Abstract
A ubiquitous component of cell membrane, phosphatidylserine (PS), is likely to play a major, but as yet unrecognized, role in the thromboinflammation of COVID-19 and other critical illnesses. PS is present in all plasma membranes but is “hidden” on the inner surface by the action of an ATP-requiring enzyme. Failure of PS to be sequestered on the inner surface of cell membranes, release of PS-containing microparticles from cells, or shedding of enveloped viruses allows it to interact with extracellular proteins, including those of the coagulation and complement systems. Detection and quantification of circulating PS is not standardized, and current methodologies have either focused on circulating cellular elements or subcellular plasma components, but not both. PS may also promote thromboinflammation without circulating if expressed on the surface of endothelial cells, a condition that might only be documented if novel imaging techniques are developed. Research into the role of PS in inflammation and coagulation, called here a “procoagulant phospholipidopathy” may provide novel insights and therapeutic approaches for patients with a variety of illnesses.
Keywords: Coagulation, Thrombosis, Phosphatidylserine, Thromboinflammation, COVD-19
Coagulation; Thrombosis; Phosphatidylserine; Thromboinflammation; COVD-19.
1. Introduction
From the beginning of the COVID-19 pandemic, observers have noted a high incidence of thrombosis involving both the arterial and venous systems and a syndrome of COVID-19 associated coagulopathy, sometimes denoted as “thromboinflammation” has become recognized [1, 2]. Left unanswered is the question “Is COVID thromboinflammation a unique entity, or simply a more highly reported upon accompaniment of other critical illnesses”? Certainly other severe viral infections, including Ebola [3], hantavirus [4], Crimean Congo hemorrhagic fever [5], Marburg virus [6] and Dengue hemorrhagic fever [7] have been associated with coagulopathy. Perhaps the wide-spread recognition of COVID-19 coagulopathy is simply due to the fact that it has occurred in large numbers of people living in higher-income nations in an era where rapid dissemination of information is possible because of the internet, rather than a unique pathophysiology.
Observations of thrombosis detected both macroscopically (clinically) and microscopically have alerted many to the occurrence of endothelial infection and inflammation along with activation of the complement system [8, 9, 10]. Experts have quickly assembled lists of potential points of intervention and drugs that might target both the coagulation and complement systems, interrelated as they are in many types of inflammation [11, 12].
Absent from discussions of COVID-19 pathophysiology (or potential treatment) is a molecule long recognized to play a role in normal human physiology but under-recognized as a significant actor in pathophysiology, the phospholipid phosphatidylserine (PS). A ubiquitous component of the inner surfaces of plasma membranes, PS is always present at sites of inflammation and cell death, but is never considered to be an active participant in causing tissue injury.
2. Phosphatidylserine, coagulation and thrombin generation
PS is one of the more abundant phospholipids of plasma membranes but is only found on the inner surface of plasma membranes under normal conditions. This is due to the action of an ATP-dependent “flippase”, an enzyme that quickly moves any PS that diffuses to the external plasma membrane, back to the cell's interior [13, 14]. Upon activation or injury, cells may “expose” PS on their external surfaces, which allows coagulation proteins to gather onto a previously “non-thrombogenic” membrane surface, interacting in the coagulation cascade to generate the enzyme thrombin. Thrombin is a key enzyme in the thromboinflammatory process, not only because it generates fibrin clots but because a number of cells known to be involved in inflammation express thrombin receptors, including platelets, neutrophils, endothelial cells, macrophages, monocytes, smooth muscle cells and fibroblasts (reviewed in [15]). Thrombin generation may play an important role in both acute COVID-19 infection as well as the chronic problems affecting a subset of infected individuals.
