mask-wearing with community transmission control (OR 1·18, 95% CI 1·07–1·30).
Communities with high amounts of self-reported mask-wearing and physical distancing were predicted by a logistic regression model to have the highest probability of community transmission control (figure 3 ). States with high rates of reported mask-wearing (57%) but with no change from baseline in physical distancing rates had a 22% (3–76%) predicted probability of community transmission control, although the confidence intervals are wide. The interaction between physical distancing and reported mask-wearing was not statistically significant (table 2, model 7).
Figure 3.
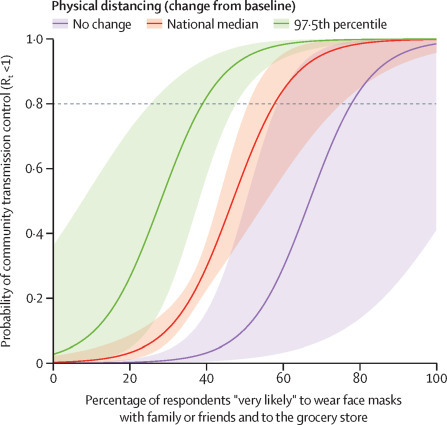
Mask wearing, physical distancing, and the predicted probability of Rt being less than 1
Projected values from a logistic regression model measuring the association of community transmission control (Rt<1) with mask-wearing and physical distancing in US states, adjusting for population density, percentage of respondents who were not White, and a time trend. Values of physical distancing were from the Google community reports of relative residential time and represent no change from baseline, the national median during the study period (June 3–July 31, 2020), and the 97·5th percentile observed during the study period. Observed mask-wearing was 8·1–73·7%, so estimates outside this range are model-based extrapolations. The horizontal line was placed at a 0·8 probability of community transmission control, though the desired percentage might be higher. Rt=instantaneous reproductive number.
We evaluated the change in self-reported mask-wearing in the 2 weeks before and after statewide mask mandates for 12 states (figure 4 ). Although there was a general trend of increased reported mask usage over this time period, the linear segmented regression models resulted in no significant change in slope in crude (β=0·04; 95% CI −0·47 to 0·54) or weighted (0·31; −0·28 to 0·91) mask usage after the interventions. There was a non-significant 2·2% (95% CI −2·1 to 6·5) change in average mask usage after the mandate in the unweighted model and a 2·31% (−2·76 to 7·38) change in the weighted model.
Figure 4.
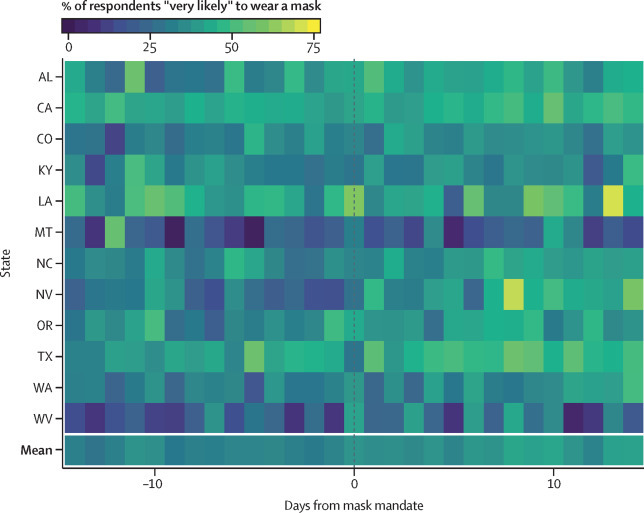
Mask wearing in the 14 days before and after statewide mask mandates
The percentage of individuals who reported that they were “very likely” to wear a mask with family or friends and to the grocery store in 12 states, in each of the 14 days before and after each state's institution of a statewide mask mandate. The mean daily value across all states is presented for the same timeframe.
Discussion
The effect of mask-wearing on community transmission of SARS-CoV-2 has been the subject of substantial debate, despite evidence of its potential effect to reduce SARS-CoV-2 spread from detailed transmission studies and population-wide data from other respiratory pathogens. In this Article, we present findings from more than 300 000 serial cross-sectional surveys administered daily in June and July, 2020, which confirm that a high percentage of self-reported face mask-wearing is associated with a higher probability of transmission control in US states. Face mask-wearing was more commonly reported among some socioeconomic groups (especially in race groups other than White and respondents with lower income). However, the effect of reported face mask-wearing on lowering the Rt to less than 1—the threshold required for transmission control—was the same despite adjustment for demographic factors, physical distancing, and peak transmissibility during the first wave of infection.
