Abstract
Background
Telecardiology has the advantage of reducing patient's access time to the hemodynamics units. Data from literature show a reduction in ST-elevation myocardial infarction (STEMI) during COVID-19 pandemic. However, there is a low number of studies on the impact of telecardiology during the pandemic.
Methods
Our telecardiology system is composed of a Hub-and-Spoke network of hospitals and ambulances that ensures a rapid exchange of information allowing STEMI patients to be treated in the shortest time possible. We compared data from electrocardiograms (ECGs) transmissions and STEMI diagnosis collected between February and April 2020 with the data from the same period of 2019.
Results
Despite a significant reduction of ECGs transmissions from the telecardiology network was observed, the number of diagnosed STEMI during 2020 was stable and did not show any significant difference compared to 2019. The total number of STEMI diagnosis in the months under examination during 2019 were 47 out of 7463 ECGs (0.63%), while in 2020 were 48 out of 5797 ECGs (0.83%).
Conclusions
The efficiency of our telecardiology system along with the low spread of the infection in our region contributed to maintaining the number of STEMI diagnosis and patient’s care in line with the past even during the pandemic.
Keywords: COVID-19, Telecardiology, STEMI, Health services
1. Introduction
Many studies have shown the usefulness of a telecardiology system for the early diagnosis of acute myocardial infarction and consequent reperfusion time reduction [1]. However, most of the results highlighted by these studies derive from telecardiology projects that are not part of an emergency network and thus are not an integral part of the clinical routine of several territorial and hospital health units [2], [3], [4]. In COVID-19 era, there are no studies on the role of telecardiology systems on STEMI myocardial infarction. Italy was one of the countries most affected by the pandemic [5], especially the North of the country. Studies published so far have shown a reduction in patients who have sought Acute Myocardial Infarction (AMI) treatment in all countries [6], [7], [8]. In this study, we present the hospitalizations data for ST-Elevation Myocardial Infarction (STEMI) during the COVID-19 pandemic period in the intensive care units of our Provincial Health Authority (ASP) of Cosenza which is one of the largest provinces in Italy. Due to its complex and particular geography the city has an active telecardiology system that has been fully integrating hospitals within the territory for five years [9].
2. Methods
2.1. Organization of the telecardiology system
The sanitary district of Cosenza is an area with a complex geography (41% of mountains, 49% of hills, and 10% of plains) covering a region of 6700 km2. The district is located in the northern part of Calabria which is a region in the south of Italy with a total population of 800,000 inhabitants.
Our telecardiology system has been designed to manage both the emergency network and the daily clinical practice. The system connects the ambulances with hub and spoke centers and shares a common database for storing ECGs. The ambulance staff was trained in both the management of patients with STEMI and the use of defibrillators. They were also provided with ECG devices equipped with 3G connection for the transmission of real-time 12 leads ECG to the Emergency ambulance coordinating center, the Hemodynamics room and the Coronary Care Unit (CCU).
The telecardiology system uses a modern technology, the MUSE information system by GE Healthcare, which allows to easily manage the entire cardiological workflow on a dedicated protected server which is accessible from any location through a web-based interface protected by login and password.
The cardiologists in charge of reporting medical findings from the ECG are provided with dedicated smartphones and tablets to allow quickly transmission from any place.
2.2. Operating processes and data flow
The main steps of the process can be summarised into the following phases:
-
•
Phase 1 (acquisition of cardiological examination): performing ECG.
-
•
Phase 2 (sending cardiological examination and reporting): ECG transmission to the reporting station for real-time assessment and, if necessary, teleconsultation with a cardiologist.
-
•
Phase 3 (Archiving and ECG comparison): each ECG is acquired with optical reading, classified using a unique identification number linked to the patient, and finally archived. The system allows immediate visualization of all the ECGs previously acquired and stored in the archive.
2.3. Data collection and statistical methods
We collected data for three months, from February to April 2020, focusing on STEMI hospitalizations during the COVID-19 pandemic. The total number of electrocardiograms transmitted (ECG) from hospital wards, territorial First Aid centers (FAC), Emergency Rooms (ER) and emergency systems with Ambulances were collected. These data were compared with those stored in our archive from the same months of 2019. Difference between the number of transmissions and STEMI diagnosis that occurred during the COVID-19 pandemic period and the same months of the previous year were statistically tested using the Pearson χ2 test.