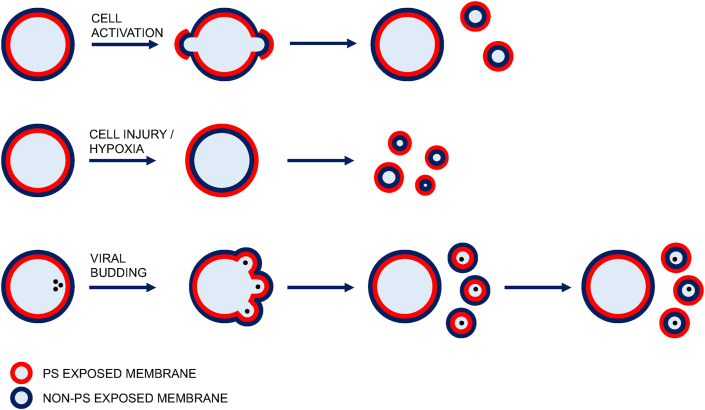
Although the exposure of PS on intact platelet surfaces has been most intensively studied, PS exposure also occurs on platelet fragments (“microparticles”) and on the surface of a variety of other cells and cell-derived microparticles, including erythrocytes [16, 17], tumor cells [18, 19], neutrophils [20], monocytes [21], and endothelial cells [22, 23]. PS may also be exposed on the surface of cells undergoing “programmed cell death” (apoptosis) as well as other types of cell death [24, 25] (Figure 1). Students of blood coagulation have concluded that exposure of PS is a major regulator of the blood coagulation system [26]. Despite a vast literature on “hypercoaguable states”, both congenital and acquired, PS remains unrecognized by those who itemize the list of potential participants in thromboinflammation. In some clinical settings procoagulant phospholipids may play an active role in promoting tissue injury, inflammation and thrombosis, a condition that might appropriately be called a “procoagulant phospholipidopathy”. As with other intracellular molecules such as nucleotides [27], DNA [28], histones [29], polyphosphates [30], RNA [31], and actin [32] that play a role in pathophysiologic states, procoagulant phospholipids may not be easily quantified in circulating blood from healthy subjects.
Figure 1.
Phosphatidylserine exposure on the outside of cells and microparticles – Phosphatidylserine (PS) is maintained on the inner surface of the plasma membrane of all cells. Several mechanisms can lead to the “exposure” of PS on the external surface of cells. Physiologic or pathologic “activation” of cells can lead to exposure of phosphatidylserine (PS) on the external surface of cells, or microparticles released by cells. Enveloped viruses bud from host cells, resulting in PS-bearing virions released into the intra- and extra-vascular spaces, depending upon the location of the infected cell.
3. PS exposure in the blood due to endothelial infection by enveloped viruses
Enveloped viruses are so named because they exit from host cells by the process known as “budding”, wherein the viral genetic material leaves the host cell with a coating (“envelope”) of plasma membrane. In many severe viral infections involving enveloped viruses, the infectious particles themselves likely mediate activation of the coagulation system directly (rather than simply stimulating a host inflammatory response) because the PS in those envelopes is not maintained on the interior of the viral particle [33]. The “exposed” PS thereby provides a surface for assembly of plasma coagulation proteins, which generate thrombin, as first shown for cytomegalovirus [34] and subsequently HIV-1 [35]. It is likely that this occurs with other severe viral infections accompanied by coagulopathy and hemorrhage. Further, “exposed” PS facilitates viral infection of some cells [36]. Targeting of PS in such infections has been proposed as a therapeutic goal [37].
The virus responsible for the COVID-19 pandemic is an enveloped virus whose main portal of entry into a variety of cells is the protein called angiotensin converting enzyme 2 receptor (ACE2R) (reviewed in [38]). This protein is found on many cell types, including epithelial cells, endothelial cells and leukocytes. Its expression on the surface of the endothelial cells means that the release of viral particles from the infected cells introduces PS-expressing particles directly into the blood stream rather than the extravascular space. It is currently unknown what proportion of PS released from other types of cells might also find its way into the circulation from the interstitial space. Given the wide-spread organ dysfunction that is seen in some patients with COVID-19 infection, release of PS from non-endothelial cells is likely to be clinically significant in some patients.
4. Measuring circulation phosphatidylserine (PS)
Two methods have been used to detect circulating PS in blood, but neither has been perfected and there is no agreed upon “gold standard” for either approach. Most of the published literature has used flow cytometry to detect microparticles (also called microvesicles), which can be found in the circulation of patients with a variety of diseases including cancer [39], as well as kidney [40], lung [41] and cardiovascular diseases [42, 43]. Importantly, detailed analysis of platelet-derived microparticles has shown that all microparticles are not equally thrombogenic [44]. Standardization of detection and reporting of microparticles (only some of which are pro-thrombotic) is an important area of investigation [45].
