Abstract
The alarming levels of spread and severity of COVID-19 have dominated global attention. In this time of crisis, there is an urgent need for studies identifying the linkages between the pandemic and social welfare. To help policymakers respond to the situation better, we investigate how the severity of the COVID-19 pandemic can condition people's psychological well-being. Employing the latest weekly panel data within an individual fixed effects framework, we uncover the damaging consequences of the COVID-19 severity, as measured by mortality rate, on the incidences of daily anxiety, worry, displeasure, and depression in the United States. Our work underlines the importance of public spending on mental health, both during and after the pandemic.
Keywords: COVID-19, Mortality rate, Psychological consequences, Mental health
1. Introduction
On March 11, 2020, the World Health Organization (WHO) officially declared Coronavirus Disease 2019 (COVID-19) a pandemic posing a significant threat to humanity. The immediate consequences of COVID-19 have been felt all over the world, highlighted by more than 8 million confirmed cases and 440,000 deaths as of mid-June 2020. In the United States alone, the death toll has climbed above 120,000 and the number is still increasing by hundreds per day. In light of such a humanitarian crisis, it is critical for researchers and policymakers to understand the extent to which the pandemic alters people's health and wellbeing.
In this paper, we evaluate how the severity of the COVID-19 pandemic can condition the psychological well-being of Americans. The contribution of our study is two folds. First, we respond to the urgent need for science-backed research on the pandemic. Second, many prior studies on COVID-19, due to time limitation, are subject to the issue of endogeneity. Thus, to have convincing interpretations, our work employs the latest weekly panel data within an individual fixed effects framework to ensure the internal validity of our estimates. In particular, the use of weekly panel data in a short period of time can reduce the possibility of time-variant confounding factors, and the within-individual comparison approach can absorb the time-constant unobserved characteristics that could contaminate our estimates.
The severity of the pandemic can be linked to individuals’ mental well-being through various channels. For example, as more people got infected and hospitalized, the risks of morbidity and mortality associated with COVID-19 contributed to the rising fear about one's own health and the health of their families. Besides, when the pandemic got more severe, the economy stumbled and individuals were brought to the brink of joblessness, which can psychologically aggravate individuals. Recently, there has been some evidence that COVID-19 is mentally devastating to individuals worldwide. Several observational studies report a high frequency of experiencing mental health symptoms for a sample of Chinese individuals at the initial stage of the pandemic (Wang et al., 2020, Xiao et al., 2020). In Iran, disease prevalence and misinformation contributed to heightening stress and mental morbidity (Zandifar and Badrfam, 2020). In the context of Japan, the outbreak triggered fear and panic behavior such as hoarding and stockpiling resources (Shigemura et al., 2020).
The study utilizes all five current waves of the Household Pulse Survey Public Use File, which is released weekly focusing on American experiences during the COVID-19 pandemic. We measure the pandemic severity by the state-level COVID-19 mortality rate. Given the shortage of testing capability in the early days, mortality rate is currently the best measure of the severity of the pandemic. Besides, Holingue et al. (2020) and Wolf et al. (2020) document that approximately 70% of Americans actively do online searching about COVID-19 and have adequate knowledge about the pandemic. Therefore, it is expected that people may understand the severity of the pandemic via the mortality rate statistic.
Employing the individual fixed effects model, our study uncovers the detrimental consequences of the severity of the COVID-19 pandemic on psychological outcomes. Specifically, an increase of 0.01% in the number of weekly COVID-19 deaths per capita (mortality rate) makes individuals 3.9, 4.4, 4.5, and 3.2 percentage points more likely to experience anxiety, worry, displeasure, and depression on a daily basis, respectively. Taking the fractions of individuals who report daily anxiety, worry, displeasure, and depression as the benchmarks, the estimates correspond to 27%, 44%, 58%, and 41% increases, respectively. Overall, a 0.01% increase in the COVID-19 mortality rate makes individuals 8 percentage points more likely to exhibit at least one of the above-mentioned symptoms on a daily basis, corresponding to a 43% increase relative to the benchmark value. Furthermore, it is worth noting that our benchmarks are the proportions of individuals experiencing psychological issues daily during the pandemic, which are higher than the values in the pre-pandemic period. Therefore, our estimates represent the lower bounds of the psychological impacts of COVID-19 severity.
As the pandemic persists and evolves, not only more studies on the impacts of COVID-19 are needed, but quick and effective mitigation strategies are also required. Our work underlines substantial psychological costs of the COVID-19 severity, thus calling for immediate responses from policymakers in the U.S. and beyond. Governments should not take public spending on mental health lightly, both during and after the pandemic. Monitoring psychological needs and delivering psychological support for the public should be an integral part of the general pandemic health care. Universal coverage of mental health services in healthcare systems could help mitigate the negative consequences of the pandemic severity. It is also important for health officials to have effective communication with the public about disease control and prevention in a timely manner to minimize fear and uncertainty.
The paper proceeds as follows. Section 2 provides a brief discussion of the data. Section 3 presents the empirical methodology. Section 4 discusses the estimating results. Section 5 concludes the study.
2. Data
2.1. Mental health and demographics
Our first primary source of data is the Household Pulse Survey Public Use File (HPS-PUF). The HPS-PUF is conducted by the United States Census Bureau along with five other agencies, namely the Bureau of Labor Statistics, the National Center for Health Statistics, the United States Department of Agriculture's Economic Research Service, the National Center for Education Statistics, and the Department of Housing and Urban Development. This is a rich dataset on American experiences during the COVID-19 pandemic. Surveys are conducted on a weekly basis starting from April 23.
In this study, we utilize all five waves that are currently available to us, including Week 1: April 23–May 5, Week 2: May 7–May 12, Week 3: May 14–May 19, Week 4: May 21–May 26, and Week 5: May 28–June 02. Appending the waves gives us unbalanced panel data because each respondent can only remain in the sample for up to two additional waves. In other words, individuals can participate in a maximum of three consecutive waves of the survey. The replacement of the sample is intended to ease the response burden of selected individuals and the sample size was adjusted each week for an anticipated five percent response rate (U.S. Census Bureau, 2020).1
The HPS-PUF allows us to construct measures reflecting individual mental health. In particular, the respondents were asked about the frequency of psychological symptoms over the previous 7 days, including (i) the frequency of feeling nervous, anxious, or on edge, (ii) the frequency of not being able to stop or control worrying, (iii) the frequency of having little interest or pleasure in doing things, and (iv) the frequency of feeling down, depressed, or hopeless. The respondents’ answers to those questions are codified into a four-point scale as follows: 1—Not at all, 2—Several days, 3—More than half the days, and 4—Nearly every day. To gauge individuals’ psychological state, we construct four indicators, namely, Daily Anxiety, Daily Worry, Daily Displeasure, and Daily Depression. They are computed as one-zero dummies taking the value of one if the answer falls into the worst state (i.e. 4—Nearly every day) and zero otherwise.