Self-reported mask-wearing is shown to increase the odds of transmission control across all levels of physical distancing, suggesting that any intervention to improve this community-based behaviour might be worthwhile. The absence of a statistically significant change in reported mask-wearing during the 2 weeks following statewide mandates highlights the point that regulation alone might not drive increased masking behaviour. However, we found that there was a general increase in reported mask-wearing before these policies went into effect, which continued after their implementation. Future research should investigate if mask mandates play a role in maintaining this trend. Masking behaviour, assessed from anonymous surveys, might provide insight into where education on the usefulness of masks in areas of low uptake of mask-wearing, or other interventions, should be directed. These results are consistent with case studies of mask-wearing in the USA,13, 14 and potentially provide some insight into why one report found no substantial effect of mask mandates in conjunction with other interventions.15 The data presented here might highlight a gap between governmental policy and user behaviour (proxied by self-reports), but more research is needed.
Our evidence supports the role of mask-wearing in controlling SARS-CoV-2 transmission; however, this ecological study cannot inform questions of causality or generalisable biological mechanisms. It is difficult to disentangle individuals' engagement in mask-wearing from their adoption of other preventive hygiene practices, and mask-wearing might be serving as a proxy for other risk avoidance behaviours not queried (eg, avoiding crowded spaces). Although our findings were the same when controlling for individual-level contacts from the Delphi Research Group survey, a proxy that probably includes other aspects of risk reduction, the possibility of residual confounding by individual hygiene practices that were unaccounted for, such as handwashing, is probable and population-level measures of distancing (such as from the Google community mobility measure) might not be reflective of individual changes. Google community mobility measures rely on mobile phones and might not accurately reflect distancing in areas of lower mobile phone ownership or weaker GPS coverage.20 Additionally, observations from smaller states are over-represented when results are aggregated at the state level, and geospatial aggregations obscure urban and rural heterogeneity that might play a large role in disease transmission and mask-wearing. Although we adjusted for state population density to address this issue, our results might be confounded if the distribution of this density is related to disease transmission and mask-wearing.
In this investigation, mask-wearing was assessed via anonymous internet surveys. Although reported mask-wearing showed a similar geographical distribution to mask-wearing assessed by an alternative instrument (eg, interviews done by the New York Times and Dynata), both of these measures rely on self-reported behaviour and it is unknown how well they are associated with actual user behaviour. Additionally, we used a four-point Likert scale, which might not fully capture the nuances of an individual's behaviour, and our results might not capture the true community variation that would be better represented by a wider range of options. However, in an analysis that weighted Likert responses by expected values, we found our results to be similar to those from the dichotomised four-point scale.
Social desirability bias might also cause individuals to report wearing face masks despite not doing so in practice, or vice-versa, which could bias these findings in either direction. The self-reported mask measures also suffer from survey bias more generally and might be under-sampling some groups, including those with lower levels of formal education or little access to the internet. Although differential participation was addressed with the use of a statistical weighting process to ensure that samples matched official demographic compositions, this survey might not be representative of groups that are also under-sampled in the census or small subgroups for which there was no sample to apply upweighting procedures. Additionally, we did not assess the representativeness of the validating data sets as in the New York Times and Dynata interviews, which might reflect similar biases, nor did we analyse if these results are mirrored outside the USA, where contact patterns and mask-wearing habits might differ substantially.
A state that has high rates of physical distancing might also be subject to additional non-modelled interventions that still have a strong effect, including gathering size reductions, travel limitations, and the closing of businesses.27 Although the physical distancing proxy used here captures the broad activity of individuals that would result from the implementation of these policies, future research should focus on incorporating data from disaggregated interventions with empirical assessments of mask-wearing. However, these measures and our methods do not account for other public health interventions, such as contact tracing and diagnostic testing, which might play a large role in transmission control.22, 28 Additionally, potential Rt and mask-wearing within a state might be the result of transmission before the observed study period. Although we showed that the effect of mask-wearing was robust to peak Rt in the first wave of the epidemic, our methods did not control for time-dependent confounding or variations in mask usage by susceptibility status, both of which might bias the results strongly depending on true biological relationships. For example, if only healthy individuals wear masks, our results could be biased away from the null by highlighting an association between high numbers of healthy people (low Rt) and high rates of mask adoption, when there is no true relationship.