Blood coagulation tests have been adapted to detect circulating PS [46, 47, 48]. Such tests have not been widely adopted, in large part because of a lack of appreciation of the importance of PS in human disease but also because they are technically demanding and require almost immediate testing of collected specimens to avoid artifactual “exposure” of PS on blood cell or fragments after venipuncture. Such tests are typically performed on plasma, which can be prepared by any of a number of centrifugation maneuvers, but the details of centrifugation (often taken for granted in clinical studies) may itself influence the apparent amount of circulating PS [46, 49]. Importantly, methods of measuring circulating PS in whole blood have not been developed, and all published studies to date have excluded circulating blood elements.
5. How could recognition of PS's role in pathophysiology improve health care?
Treatments to ameliorate PS exposure would be a clear avenue to explore. Since PS is known to be “neutralized” (from a coagulation standpoint) by proteins such as annexin V [50] and lactadherin [51] it would be logical to explore their use as therapeutics. Unlike lactadherin which is glycosylated, annexin V (a circulating human plasma protein [52]) is not, and can be produced by bacteria as a monomer, dimer [53], or chimeric fusion protein [54, 55]. Annexin V has been utilized for imaging and drug delivery [56] and is an attractive [57, 58] (though perhaps hard-to-patent) candidate for developmental therapeutics. Alternatively, monoclonal antibodies to phosphatidylserine have been produced [59] and proposed as potential anti-viral agents [37]. Since many proteins, notably including those involved in blood coagulation, have PS-binding domains, protein engineering of high-affinity, non-immunogenic proteins would be another avenue to pursue.
Novel treatments that are only based upon tests of circulating procoagulant PS run the risk of overlooking possible benefits of endothelial-directed PS-neutralizing therapies. Endothelial cells express receptors for SARS-CoV-2, and endothelial cell budding of the virus may result in endothelial surface expression of PS. Some therapies might prove to be useful by targeting PS on endothelial surfaces, even in the absence of circulating PS. Imaging of vascular beds may be useful in documenting PS-exposing endothelium, since the surface area of the vascular system is quite large [60]. Development of such imaging modalities could be used not only to explore the contribution of the endothelium to thrombosis in severe infections, but other conditions where endothelial dysfunction may contribute to pathophysiology, such as acute kidney injury or systemic hypotension. Studies with an engineered annexin V dimer, for example, suggest its potential for improving health, even in the absence of proof of high levels of circulating PS in targeted disease states [61, 62, 63].
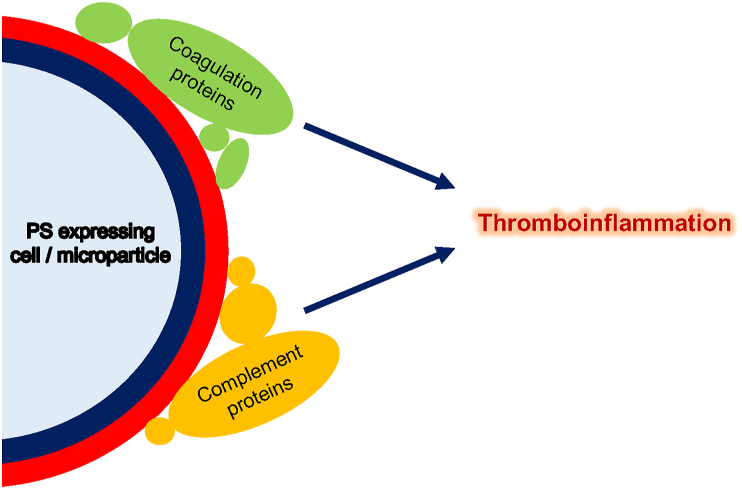
There are a number of additional reasons for the research community to turn its attention to the importance of “exposed” (i.e. procoagulant) PS: 1) there is a documented interaction between PS and the complement system, shown to be activated in COVID-19 and likely other infectious states [64]. Complement-mediated injury of cells leads to exposure of procoagulant PS on the cell surface, thereby promoting thrombosis [22, 65] (Figure 2). Further, exposure of PS leads to activation of the complement system, as shown with apoptotic cells [66]; 2) Immune suppression is recognized to accompany exposure of apopotic (i.e. PS-bearing cells) to macrophages [67], and may play a role in the development of secondary infections in patients with COVID-19 and/or other critical illnesses [68]; 3) several plasma proteins bind to PS, and some may play a protective role in neutralizing the effect of PS upon coagulation and inflammatory pathways. Provision of these proteins by plasma infusions may be useful for future pandemics before specific antibodies are available for treatment or may explain beneficial effects of plasma infusions that do not contain appreciable amounts of antibody; 4) exaggerated release of PS-containing microparticles from platelets, neutrophils and monocytes of diabetic patients [69] may explain, in part, the increased susceptibility diabetic patients to COVID-19; and 5) PS may be an unrecognized but active contaminant of many biological preparations [70].