Furthermore, we construct an additional measure of mental health. Psychological Distress is an indicator for having at least one of the above-mentioned experiences (anxiety, worry, displeasure, and depression) on a daily basis. In other words, Psychological Distress takes the value of one if at least one of the variables Daily Anxiety, Daily Worry, Daily Displeasure, and Daily Depression equals one, zero otherwise. We believe that this measure (Psychological Distress) more accurately reflects the psychological consequences because individuals do not have to experience all four symptoms to be considered psychologically affected. Finally, information on standard background characteristics, such as gender, race, birth year, educational attainment, marital status, state of residence, and occupation, is obtained directly from the HPS-PUF.
2.2. COVID-19 mortality rate
The severity of the COVID-19 pandemic is proxied by the mortality rate. According to the Centers for Disease Control and Prevention (CDC), the COVID-19 mortality rate is a measure of the frequency of occurrence of death in a defined population during a given interval.2 Our main explanatory variable is COVID-19 Mortality Rate () at the week level for each state. We choose weekly intervals for each state because the HPS-PUF's surveys are conducted on a weekly basis and the lowest residential level is the state. For simplicity, let us consider an individual living in California and surveyed in the first wave (Week 1: April 23–May 5). The COVID-19 mortality rate that he/she is exposed to, as measured by , is the total number of people in California who have died as a result of COVID-19 a week from the survey start date (i.e. from April 17 to April 23), divided by California's population, and multiplied by 10,000.
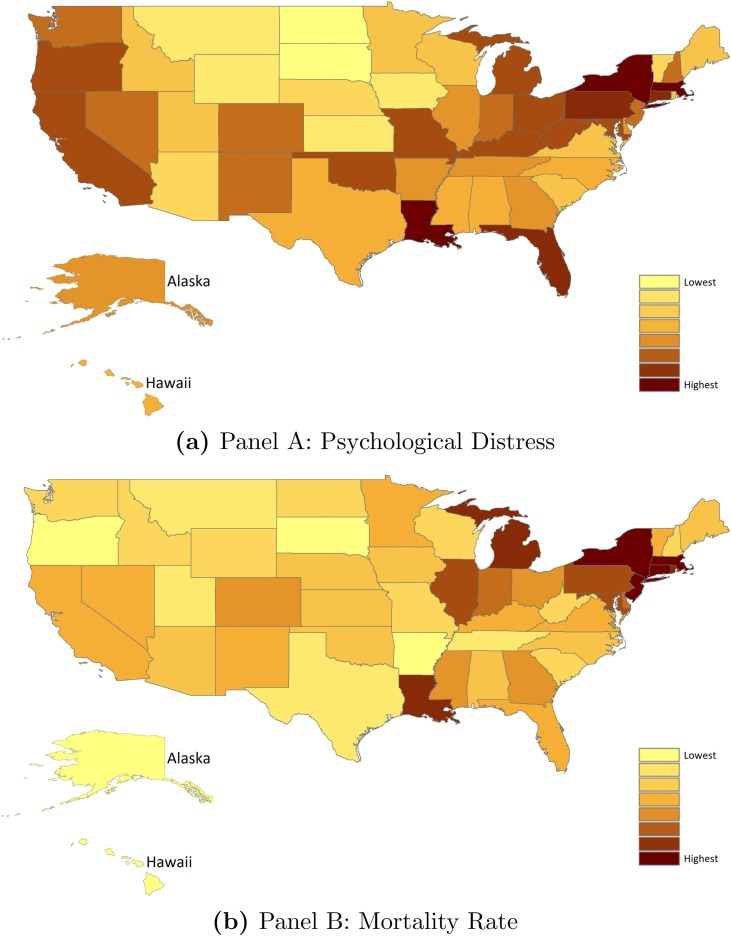
To compute the COVID-19 mortality rate variable , we need both COVID-19 daily deaths and the state population. Since the CDC is not publishing COVID-19 deaths for each state on a daily basis, we rely on the COVID Tracking Project for the statistics.3 It is worth noting that Johns Hopkins also relies on this data for its COVID-19 Testing Insights Initiative in supporting the public and policymakers to understand and make decisions about the pandemic related matters. Last but not least, we obtain the latest state population data from the U.S. Census Bureau. Table 1 presents the descriptive statistics of our dependent and control variables. Table A.2 in the appendix reports the variation in the COVID-19 mortality rate across states and time. Specifically, in each state, the COVID-19 mortality rate is shown for each survey week. Fig. A.1 further provides a visual illustration of the variations in the overall mental health measure (the psychological distress indicator for having at least one of the following experiences: anxiety, worry, displeasure, and depression, on a daily basis) and the COVID-19 mortality rate. Fig. A.1 consists of two maps in Panels A and B which give the overall mental health and mortality rate measures averaged across survey weeks for each state, respectively. The shade represents the severity of the pandemic and overall mental health (e.g. in Panel B, the pandemic is more severe in the darker shaded states).
Table 1.
Summary statistics.
| Mean | S.D. | Obs. | |
|---|---|---|---|
| (1) | (2) | (3) | |
| Panel A: Control variables | |||
| Respondent is white | 0.829 | 0.377 | 455,651 |
| Respondent is black | 0.078 | 0.269 | 455,651 |
| Respondent is Hispanic | 0.083 | 0.276 | 455,651 |
| Age of Respondent | 51.53 | 15.73 | 455,651 |
| Respondent is married | 0.575 | 0.494 | 455,651 |
| Respondent is male | 0.408 | 0.492 | 455,651 |
| Respondent has bachelor's degree | 0.540 | 0.498 | 455,651 |
| Respondent works for government | 0.103 | 0.303 | 455,651 |
| COVID-19 mortality rate | 0.229 | 0.287 | 455,651 |
| Panel B: Outcome variables | |||
| Daily anxiety | 0.147 | 0.354 | 411,366 |
| Daily worry | 0.099 | 0.299 | 411,180 |
| Daily displeasure | 0.077 | 0.267 | 410,950 |
| Daily depression | 0.078 | 0.269 | 411,348 |
| Psychological distress | 0.186 | 0.389 | 409,961 |
Fig. A.1.
COVID-19 mortality rate and mental health. Note: The figure illustrates the variations in average measures of psychological distress (Panel A) and COVID-19 mortality rate (Panel B) across states. Psychological Distress is an indicator for having at least one of the following experiences (anxiety, worry, displeasure, and depression) on a daily basis. The shade represents the severity of the pandemic and overall mental health.