The validity of epidemiological parameters of transmission are only as accurate as the incidence data to which the models are fitted. If states reporting low mask-wearing also under-report incidence (eg, low rates of testing), we might be underestimating the true effect of mask-wearing. Conversely, Rt estimations of transmission are subject to uncertainty, especially towards the end of the time-series before reports are complete.29 Although our results were robust to different estimators, our model does not account for estimation error. Additionally, mask-wearing measures, physical distancing, and Rt all show substantial temporal autocorrelation. To combat this, we dichotomised Rt and aggregated our exposures by week, but further analyses might consider complex time-series models, mechanistic, and quasi-experimental methods to estimate the effect of face masks.
We find a community benefit for face masks, a definition which collectively includes masks of various hypothesised efficacies.30 We did not query specific mask type or the use of face shields in conjunction with masks. The reported association might understate the maximum potential for face masks to curb respiratory transmission, which can only be established through increasing the use of better mask materials (ie, choosing surgical masks over fleece gaiters). Additional study of the effect modification by mask type is necessary to estimate true causal effects.
When considering the various challenges that the US population has faced in slowing the spread of SARS-CoV-2, evidence on the effect of non-pharmaceutical interventions is paramount. Our data suggest that the widespread use of face masks by the general public might aid in limiting the SARS-CoV-2 epidemic as physical distancing restrictions are rolled back around the USA. Given mixed evidence on the effect of mask mandates, but a strengthening body of evidence on the effect of masks, policy makers should consider innovative strategies for evaluating and increasing mask usage to help control the epidemic.
For the up-to-date values for Rt see https://www.rt.live/
For the masks4all database see https://masks4all.co/
For deidentified data see https://www.atscale.com/covidnearyou
Data sharing
Public health practitioners can request direct access to deidentified data online. Anonymous aggregated data are available in a dashboard for the public.31
Acknowledgments
Acknowledgments
We thank Kara Sewalk and Laura Wronski for their assistance. This study was supported by the Flu Lab, Ending Pandemics, and the Centers for Disease Control and Prevention (USA).
Contributors
BR, LFW, and JSB conceived the study. BR, LFW, CMA, and JSB wrote the first draft of the manuscript. JCh, JB, and JCo oversaw and implemented data collection. BR and JSB have verified the underlying data. BR, LFW, MRB, and CMA contributed to the analysis. BR, LFW, JCh, JCo, JS, MUGK, CMA, and JSB contributed to the revision. MRB, LB, JBH, SVS, and JS edited the first draft of the manuscript. All authors contributed to the interpretation of the data, decision to include sensitivity analyses, and editing of the final manuscript. All authors have seen and approve the final text.
Declaration of interests
LB sits on the board of Ending Pandemics and the Skoll Foundation. BR declares funding from Google.org via the Tides Foundation (TF2003–089662) for infectious disease research. JSB declares funding from Google.org via the Tides Foundation (TF2003–089662) for infectious disease research. JS has received fees outside of this work from Business Network International and Merck; declares partial ownership of SK Analytics; and declares funding from the National Science Foundation (DMS-2027369) and the Morris-Singer Foundation. SVS has received funding or fees outside of this work from Pandefense Advisory, Booze Allen Hamilton, BioFire Diagnostics, Iliad Biotechnologies, and Salesforce. LFW declares funding from the National Institutes of Health (NIH; R01 GM122876). CMA declares funding from the NIH (K23-DK120899). MUGK declares funding from the EU Horizon 2020 programme MOOD and a Branco Weiss Fellowship. All other authors declare no competing interests.