Figure 2.
Phosphatidylserine exposure on the surface of cells exposed to plasma results in thrombin generation and complement system activation - Blood coagulation proteins have phosphatidylserine-binding domains, which allows them to cluster together on exposed PS, accelerating their interaction and the subsequent generation of thrombin. PS can lead to activation of the complement system. Together, the coagulation and complement systems contribute to the complex clinical phenotype of thromboinflammation.
6. Summary
PS may be an overlooked actor in many inflammatory states and should become the subject of more robust and widely available testing. Inflammation always involves multiple mediators and regulatory pathways, and it is unlikely that a single molecular entity (or novel blood test) will fully explain the wide spectrum of host responses in complex disease states. In fact, therapeutic interventions may ultimately be required to define which of many possible mediators are active in a given sub-group of patients. Increasingly, molecules that are familiar to us because of their defined roles in intracellular biochemistry (such as ADP, DNA, histones, polyphosphate, and actin) are being found to play important extracellular roles in a variety of pathophysiologic states. Phosphatidylserine (PS) should be added to this list so that it too is considered when multi-disciplinary approaches to critical illness are considered. A “procoagulant phospholipidopathy” may emerge as a heretofore unrecognized mediator of morbidity and mortality in several disease states.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
No data was used for the research described in the article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Iba T., Levy J.H., Levi M., Connors J.M., Thachil J. Coagulopathy of Coronavirus disease 2019. Crit. Care Med. 2020;48(9):1358–1364. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Samkari H., Karp Leaf R.S., Dzik W.H., Carlson J.C.T., Fogerty A.E., Waheed A. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136(4):489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rollin P.E., Bausch D.G., Sanchez A. Blood chemistry measurements and D-Dimer levels associated with fatal and nonfatal outcomes in humans infected with Sudan Ebola virus. J. Infect. Dis. 2007;196(Suppl 2):S364–S371. doi: 10.1086/520613. [DOI] [PubMed] [Google Scholar]
- 4.Laine O., Makela S., Mustonen J., Huhtala H., Szanto T., Vaheri A. Enhanced thrombin formation and fibrinolysis during acute Puumala hantavirus infection. Thromb. Res. 2010;126(2):154–158. doi: 10.1016/j.thromres.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 5.Hasanoglu I., Guner R., Carhan A., Kocak Tufan Z., Yagci-Caglayik D., Guven T. Crucial parameter of the outcome in Crimean Congo hemorrhagic fever: viral load. J. Clin. Virol. 2016;75:42–46. doi: 10.1016/j.jcv.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Ewers E.C., Pratt W.D., Twenhafel N.A., Shamblin J., Donnelly G., Esham H. Natural history of aerosol exposure with Marburg virus in rhesus macaques. Viruses. 2016;8(4):87. doi: 10.3390/v8040087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jong J.B., Pohan H.T., Zulkarnain I., Tambunan K.L., Panggabean M.M., Setiabudy R.D. The correlation between coagulation test and albumin with antithrombin III in Dengue hemorrhagic fever. Acta Med. Indones. 2004;36(2):57–61. [PubMed] [Google Scholar]