3. Empirical methodology
To examine the extent to which the severity of the COVID-19 pandemic influences the mental health of individuals, we estimate the following model,
| (1) |
where the subscripts , , and refers to the individual, state, and week of survey. The outcome variable represents different measures of individual mental health, including: (i) whether the individual feels anxious on a daily basis (Daily Anxiety), (ii) whether the individual is worried every day (Daily Worry), (iii) whether the individual has little pleasure or interest in things on a daily basis (Daily Displeasure), (iv) whether the individual suffers from depression every day (Daily Depression), and (v) whether the individual has any of the above-mentioned experiences on a daily basis (Psychological Distress).
Our main explanatory variable, , is the COVID-19 mortality rate proxying for the severity of the pandemic. This variable refers to the number of new COVID-19 deaths per capita during the week preceding the survey date in the individual's state of residence (and multiplied by 10,000). The terms and denote state and survey week fixed effects, respectively. The vector is a covariate of background characteristics at the individual level, including age, age squared, marital status, race, gender, occupational sector, and educational attainment. Finally, stands for the error term. Standard errors throughout the paper are clustered at the state-by-week level.
In the model given in equation (1), our identification hinges upon the variation in the exposure to the COVID-19 mortality rate across individuals within the same state. The variation is due to the timing of the survey if it is within state. However, such a between-individual comparison can bias our coefficient of interest if there exist individual-specific characteristics that are correlated with both mental health outcomes and the COVID-19 mortality rate in the state. For example, risk-averse people may temporarily migrate into a state where the outbreak is less severe. If such individuals also tend to take good care of their mental health, then the effects captured by in equation (1) will fail to deliver the causal interpretation.
To tackle these issues, we implement the individual fixed effects model where the identification comes from the within-individual variation in the exposure to the COVID-19 mortality rate in the state of residence at the time of survey, given by,
| (2) |
where stands for individual fixed effects. Our coefficient of interest is now which summarizes the impacts of the COVID-19 severity proxied by the mortality rate on individuals’ psychological health within the individual fixed effects framework. Other notations remain the same. The state fixed effects account for the fact that states vary in their responses to the pandemic. The week fixed effects account for the time-varying aggregate events affecting all states. The within-individual comparison approach will absorb the time-constant individual characteristics that cannot be observed, thus lending support to the internal validity of the estimates. Given that the surveys are conducted on a weekly basis during a short period, the model can account for many characteristics that could vary over time, hence reduces the contamination of such time-variant confounders. Nevertheless, the model cannot control for all individual time-variant factors. If the remaining unobserved individual-specific time-variant characteristics are correlated with state-level COVID-19 mortality rate and individual mental health, our estimates could be biased. Another limitation of our model is the loss of a considerable amount of observations because the panel data is unbalanced.
4. Results
4.1. Main results
The estimated impacts of the COVID-19 severity on mental health are reported in Tables 2 through 6. First, Tables 2 through 5 present the results on the experiences of anxiety, worry, displeasure, and depression separately. Then, Table 6 provides the estimates for the experience of either symptom. For Tables 2 through 5, the dependent variables in Columns 1 through 3 are the constructed indicators for experiencing anxiety, worry, displeasure, and depression on a daily basis (Daily Anxiety, Daily Worry, Daily Displeasure, and Daily Depression). The dependent variables in Columns 4 through 6 are the raw measures of psychological health, i.e. the four-point scale of the frequency of having such feelings (Uncoded Anxiety, Uncoded Worry, Uncoded Displeasure, Uncoded Depression). For Table 6, the outcome variable is the incidence of psychological distress, defined as having at least one of the four symptoms (anxiety, worry, displeasure, and depression) on a daily basis.
Table 2.
Pandemic severity and anxiety.
| Y = Daily anxiety |
Y = Uncoded anxiety |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| COVID-19 mortality rate | 0.030*** | 0.030*** | 0.039*** | 0.116*** | 0.118*** | 0.120*** |
| (0.010) | (0.009) | (0.013) | (0.026) | (0.025) | (0.044) | |
| Controls | ||||||
| Individual fixed effects | . | . | ✓ | . | . | ✓ |
| Individual characteristics | . | ✓ | ✓ | . | ✓ | ✓ |
| State & Week fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 411,366 | 411,366 | 157,760 | 411,366 | 411,366 | 157,760 |
| -squared | 0.002 | 0.031 | 0.816 | 0.004 | 0.071 | 0.882 |
Note: Daily Anxiety is an indicator taking the value of one if the individual feels nervous, anxious, or on edge every day, zero otherwise. Uncoded Anxiety is the frequency of feeling nervous, anxious, or on edge, ranging from 1—not at all to 4—nearly every day. Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. Individual Characteristics include age, age-squared, marital status, race, gender, occupational sector, and educational attainment. With the inclusion of individual fixed effects, time-constant individual characteristics will automatically be dropped due to multicollinearity. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , , ***.
Table 6.
Pandemic severity and psychological distress.
| Y=Psychological distress |
|||
|---|---|---|---|
| (1) | (2) | (3) | |
| COVID-19 mortality rate | 0.043*** | 0.044*** | 0.080*** |
| (0.009) | (0.009) | (0.015) | |
| Controls | |||
| Individual fixed effects | . | . | ✓ |
| Individual characteristics | . | ✓ | ✓ |
| State & week fixed effects | ✓ | ✓ | ✓ |
| Observations | 409,961 | 409,961 | 157,035 |
| -squared | 0.003 | 0.039 | 0.822 |
Note: Psychological Distress is an indicator taking the value of one if the individual has at least one of the following feelings on a daily basis, namely, anxiety, worry, displeasure, and depression, and zero otherwise. Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. Individual Characteristics include age, age-squared, marital status, race, gender, occupational sector, and educational attainment. With the inclusion of individual fixed effects, time-constant individual characteristics will automatically be dropped due to multicollinearity. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , , ***.
Table 5.
Pandemic severity and depression.
| Y = Daily depression |
Y = Uncoded depression |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| COVID-19 mortality rate | 0.018*** | 0.019*** | 0.032*** | 0.118*** | 0.120*** | 0.161*** |
| (0.006) | (0.005) | (0.008) | (0.019) | (0.019) | (0.045) | |
| Controls | ||||||
| Individual fixed effects | . | . | ✓ | . | . | ✓ |
| Individual characteristics | . | ✓ | ✓ | . | ✓ | ✓ |
| State & Week Fixed Effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 411,348 | 411,348 | 157,915 | 411,348 | 411,348 | 157,915 |
| -squared | 0.002 | 0.028 | 0.833 | 0.004 | 0.066 | 0.887 |
Note: Daily Depression is an indicator taking the value of one if the individual feels down, depressed, or hopeless every day, zero otherwise. Uncoded Depression is the frequency of feeling down, depressed, or hopeless, ranging from 1-not at all to 4-nearly every day. Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. Individual Characteristics include age, age-squared, marital status, race, gender, occupational sector, and educational attainment. With the inclusion of individual fixed effects, time-constant individual characteristics will automatically be dropped due to multicollinearity. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , , ***.