3. Results
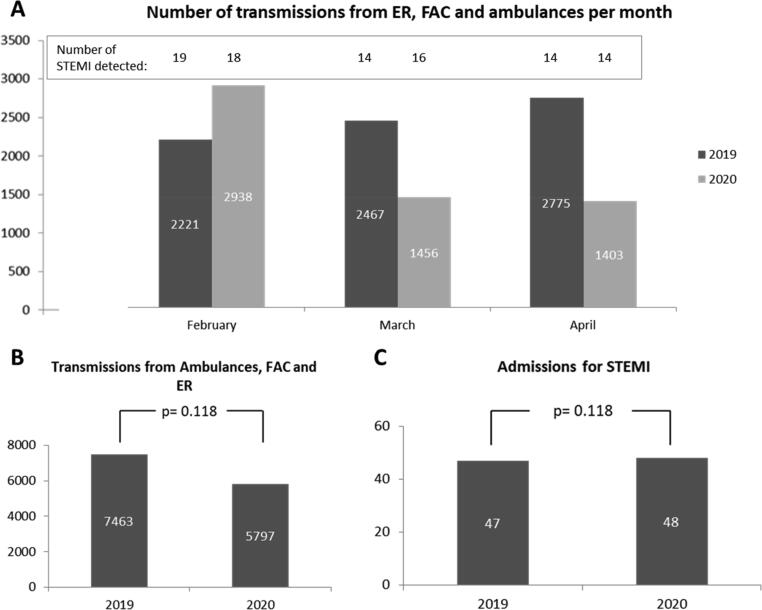
The three months of 2020 showed a 37.5% reduction in ECG transmissions with 15,927 ECG transmitted against the 25,496 of the same period in 2019. The number of transmissions during the month of February resulted less affected by COVID-19 pandemic as shown in Fig. 1A. On the other hand, if we consider March and April separately, we noted a much more significant reduction in ECG transmission, with a total of 17,458 transmissions in 2019 against the 7856 in 2020 with a reduction of 55%.
Fig. 1.
(A) Number of transmissions from ER (Emergency room), FAC (First Aid centers) and ambulances per month with the number of diagnosed STEMI. (B) Comparison of total number of transmissions for 2019 and 2020 (during COVID-19 pandemic). (C) Comparison of total number of STEMI for 2019 and 2020 (during COVID-19 pandemic).
In the three months of the observation, the ECGs transmitted in emergency by the ER, Ambulances and FAC were 7463 in 2019 and 5797 in 2020 with a reduction of 29.8% (Fig. 1B). As in the previous case, if we account only for the month of February, the decrement of ECGs transmissions is also more significant, with 6042 transmissions in 2019 versus 2859 in 2020 with a consequent reduction of 52.7%.
The total number of STEMI diagnosis in the months under examination in 2019 was 47 out of 7463 ECGs (0.63%) while in 2020 it was 48 on a total of 5797 ECG (0.83%). The difference between the two years did not show any statistical significance (p = 0.118). If we differentiate the STEMI according to the origin, the diagnosis transported by the 118 emergency service were 14 in 2019 out of 250 (5.6%) ECGs transmitted by ambulances, and 13 in 2020 out of 183 ECGs (7.1%). On the other hand, the number of STEMI diagnosis coming from the ER and FAC were 33 in 2019 out of 7213 ECGs (0.46%) and 35 in 2020 from a total of 5614 ECG (0.62%).
There was no reduction in the number of STEMIs in each individual month examined as it is showed in Table 1.
Table 1.
Data of transmission and diagnosed STEMI per month compared for 2019 and 2020.
| February |
March |
April |
Total |
|||||
|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| Total ECG evaluated | 8038 | 8071 | 8830 | 3865 | 8628 | 3991 | 25,496 | 15,927 |
| ECG transmitted by ambulances, FAC, ER | 2221 | 2938 | 2467 | 1456 | 2775 | 1403 | 7463 | 5797 |
| STEMI | 19 | 18 | 14 | 16 | 14 | 14 | 47 | 48 |
4. Discussion
The data from this analysis demonstrated and confirmed a dramatic reduction in total number of ECG transmissions, both from hospital departments and ER, FAC and ambulances. Conversely, the data on the number of diagnosed STEMI in our analysis are in countertrend with what has been published so far, since we did not find a significant reduction during the COVID-19 pandemic [6], [7]. It is not immediate to give an explanation for these findings, but surely a multiplicity of factors contributed to the phenomenon.
First of all, it is necessary to identify the most critical issues that may have contributed to a significant reduction of STEMI diagnosis during the pandemic as reported in previously published analyses:
-
(i)
Late presentation or no-show in hospital due to the patient's fear of being infected, with a consequent increase in the risk of death;
-
(ii)
Inadequate health system, due to overload or lack of adequate controls, and poor ability to develop resilient systems that are able to speed up the diagnosis and protect critical patients.
In our case, the telecardiology system was already active and consolidated over five years. The system was not only dedicated to the emergency but was integrated in the whole territory of the ASP and in the hospitals. Therefore, it was possible to take charge of the cardiological patients in all the phases, playing a key role for the safety of critical patients. A real-time exchange between hospitals and ambulances is essential because it allows to immediately view and compare the patient's ECG history for quick and specific decisions, especially in cases of emergency and regardless of the distance from adequate clinical facilities.