- 8.Magro C., Mulvey J.J., Berlin D., Nuovo G., Salvatore S., Harp J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl. J. Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bikdeli B., Madhavan M.V., Gupta A., Jimenez D., Burton J.R., Der Nigoghossian C. Pharmacological agents targeting thromboinflammation in COVID-19: review and implications for future research. Thromb. Haemostasis. 2020;120(7):1004–1024. doi: 10.1055/s-0040-1713152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merrill J.T., Erkan D., Winakur J., James J.A. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat. Rev. Rheumatol. 2020:1–9. doi: 10.1038/s41584-020-0474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leventis P.A., Grinstein S. The distribution and function of phosphatidylserine in cellular membranes. Annu. Rev. Biophys. 2010;39:407–427. doi: 10.1146/annurev.biophys.093008.131234. [DOI] [PubMed] [Google Scholar]
- 14.Clarke R.J., Hossain K.R., Cao K. Physiological roles of transverse lipid asymmetry of animal membranes. Biochim. Biophys. Acta Biomembr. 2020;1862(10):183382. doi: 10.1016/j.bbamem.2020.183382. [DOI] [PubMed] [Google Scholar]
- 15.Jackson S.P., Darbousset R., Schoenwaelder S.M. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133(9):906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 16.Franck P.F., Bevers E.M., Lubin B.H., Comfurius P., Chiu D.T., Op den Kamp J.A. Uncoupling of the membrane skeleton from the lipid bilayer. The cause of accelerated phospholipid flip-flop leading to an enhanced procoagulant activity of sickled cells. J. Clin. Invest. 1985;75(1):183–190. doi: 10.1172/JCI111672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Föller M., Lang F. Ion transport in eryptosis, the suicidal death of erythrocytes. Front. Cell Dev. Biol. 2020;8:597. doi: 10.3389/fcell.2020.00597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.VanDeWater L., Tracy P.B., Aronson D., Mann K.G., Dvorak H.F. Tumor cell generation of thrombin via functional prothrombinase assembly. Canc. Res. 1985;45(11 Pt 1):5521–5525. [PubMed] [Google Scholar]
- 19.Bastida E., Escolar G., Ordinas A., Jamieson G.A. Morphometric evaluation of thrombogenesis by microvesicles from human tumor cell lines with thrombin-dependent (U87MG) and adenosine diphosphate-dependent (SKNMC) platelet-activating mechanisms. J. Lab. Clin. Med. 1986;108(6):622–627. [PubMed] [Google Scholar]
- 20.Gasser O., Hess C., Miot S., Deon C., Sanchez J.C., Schifferli J.A. Characterisation and properties of ectosomes released by human polymorphonuclear neutrophils. Exp. Cell Res. 2003;285(2):243–257. doi: 10.1016/s0014-4827(03)00055-7. [DOI] [PubMed] [Google Scholar]
- 21.Satta N., Toti F., Feugeas O., Bohbot A., Dachary-Prigent J., Eschwege V. Monocyte vesiculation is a possible mechanism for dissemination of membrane-associated procoagulant activities and adhesion molecules after stimulation by lipopolysaccharide. J. Immunol. 1994;153(7):3245–3255. [PubMed] [Google Scholar]
- 22.Hamilton K.K., Hattori R., Esmon C.T., Sims P.J. Complement proteins C5b-9 induce vesiculation of the endothelial plasma membrane and expose catalytic surface for assembly of the prothrombinase enzyme complex. J. Biol. Chem. 1990;265(7):3809–3814. [PubMed] [Google Scholar]
- 23.Combes V., Simon A.C., Grau G.E., Arnoux D., Camoin L., Sabatier F. In vitro generation of endothelial microparticles and possible prothrombotic activity in patients with lupus anticoagulant. J. Clin. Invest. 1999;104(1):93–102. doi: 10.1172/JCI4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fadok V.A., Voelker D.R., Campbell P.A., Cohen J.J., Bratton D.L., Henson P.M. Exposure of phosphatidylserine on the surface of apoptotic lymphocytes triggers specific recognition and removal by macrophages. J. Immunol. 1992;148(7):2207–2216. [PubMed] [Google Scholar]
- 25.Shlomovitz I., Speir M., Gerlic M. Flipping the dogma - phosphatidylserine in non-apoptotic cell death. Cell Commun. Signal. 2019;17(1):139. doi: 10.1186/s12964-019-0437-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lentz B.R. Exposure of platelet membrane phosphatidylserine regulates blood coagulation. Prog. Lipid Res. 2003;42(5):423–438. doi: 10.1016/s0163-7827(03)00025-0. [DOI] [PubMed] [Google Scholar]