As suggested by the National Institute of Mental Health, anxiety, worry, displeasure, and depression can cause serious consequences to personal well-being. While occasional worry or anxiety is a normal part of life, individuals experiencing such feelings on a high-frequency level might suffer from anxiety disorders. People with anxiety disorders might feel restless, wound-up, or on-edge and have difficulty controlling feelings of worry. Constant anxiety and worry can disrupt the everyday routine, social interactions, and personal well-being. Such psychological problems could persist to the future and turn into disruptive behavior disorders as well as failing cognition (Bubier and Drabick, 2009, Vytal et al., 2013). Depression, also referred to as major depressive disorder, is a common but serious mood disorder. Experiencing hopelessness and pessimism as well as a loss of interest and pleasure on a high-frequency level can be associated with major depressive disorder. In the short run, such a mental health problem can negatively influence daily activities. In the long run, depression can be linked to deteriorating cognitive functioning and a higher risk of cardiovascular diseases (Bierman et al., 2005, Penninx, 2017).
Anxiety: Starting with Table 2, we find that the pandemic severity exacerbates the levels of anxiety for individuals. As evident from Column 1, the number of new deaths due to COVID-19 is positively linked to the incidence of anxiety. A 0.01% increase in the mortality rate is associated with the rise in the probability of feeling anxious every day by 3 percentage points. With the introduction of the set of individual controls, the point estimates vary little, as shown in Column 2. The estimation results reported so far come from the variation in the exposure to COVID-19 mortality rate across individuals within the same state.
In Column 3, we make the within-individual comparison in the degree of exposure to the COVID-19 mortality rate. In other words, the individual fixed effects model allows us to see the change in the anxiety level within an individual as the pandemic gets more severe. Our individual fixed effects model suggests that a 0.01% increase in the number of weekly new deaths per capita raises the incidence of daily anxiety by 3.9 percentage points. Compared to the proportion of individuals experiencing anxiety every day in Table 1, the effect on Daily Anxiety implies an increase of approximately 27%. To show that our results are not driven by how we construct the variable Daily Anxiety, we repeat the exercise using the uncoded variable (Uncoded Anxiety) and report the results in Columns 4, 5, and 6. The conclusion remains the same.
Worry: The estimated effects of the COVID-19 severity on worrying are provided in Table 3 . Overall, the pandemic severity aggravates individuals’ psychological health by impeding their ability to control worry. According to the most parsimonious specifications, a 0.01% increase in the COVID-19 mortality rate in the individual's residence state makes him/her 2.5 percentage points more likely to be worried on a daily basis (Column 1). According to the estimate reported in Column 2, the impacts of the COVID-19 mortality rate on the incidence of worry remain virtually unchanged with the inclusion of individual characteristics.
Table 3.
Pandemic severity and worry.
| Y = Daily worry |
Y = Uncoded worry |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| COVID-19 mortality rate | 0.025** | 0.025*** | 0.044*** | 0.111*** | 0.112*** | 0.152*** |
| (0.010) | (0.010) | (0.011) | (0.022) | (0.023) | (0.042) | |
| Controls | ||||||
| Individual fixed effects | . | . | ✓ | . | . | ✓ |
| Individual characteristics | . | ✓ | ✓ | . | ✓ | ✓ |
| State & Week fixed effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 411,180 | 411,180 | 157,748 | 411,180 | 411,180 | 157,748 |
| -squared | 0.002 | 0.025 | 0.827 | 0.004 | 0.068 | 0.886 |
Note: Daily Worry is an indicator taking the value of one if the individual cannot stop or control worry every day, zero otherwise. Uncoded Worry is the frequency of not being able to stop or control worrying, ranging from 1—not at all to 4—nearly every day. Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. Individual Characteristics include age, age-squared, marital status, race, gender, occupational sector, and educational attainment. With the inclusion of individual fixed effects, time-constant individual characteristics will automatically be dropped due to multicollinearity. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , **, ***.
Moving to Column 3, the within-individual estimate is both statistically and economically significant. A 0.01% increase in the COVID-19 mortality rate is associated with the rise in the incidence of daily worry by 4.4 percentage points. Taking the fraction of individuals who report daily worry as the benchmark (Table 1), the estimate implies the average increase of 44%. As shown in Columns 4, 5, and 6, using the raw measure of worry as the outcome variable tells us the same story. The severity of the COVID-19 pandemic is positively linked to the frequency of worry.
Displeasure: We report the estimated effects of the pandemic severity on displeasure in Table 4 . Regardless of the measures used, we find strong evidence that the higher the COVID-19 mortality rate of the state, the more dissatisfaction its residents experience. According to the specification with only state and week fixed effects, a 0.01% increase in the COVID-19 mortality rate raises the likelihood of the individual feeling disinterested in things on a daily basis by 3.1 percentage points (Column 1). Controlling for individual characteristics does not alter the effects of the COVID-19 mortality rate in terms of both economic and statistical senses (Column 2).
Table 4.
Pandemic severity and displeasure.
| Y = Daily displeasure |
Y = Uncoded displeasure |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| COVID-19 mortality rate | 0.031*** | 0.032*** | 0.045*** | 0.111*** | 0.113*** | 0.087* |
| (0.010) | (0.010) | (0.010) | (0.025) | (0.024) | (0.050) | |
| Controls | ||||||
| Individual fixed effects | . | . | ✓ | . | . | ✓ |
| Individual characteristics | . | ✓ | ✓ | . | ✓ | ✓ |
| State & Week Fixed Effects | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 410,950 | 410,950 | 157,642 | 410,950 | 410,950 | 157,642 |
| -squared | 0.002 | 0.025 | 0.797 | 0.004 | 0.063 | 0.867 |
Note: Daily displeasure is an indicator taking the value of one if the individual has little interest or pleasure in doing things every day, zero otherwise. Uncoded Displeasure is the frequency of having little interest or pleasure in doing things, ranging from 1-not at all to 4-nearly every day. Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. Individual Characteristics include age, age-squared, marital status, race, gender, occupational sector, and educational attainment. With the inclusion of individual fixed effects, time-constant individual characteristics will automatically be dropped due to multicollinearity. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , *, ***.