Supplementary Material
References
- 1.Zhu N, Zhang D, Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu B, Gutierrez B, Mekaru S. Epidemiological data from the COVID-19 outbreak, real-time case information. Sci Data. 2020;7:106. doi: 10.1038/s41597-020-0448-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaiser Family Foundation State data and policy actions to address coronavirus. Nov 24, 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/state-data-and-policy-actions-to-address-coronavirus/
- 4.Yong E. Everyone thinks they're right about masks: how the coronavirus travels through the air has become one of the most divisive debates in this pandemic. April 1, 2020. https://www.theatlantic.com/health/archive/2020/04/coronavirus-pandemic-airborne-go-outside-masks/609235/
- 5.Clinton J, Cohen J, Lapinski J, Trussler M. Partisan pandemic: How partisanship and public health concerns affect individuals' social mobility during COVID-19. Sci Adv. 2020 doi: 10.1126/sciadv.abd7204. published online Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz J, Sanger-Katz M, Quealy K. A detailed map of who is wearing a mask in the U.S. July 17, 2020. https://www.nytimes.com/interactive/2020/07/17/upshot/coronavirus-face-mask-map.html
- 7.Centers for Disease Control and Prevention Strategies for optimizing the supply of N95 respirators. Nov 23, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
- 8.Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission-the time is now. JAMA. 2020;324:635–637. doi: 10.1001/jama.2020.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hou YJ, Okuda K, Edwards CE. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182:429. doi: 10.1016/j.cell.2020.05.042. 46.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stutt ROJH, Retkute R, Bradley M, Gilligan CA, Colvin J. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the COVID-19 pandemic. Proc Math Phys Eng Sci. 2020;476 doi: 10.1098/rspa.2020.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatzius J, Struyven D, Rosenberg I. Face masks and GDP. Jun 29, 2020. https://www.goldmansachs.com/insights/pages/face-masks-and-gdp.html
- 12.Cowling BJ, Zhou Y, Ip DKM, Leung GM, Aiello AE. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infect. 2010;138:449–456. doi: 10.1017/S0950268809991658. [DOI] [PubMed] [Google Scholar]
- 13.Hendrix MJ, Walde C, Findley K, Trotman R. Absence of apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy - Springfield, Missouri, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:930–932. doi: 10.15585/mmwr.mm6928e2. [DOI] [PubMed] [Google Scholar]
- 14.Wang X, Ferro EG, Zhou G, Hashimoto D, Bhatt DL. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. JAMA. 2020;324:703–704. doi: 10.1001/jama.2020.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brauner JM, Mindermann S, Sharma M. The effectiveness of eight nonpharmaceutical interventions against COVID-19 in 41 countries. medRxiv. 2020 doi: 10.1101/2020.05.28.20116129. published online Oct 14. (preprint) [DOI] [Google Scholar]
- 16.Chan AT, Brownstein JS. Putting the public back in public health — surveying symptoms of COVID-19. N Engl J Med. 2020;383:e45. doi: 10.1056/NEJMp2016259. [DOI] [PubMed] [Google Scholar]
- 17.SurveyMonkey How SurveyMonkey gets its data. www.surveymonkey.com/mp/survey-methodology
- 18.US Census Bureau American Community Survey 2014-2018 5-year estimates now available. Dec 19, 2019. https://www.census.gov/newsroom/press-releases/2019/acs-5-year.html
- 19.Wronski L, Cohen J, Chen J. COVIDNearYou and SurveyMonkey COVID-19 Syndromic Surveillance Survey Instrument. Jan 13, 2021. [DOI]
- 20.Google COVID-19 Community mobility reports. 2020. https://support.google.com/covid19-mobility/answer/9824897?hl=en&ref_topic=9822927
- 21.Delphi Group COVID Symptom Survey. 2020. https://cmu-delphi.github.io/delphi-epidata/symptom-survey/
- 22.Abbott S, Hellewell J, Thompson RN. Estimating the time-varying reproduction number of SARS-CoV-2 using national and subnational case counts. Wellcome Open Res. 2020;5:112. [Google Scholar]
- 23.Rader B, Scarpino SV, Nande A. Crowding and the shape of COVID-19 epidemics. Nat Med. 2020 doi: 10.1038/s41591-020-1104-0. published online Oct 5. [DOI] [PubMed] [Google Scholar]
- 24.Rader B, Astley CM, Sy KTL. Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates. J Travel Med. 2020;27:1–4. doi: 10.1093/jtm/taaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sy KTL, Martinez ME, Rader B, White LF. Socioeconomic disparities in subway use and COVID-19 outcomes in New York City. Am J Epidemiol. 2020 doi: 10.1093/aje/kwaa277. published online Dec 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bollen KA, Jackman RW. Regression diagnostics: an expository treatment of outliers and influential cases. Sociol Methods Res. 1985;13:510–542. [Google Scholar]
- 27.Zheng Q, Jones FK, Leavitt S V. HIT-COVID, a global database tracking public health interventions to COVID-19. Sci Data. 2020;7:286. doi: 10.1038/s41597-020-00610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tian H, Liu Y, Li Y. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gostic KM, McGough L, Baskerville E. Practical considerations for measuring the effective reproductive number, Rt. PLoS Comput Biol. 2020 doi: 10.1371/journal.pcbi.1008409. published online Dec 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stadnytskyi V, Bax CE, Bax A, Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc Natl Acad Sci USA. 2020;117:11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tableau Public SurveyMonkey research profile. https://public.tableau.com/profile/surveymonkey#!/vizhome/CovidNearYouSurveyMonkeyMasks/CNYSVMK
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Public health practitioners can request direct access to deidentified data online. Anonymous aggregated data are available in a dashboard for the public.31