- 27.von Kügelgen I. Molecular pharmacology of P2Y receptor subtypes. Biochem. Pharmacol. 2020:114361. doi: 10.1016/j.bcp.2020.114361. [DOI] [PubMed] [Google Scholar]
- 28.Shi C., Yang L., Braun A., Anders H.J. Extracellular DNA-A danger signal triggering immunothrombosis. Front. Immunol. 2020;11:568513. doi: 10.3389/fimmu.2020.568513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meara C.H.O., Coupland L.A., Kordbacheh F., Quah B.J.C., Chang C.W., Simon Davis D.A. Neutralizing the pathological effects of extracellular histones with small polyanions. Nat. Commun. 2020;11(1):6408. doi: 10.1038/s41467-020-20231-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith S.A., Gajsiewicz J.M., Morrissey J.H. Ability of polyphosphate and nucleic acids to trigger blood clotting: some observations and caveats. Front. Med. 2018;5:107. doi: 10.3389/fmed.2018.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gajsiewicz J.M., Smith S.A., Morrissey J.H. Polyphosphate and RNA differentially modulate the contact pathway of blood clotting. J. Biol. Chem. 2017;292(5):1808–1814. doi: 10.1074/jbc.M116.754325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coleman J.R., Moore E.E., Freeman K., Grubinger N.D., Hennig G.W., Cohen M.J. Actin is associated with tissue injury in trauma patients and produces a hypercoagulable profile in vitro. J. Trauma Acute Care Surg. 2020;89(1):87–95. doi: 10.1097/TA.0000000000002739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rothman J.E., Tsai D.K., Dawidowicz E.A., Lenard J. Transbilayer phospholipid asymmetry and its maintenance in the membrane of influenza virus. Biochemistry. 1976;15(11):2361–2370. doi: 10.1021/bi00656a018. [DOI] [PubMed] [Google Scholar]
- 34.Pryzdial E.L., Wright J.F. Prothrombinase assembly on an enveloped virus: evidence that the cytomegalovirus surface contains procoagulant phospholipid. Blood. 1994;84(11):3749–3757. [PubMed] [Google Scholar]
- 35.Aupeix K., Hugel B., Martin T., Bischoff P., Lill H., Pasquali J.L. The significance of shed membrane particles during programmed cell death in vitro, and in vivo, in HIV-1 infection. J. Clin. Invest. 1997;99(7):1546–1554. doi: 10.1172/JCI119317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morizono K., Chen I.S. Role of phosphatidylserine receptors in enveloped virus infection. J. Virol. 2014;88(8):4275–4290. doi: 10.1128/JVI.03287-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soares M.M., King S.W., Thorpe P.E. Targeting inside-out phosphatidylserine as a therapeutic strategy for viral diseases. Nat. Med. 2008;14(12):1357–1362. doi: 10.1038/nm.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salamanna F., Maglio M., Landini M.P., Fini M. Body localization of ACE-2: on the trail of the keyhole of SARS-CoV-2. Front. Med. 2020;7(935) doi: 10.3389/fmed.2020.594495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saber S.H., Ali H.E.A., Gaballa R., Gaballah M., Ali H.I., Zerfaoui M. Exosomes are the driving force in preparing the soil for the metastatic seeds: lessons from the prostate cancer. Cells. 2020;9(3) doi: 10.3390/cells9030564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang W., Zhou X., Zhang H., Yao Q., Liu Y., Dong Z. Extracellular vesicles in diagnosis and therapy of kidney diseases. Am. J. Physiol. Ren. Physiol. 2016;311(5):F844–F851. doi: 10.1152/ajprenal.00429.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kubo H. Extracellular vesicles in lung disease. Chest. 2018;153(1):210–216. doi: 10.1016/j.chest.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 42.Santilli F., Marchisio M., Lanuti P., Boccatonda A., Miscia S., Davi G. Microparticles as new markers of cardiovascular risk in diabetes and beyond. Thromb. Haemostasis. 2016;116(2):220–234. doi: 10.1160/TH16-03-0176. [DOI] [PubMed] [Google Scholar]