Since the strong effects reported in Columns 1 and 2 might have just captured the confounding influence of unobserved time-invariant individual characteristics simultaneously correlated with the COVID-19 mortality rate and individuals’ displeasure, we tackle the issue by exploiting the within-individual variation in the exposure to the COVID-19 mortality rate. The individual fixed effects estimates are presented in Column 3, pointing to the same direction as those in the remaining columns. A 0.01% increase in the number of weekly new COVID-19 deaths per capita makes the individual 4.5 percentage points more likely to experience displeasure or disinterest on a daily basis, which corresponds to the 58% increase relative to the mean reported in Table 1. Our conclusion is unaffected by the use of the uncoded displeasure variable (Columns 4, 5, and 6).
Depression: We proceed to the relationship between COVID-19 severity and depression. Overall, the estimates shown in Table 5 suggest that a high COVID-19 mortality rate provokes the feelings of depression and hopelessness. According to the most parsimonious specification reported in the first column, a 0.01% increase in the number of weekly new deaths per capita raises the incidences of daily depression by 1.8 percentage points. With the inclusion of individual covariate, the estimated effect slightly increases in both economic and statistical senses (Column 2).
To ensure the internal validity of our estimates for the relationship between COVID-19 mortality rate and depression, we adopt the individual fixed effects model. Evident from Column 3, the individual is 3.2 percentage points more likely to feel depressed and hopeless every day in response to a 0.01% increase in the COVID-19 mortality rate in his/her residence state. Compared to the proportion of individuals reporting daily depression, this effect implies an average increase of 41%. As for the uncoded measure of depression, a higher COVID-19 mortality rate is also positively associated with the frequency of depression, thus keeping our conclusion unchanged.
Psychological distress: Finally, we summarize the impacts of pandemic severity using a single measure, Psychological Distress, which is an indicator taking the value of one if the individual has at least one of the following feelings on a daily basis, namely, anxiety, worry, displeasure, and depression, and zero otherwise. The reason is that experiencing one of these four symptoms is enough to be considered psychologically affected.
The estimated effects of the pandemic severity on the probability of experiencing psychological distress are reported in Table 6. The results show that the more severe the pandemic becomes, the more likely individuals are to have at least one of the four psychologically negative experiences (anxiety, worry, displeasure, and depression) every day. The most parsimonious point to the positive relationship between the COVID-19 mortality rate and the probability of the individual feeling psychologically distressed (Column 1). Controlling for individual characteristics leaves the estimate unchanged (Column 2).
Our most extensive specification in Column 3 suggests that a 0.01% increase in the number of weekly COVID-19 deaths per capita (mortality rate) raises the likelihood of having at least one of the four psychologically negative experiences (anxiety, worry, displeasure, and depression) on a daily basis by 8 percentage points. Taking the fraction of individuals having at least one of such feelings as the benchmark, our estimate represents the 43% increase in the incidence of being psychologically affected daily (i.e. having at least one of the four negative experiences daily).
4.2. Heterogeneity
It is also of interest to explore the heterogeneous impacts of the severity of COVID-19 along the lines of temporal, political, racial, and gender dimensions. The results from the heterogeneity exercises are provided in Table 7 . For each panel in Table 7, each column represents a separate regression and the column heading indicates the dimension of heterogeneity. The dependent variable in all regression is the overall mental health measure, Psychological Distress, which is an indicator for whether the individual has at least one of the four negative psychological experiences (anxiety, worry, displeasure, depression) on a daily basis. All estimates come from the most extensive specification (the specification in Column 3 of Table 6).
Table 7.
Heterogeneity analyses.
| Y=Psychological distress |
|||||
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Panel A: Stages of Pandemic and Political Affiliations | |||||
| Upswing of | Downswing of | Republican in | Democrat in | ||
| Pandemic | Pandemic | 2016 Election | 2016 Election | ||
| COVID-19 mortality rate | 0.404** | 0.104** | 0.085*** | 0.067*** | |
| (0.185) | (0.022) | (0.032) | (0.020) | ||
| Observations | 38,306 | 66,319 | 82,873 | 72,834 | |
| Panel B: Race and Gender | |||||
| White | Hispanic | Black | Male | Female | |
| COVID-19 mortality rate | 0.095*** | 0.014 | 0.075 | 0.065** | 0.101*** |
| (0.020) | (0.040) | (0.049) | (0.031) | (0.023) | |
| Observations | 125,656 | 8,740 | 7,901 | 64,230 | 86,636 |
Note: Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. For each panel in the table, each column represents a separate regression and the column heading indicates the dimension of heterogeneity. The dependent variable is Psychological Distress. All regressions are the most extensive individual fixed effects specifications. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , **, ***.
First, we want to explore if there are heterogeneous impacts between the upswing and the downswing of the pandemic wave. Taking the first week as the reference week, the upswing and the downswing of the pandemic consist of weeks with higher and lower COVID-19 mortality rate than that of the first week, respectively. The results reported in the first two columns of Panel A in Table 7 show that the psychological consequences of the COVID-19 severity are larger during the upswing of the pandemic wave.
Next, we proceed to examine the heterogeneity along the line of political affiliations by categorizing the US states into red and blue states. Since red and blue states may differ in the way of handling the pandemic, we expect the impacts also differ. The results are reported in Columns 3 and 4 of Panel A where the samples consist of individuals residing in states carried by the Republican and Democrat, according to the 2016 election, respectively. We find that the psychological impacts of the pandemic severity are larger for individuals living in states carried by the Republican. Our finding contributes to studies on the partisan differences in the impacts of the COVID-19 pandemic. Some studies show that individuals who identify themselves as Republicans are less likely to be worried about COVID-19 and less likely to adhere to social distancing measures, relative to those who identify themselves as Democrats (Allcott et al., 2020, Calvillo et al., 2020). However, other studies point to the larger psychological impacts on Republicans (Donnelly and Farina, 2020, Zhou et al., 2020). Particularly, Donnelly and Farina (2020) report worse consequences of household income shock for anxiety and depression during the COVID-19 pandemic among individuals living in red states than those living in blue states. Zhou et al. (2020) show that individuals identified as Republicans report higher stress and anxiety compared to Democrats. Our finding on the heterogeneous effects of COVID-19 pandemic severity by political affiliation supports the latter line of studies.
In Panel B, we examine if the psychological impacts of the pandemic severity differ by race and gender. Evident from Columns 1 through 3, there is a lack of statistical evidence for the impacts on Hispanic and Black individuals despite the significant psychological effect among whites. The results are consistent with Wolf et al. (2020) who find that black and Hispanic individuals are more likely than whites to report that they are “not worried at all” about COVID-19. Furthermore, Holingue et al. (2020) document that exposure to the pandemic-related content on social media worsens mental well-being. Compared to whites, the disadvantaged groups of Hispanics and blacks might be less exposed to social media, which could potentially explain the non-existence of the impacts of the pandemic severity among these groups.