Therefore, patients benefited from a fully integrated system of telecardiology that contributed to maintain the number of STEMI diagnosis in line with the past, without any reduction. Furthermore, it has to be pointed out that the low spread of the pandemic in our territories certainly was among the causes that failed to reduce the number of STEMI diagnosis. The percentage of STEMI compared to the total number of ECGs indicates that calls to ambulances or access to the ERs were even more appropriate in 2020 during COVID-19 pandemic than in 2019.
The capillarity of the system throughout the territory, the cultural revolution and the awareness of this system that involved citizens, family doctors and emergency workers made a less “distant” diagnosis possible transforming the system in a “proximity” telecardiology.
Important considerations emerge from these findings as pandemics pose great challenges to healthcare. Although telehealth does not solve all of the issues, structures, such as ours, which have already invested in telemedicine are well positioned to ensure better management of patients with STEMI even during COVID pandemic [10], [11], [12]. Moreover, it is certain that who have already invested in telemedicine is well positioned to ensure appropriate pathways and timely care to patients. A telecardiology system like ours may also be helpful in the future beyond COVID-19. Indeed, a well-integrated and even more widespread telecardiology system may facilitate the approach of patients to health services. For instance, first-aid stations of small villages may benefit from remote and rapid cardiologic advice without the need to transfer patients to the hospital. Furthermore, in the future this system may be enhanced with the possibility to perform rapid troponin test both in the comfort of the patient's home and aboard the ambulance. Finally, this infrastructure could also be helpful to prevent ED visits with economic benefits for society and hospitals. Indeed, telecardiology may be extended to televisit from which bedridden hearth failure patients may benefit avoiding relatives to accompany them to the hospital and saving travel costs. In a similar manner, hospitals may have a positive economic impact. Indeed, medical data transmissions and rapid diagnosis may reduce hospital stay resulting in a money-saving because of early discharge. Telecardiology makes the emergency network a safe and fast link between hospitals within the territory helping to manage resources effectively and align with patients' behaviors and health-care needs during epidemics and beyond.
5. Conclusions
This analysis highlighted that despite the reduction in number of ECGs transmissions during COVID-19 pandemic compared to the same period in 2019, the number of diagnosed STEMI resulted equivalent because of a telecardiology system that is fully integrated in the territory and trusted by patients. The low spread of the infection in our territory also had an impact. A resilient health system that uses telecardiology to reduce time and improve acute care pathways allows to be more protective and efficient towards vulnerable patients.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors would like to thank Gianluca Ceravolo for his assistance in manuscript drafting.
Data availability
The data underlying this article are available in the article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Wu J., Hall M., Dondo T.B. Association between time of hospitalization with acute myocardial infarction and in-hospital mortality. Eur. Heart J. 2019 Apr 14;40(15):1214–1221. doi: 10.1093/eurheartj/ehy835. [DOI] [PubMed] [Google Scholar]
- 2.Brunetti N.D., Bisceglia L., Dellegrottaglie G. Lower mortality with pre-hospital electrocardiogram triage by telemedicine support in high risk acute myocardial infarction treated with primary angioplasty: preliminary data from the Bari-BAT public Emergency Medical Service 118 registry. Int. J. Cardiol. 2015;185:224–228. doi: 10.1016/j.ijcard.2015.03.138. [DOI] [PubMed] [Google Scholar]
- 3.Rasmussen M.B., Frost L., Stengaard C. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triage and treatment of STEMI. Heart. 2014;100(9):711–715. doi: 10.1136/heartjnl-2013-304576. [DOI] [PubMed] [Google Scholar]
- 4.Molinari G., Molinari M., Di Biase M., Brunetti N.D. Telecardiology and its setting of application: An update. J. Telemed. Telecare. 2018 Jun;24(5):373–381. doi: 10.1177/1357633X16689432. [DOI] [PubMed] [Google Scholar]
- 5.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 6.De Rosa S., Spaccarotella C. Basso C et al Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020:1–6. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in STsegment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J. Am. Coll. Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam C.F., Cheung K.S., Lam S. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ. Cardiovasc. Qual. Outcomes. 2020 Apr;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bisignani G., De Bonis S., Bisignani A., Verta A. Telecardiologia: aspetti clinici, tecnici e sociali. Il progetto dell’ASP di Cosenza. G. Ital. Cardiol. 2016;17(12):959–965. doi: 10.1714/2612.26888. [DOI] [PubMed] [Google Scholar]
- 10.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19 N Engl. J. Med. 2020 Apr 30;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 11.Ardati A.K., Mena Lora A.J. Be Prepared. Circ. Cardiovasc. Qual. Outcomes. 2020 Apr;13(4) doi: 10.1161/CIRCOUTCOMES.120.006661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller A.C., Ward M.M., Ullrich F., Merchant K.A.S., Swanson M.B., Mohr N.M. Emergency department telemedicine consults are associated with faster time-to-electrocardiogram and time-to-fibrinolysis for myocardial in- farction patients. Telemed. J. E Health. 2020 doi: 10.1089/tmj.2019.0273. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article.