- 43.Zaldivia M.T.K., McFadyen J.D., Lim B., Wang X., Peter K. Platelet-derived microvesicles in cardiovascular diseases. Front. Cardiovasc. Med. 2017;4:74. doi: 10.3389/fcvm.2017.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Connor D.E., Exner T., Ma D.D., Joseph J.E. The majority of circulating platelet-derived microparticles fail to bind annexin V, lack phospholipid-dependent procoagulant activity and demonstrate greater expression of glycoprotein Ib. Thromb. Haemostasis. 2010;103(5):1044–1052. doi: 10.1160/TH09-09-0644. [DOI] [PubMed] [Google Scholar]
- 45.Cointe S., Judicone C., Robert S., Mooberry M.J., Poncelet P., Wauben M. Standardization of microparticle enumeration across different flow cytometry platforms: results of a multicenter collaborative workshop. J. Thromb. Haemostasis. 2017;15(1):187–193. doi: 10.1111/jth.13514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howard M.A., Coghlan M., David R., Pfueller S.L. Coagulation activities of plasma microparticles. Thromb. Res. 1988;50(1):145–156. doi: 10.1016/0049-3848(88)90182-x. [DOI] [PubMed] [Google Scholar]
- 47.Jy W., Horstman L.L., Wang F., Duncan R.C., Ahn Y.S. Platelet factor 3 in plasma fractions: its relation to microparticle size and thromboses. Thromb. Res. 1995;80(6):471–482. doi: 10.1016/0049-3848(95)00202-2. [DOI] [PubMed] [Google Scholar]
- 48.Exner T., Joseph J., Low J., Connor D., Ma D. A new activated factor X-based clotting method with improved specificity for procoagulant phospholipid. Blood Coagul. Fibrinolysis. 2003;14(8):773–779. doi: 10.1097/00001721-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Stagnara J., Garnache Ottou F., Angelot F., Mourey G., Seilles E., Biichle S. Correlation between platelet-derived microparticle enumeration by flow cytometry and phospholipid-dependent procoagulant activity in microparticles: the centrifugation step matters! Thromb. Haemostasis. 2012;107(6):1185–1187. doi: 10.1160/TH11-07-0509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chap H., Comfurius P., Bevers E.M., Fauvel J., Vicendo P., Douste-Blazy L. Potential anticoagulant activity of lipocortins and other calcium/phospholipid binding proteins. Biochem. Biophys. Res. Commun. 1988;150(3):972–978. doi: 10.1016/0006-291x(88)90724-3. [DOI] [PubMed] [Google Scholar]
- 51.Shi J., Gilbert G.E. Lactadherin inhibits enzyme complexes of blood coagulation by competing for phospholipid-binding sites. Blood. 2003;101(7):2628–2636. doi: 10.1182/blood-2002-07-1951. [DOI] [PubMed] [Google Scholar]
- 52.Gonzalez-Conejero R., Corral J., Roldan V., Martinez C., Marin F., Rivera J. A common polymorphism in the annexin V Kozak sequence (-1C>T) increases translation efficiency and plasma levels of annexin V, and decreases the risk of myocardial infarction in young patients. Blood. 2002;100(6):2081–2086. [PubMed] [Google Scholar]
- 53.Kuypers F.A., Larkin S.K., Emeis J.J., Allison A.C. Interaction of an annexin V homodimer (Diannexin) with phosphatidylserine on cell surfaces and consequent antithrombotic activity. Thromb. Haemostasis. 2007;97(3):478–486. [PubMed] [Google Scholar]
- 54.Tait J.F., Engelhardt S., Smith C., Fujikawa K. Prourokinase-annexin V chimeras. Construction, expression, and characterization of recombinant proteins. J. Biol. Chem. 1995;270(37):21594–21599. doi: 10.1074/jbc.270.37.21594. [DOI] [PubMed] [Google Scholar]