Exploring the heterogeneous impacts of COVID-19 severity by gender in Columns 4 and 5 of Panel B, we detect positive and statistically significant effects for both males and females. A 0.01% increase in the COVID-19 mortality rate is associated with the rises in the probability of having at least one of the four negative experiences (anxiety, worry, displeasure, and depression) on a daily basis by 6.5 and 10.1 percentage points among males and females, respectively. The magnitude of the impact is larger for females. The finding is consonant with studies showing that women are particularly vulnerable to adverse events (Shemyakina, 2011, Hamidazada et al., 2019, Le and Nguyen, 2020).
4.3. The death of George Floyd
In this section, we want to test if the impacts of pandemic severity are affected by the death of George Floyd on May 25th. The results from the most extensive specification are presented in Table 8 . The dependent variable is Psychological Distress, an indicator for whether the individual has at least one of the four negative psychological experiences (anxiety, worry, displeasure, depression) on a daily basis. Column 1 gives the estimated impact on overall mental health in all five weeks (corresponding to five survey waves, from April 23 to May 26). The estimate in Column 1 is exactly the same as the estimate in Column 3 of Table 6. In Column 2, we estimate the impact excluding the fifth week (from May 28 to June 2) because George Floyd was killed just before this week, leading to riots across the U.S. in the following weeks. The coefficient estimates in Columns 1 and 2 are not significantly different from each other, suggesting that the psychological effects of the pandemic severity are unlikely to be biased by the occurrence of George Floyd's death (or they have already been captured by week fixed effects).
Table 8.
Are the impacts influenced by the death of George Floyd.
| Y=Psychological distress |
||
|---|---|---|
| All Five Weeks | Excluding Week 5 | |
| (1) | (2) | |
| COVID-19 mortality rate | 0.080*** | 0.084*** |
| (0.015) | (0.015) | |
| Observations | 157,035 | 116,066 |
Note: Our main explanatory variable, COVID-19 Mortality Rate, is the total number of people in the state who have died as a result of COVID-19 a week from the survey start date, divided by the state's population, and multiplied by 10,000. The dependent variable is Psychological Distress. All regressions are the most extensive individual fixed effects specifications. Robust standard errors are clustered at the state-by-week level. Sampling weights are used since the unweighted estimates may be biased in the presence of endogenous sampling. , , ***.
4.4. Discussion
So far, we have provided evidence that the severity of the COVID-19 pandemic proxied by the COVID-19 mortality rate aggravates the psychological health of individuals. Specifically, a 0.01% increase in the COVID-19 mortality rate makes individuals more likely to feel anxious, worried, displeased, and depressed on a daily basis by 3.9, 4.4, 4.5, and 3.2 percentage points, respectively. Taking the fractions of individuals reporting such feelings as our benchmarks, these estimates imply the average increases in the incidences of daily anxiety, worry, displeasure, and depression by 27%, 44%, 58%, and 41%, respectively. Overall, individuals are also 8 percentage points more inclined to be psychologically distressed (i.e. have at least one of those experiences) on a daily basis, corresponding to a 43% increase relative to the benchmark value. As the fractions of individuals with daily psychological issues during the pandemic, our benchmark values are higher than the corresponding values prior to the pandemic. Therefore, our estimates represent the lower bounds of the psychological impacts of COVID-19 severity. We further explore the heterogeneity in the impacts of COVID-19 severity. Particularly, we detect larger consequences during the upswing of the pandemic wave. We also find that the adverse repercussions tend to concentrate on individuals living in states carried by the Republican as well as on the white and female populations.
Our estimated psychological consequences of COVID-19 severity are comparable to those of other disastrous events such as terrorist attacks and hurricanes (Davis et al., 2010, Henriksen et al., 2010). In particular, Henriksen et al. (2010) find that compared to those with no exposure to the 9/11 terrorist attacks, exposed individuals are at least 42 percentage points more likely to experience anxiety. Meanwhile, our results indicate that the incidence of daily anxiety rises by 27% relative to the mean, in response to a 0.01% increase in the COVID- 19 mortality rate. To put it differently, moving from the week with the lowest COVID-19 mortality rate to the week with the highest rate, the incidence of daily anxiety rises by 350% relative to the mean. Davis et al. (2010) uncover the deterioration in mental health among individuals affected by the Katrina hurricane. The authors document an approximately 73% increase in depression compared to the mean depression measure. Meanwhile, we detect a 41% increase in the incidence of daily depression relative to the mean, due to the pandemic severity. Otherwise speaking, our results imply a 540% increase relative to the mean in the incidence of daily depression as moving from the least severe week to the most severe week. Furthermore, because the proportions of individuals who have psychological issues on a daily basis during the pandemic (our benchmark mean values) should be higher than the fractions prior to the pandemic, our estimates are smaller than the true psychological impacts of COVID-19 severity.
The increased feelings of anxiety, worry, displeasure, and depression might precipitate underlying psychiatric problems in response to the heightening severity of the COVID-19 pandemic. As the global pandemic leads to tremendous economic losses, massive business closure, insufficient resources for medical response, and deficient distribution of necessities (Pfefferbaum and North, 2020), such circumstances could translate into substantial emotional distress. In the presence of infection risks and widespread uncertainty, fear can trigger anxiety, depression, and various mental disorders in both healthy individuals and those with pre-existing mental health conditions (Rubin and Wessely, 2020).
The serious consequences associated with the exacerbation of psychological health induced by the severity of the COVID-19 pandemic are far-reaching. In the short run, such emotional distress can interfere with everyday life, for example, insomnia, fatigue, or digestive disorders, thus lowering the quality of life (Nutt et al., 2008). The aggravation of mental health may also engender negative social behaviors such as aggression, violence, or discrimination (Rubin and Wessely, 2020). Furthermore, the pernicious impacts of the deterioration of mental health can linger in the long run, including the risk of cardiovascular diseases, declining cognition, and the development of disruptive behavior disorders (Bubier and Drabick, 2009, Vytal et al., 2013).
Our study emphasizes the damaging psychological costs of the severity of the COVID-19 pandemic, thus calling for immediate actions from policymakers. Interventions that help to mitigate the adverse impacts of the pandemic on mental health should be implemented in a timely manner. Some examples include the universal coverage of mental health services in healthcare systems and the provision of better information on various sources of public support for psychological needs. Communication between health officials and the public about disease control and prevention should be conducted effectively to minimize fear and uncertainty. It is also essential for the government to control the dissemination of non-official information which could create unnecessary anxiety and panic (Johal, 2009).
5. Conclusion
We utilize five weekly rounds of the Household Pulse Survey Public Use File to quantify the psychological impacts of the COVID-19 pandemic severity in the U.S. The severity of the pandemic is proxied by the state-level COVID-19 mortality rate. Our identification strategy hinges upon the within-individual comparison in a short period of time and the individual fixed effects model absorbs the individual-specific time-invariant unobserved characteristics that could contaminate our estimates.
We uncover the detrimental repercussions of the COVID-19 mortality rate on psychological outcomes. An increase of 0.01% in the number of weekly COVID-19 deaths per capita (mortality rate) makes individuals 3.9, 4.4, 4.5, and 3.2 percentage points more likely to feel anxious, worried, displeased, and depressed on a daily basis, respectively. Taking the fractions of individuals reporting such feelings as our benchmark, these estimates imply the average increases in the incidences of daily anxiety, worry, displeasure, and depression by 27%, 44%, 58%, and 41%, respectively. Overall, individuals are also 8 percentage points more inclined to have at least one of those experiences on a daily basis, corresponding to a 43% increase relative to the benchmark value.
More studies on the consequences of the COVID-19 pandemic and effective mitigation strategies are in urgent need as the pandemic persists and evolves. Our work underlines the tremendous psychological cost of the COVID-19 pandemic which tends to be less visible among other consequences such as the loss of lives and the stumble of the economy. The damaging psychological repercussions of COVID-19 severity require prompt actions be taken from policymakers. For example, public spending on mental health should be taken seriously both during and after the pandemic. The general pandemic health care should include the monitoring of psychological needs and the delivery of psychological support for the public. It is also important for health officials to have effective communication with the public about disease control and prevention in a timely manner to curtail panic and uncertainty.
Declarations of interest
None declared.
Footnotes
Nevertheless, the composition of the survey varies little over time as suggested by Table A.1 in the appendix. According to Table A.1, the mean values of demographic characteristics such as race, gender, among others, vary little across the survey weeks.
See www.cdc.gov/csels/dsepd/ss1978/lesson3/section3.html for definitions, applications, and examples.
Further information can be found at www.covidtracking.com.
Appendix A
Table A.1.
Summary statistics by survey week.
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | |
|---|---|---|---|---|---|
| Mean | |||||
| (Standard deviations) | |||||
| Observations | |||||
| Respondent is white | 0.762 | 0.780 | 0.757 | 0.772 | 0.7590 |
| (0.426) | (0.414) | (0.429) | (0.419) | (0.428) | |
| 74,413 | 41,996 | 132,961 | 101,215 | 105,066 | |
| Age of respondent | 50.94 | 52.27 | 51.10 | 52.13 | 51.67 |
| (15.68) | (15.65) | (15.76) | (15.68) | (15.78) | |
| 74,413 | 41,996 | 132,961 | 101,215 | 105,066 | |
| Respondent is married | 0.576 | 0.579 | 0.571 | 0.578 | 0.574 |
| (0.494) | (0.494) | (0.495) | (0.494) | (0.494) | |
| 74,413 | 41,996 | 132,961 | 101,215 | 105,066 | |
| Respondent is male | 0.394 | 0.410 | 0.412 | 0.415 | 0.407 |
| (0.489) | (0.492) | (0.492) | (0.493) | (0.491) | |
| 74,413 | 41,996 | 132,961 | 101,215 | 105,066 | |
Table A.2.
COVID-19 mortality rate across states and time.
| COVID-19 mortality rate |
COVID-19 mortality rate |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| St. | Wk.1 | Wk.2 | Wk.3 | Wk.4 | Wk.5 | All | St. | Wk.1 | Wk.2 | Wk.3 | Wk.4 | Wk.5 | All |
| AK | 0.000 | 0.014 | 0.000 | 0.000 | 0.000 | 0.001 | MT | 0.055 | 0.000 | 0.000 | 0.000 | 0.009 | 0.012 |
| AL | 0.108 | 0.143 | 0.187 | 0.108 | 0.108 | 0.133 | NC | 0.095 | 0.102 | 0.083 | 0.071 | 0.093 | 0.087 |
| AR | 0.026 | 0.076 | 0.030 | 0.039 | 0.023 | 0.034 | ND | 0.079 | 0.105 | 0.092 | 0.118 | 0.066 | 0.091 |
| AZ | 0.108 | 0.163 | 0.145 | 0.152 | 0.111 | 0.134 | NE | 0.108 | 0.082 | 0.087 | 0.128 | 0.102 | 0.103 |
| CA | 0.121 | 0.108 | 0.112 | 0.109 | 0.086 | 0.106 | NH | 0.080 | 0.284 | 0.263 | 0.226 | 0.175 | 0.204 |
| CO | 0.229 | 0.246 | 0.173 | 0.356 | 0.140 | 0.220 | NJ | 1.710 | 1.413 | 1.112 | 0.789 | 0.466 | 1.017 |
| CT | 1.692 | 1.285 | 0.968 | 0.834 | 0.530 | 0.970 | NM | 0.129 | 0.219 | 0.281 | 0.196 | 0.167 | 0.204 |
| DC | 0.735 | 0.749 | 0.749 | 0.611 | 0.486 | 0.667 | NV | 0.150 | 0.137 | 0.121 | 0.124 | 0.080 | 0.117 |
| DE | 0.315 | 0.437 | 0.478 | 0.468 | 0.234 | 0.394 | NY | 1.501 | 1.141 | 0.579 | 0.401 | 0.271 | 0.678 |
| FL | 0.127 | 0.161 | 0.095 | 0.105 | 0.081 | 0.105 | OH | 0.203 | 0.229 | 0.194 | 0.217 | 0.192 | 0.204 |
| GA | 0.207 | 0.170 | 0.140 | 0.183 | 0.165 | 0.169 | OK | 0.109 | 0.076 | 0.046 | 0.048 | 0.048 | 0.059 |
| HI | 0.021 | 0.007 | 0.000 | 0.000 | 0.000 | 0.003 | OR | 0.030 | 0.040 | 0.030 | 0.019 | 0.009 | 0.024 |
| IA | 0.101 | 0.192 | 0.236 | 0.220 | 0.248 | 0.209 | PA | 0.519 | 0.828 | 0.470 | 0.411 | 0.303 | 0.463 |
| ID | 0.071 | 0.016 | 0.011 | 0.027 | 0.027 | 0.030 | RI | 0.899 | 1.032 | 0.653 | 0.729 | 0.928 | 0.808 |
| IL | 0.438 | 0.517 | 0.543 | 0.434 | 0.372 | 0.463 | SC | 0.079 | 0.094 | 0.106 | 0.052 | 0.098 | 0.086 |
| IN | 0.277 | 0.354 | 0.295 | 0.329 | 0.188 | 0.280 | SD | 0.022 | 0.111 | 0.133 | 0.044 | 0.044 | 0.071 |
| KS | 0.096 | 0.058 | 0.041 | 0.021 | 0.069 | 0.052 | TN | 0.041 | 0.048 | 0.067 | 0.033 | 0.059 | 0.052 |
| KY | 0.124 | 0.096 | 0.071 | 0.107 | 0.031 | 0.081 | TX | 0.045 | 0.053 | 0.072 | 0.057 | 0.041 | 0.055 |