- 55.Huang X., Ding W.Q., Vaught J.L., Wolf R.F., Morrissey J.H., Harrison R.G. A soluble tissue factor-annexin V chimeric protein has both procoagulant and anticoagulant properties. Blood. 2006;107(3):980–986. doi: 10.1182/blood-2005-07-2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schutters K., Reutelingsperger C. Phosphatidylserine targeting for diagnosis and treatment of human diseases. Apoptosis. 2010;15(9):1072–1082. doi: 10.1007/s10495-010-0503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kennedy J.R. Attenuating a sickle cell crisis with annexin V. Med. Hypotheses. 2015;84(5):434–436. doi: 10.1016/j.mehy.2015.01.037. [DOI] [PubMed] [Google Scholar]
- 58.Kennedy J.R. Phosphatidylserine's role in Ebola's inflammatory cytokine storm and hemorrhagic consumptive coagulopathy and the therapeutic potential of annexin V. Med. Hypotheses. 2020;135:109462. doi: 10.1016/j.mehy.2019.109462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beck A.W., Luster T.A., Miller A.F., Holloway S.E., Conner C.R., Barnett C.C. Combination of a monoclonal anti-phosphatidylserine antibody with gemcitabine strongly inhibits the growth and metastasis of orthotopic pancreatic tumors in mice. Int. J. Canc. 2006;118(10):2639–2643. doi: 10.1002/ijc.21684. [DOI] [PubMed] [Google Scholar]
- 60.Pries A.R., Secomb T.W., Gaehtgens P. The endothelial surface layer. Pflügers Archiv. 2000;440(5):653–666. doi: 10.1007/s004240000307. [DOI] [PubMed] [Google Scholar]
- 61.Shen X.D., Ke B., Zhai Y., Tsuchihashi S.I., Gao F., Duarte S. Diannexin, a novel annexin V homodimer, protects rat liver transplants against cold ischemia-reperfusion injury. Am. J. Transplant. 2007;7(11):2463–2471. doi: 10.1111/j.1600-6143.2007.01967.x. [DOI] [PubMed] [Google Scholar]
- 62.Beattie G., Cohan C., Miraflor E., Brigode W., Victorino G.P. Protective effect of phosphatidylserine blockade in sepsis induced organ dysfunction. Surgery. 2019;166(5):844–848. doi: 10.1016/j.surg.2019.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cohan C., Beattie G., Brigode W., Yeung L., Miraflor E., Victorino G.P. Protective effect of phosphatidylserine blockade in hemorrhagic shock. J. Surg. Res. 2020;245:604–609. doi: 10.1016/j.jss.2019.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Song W.C., FitzGerald G.A. COVID-19, microangiopathy, hemostatic activation, and complement. J. Clin. Invest. 2020;130(8):3950–3953. doi: 10.1172/JCI140183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sims P.J., Faioni E.M., Wiedmer T., Shattil S.J. Complement proteins C5b-9 cause release of membrane vesicles from the platelet surface that are enriched in the membrane receptor for coagulation factor Va and express prothrombinase activity. J. Biol. Chem. 1988;263(34):18205–18212. [PubMed] [Google Scholar]
- 66.Mevorach D., Mascarenhas J.O., Gershov D., Elkon K.B. Complement-dependent clearance of apoptotic cells by human macrophages. J. Exp. Med. 1998;188(12):2313–2320. doi: 10.1084/jem.188.12.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kornbluth R.S. The immunological potential of apoptotic debris produced by tumor cells and during HIV infection. Immunol. Lett. 1994;43(1-2):125–132. doi: 10.1016/0165-2478(94)00149-9. [DOI] [PubMed] [Google Scholar]
- 68.Vaillancourt M., Jorth P. The unrecognized threat of secondary bacterial infections with COVID-19. mBio. 2020;11(4) doi: 10.1128/mBio.01806-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li S., Wei J., Zhang C., Li X., Meng W., Mo X. Cell-derived microparticles in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Cell. Physiol. Biochem. 2016;39(6):2439–2450. doi: 10.1159/000452512. [DOI] [PubMed] [Google Scholar]
- 70.Novakovic V., Gilbert G.E. Procoagulant activities of skeletal and cardiac muscle myosin depend on contaminating phospholipid. Blood. 2020 doi: 10.1182/blood.2020005930. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.