| LA | 0.704 | 0.605 | 0.409 | 0.390 | 0.155 | 0.388 | UT | 0.037 | 0.046 | 0.043 | 0.046 | 0.040 | 0.042 |
| MA | 1.357 | 1.198 | 1.118 | 0.797 | 0.591 | 0.987 | VA | 0.163 | 0.218 | 0.166 | 0.141 | 0.234 | 0.180 |
| MD | 0.477 | 0.500 | 0.480 | 0.378 | 0.373 | 0.435 | VT | 0.127 | 0.048 | 0.000 | 0.016 | 0.016 | 0.037 |
| ME | 0.111 | 0.052 | 0.045 | 0.030 | 0.067 | 0.060 | WA | 0.088 | 0.072 | 0.108 | 0.069 | 0.065 | 0.084 |
| MI | 0.724 | 0.403 | 0.290 | 0.229 | 0.164 | 0.326 | WI | 0.089 | 0.080 | 0.085 | 0.072 | 0.092 | 0.084 |
| MN | 0.156 | 0.240 | 0.226 | 0.221 | 0.221 | 0.214 | WV | 0.090 | 0.028 | 0.051 | 0.045 | 0.017 | 0.046 |
| MO | 0.086 | 0.131 | 0.183 | 0.138 | 0.058 | 0.124 | WY | 0.088 | 0.000 | 0.000 | 0.071 | 0.053 | 0.042 |
| MS | 0.204 | 0.385 | 0.238 | 0.291 | 0.324 | 0.281 | Avg. | 0.293 | 0.291 | 0.244 | 0.209 | 0.161 | 0.229 |
Note: The table presents COVID-19 mortality rates across states for each survey week. Wk.1, Wk.2, Wk.3, Wk.4, and Wk.5 stand for Week 1 (April 23–May 5), Week 2 (May 7–May 12), Week 3 (May 14–May 19), Week 4 (May 21–May 26), and Week 5 (May 28–June 2) surveys, respectively. The All Column indicates the weighted average (by sample size) of mortality rates across weeks.
References
- Allcott H., Boxell L., Conway J., Gentzkow M., Thaler M., Yang D.Y. NBER Working Paper. (w26946); 2020. Polarization and public health: Partisan differences in social distancing during the Coronavirus pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman E.J.M., Comijs H.C., Jonker C., Beekman A.T.F. Effects of anxiety versus depression on cognition in later life. Am. J. Geriatr. Psychiatry. 2005;13(8):686–693. doi: 10.1176/appi.ajgp.13.8.686. [DOI] [PubMed] [Google Scholar]
- Bubier J.L., Drabick D.A. Co-occurring anxiety and disruptive behavior disorders: The roles of anxious symptoms, reactive aggression, and shared risk processes. Clin. Psychol. Rev. 2009;29(7):658–669. doi: 10.1016/j.cpr.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvillo D.P., Ross B.J., Garcia R.J., Smelter T.J., Rutchick A.M. Political ideology predicts perceptions of the threat of covid-19 (and susceptibility to fake news about it) Soc. Psychol. Personal. Sci. 2020;11(8):1119–1128. [Google Scholar]
- Davis T.E., III, Grills-Taquechel A.E., Ollendick T.H. The psychological impact from hurricane Katrina: Effects of displacement and trauma exposure on university students. Behav. Therapy. 2010;41(3):340–349. doi: 10.1016/j.beth.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly R., Farina M.P. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Soc. Sci. Med. 2020:113557. doi: 10.1016/j.socscimed.2020.113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidazada M., Cruz A.M., Yokomatsu M. Vulnerability factors of Afghan rural women to disasters. Int. J. Disaster Risk Sci. 2019;10(4):573–590. [Google Scholar]
- Henriksen C.A., Bolton J.M., Sareen J. The psychological impact of terrorist attacks: examining a dose-response relationship between exposure to 9/11 and Axis I mental disorders. Depression Anxiety. 2010;27(11):993–1000. doi: 10.1002/da.20742. [DOI] [PubMed] [Google Scholar]
- Holingue C., Badillo-Goicoechea E., Riehm K.E., Veldhuis C.B., Thrul J., Johnson R.M., Kalb L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: Findings from American trend panel survey. Prevent. Med. 2020;139:106231. doi: 10.1016/j.ypmed.2020.106231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johal S.S. Psychosocial impacts of quarantine during disease outbreaks and interventions that may help to relieve strain. N. Z. Med. J. 2009;122(1296):47–52. [PubMed] [Google Scholar]
- Le K., Nguyen M. Aerial bombardment and educational attainment. Int. Rev. Appl. Econ. 2020;34(3):361–383. [Google Scholar]
- Nutt D., Wilson S., Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin. Neurosci. 2008;10(3):329. doi: 10.31887/DCNS.2008.10.3/dnutt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx B.W. Depression and cardiovascular disease: epidemiological evidence on their linking mechanisms. Neurosci. Biobehav. Rev. 2017;74:277–286. doi: 10.1016/j.neubiorev.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020:368. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Shemyakina O. The effect of armed conflict on accumulation of schooling: Results from Tajikistan. J. Develop. Econ. 2011;95(2):186–200. [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020;74(4):281. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2020). Source of the Data and Accuracy of the Estimates for the 2020 Household Pulse Survey. Available at: https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Source-and-Accuracy-Statement-May-28-June2.pdf.
- Vytal K.E., Cornwell B.R., Arkin N.E., Letkiewicz A.M., Grillon C. The complex interaction between anxiety and cognition: insight from spatial and verbal working memory. Front. Human Neurosci. 2013;7:93. doi: 10.3389/fnhum.2013.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf M.S., Serper M., Opsasnick L., O’Conor R.M., Curtis L.M., Benavente J.Y., Russell A. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the US outbreak: a cross-sectional survey. Ann. Inter. Med. 2020 doi: 10.7326/M20-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Science Monitor: Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.923921. e923921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry. 2020:51. doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., MacGeorge E.L., Myrick J.G. Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. Int. J. Environ. Res. Public Health. 2020;17(17):6315. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]